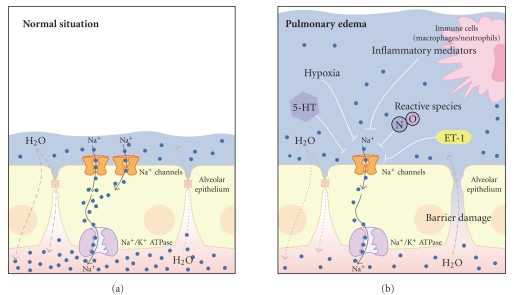
Figure 2.
Impaired Na+ channel activity is associated with the development of pulmonary edema. (a) under normal conditions transepithelial Na+ transport mediated via Na+ channels in the alveolar epithelium drives water reabsorption from the airspaces to the interstitium. This mechanism counteracts water filtration into the airspaces and keeps the fluid layer covering the alveolar epithelium low. (b) a variety of factors that inhibit Na+ channels in the alveolar epithelium have been identified under diseases associated with pulmonary edema such as HAPE or ALI/ARDS: hypoxia, inflammatory mediators which are released by activated immune cells (such as macrophages or neutrophils), endothelin 1 (ET-1), reactive species such as nitric oxide (NO), or factors which are released due to hypoxia or epithelial stress such as serotonin (5-HT). The decreased activity of Na+ channels leads to decreased water reabsorption and fluid accumulation in the airspaces. Under pathological conditions such as HAPE or ALI/ARDS, there is additionally increased fluid filtration into the airspaces due to impaired epithelial barrier integrity. The consequence of both impaired Na+ and thus water reabsorption and increased fluid filtration is the development of pulmonary edema. The figure has been modified from [2]. For clarity, aquaporins and potassium fluxes/channels, as indicated in Figure 1, have been omitted.