Abstract
Background
CT allows for accurate measurement of acetabular orientation and shape, but malpositioning of the pelvis may lead to measurement variance.
Purpose
We therefore sought to determine: (1) whether acetabular anteversion measurements using the femoral head centers differed from those using the posterior ischia, and (2) the extent to which changing obliquity, rotation, and tilt of a pelvis in a CT scanner affected the measurement of acetabular variables.
Methods
A radiopaque human pelvis model with articulated hips was suspended from a plastic sheet as part of an adjustable frame. Changes in the transverse and sagittal planes created rotation and tilt, while rotating the frame in the coronal plane created obliquity. CT scans were obtained, varying the combinations of obliquity, rotation, and tilt by intervals of 5°, up to 20°. Acetabular anteversion (AA), anterior acetabular sector angle (AASA), posterior acetabular sector angle (PASA), and horizontal acetabular sector angle (HASA) were measured.
Results
The two methods for measuring AA yielded values differing by 1° to 4° but correlated (r = 0.981) across the spectrum of pelvis positioning. Pelvic obliquity and tilt were linearly associated with changes in the measurements. For each 1°-increase in pelvic obliquity, AA changed −0.4°, and AASA, PASA, and HASA changed 1.93°, 0.99°, and 2.80°, respectively. For each 1°-increase in pelvic tilt, AA changed 0.8°, and AASA, PASA, and HASA changed −1.07°, 0.52°, and −0.51°, respectively. Rotation had no affect on the variables.
Conclusions
Small changes in pelvic obliquity and tilt were associated with variances in acetabular measurements. The measured changes were directly proportional to the changes in obliquity and tilt, and were additive. Pelvic rotation created no changes in measurement.
Clinical Relevance
Incorrect interpretation of acetabular anteversion and coverage may lead to unsatisfactory acetabular fragment positioning during reorientational surgery. Although intraoperative positioning of an acetabular fragment may not be as precise as the tools for preoperative planning, it is important for a surgeon to have the most precise data available for planning a procedure, and know where error can occur in collecting the data.
Introduction
Surgical advancements in the treatment of acetabular dysplasia include multiple techniques that reorient the acetabulum to achieve better femoral head coverage [17, 38, 51]. When successfully performed, a reorientation will increase the hip surface contact area, decrease joint pressures, and reduce potential femoroacetabular impingement [8, 18, 21, 37, 46]. Intermediate and longer-term followup studies report survival rates of 72% to 87% at 9 years or greater [20, 35, 47, 53, 60], and a 20-year delay before the Merle d’Aubigné and Postel scores returned to their preoperative values [47]. Thawrani et al. found that the percentage of hips with no radiographic signs of osteoarthritis (Tönnis grade 0) increased from 11% preoperatively to 41% at greater than 2 years after pelvic osteotomy [50].
Achieving optimal placement of the acetabular fragment is one of the biggest challenges of an acetabular reorientation [40, 50, 54]. Malpositioning leads to insufficient femoral head coverage, restricted ROM, femoroacetabular impingement, and progressive osteoarthritis leading to hip arthroplasty [9, 16, 20, 28, 53]. The position for optimal correction is specific for each patient, and fairly narrowly defined [54]. Tsumura et al. studied three-dimensional joint pressure redistribution in dysplastic hips, and noted that the lowest peak pressures were achieved by transposing the acetabular fragment to within 5° of the optimal transposition point [55]. Individualized preoperative planning with understanding of a patient’s specific deformity is crucial to proper acetabular reorientation [21, 40, 46, 56]. For example, uncovering of the femoral head by excessive acetabular anteversion or over-covering by retroversion are associated with acetabular dysplasia, hip pain, and development of osteoarthritis, but are addressed differently surgically [2, 11, 42, 43, 46, 49, 52]. Accurate preoperative knowledge of the patient’s pathoanatomy requires thorough diagnostic imaging of the hip [3, 17, 19, 34, 52].
Plain radiographs are important for assessing the acetabular shape and morphologic features [15, 25, 30, 31, 43, 46]. Accurate assessment of acetabular version and anterior and posterior femoral head coverage can be difficult, and changes in patient positioning can lead to errors in measurement [4, 24, 45, 48]. Two-dimensional CT studies have become an integral part of diagnosis and preoperative planning, especially when assessing deficiencies in the transverse plane [5, 26, 29, 33, 41, 59]. They allow for assessment of acetabular version and anterior and posterior femoral head coverage, defined by acetabular sector angles [4, 7, 22]. Patient positioning has the potential to cause errors in measurements on CT studies just as it does with plain radiographs. Abel et al. observed the acetabular anteversion decreased 30° as pelvic tilt was varied from 15° posterior tilt to 35° anterior tilt [1]. Anda et al. similarly found a change of 0.5° in anteversion and 0.7° in acetabular sector angles for every 1°-change in pelvic tilt [4, 5]. Visser et al. noted that pelvic tilt changed measured anteversion, but rotation along the body’s longitudinal axis did not [58]. Whether pelvic measurements vary with differing pelvic obliquity is unclear. However, we presumed altering the position of the pelvis in the CT scanner would cause variance in measurements of the acetabulum. There are differing ways to define and to measure acetabular anteversion on CT scans [4, 5, 7, 29, 32, 41, 52, 57–59], although it is unclear how these differing methods influence the values of anteversion.
We therefore sought to determine: (1) whether acetabular anteversion measurements using the femoral head centers differed from those using the posterior ischia and (2) the extent to which changing obliquity, rotation, and tilt of a pelvis in a CT scanner affected the measurement of acetabular variables.
Materials and Methods
We mounted a radiopaque model of a human pelvis (Sawbones, Vashon, WA, USA) on a frame in a CT scanner, so that the orientational variables of pelvic obliquity, rotation, and tilt could be changed. The acetabular variables of AA, AASA, PASA, and HASA were measured with different positions of the orientational variables, and these measurements were compared with the values found when the pelvis model was positioned anatomically.
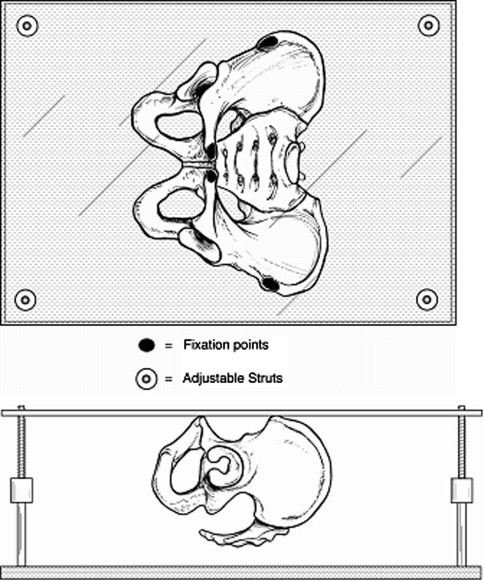
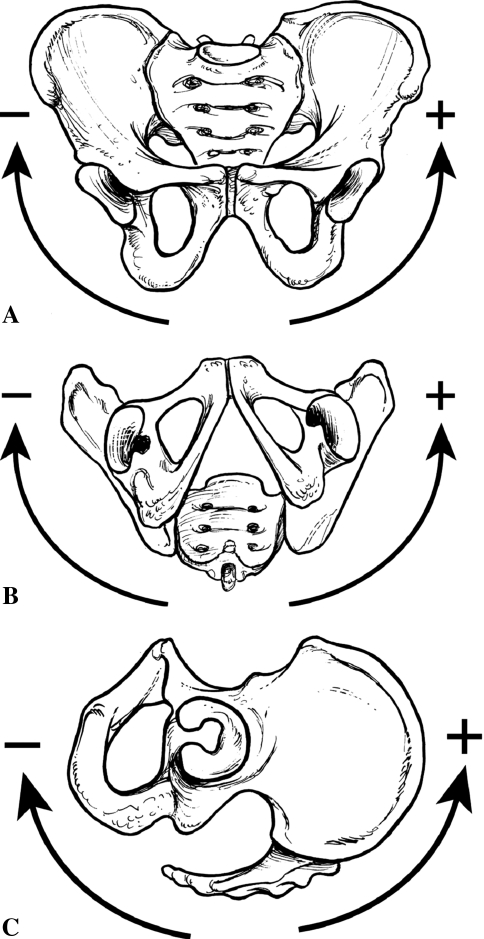
The frame was constructed of a rectangular clear plastic sheet from which the pelvis model was suspended by its anterior-superior iliac spines and pubic symphysis, using epoxy. The plastic sheet then was mounted over a rectangular wooden base using four adjustable struts, one at each corner (Fig. 1). When all four struts were of equal length and a line drawn between the anterior-superior iliac spines was parallel to the transverse laser reference beam of the CT scanner, the pelvis was positioned anatomically, according to McKibbin’s definition (the top of the symphysis pubis in the same coronal plane as the anterior-superior iliac spines, and the anterior-superior iliac spines in the same transverse plane) [36]. The struts were adjusted to reposition the pelvis model around axes perpendicular to the transverse and sagittal planes, thereby creating pelvic rotation and tilt, respectively. Pelvic rotation and tilt adjustments were set relative to the floor using an inclinometer. Pelvic obliquity was created by revolving the entire frame around an axis perpendicular to the coronal plane. A plastic compass was mounted on the frame’s plastic sheet, aligned anatomically with the anterior-superior iliac spines. The desired angle of obliquity was obtained using the CT scanner’s laser reference beams and the compass. As a matter of convention, positioning was defined as either positive or negative for the orientational variables. In obliquity, the hemipelvis that moved cephalad moved in a positive direction, whereas the contralateral side, moving caudad, had a negative obliquity (Fig. 2A). In rotation, the hemipelvis that moved anteriorly moved in a positive direction, and the contralateral side, moving posteriorly, rotated in a negative direction (Fig. 2B). For tilt, the positive direction was defined as tilting the superior pelvis anteriorly (pelvic extension), while the negative direction was defined as tilting the superior pelvis posteriorly (Fig. 2C).
Fig. 1.
A drawing shows how the pelvis model was mounted in the anatomic plane.
Fig. 2A–C.
(A) Positive and negative directions for pelvic obliquity, in reference to the left hip, are shown. For the right hip, positive and negative directions would be reversed. (B) Positive and negative directions for pelvic rotation, in reference to the left hip, are shown. For the right hip, positive and negative would be reversed. (C) Positive and negative directions for pelvic tilt, in reference to the left hip, are shown.
The orientational variables were varied by increments of 5°, from −20° to 20°. CT images of the pelvis model were obtained at 3-mm increments using a GE HiSpeed Advantage RP spiral scanner (GE Healthcare Bio-Sciences Corp, Piscataway, NJ, USA). A total of 729 combinations of orientational variables were possible. All acetabular variable measurements were recorded as the variance from the measurement obtained at the anatomic position defined by McKibbin [36]. Therefore, even if the two acetabula of the pelvis model were not exact mirror images, the measurements obtained could still be compared and interchanged, as they were not an absolute number, but were instead the amount of change attributable to the pelvic positioning. Orientating the pelvis model to create positive obliquity for one acetabulum would simultaneously create negative obliquity for the contralateral acetabulum. The same was true for pelvic rotation. Therefore, only 369 sequences needed to be completed to create all the combinations of the orientational variables. For each sequence, a representative slice was needed for each acetabulum where the femoral head was at its largest and most circular dimension, and the center of the contralateral femoral head could be determined [44]. With extremes of pelvic positioning, some measurements could not be made owing to the absence of the required anatomy in the CT frame, and these sequences were excluded. A total of 182 sequences (324 acetabular positions) met the criteria for use in the study.
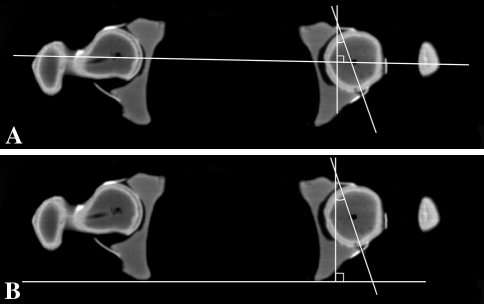
One of us (HvB) measured AA, AASA, PASA, and HASA for each sequence. Three methods of measuring AA have been described, differing only in the landmarks used to orient the transverse reference or baseline: bilateral femoral head centers (Fig. 3A) [4, 5, 7, 32], the posterior walls of bilateral acetabula [27, 52, 57, 58], and posterior aspects of bilateral ischia (Fig. 3B) [41, 59]. To see if there were any substantive differences between the various methods, we compared AAs using the femoral head centers (AAFemoral) and the posterior ischia (AAIschial).
Fig. 3A–B.
The CT scans show how the AA measurement used (A) femoral head centers and (B) posterior aspects of the ischium for reference.
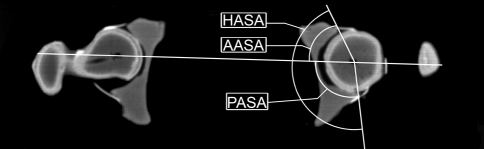
Sector angle measurements using two-dimensional CT were described originally by Anda et al. [4, 6] (Fig. 4). A baseline through the center of the femoral heads was drawn. The AASA was described as the angle between the baseline and the line from the center of the femoral head to the anterior acetabular margin. Similarly, the PASA was the angle between the baseline and a line from the center of the femoral head to the posterior acetabular margin. The HASA was calculated by adding the AASA to the PASA. In the case of an otherwise normal acetabulum with excessive anteversion, the AASA is expected to increase, the PASA to decrease, and the HASA to remain unchanged. In cases of dysplasia, the HASA should become smaller as the entire acetabulum becomes shallower.
Fig. 4.
A CT scan shows the acetabular sector angle measurements: AASA = anterior acetabular sector angle; PASA = posterior acetabular sector angle; HASA = horizontal acetabular sector angle.
We determined the correlation between the two methods of AA measurement, AAIschial and AAFemoral, using the Pearson Product Moment Correlation Coefficient (r). Acetabular variables were plotted on a scatter plot as a function of each orientational variable, to assess the linearity of the results. The individual effects of varying the orientational variables (pelvic obliquity, rotation, and tilt) on acetabular variable measurements (AAIschial, AAFemoral, AASA, PASA, HASA) were determined using multiple regression analysis (SPSS 10.0 software, SPSS Inc, Chicago, IL, USA). From these data, equations were generated for predicting the change expected in an acetabular variable for a given position of obliquity, rotation, or tilt. We defined an acceptable measurement error as +/− 3° variance from the value at the anatomic position for each of the acetabular variables. We then used the equations to calculate the maximum allowable degrees of obliquity, rotation, or tilt to limit the measurement variance to +/− 3°. Our purpose was to identify an allowable range of obliquity, rotation, and tilt that would alter the acetabular variable measurements by 3° or less.
Results
The two methods for measuring AA, AAIschail and AAFemoral, yielded values differing by 1° to 4°, but otherwise were correlated (r = 0.981) across the spectrum of pelvis positioning.
The individual acetabular variable measurements had a direct or linear relationship with the different orientational variables.
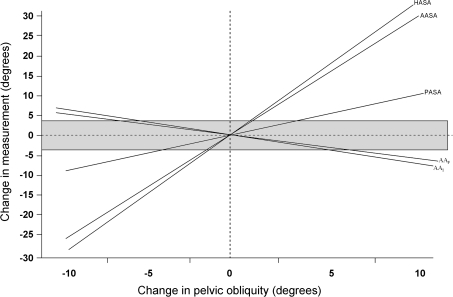
Pelvic obliquity was a source of variance in the AA and sector angles (Table 1). For every degree obliquity increased, the measured AAIschial and AAFemoral decreased (p < 0.001) by approximately 0.4°. Therefore, maintaining measurement variance to +/− 3° for either AAFemoral or AAIschial would require keeping the obliquity less than 7°. The three sector angles, AASA, PASA, and HASA, also were affected by changing obliquity. For each 1°-change in pelvic obliquity, AASA, PASA, and HASA changed 1.93°, 0.99°, and 2.80°, respectively. Therefore, the maximum allowable variance of +/− 3° for AASA, PASA, and HASA would occur for an obliquity of +/− 1.6°, 3.0°, and 1.1°, respectively (Fig. 5).
Table 1.
Acetabular and orientational variables
| Acetabular variable | Value at anatomic position | Acetabular variable range (net range) | Orientational variable | Individual variance contribution (%) | Significance of variance contribution (p value) | Allowable change in orientational variable with ± 3° change in acetabular variable |
|---|---|---|---|---|---|---|
| AAI | 28° | −7° to 44° (51°) | Obliquity | 11.5 | < 0.0001 | +/− 6.8° |
| Rotation | 0.0 | 0.93 | NS | |||
| Tilt | 62.0 | < 0.0001 | +/− 3.9° | |||
| AAF | 24° | −5° to 43° (48°) | Obliquity | 10.4 | < 0.0001 | +/− 7.1° |
| Rotation | 0.0 | 0.70 | NS | |||
| Tilt | 65.1 | < 0.0001 | +/− 4.0° | |||
| AASA | 67° | 41° to 136° (95°) | Obliquity | 41.1 | < 0.0001 | +/− 1.6° |
| Rotation | 0.0 | 0.55 | NS | |||
| Tilt | 23.0 | < 0.0001 | +/− 2.8° | |||
| PASA | 115° | 91° to 146° (55°) | Obliquity | 39.7 | < 0.0001 | +/− 3.0° |
| Rotation | 0.8 | 0.0538 | NS | |||
| Tilt | 20.1 | < 0.0001 | +/− 5.8° | |||
| HASA | 182° | 145° to 277° (132°) | Obliquity | 53.7 | < 0.0001 | +/− 1.1° |
| Rotation | 0.5 | 0.18 | NS | |||
| Tilt | 3.3 | 0.0004 | +/− 5.9° |
AAI = acetabular anteversion referenced by posterior ischia; AAF = acetabular anteversion referenced by femoral head centers; AASA = anterior acetabular sector angle; PASA = posterior acetabular sector angle; HASA = horizontal acetabular sector angle; NS = not significant.
Fig. 5.
A graph shows the changes in pelvic measurements attributable to changing pelvic obliquity. The gray zone denotes measurements +/− 3° of the measurement at anatomic position. The dotted lines correspond to the amount of obliquity at which the corresponding measurement exceeds 3° from the measurement at anatomic position. AAI = acetabular anteversion referenced by posterior ischia; AAF = acetabular anteversion referenced by femoral head centers; AASA = anterior acetabular sector angle; PASA = posterior acetabular sector angle; HASA = horizontal acetabular sector angle.
Changing pelvic rotation had no effect on the AAs measured. Likewise, the three sector angles were unaffected by rotation.
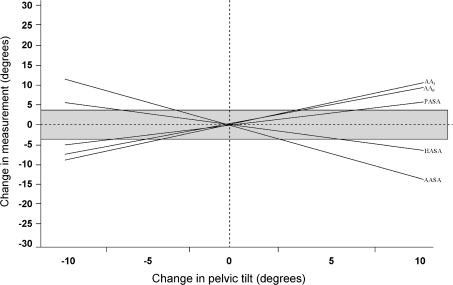
Pelvic tilt was a source of substantial variance in measurements for acetabular variables. It was responsible for 62% of the observed measurement variance for AA. For each 1°-change in pelvic tilt, AAFemoral changed 0.77° and AAIschial changed 0.75° (p < 0.001 and p < 0.001 respectively). Therefore, maintaining the variance to +/− 3° for either AA measurement would require keeping the tilt at less than 4°. The three sector angles, AASA, PASA, and HASA, also were affected by tilt (p < 0.001, p < 0.001, p = 0.0004, respectively). With each 1°-change in pelvic tilt, AASA changed −1.07°, PASA changed 0.52°, and HASA changed −0.51°. Also, the maximum allowable variance of +/− 3° for AASA, PASA, and HASA would occur for a tilt of +/− 2.8°, 5.8°, and 5.9°, respectively (Fig. 6).
Fig. 6.
A graph shows the changes in pelvic measurements attributable to changing pelvic tilt. The gray zone denotes measurements +/− 3° of the measurement at anatomic position. The dotted lines correspond to the amount of tilt at which the corresponding measurement exceeds 3° from the measurement at anatomic position. AAI = acetabular anteversion referenced by posterior ischia; AAF = acetabular anteversion referenced by femoral head centers; AASA = anterior acetabular sector angle; PASA = posterior acetabular sector angle; HASA = horizontal acetabular sector angle.
Changing both orientational parameters of obliquity and tilt created an additive change in the acetabular variables. We developed equations for predicting the change in the acetabular variables, based on the degree of obliquity and tilt (Table 2).
Table 2.
Predictive equations relating orientational variables to change in acetabular variables
| Acetabular variable | Equation |
|---|---|
| AAI | – 0.44 × obliquity (°) + 0.75 × tilt (°) = ΔAAIschial |
| AAF | – 0.42 × obliquity (°) + 0.77 × tilt (°) = ΔAAFemoral |
| AASA | 1.93 × obliquity (°) − 1.07 × tilt (°) = ΔAASA |
| PASA | 0.99 × obliquity (°) + 0.52 × tilt (°) = ΔPASA |
| HASA | 2.80 × obliquity (°) − 0.51 × tilt (°) = ΔHASA |
AAI = acetabular anteversion referenced by posterior ischia; AAF = acetabular anteversion referenced by femoral head centers; AASA = anterior acetabular sector angle; PASA = posterior acetabular sector angle; HASA = horizontal acetabular sector angle; Δ = change in.
Discussion
The anatomic position of the pelvis was defined by McKibbin as “the top of the symphysis pubis in the same vertical plane as the anterior superior spine” [36]. This is the position in which the pelvis is assumed to be for radiographic examinations, in supine and standing positions [5]. However, several studies of healthy volunteers show pelvic tilt is not constant [14, 31, 32]: the standing pelvis is tilted posteriorly (reclining, or negative tilt angle) on average between 4° and 7° compared with the supine position but with considerable variability. Eddine et al. found intersubject pelvic tilt measurements ranged 25° for standing and 26° for supine [14]. Lembeck et al., in their cohort, observed a range of supine pelvic tilt from −17° to 3°, and standing pelvic tilt ranged from −27° to 3° [32]. Patients with hip disorders similarly have a wide range of individual pelvic tilt measurements [10], ranging greater than 60° in one study [39]. We (1) asked if acetabular anteversion measurements using the femoral head centers differed from those using the posterior ischia and (2) sought to understand the effects of changing obliquity, rotation, and tilt of a pelvis in a CT scanner on the measurement of acetabular variables.
We note several limitations of this study. First, all measurements were made by only one investigator. As the CT images were made from a model without soft tissues, the landmarks were more easily identifiable. Others have found satisfactory reproducibility for acetabular measures on two-dimensional CT scans of hips, including a 95% intraobserver reproducibility within 3.5° for acetabular anteversion [27], intraobserver intraclass coefficients (ICC) ranging from 0.79 and 0.87 for measures including AASA, PASA, HASA, and acetabular anteversion [23], and mean interobserver ICC of 0.96 for measures including acetabular anteversion for normal and dysplastic hips [13]. Second, we used one pelvis model, rather than several different human pelves with a spectrum of acetabular anatomy. The pelvis model used was modeled on a real human pelvis. As our goal was to examine the effects of changing pelvic positioning on measuring acetabular variables, we report on the change in those variables, not their absolute measurements. We reasoned that pelves of differing anatomies would have similar amounts of change in their acetabular measurements owing to nonanatomic positioning, regardless of an acetabular variable’s absolute measurement. Third, the acetabulum of the pelvis model was normal, whereas most hips undergoing preoperative CT scans before an acetabular reorientational osteotomy will be dysplastic to some extent, and irregular. We assumed that if the acetabular opening was less circular, the changes in measurements of acetabular variables would be accentuated, although we did not confirm that assumption. Fourth, although superior and/or lateral femoral head subluxation is often a component of hip dysplasia, the pelvic model used had anatomically positioned femoral heads. We expect that femoral head subluxation would alter the measurement of any variable that is based on the femoral head centers (eg, the sector angles), but we would be unable to predict the added error caused by varying the pelvic orientation.
Our data indicate that using the center of the femoral heads as a baseline for the version measures yielded 1° to 4° smaller values compared with using the posterior ischial rami for the baseline. Basing AA on the posterior ischium would not be affected by femoral head subluxation, and as such may be more reproducible.
Obliquity has been cited as a potential source of measurement error [4, 52]; however, we found no verifying reports. Our data indicated that the sector angles were more sensitive to obliquity than AA was. For an average adult pelvis, 5° pelvic obliquity translates into 15- to 20-mm height difference between the iliac crest. That small amount of obliquity would change the AASA by nearly 10° and the HASA by 14°. Anda et al. found the difference between the mean AASAs for dysplastic and normal hips was 16°, and 30° for HASAs [6, 7]. Therefore, a relatively small pelvic obliquity could influence whether an acetabulum is considered to be deficient in femoral head coverage.
There are limited data addressing the influence of pelvic rotation on radiographic measurements. Visser et al. [58] noted that pelvic rotation had no influence on acetabular anteversion, but no supporting data were given. In our study, the minimal effect of pelvic rotation on AA and the sector angles was intuitive, as these measurements are performed on transverse sections of the body, the same plane as the CT slices. Therefore, as the pelvis rotates, it would be as if rotating the CT scan slice, but not changing the actual view of the pelvis.
Some authors have assessed the changes pelvic tilt causes on acetabular measurements. Zilber et al. [61] reported an increase in measured acetabular anteversion of 15° when going from simulated standing to simulated lying (20° pelvic extension). Others have reported that acetabular anteversion increases linearly with increasing pelvic tilt, between 0.5° and 0.7° for every 1° of pelvic tilt [1, 5, 32]. Our findings of a 0.75° to 0.77°-change per degree increase in tilt are in close agreement with these findings. Fewer studies have investigated the relationship between pelvic tilt and the acetabular sector angles. Anda et al. [5] noted that each 1°-increase in pelvic tilt proportionally changed AASA and PASA by 0.7° and −0.5°, respectively, similar to our findings of 1.1° and −0.5°.
For anteversion and the sector angles, the variance induced by combined pelvic obliquity and tilt remained linear, and therefore was additive, as represented by their resolution equations (Table 2). Therefore, a malorientation of 10° tilt and 5° obliquity would alter acetabular anteversion by 10°, AASA by 20°, and PASA by 10°. Tönnis and Heinecke categorized acetabular anteversion in 5°-increments, starting with Grade 1 (normal) at 15° to 20° [52]. Therefore, a 10°-increment in acetabular anteversion would change two Tönnis grades, for example, from Grade −2 (10°–14°) to Grade 2 (21°–25°), mistaking decreased acetabular anteversion as increased. Anda et al. reported that the normal range for AASA was 48° to 75° [7], therefore a 20°-change in AASA measurement could greatly affect whether anterior femoral head coverage was seen as normal.
Some authors have sought to describe the changes in measured acetabular variables, especially anteversion, with changes in pelvic positioning. Our data suggest small (eg, 5°–10°) changes in pelvic orientation were related to statistically significant changes in the measurements used to plan correction of hip dysplasia, but we believe it is important for a surgeon to have the most precise data available for planning a procedure, and know where error can occur in collecting the data. The need for standardized positioning of patients’ pelves when obtaining CT scans for evaluating acetabular shape and orientation is well known [19, 31, 32, 58], but factors such as posture and body habitus are confounding variables [31]. Techniques suggested to standardize positioning include an inclinometer applied to the patient’s pelvis [5], and using an ultrasound to evaluate the thickness of soft tissues overlying bony landmarks [32]. More exacting techniques are a shoot-through lateral radiograph of the pelvis on the CT scanner bed [14], or obtaining a three-dimensional CT scan so that the reconstructed pelvis can be reoriented anatomically before making measurements [1, 19]. It is possible that inconsistencies in pelvic orientation explain the conflicting findings between studies that associate hip dysplasia with increased acetabular anteversion [7, 12, 22, 29, 42], retroversion [15, 27, 43, 46], or no difference in acetabular orientation [26].
The assumption that most people walk with their pelvis oriented in the anatomic plane may have important consequences. Some authors have noted that pelvic tilt varies substantially between standing and lying down, and there is considerable intersubject variability in pelvic orientation in standing and supine positions [14, 32, 61]. Also, patients with hip pain and/or early osteoarthritis stand with increased pelvic tilt [30]. An important concept to be further elucidated is whether orientation of an acetabular fragment or prosthetic cup should be based on the true anatomic position of the pelvis, or the natural position of the patient in stance.
Acknowledgment
We thank Zehava Rosenberg MD, Department of Radiology, NYU-Hospital for Joint Diseases, for assistance operating the CT scanner.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
This study was conducted at NYU Hospital for Joint Diseases, New York, NY.
References
- 1.Abel MF, Sutherland DH, Wenger DR, Mubarak SJ. Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip. J Pediatr Orthop. 1994;14:48–53. doi: 10.1097/01241398-199401000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip: implications for secondary procedures. J Bone Joint Surg Br. 2004;86:876–886. doi: 10.1302/0301-620X.86B6.14441. [DOI] [PubMed] [Google Scholar]
- 3.Aminian A, Mahar A, Yassir W, Newton P, Wenger D. Freedom of acetabular rotation following three surgical techniques for correction of congenital deformities of the hip. J Pediatr Orthop. 2005;25:10–13. doi: 10.1097/00004694-200501000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Anda S, Svenningsen S, Dale LG, Benum P. The acetabular sector angle of the adult hip determined by computed tomography. Acta Radiol Diagn (Stockh) 1986;27:443–447. doi: 10.1177/028418518602700415. [DOI] [PubMed] [Google Scholar]
- 5.Anda S, Svenningsen S, Grontvedt T, Benum P. Pelvic inclination and spatial orientation of the acetabulum: a radiographic, computed tomographic and clinical investigation. Acta Radiol. 1990;31:389–394. [PubMed] [Google Scholar]
- 6.Anda S, Terjesen T, Kvistad KA. Computed tomography measurements of the acetabulum in adult dysplastic hips: which level is appropriate? Skeletal Radiol. 1991;20:267–271. doi: 10.1007/BF02341662. [DOI] [PubMed] [Google Scholar]
- 7.Anda S, Terjesen T, Kvistad K, Svenningsen S. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comp Assist Tomogr. 1991;15:115–120. doi: 10.1097/00004728-199101000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Armand M, Lepisto J, Tallroth K, Elias J, Chao E. Outcome of periacetabular osteotomy: joint contact pressure calculation using standing AP radiographs, 12 patients followed for average 2 years. Acta Orthop. 2005;76:303–313. [PMC free article] [PubMed] [Google Scholar]
- 9.Azuma H, Taneda H, Igarashi H, Fujioka M. Preoperative and postoperative assessment of rotational acetabular osteotomy for dysplastic hips in children by three-dimensional surface reconstruction computed tomography imaging. J Pediatr Orthop. 1990;10:33–38. [PubMed] [Google Scholar]
- 10.Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008;90:357–365. doi: 10.2106/JBJS.F.00628. [DOI] [PubMed] [Google Scholar]
- 11.Banks KP, Grayson DE. Acetabular retroversion as a rare cause of chronic hip pain: recognition of the “figure-eight” sign. Skeletal Radiol. 2007;36(suppl 1):S108–111. doi: 10.1007/s00256-006-0150-0. [DOI] [PubMed] [Google Scholar]
- 12.Browning WH, Rosenkrantz H, Tarquinio T. Computed tomography in congenital hip dislocation: the role of acetabular anteversion. J Bone Joint Surg Am. 1982;64:27–31. [PubMed] [Google Scholar]
- 13.Dandachli W, Kannan V, Richards R, Shah Z, Hall-Craggs M, Witt J. Analysis of cover of the femoral head in normal and dysplastic hips: new CT-based technique. J Bone Joint Surg Br. 2008;90:1428–1434. doi: 10.1302/0301-620X.90B11.20073. [DOI] [PubMed] [Google Scholar]
- 14.Eddine TA, Migaud H, Chantelot C, Cotten A, Fontaine C, Duquennoy A. Variations of pelvic anteversion in the lying and standing positions: analysis of 24 control subjects and implications for CT measurement of position of a prosthetic cup. Surg Radiol Anat. 2001;23:105–110. doi: 10.1007/s00276-001-0105-z. [DOI] [PubMed] [Google Scholar]
- 15.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372–379. doi: 10.2106/JBJS.D.02385. [DOI] [PubMed] [Google Scholar]
- 16.Frick SL, Kim SS, Wenger DR. Pre- and postoperative three-dimensional computed tomography analysis of triple innominate osteotomy for hip dysplasia. J Pediatr Orthop. 2000;20:116–123. doi: 10.1097/00004694-200001000-00023. [DOI] [PubMed] [Google Scholar]
- 17.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 18.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garbuz DS, Masri BA, Haddad F, Duncan CP. Clinical and radiographic assessment of the young adult with symptomatic hip dysplasia. Clin Orthop Relat Res. 2004;418:18–22. doi: 10.1097/00003086-200401000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Hasegawa Y, Masui T, Yamaguchi J, Kawabe K, Suzuki S. Factors leading to osteoarthritis after eccentric rotational acetabular osteotomy. Clin Orthop Relat Res. 2007;459:207–215. doi: 10.1097/BLO.0b013e31803df968. [DOI] [PubMed] [Google Scholar]
- 21.Hipp JA, Sugano N, Millis MB, Murphy SB. Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res. 1999;364:134–143. doi: 10.1097/00003086-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Jacobsen S, Rømer L, Søballe K. Degeneration in dysplastic hips: a computer tomography study. Skeletal Radiol. 2005;34:778–784. doi: 10.1007/s00256-005-0019-7. [DOI] [PubMed] [Google Scholar]
- 23.Jacobsen S, Romer L, Soballe K. The other hip in unilateral hip dysplasia. Clin Orthop Relat Res. 2006;446:239–246. doi: 10.1097/01.blo.0000201151.91206.50. [DOI] [PubMed] [Google Scholar]
- 24.Jacobsen S, Sonne-Holm S, Lund B, Søballe K, Kiær T, Rovsing H, Monrad H. Pelvic orientation and assessment of hip dysplasia in adults. Acta Orthop Scand. 2004;75:721–729. doi: 10.1080/00016470410004094. [DOI] [PubMed] [Google Scholar]
- 25.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 26.Kim SS, Frick SL, Wenger DR. Anteversion of the acetabulum in developmental dysplasia of the hip: analysis with computed tomography. J Pediatr Orthop. 1999;19:438–442. doi: 10.1097/00004694-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Kim WY, Hutchinson CE, Andrew JG, Allen PD. The relationship between acetabular retroversion and osteoarthritis of the hip. J Bone Joint Surg Br. 2006;88:727–729. doi: 10.2106/JBJS.E.00550. [DOI] [PubMed] [Google Scholar]
- 28.Kiyama T, Naito M, Shiramizu K, Shinoda T. Postoperative acetabular retroversion causes posterior osteoarthritis of the hip. Int Orthop. 2009;33:625–631. doi: 10.1007/s00264-007-0507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klaue K, Wallin A, Ganz R. CT evaluation of coverage and congruency of the hip prior to osteotomy. Clin Orthop Relat Res. 1988;232:15–25. [PubMed] [Google Scholar]
- 30.Kojima A, Nakagawa T, Tohkura A. Simulation of acetabular coverage of femoral head using anteroposterior pelvic radiographs. Arch Orthop Trauma Surg. 1998;117:330–336. doi: 10.1007/s004020050260. [DOI] [PubMed] [Google Scholar]
- 31.Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph: a new computerized technique. J Bone Joint Surg Am. 1993;75:1318–1333. doi: 10.2106/00004623-199309000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 33.Mandel DM, Loder RT, Hensinger RN. The predictive value of computed tomography in the treatment of developmental dysplasia of the hip. J Pediatr Orthop. 1998;18:794–798. doi: 10.1097/00004694-199811000-00018. [DOI] [PubMed] [Google Scholar]
- 34.Mast JW, Brunner RL, Zebrack J. Recognizing acetabular version in the radiographic presentation of hip dysplasia. Clin Orthop Relat Res. 2004;418:48–53. doi: 10.1097/00003086-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 36.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–159. [PubMed] [Google Scholar]
- 37.Mechlenburg I, Nyengaard JR, Romer L, Soballe K. Changes in load-bearing area after Ganz periacetabular osteotomy evaluated by multislice CT scanning and stereology. Acta Orthop Scand. 2004;75:147–153. doi: 10.1080/00016470412331294395. [DOI] [PubMed] [Google Scholar]
- 38.Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984;66:430–436. [PubMed] [Google Scholar]
- 39.Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop Relat Res. 2003;411:140–151. doi: 10.1097/01.blo.0000069891.31220.fd. [DOI] [PubMed] [Google Scholar]
- 40.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926. doi: 10.2106/JBJS.E.00515. [DOI] [PubMed] [Google Scholar]
- 41.Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum in patients with idiopathic increased anteversion of the femoral neck. Acta Orthop Scand. 1982;53:847–852. doi: 10.3109/17453678208992837. [DOI] [PubMed] [Google Scholar]
- 42.Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop Scand. 1983;54:18–23. doi: 10.3109/17453678308992864. [DOI] [PubMed] [Google Scholar]
- 43.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 44.Salter RB, Dubos JP. The first fifteen year’s personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res. 1974;98:72–103. doi: 10.1097/00003086-197401000-00009. [DOI] [PubMed] [Google Scholar]
- 45.Siebenrock KA, Kalbermatten D, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 46.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 47.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 49.Terjesen T, Benum P, Anda S, Svenningsen S. Increased femoral anteversion and osteoarthritis of the hip joint. Acta Orthop Scand. 1982;53:571–575. doi: 10.3109/17453678208992260. [DOI] [PubMed] [Google Scholar]
- 50.Thawrani D, Sucato DJ, Podeszwa DA, DeLaRocha A. Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents. J Bone Joint Surg Am. 2010;92:1707–1714. doi: 10.2106/JBJS.I.00829. [DOI] [PubMed] [Google Scholar]
- 51.Tonnis D, Behrens K, Tscharani F. A modified technique of the triple pelvic osteotomy: early results. J Pediatr Orthop. 1981;1:241–249. doi: 10.1097/01241398-198111000-00001. [DOI] [PubMed] [Google Scholar]
- 52.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 53.Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 54.Trousdale RT, Cabanela ME. Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop Scand. 2003;74:119–126. doi: 10.1080/00016470310013824. [DOI] [PubMed] [Google Scholar]
- 55.Tsumura H, Kaku N, Ikeda S, Torisu T. A computer simulation of rotational acetabular osteotomy for dysplastic hip joint: does the optimal transposition of the acetabular fragment exist? J Orthop Sci. 2005;10:145–151. doi: 10.1007/s00776-004-0866-4. [DOI] [PubMed] [Google Scholar]
- 56.Turgeon TR, Phillips W, Kantor SR, Santore RF. The role of acetabular and femoral osteotomies in reconstructive surgery of the hip: 2005 and beyond. Clin Orthop Relat Res. 2005;441:188–199. doi: 10.1097/01.blo.0000193541.72443.73. [DOI] [PubMed] [Google Scholar]
- 57.Visser JD, Jonkers A. A method for calculating acetabular anteversion, femur anteversion and the instability index of the hip joint. Neth J Surg. 1980;32:146–149. [PubMed] [Google Scholar]
- 58.Visser JD, Jonkers A, Hillen B. Hip joint measurements with computerized tomography. J Pediatr Orthop. 1982;2:143–146. doi: 10.1097/01241398-198202020-00005. [DOI] [PubMed] [Google Scholar]
- 59.Weiner LS, Kelley MA, Ulin RI, Wallach D. Development of the acetabulum and hip: computed tomography analysis of the axial plane. J Pediatr Orthop. 1993;13:421–425. doi: 10.1097/01241398-199307000-00001. [DOI] [PubMed] [Google Scholar]
- 60.Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am. 2006;88:1915–1919. doi: 10.2106/JBJS.E.00715. [DOI] [PubMed] [Google Scholar]
- 61.Zilber S, Lazennec JY, Gorin M, Saillant G. Variations of caudal, central, and cranial acetabular anteversion according to the tilt of the pelvis. Surg Radiol Anat. 2004;26:462–465. doi: 10.1007/s00276-004-0254-y. [DOI] [PubMed] [Google Scholar]