Abstract
Study Design
This was a prospective cross-sectional study for people with chronic SCI.
Objectives
To (1) evaluate the intensity level and nature of physical activity in community-dwelling individuals living with SCI, and (2) explore the relation between descriptive individual variables (e.g. lesion level), secondary complications, and participation in physical activity.
Setting
Urban community setting
Methods
Forty-nine subjects with SCI who used a manual wheelchair for primary mode of mobility (mean years since injury, 11.8; mean age, 43.7 years; 67% paraplegia) completed the physical activity recall assessment for people with spinal cord injury (PARA-SCI).
Results
Approximately 50% of reported physical activity among individuals with SCI is due to activities of daily living. The amount of physical activity was not related to lesion level, age, BMI, or waistline size. Greater heavy intensity activity was related to lower levels of pain and fatigue and higher levels of self efficacy while higher amounts of mild intensity activity and total activity were related to less depressive symptoms.
Conclusions
Activities of daily living are a large component for physical activity among individuals with SCI. It appears that greater physical activity is associated with less secondary complications (pain, fatigue and depression) in individuals with SCI.
Keywords: spinal cord injury, exercise, physical activity, participation, quality of life
INTRODUCTION
Physical activity has the potential to promote health and enhance quality of life. However, despite the known benefits of physical activity, large proportions of the population are physically inactive to the point that it impacts negatively on health1. This is true to an even greater extent for people with spinal cord injury (SCI)2, 3.
Although physical activity has the potential to reduce the risk of chronic disease after SCI (i.e. heart disease, diabetes 4), the relationship between physical activity and secondary complications has not been established. For example, it is not known whether exercise (e.g. wheeling, sports) can reduce pain or depression, or whether activities such as gardening or household chores could have emotional and physical health enhancing benefits5. Further, little is currently known about which factors can predict the likelihood of someone with SCI performing physical activities. While determinants of physical activity among the general population are relatively weak, they are virtually unknown in the SCI population. Though basic mobility function was found to predict physical activity participation in ambulatory individuals with chronic conditions6, no link between injury severity and physical activity participation has been reported within the SCI population. Conditions such as pain7, fatigue8, and depression9 have been linked to physical inactivity in both the general population and adults with chronic conditions. However, despite the fact that these conditions are commonly reported after SCI10, their relation to physical inactivity has not yet been explored. In addition, though social support6 and self-efficacy11 have been shown to influence leisure-time physical activity participation in able-bodied individuals, their role within the SCI population is unclear. Social support12 and self-efficacy13 may be altered following SCI. Given their influence on physical activity participation in the able-bodied population, it would be pertinent to determine the effect of these factors on physical activity participation in individuals with SCI.
Currently, information regarding the type and level of physical activity necessary for positive health outcomes in individuals with SCI is limited. Further, determinants for physical activity among individuals with SCI are relatively unknown. Yet, this information is necessary for developing physical activity guidelines for this population. Therefore, the primary objectives of this cross-sectional study were to (1) evaluate the level and nature of physical activity, (2) determine what demographic factors (e.g. sex, age, injury severity) and secondary complications (pain, fatigue, and depression) best relate to participation in physical activity, and (3) quantify the roles of social support and self efficacy in physical activity participation among community-dwelling individuals living with SCI.
METHODS
The study was a prospective cross-sectional design. The inclusion criteria for participation were: (1) adults (19 years or older) living in the community; (2) minimum of 1 year since SCI; and (3) use a manual wheelchair for primary mode of mobility. We selected community dwelling individuals with SCI (rather than those in residential care facilities) who primarily used manual wheel-chairs (rather than power chairs) as this group of individuals would likely have similar opportunities for physical activity. Participants were recruited on a volunteer basis in Taipei, Taiwan. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Participants completed evaluations through standardized assessments and face-to-face interviews led by trained assessors. The study cohort was described with the following demographic information: date of birth, sex, body weight/height, waistline circumference, ASIA motor score, lesion level, and date of injury. Physical activity was quantified with the physical activity recall assessment for people with spinal cord injury (PARA-SCI). Three potential secondary complications following SCI (fatigue, pain, and depression), social support and self efficacy were assessed.
The primary variable of interest was amount of physical activity. Until recently, no valid and reliable self-report measure of physical activity for people with SCI existed. Self-report physical activity measures developed for the general population are not applicable for the vast majority of individuals with SCI, most of whom use a wheelchair for mobility14 and expend substantial energy through activities of daily living (ADLs)15. Thus, the PARA-SCI was developed 5, 16. Briefly, this assessment is administered via a semi-structured interview, providing an estimate of time (in minutes) spent participating in mild, moderate, and heavy intensity physical activity (Table 1). The PARA-SCI captures three categories of physical activity: leisure time physical activity (activity that one chooses to do during their free time1); lifestyle activity (activities that are part of one’s daily routine: personal hygiene, household chores, work-related activity3); and cumulative activity (the combination of leisure time physical activity and lifestyle activity)5. For the purpose of our study, we further captured two components of lifestyle activity: (1) ADLs (self-maintenance tasks, such as bathing, dressing, necessary for meeting the demands of daily living17); and (2) household chores (i.e. all other household tasks not classified as ADLs). The PARA-SCI is a valid measure of physical activity for individuals with SCI who use a wheelchair as their primary mode of mobility16. Convergent validity of the leisure time physical activity category has shown that individuals reporting more minutes of moderate and heavy intensity leisure time physical activity show better physical fitness (measured by VO2 peak) than those who report fewer minutes of such activities16. Thus, this instrument captures low level activities (which individuals with a high degree of impairment find physically demanding) that may be overlooked on other scales.
Table 1.
PARA-SCI Classification System. Modified from Martin-Ginis et al. (2005)5
| Nothing at all | Mild | Moderate | Heavy | |
|---|---|---|---|---|
| How hard are you working? | Includes activities that even when you are doing them, you do not feel like you are working at all. | Includes physical activities that require you to do very light work. You should feel like you are working a little bit but overall you shouldn’t find yourself working too hard. | Includes physical activities that require some physical effort. You should feel like you are working somewhat hard but can maintain the effort for a long time. | Includes physical activities that require a lot of physical effort. You should feel like you are working really hard (almost at your maximum) and can only do the activity for a short time before getting tired. These activities can be exhausting. |
| How does your body feel? | ||||
| Breathing & heart rate | Normal | Stays normal or is only a little bit harder and/or faster than normal. | Noticeable harder and faster than normal but not extremely hard or fast. | Fairly hard and much faster than normal. |
| Muscles | Normal | Feel loose, warmed up, and relaxed. Feel normal temperature or a little bit warmer and not tired at all. | Feel pumped and worked. Feel warmer than normal and starting to get tired after a while. | Burn and feel tight and tense. Feel a lot warmer than normal and feel tired. |
| Skin | Normal | Normal temperature is only a little bit warmer and not sweaty. | A little bit warmer than normal and might be a little sweaty. | Much warmer than normal and might be sweaty. |
| Mind | Normal | You might feel very alert. Has no effect on concentration. | Requires some concentration to complete. | Requires a lot of concentration (almost full) to complete. |
Fatigue, pain and depression were assessed as these are secondary complications which may affect participation in physical activity7–9. The Fatigue Severity Scale (FSS) was used to quantify the effect of fatigue on daily living an is reliable and valid in people with neurological disorders18, 19. The 3-item Graded Chronic Pain (GCP) questionnaire20 was used to assess pain and is reliable and valid in people with SCI21,. Respondents rate pain’s interference with (1) daily activities, (2) ability to participate in recreational, social, and family activities, and (3) ability to work (including housework). Depression was measured using the 10 item Centre for Epidemiological Studies–Depression scale (CESD-10)22. The CES-D has been shown to be reliable and valid within the SCI population10.
Social support was assessed using the Instrumental Support Evaluation List (ISEL) which measures perceived availability of social resources23. Higher scores indicate better availability of support. Self-efficacy was assessed via the Stanford Self-efficacy for Managing Chronic Disease scale (ESE), six questions which assess participants’ confidence in coping with the impact of living with a chronic disease24. This scale has been successfully used for individuals with various chronic conditions, including lung and/or heart disease, diabetes, and arthritis25.
Descriptive characteristics of the cohort were quantified using means, standard deviations, and frequencies. Scatterplots were generated to ensure there were no outliers or leverage of influential data points. Spearman correlation coefficients were calculated to determine the strength of the associations between continuous variables because the physical activity variables were not normally distributed (Kolmogorov - Smirnov test). With regards to the PARA-SCI, correlations were computed for cumulative activity and for each intensity level. The influence of categorical variables of sex (male/female) and lesion level (tetraplegic, paraplegic) on physical activity (three intensity levels) was assessed by chi-square. All statistical analyses were performed using SPSS v. 13 software (SPSS Inc., Chicago, IL) using a significant level of P≤ 0.05 (two-tailed).
RESULTS
Forty-nine people were assessed. Subject characteristics are reported in Table 2. Measures of pain, depression, fatigue, social support, and self-efficacy are presented in Table 3.
Table 2.
Demographic information and PARA-SCI results, (reported in minutes) are presented for “All subjects” (top row) (ie., included even if they reported 0 minutes of activity in that intensity category) and for “Subgroups” who reported participating in each intensity level of activity (i.e. those participants who recorded > 0 minutes of activity in that intensity category). This table highlights that participant demographics are similar across all exercise intensity levels.
| Para-SCI activity | Demographic information | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Intensity Level | N | Minutes | Age (years) | Duration of Injury (years) | % Paraplegia | % Complete Injuries | ASIA Motor Score | Body Mass Index (kg/m2) | Waist Circumference (cm) | |
| All subjects | Mild | 49 | 135.8 (177.9) | 43.7 (11.7) | 11.8 (9.2) | 67% | 61% | 50.65 (14.9) | 24.0 (5.0) | 89.3 (13.6) |
| Moderate | 49 | 81.5 (149.4) | ||||||||
| Heavy | 49 | 16.5 (30.0) | ||||||||
|
| ||||||||||
| Subgroups | Mild | 47 | 135.8 (177.9) | 43.4 (11.7) | 11.6 (9.0) | 70% | 60% | 51.62 (14.4) | 24.1 (5.1) | 89.5 (13.7) |
| Moderate | 33 | 108.0 (119.3) | 42.7 (12.1) | 10.9 (8.2) | 70% | 67% | 49.42 (15.4) | 24.2 (4.6) | 88.6 (14.1) | |
| Heavy | 15 | 53.7 (34.1) | 47.2 (10.5) | 12.7 (9.1) | 60% | 53% | 51.47 (16.4) | 23.6 (4.8) | 85.6 (13.9) | |
Mean values are reported with standard deviations in brackets.
Table 3.
Measures of secondary complications (FSS, GCP, CESD-10), social support (ISEL) and self-efficacy (ESE). Mean scores are presented with standard deviations in brackets.
| Measure | Score | Range |
|---|---|---|
|
| ||
| Instrumental Support Evaluation List (ISEL) (Max. = 48) | 29.1 (8.3) | 7.0 – 45.0 |
| Stanford Self-efficacy for Managing Chronic Disease Scale (ESE) (Max. = 10) | 6.5 (1.6) | 2.0 – 10.0 |
| Fatigue Severity Scale (FSS) (Max. = 7.0) | 4.1 (1.2) | 1.4 – 6.6 |
| Graded Chronic Pain questionnaire (GCP) (Max. = 10) | 3.7 (2.8) | 0.0 – 9.33 |
| Centre for Epidemiological Studies-Depression Scale (CESD-10) (Max. = 30) | 11.0 (6.8) | 1.0 – 27.0 |
Higher scores for FFS, GCP and CESD-10 indicate greater impairment.
Higher scores for ISEL and ESE indicate better scores.
Forty-seven subjects reported participating in mild intensity activity, while 33 and 16 subjects reported participating in moderate and heavy intensity activity respectively (Table 2). Approximately 50% of all heavy and moderate intensity physical activity included lifestyle tasks (Table 4). Specifically, ADLs made up 96% of the time spent doing heavy or moderate intensity lifestyle tasks.
Table 4.
Average percentage of the total time doing each of heavy and moderate intensity physical activity. For example, on average, exercise makes up 19% of total heavy intensity physical activity.
| Type of physical activity | Heavy Intensity (n=15) | Moderate Intensity (n=33) |
|---|---|---|
| Lifestyle activity | 59% | 49% |
| ADLs | 59% | 45% |
| Chores | 0% | 4% |
|
| ||
| Leisure time physical activity | 41% | 51% |
| Exercise | 19% | 37% |
| Other | 22% | 14% |
One participant was noted to be an outlier in correlations with heavy intensity physical activity with values greater than two standard deviations from the mean. Subsequent calculations confirmed the subject’s data points to have unacceptable leverage (leverage score: 0.27)26, supporting the removal of this subject from correlations with heavy intensity.
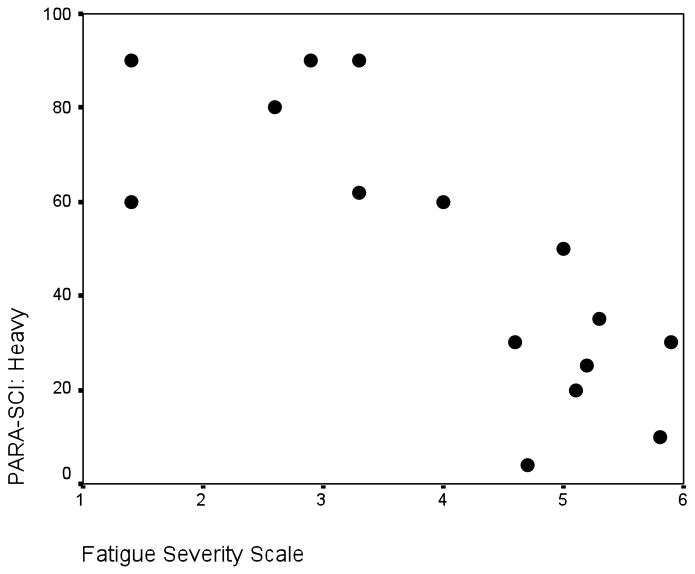
No significant correlations were found between physical activity and any demographic factors. Chi-square tests did not reveal any influence of sex or lesion on physical activity participation. However, physical activity was significantly related to secondary complications (Table 5). Specifically, high amounts of heavy intensity physical activity corresponded with: (1) lower levels of fatigue; (2) higher levels of self-efficacy; and (3) lower levels of pain. As an example, the scatter-plot of heavy physical activity versus fatigue is highlighted in Figure 1. Higher amounts of mild intensity physical activity correlated with: (1) lower levels of pain; (2) higher levels of social support; and (3) lower levels of depression, while moderate physical activity did not correlate with any factors. Lastly, more total physical activity was related to higher self-efficacy and less depression.
Table 5.
Heavy and mild intensity physical activities are related to secondary complications and personal factors. Correlations are noted as p<0.05*, and p<0.01**.
| Fatigue Severity Scale | Self-Efficacy | GCP | ISEL | CES-D | ||
|---|---|---|---|---|---|---|
| PARA-SCI: Heavy (n = 15) | Pearson Correlation | −.767 | .656 | −.612 | .478 | −.270 |
| Sig. (2-tailed) | .001** | .008** | .015* | .072 | .331 | |
|
| ||||||
| PARA-SCI: Moderate (n = 33) | Pearson Correlation | −.164 | .295 | −.132 | −.099 | −.100 |
| Sig. (2-tailed) | .361 | .095 | .464 | .582 | .580 | |
|
| ||||||
| PARA-SCI: Mild (n = 47) | Pearson Correlation | −.001 | .253 | −.294 | .312 | −.565 |
| Sig. (2-tailed) | .994 | .086 | .045* | .033* | .0001** | |
|
| ||||||
| PARA-SCI: Total (n = 49) | Pearson Correlation | −.103 | .288 | −.266 | .185 | −.318 |
| Sig. (2-tailed) | .481 | .045* | .064 | .203 | .026* | |
Figure 1.
Scatterplot highlighting heavy physical activity (PARA-SCI) vs fatigue (Fatigue Severity Scale) for 15 participants with SCI (r = −0.767; p<0.001).
The removal of one participant from correlations with heavy intensity physical activity participation had minimal effects on the pain and fatigue analysis (both remained significant at p< 0.01 and p< 0.001, respectively). However, removing the high leverage data point for the correlation between self efficacy and heavy intensity physical activity caused the correlation co-efficient to increase from 0.437 (p= 0.091) to 0.656 (p=0.008).
DISCUSSION
This study provides an evaluation of the level and nature of physical activity among a cohort of individuals with SCI. Secondly, we provide novel data highlighting the relationships between physical activity participation and secondary complications in this group.
Demographic variables were consistent with the general SCI population27. Mean scores on the FSS and CESD-10 suggest that our participants were experiencing mild fatigue18 and mild depression28, while scores on the 3-item GCP and ESE reflected fairly low levels of pain-related disability20 and relatively high levels of perceived disease-management self-efficacy25.
Physical activity participation in this cohort was similar to earlier investigations using the PARA-SCI 5, 29. Most of our participants stated doing some mild physical activity, yet less than two thirds reported moderate levels of exertion and only a third reported heavy levels of exertion. Similarly high levels of inactivity, as measured by heart rate monitors over a 3-day period, was previously documented in a group of individuals with paraplegia3. In our study, ADL tasks were responsible for approximately 50% of time spent doing moderate and heavy intensity activities, supporting the pre-existing notion that lifestyle activity can be particularly taxing for individuals with SCI 15.
Surprisingly, demographic factors such as age, injury duration, or lesion level (paraplegic/tetraplegic), were not related to physical activity participation in this study. Although Dearwater et al. (1985) suggested that people with paraplegia were more active than those with tetraplegia, their data came from a diverse sample from an inpatient rehabilitation setting2. Our sample included only adult manual wheelchairs users living in the community, where secondary complications and environmental factors would likely influence physical activity participation.
Reduced secondary complications were related to the amount of physical activity. Our finding that greater participation in mild intensity activity relates to decreased secondary complications supports evidence that very sedentary people may derive health benefits from low intensities of activity.
Our results showed that heavy intensity activity was strongly correlated with measures of fatigue, pain, and self-efficacy. As our results are correlational, no causality can be inferred. It is possible that lower levels of secondary complications such as fatigue and pain allow one to participate more effectively in heavy intensity physical activity. Alternatively, the engagement in physical activity may prevent or reduce the occurrence of secondary complications.
The relationship between self-efficacy and physical activity may be more complex. People who have higher beliefs in their abilities to perform exercise are more likely to participate in intense leisure time physical activity11, 30. Likewise, those with higher beliefs in their abilities to perform lifestyle activities may be more likely to accomplish ADLs as independently as possible, thereby rating these tasks as high intensity. Conversely, the ability to exercise and perform lifestyle activities may positively influence one’s self-efficacy in managing his/her condition. Removing one outlying participant strengthened the correlation between heavy intensity activity participation and self-efficacy, suggesting this participant did not experience a similar relationship between these entities.
The positive correlation between social support and physical activity found in this study supports that of previous research in other populations. Social support was positively related to 7-days of accelerometer measurement in individuals with Multiple Sclerosis31. Using the social cognitive theory, these authors proposed that social support was associated with physical activity due to an intermediary relationship with self-efficacy (i.e. social support correlated with physical activity because both serve as a source of efficacy information). This theory may have merit for our group as post-hoc analyses showed strong positive correlations between social support and self-efficacy.
LIMITATIONS
This was a cross-sectional observational investigation; therefore we cannot interpret any causality from the results. A multiple regression analysis was not performed to predict physical activity because although heavy activity was related to several variables, only a small number of subjects (n=16) reported participating in heavy activity. Further, because of our small sample size, one outlier was overly influential on our results and was removed from correlations involving heavy intensity physical activity. Lastly, by using a p-value of 0.05, our study (which involved 20 correlations) would have a chance that, at a maximum, one correlation may be significant by chance alone.
CONCLUSIONS
Although there are a number of potential barriers to participating in physical activity, some people with SCI do adopt a physically active lifestyle. Demographic factors measured in this study (sex, age, time since injury, and lesion level) were not determinants of physical activity. Rather, this data highlights that secondary complications (pain, fatigue) are barriers, while self efficacy is a facilitator, to physical activity participation. Further, performance of activities which were not necessarily physically taxing were related to decreased secondary complications. Ultimately, this study reinforces that physical activity is a complex issue for individuals with SCI. Further research needs to be conducted in order to better understand the predictors of physical activity participation for this population.
Acknowledgments
We would like to thank Dr. Yen-Ho Wang, Mrs. Yueh-Er Lee, and Ms. Zu-Si Lei for subject recruitment; Ms. Ron-Jyuan Liing, Ms. Yin-Chen Chen, and Mr. Li-Hsueh Chen for data collection; the National Science Council (#NSC 96-2811-B-002-001, Taiwan) and the International Collaboration on Repair Discovery for visiting professor awards (to JJE); and the Canadian Institutes for Health Research (#MSH-63617) and the Michael Smith Foundation for Health Research for career scientist awards (to JJE).
References
- 1.Bouchard C, Blair SN, Haskell WL. Physical activity and health. Champaign, IL: 2007. [Google Scholar]
- 2.Dearwater SR, LaPorte RE, Cauley JA, Brenes G. Assessment of physical activity in inactive populations. Med Sci Sports Exerc. 1985;17:651–655. doi: 10.1249/00005768-198512000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Buchholz AC, McGillivray CF, Pencharz PB. Physical activity levels are low in free-living adults with chronic paraplegia. Obes Res. 2003;11:563–570. doi: 10.1038/oby.2003.79. [DOI] [PubMed] [Google Scholar]
- 4.Johnson EP. American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 5.Ginis KA, Latimer AE, Hicks AL, Craven BC. Development and evaluation of an activity measure for people with spinal cord injury. Med Sci Sports Exerc. 2005;37:1099–1111. doi: 10.1249/01.mss.0000170127.54394.eb. [DOI] [PubMed] [Google Scholar]
- 6.Ashe MC, Eng JJ, Miller WC, Soon JA. Disparity between physical capacity and participation in seniors with chronic disease. Med Sci Sports Exerc. 2007;39:1139–1146. doi: 10.1249/mss.0b013e31804d2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosemann T, Kuehlein T, Laux G, Szecsenyi J. Osteoarthritis of the knee and hip: a comparison of factors associated with physical activity. Clin Rheumatol. 2007;26:1811–1817. doi: 10.1007/s10067-007-0579-0. [DOI] [PubMed] [Google Scholar]
- 8.Rosqvist E, et al. Factors affecting the increased risk of physical inactivity among older people with depressive symptoms. Scand J Med Sci Sports. 2008 doi: 10.1111/j.1600-0838.2008.00798.x. [DOI] [PubMed] [Google Scholar]
- 9.Galper DI, Trivedi MH, Barlow CE, Dunn AL, Kampert JB. Inverse association between physical inactivity and mental health in men and women. Med Sci Sports Exerc. 2006;38:173–178. doi: 10.1249/01.mss.0000180883.32116.28. [DOI] [PubMed] [Google Scholar]
- 10.Miller WC, Anton HA, Townson AF. Measurement properties of the CESD scale among individuals with spinal cord injury. Spinal Cord. 2008;46:287–292. doi: 10.1038/sj.sc.3102127. [DOI] [PubMed] [Google Scholar]
- 11.Cerin E, Vandelanotte C, Leslie E, Merom D. Recreational facilities and leisure-time physical activity: An analysis of moderators and self-efficacy as a mediator. Health Psychol. 2008;27:S126–35. doi: 10.1037/0278-6133.27.2(Suppl.).S126. [DOI] [PubMed] [Google Scholar]
- 12.Hammell KR. Psychosocial outcome following spinal cord injury. Paraplegia. 1994;32:771–779. doi: 10.1038/sc.1994.123. [DOI] [PubMed] [Google Scholar]
- 13.Middleton J, Tran Y, Craig A. Relationship between quality of life and self-efficacy in persons with spinal cord injuries. Arch Phys Med Rehabil. 2007;88:1643–1648. doi: 10.1016/j.apmr.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 14.http://canparaplegic.org.
- 15.Janssen TW, van Oers CA, van der Woude LH, Hollander AP. Physical strain in daily life of wheelchair users with spinal cord injuries. Med Sci Sports Exerc. 1994;26:661–670. doi: 10.1249/00005768-199406000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Latimer AE, Ginis KAM, Craven BC, Norman GR, Hicks AL. The Physical Activity Recall Assessment for Individuals with SCI: Preliminary Reliability and Validity Data. Medicine & Science in Sports & Exercise. 2004;36:S110. [Google Scholar]
- 17.Crepeau EB, Cohn ES, Schell BAB. Willard & Spackman’s occupational therapy. Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 18.Herlofson K, Larsen JP. Measuring fatigue in patients with Parkinson’s disease - the Fatigue Severity Scale. Eur J Neurol. 2002;9:595–600. doi: 10.1046/j.1468-1331.2002.00444.x. [DOI] [PubMed] [Google Scholar]
- 19.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 20.Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50:133–149. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 21.Raichle KA, Osborne TL, Jensen MP, Cardenas D. The reliability and validity of pain interference measures in persons with spinal cord injury. J Pain. 2006;7:179–186. doi: 10.1016/j.jpain.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 23.Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. Social support: Theory, research, and applications. 1985;73:94. [Google Scholar]
- 24.Lorig K. Outcome Measures for Health Education and Other Health Care Interventions. Sage Publications Inc; 1996. [Google Scholar]
- 25.Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4:256–262. [PubMed] [Google Scholar]
- 26.Pallant J, Pallant JF. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using SPSS. Allen & Unwin; 2007. [Google Scholar]
- 27.Ackery A, Tator C, Krassioukov A. A global perspective on spinal cord injury epidemiology. J Neurotrauma. 2004;21:1355–1370. doi: 10.1089/neu.2004.21.1355. [DOI] [PubMed] [Google Scholar]
- 28.Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. 1999;14:608–617. doi: 10.1002/(sici)1099-1166(199908)14:8<608::aid-gps991>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 29.Latimer AE, Ginis KA, Craven BC, Hicks AL. The physical activity recall assessment for people with spinal cord injury: validity. Med Sci Sports Exerc. 2006;38:208–216. doi: 10.1249/01.mss.0000183851.94261.d2. [DOI] [PubMed] [Google Scholar]
- 30.Kamphuis CB, et al. Socioeconomic status, environmental and individual factors, and sports participation. Med Sci Sports Exerc. 2008;40:71–81. doi: 10.1249/mss.0b013e318158e467. [DOI] [PubMed] [Google Scholar]
- 31.Motl RW, Snook EM, McAuley E, Scott JA, Douglass ML. Correlates of physical activity among individuals with multiplesclerosis. Ann Behav Med. 2006;32:154–161. doi: 10.1207/s15324796abm3202_13. [DOI] [PubMed] [Google Scholar]