Abstract
We looked at the functional outcome of 32 consecutive patients with proximal humeral fractures that required hemiarthroplasty. Functional status was assessed using University of California Los Angeles (UCLA) shoulder end result assessment, simple shoulder test (SST) and American Shoulder and Elbow Society (ASES) shoulder index. Mean age of the patients was 72.2 years and the mean follow-up was 25.3 months. The mean score on UCLA shoulder end result assessment was 24.8, the mean SST score was 7.4 and the mean ASES shoulder index was 67.2. Mean active forward elevation was 85.1°. Patient satisfaction was around 81%. Radiologically, no dislocation, loosening or greater tuberosity pull off was seen. Superior migration of the humeral head was seen in 11 patients (34%). There was no significant difference seen in functional outcome among different genders, age and those who had radiological superior migration of the prosthesis. However, there was a significant statistical difference seen in the functional outcome between patients who had a deficient or a good quality cuff showing that quality of the rotator cuff is an important predicator of functional outcome.
Introduction
Proximal humeral fractures account for 4–8% of all fractures [1]. About 80% of these can be treated non-surgically when they are undisplaced or minimally displaced. However, displaced fractures usually require surgical intervention [2]. The management of severely displaced fractures of the proximal humerus remains difficult. Many treatment options have been suggested [3]. Stableforth [4] reported that nonoperative management of four-part proximal humeral fractures is frequently followed by persistent pain, stiffness and dysfunction of the shoulder. The results of internal fixation for four-part fracture dislocations have been extremely poor [5]. Hemiarthroplasty is typically reserved for comminuted four-part fractures in patients older than 70 years, anatomical neck fractures in elderly patients, head splitting fractures and fracture dislocations [6]. Hemiarthroplasty is also recommended in younger patients with similar fractures where stable and nearly anatomical reduction cannot be achieved [7].
This prospective study was performed to examine the functional outcome and the radiological results of proximal humeral hemiarthroplasty for fractures using the Comprehensive® Fracture System (Biomet, Inc., Warsaw, IN). We also investigated the influence of different parameters including age, gender, cuff deficiency and superior migration on the results and outcome.
Materials and methods
This study included patients between July 2004 and December 2006 who were admitted with proximal humeral fractures requiring hemiarthroplasty. All operations were performed by the senior author (CS) or under his direct supervision. The inclusion criteria were isolated injury, closed fracture, surgical intervention within two weeks of the injury and at least one year of follow-up. The exclusion criteria included previous history of fracture to the same shoulder, previous surgery and internal fixation of the shoulder, open fractures, pathological fractures and multiple injuries. Fifty-two patients were identified who had been treated with the hemiarthroplasty. However, when the inclusion and exclusion criteria’s were applied, only 32 were deemed suitable to be included in the study.
We used Neer’s classification to describe the fracture configuration. However, we are aware of the limitations of this classification [8, 9]. Cefuroxime (1.5 g) was given intravenously at the time of induction. Patients were placed in the beach chair position and a standard deltopectoral approach was used. Long head of biceps tendon was used to identify the tuberosities. Biceps tenodesis was performed in all patients. Rotator cuff anatomy was visually inspected. Comprehensive® Fracture stem (Biomet, Inc., Warsaw, IN) was implanted with cement. The Comprehensive® Fracture stem (Fig. 1) is made of chromium cobalt. It has two lateral fins and a single medial fin for tuberosity fixation. The lateral fin has three suture holes and the medial fin has one suture hole. The distal end of the stem is smooth for cement fixation while the compact low profile proximal end is coated with titanium plasma spray to enhance the tuberosity fixation. We used Gentamycin impregnated Palacos® cement (Heraeus Medical GmbH, Germany), which was inserted with hand after vacuum mixing and pressurised with thumb. Number 2 Orthocord (DePuy Mitek, Raynham, MA) was used to reconstruct the tuberosities with two sutures in the medial circumflex cerclage fashion through the medial fin of the implant, two sutures in circumflex fashion through the two tuberosities and the fins of the implant, with another two transosseous sutures in the vertical tension band configuration [10, 11]. Autogenous bone graft was taken from the extracted humeral head. The stem was implanted in approximately 30° retroversion, using an external alignment rod in the stem parallel to the forearm. The height of the prosthesis was reconstructed taking care to keep the head to tuberosity distance to around 10 mm as described by Mighell et al. [12]. Drains were not used routinely and the arm was placed in a sling. However, active elbow, wrist and hand movements were started from the first postoperative day [13].
Fig. 1.

Comprehensive® Fracture stem
The arm was kept in a sling in neutral rotation for six weeks, with only elbow exercises being allowed. From the seventh to 12th weeks, the patients progressed from pendulum to active-assisted exercises, and from the 13th week, active exercises were started. Postoperative mobilisation protocol was supervised by a team of specialist shoulder physiotherapists [13]. Patients were reviewed again at two weeks, six weeks, twelve weeks, six months and then yearly afterwards. Standardised radiographs were also taken at these intervals.
Patients were assessed independently by other authors (NHS, SBF). Functional status was assessed using University of California Los Angeles (UCLA) shoulder end result assessment [14], simple shoulder test (SST) [15] and American Shoulder and Elbow Society (ASES) shoulder index [16].
Radiological evaluation was performed with standardised anteroposterior and axillary radiographs which were performed using the previously defined protocols [13] (Fig. 2). If a patient was uncomfortable having an axillary radiograph then a modified axillary view was taken [17]. Images were compared to previous follow-up radiographs for any interval change in the position of the prosthesis, displacement and union of the tuberosities, superior migration or dislocation of the humeral head, radiolucent lines [18] and ectopic bone formation. Subluxation was defined when the prosthetic head was eccentrically positioned on the glenoid. Prosthetic migration was recorded by measuring the distance from the lowest part of the articular portion of the prosthetic head to a specific identifiable bony land mark on the humerus as described by Zyto et al. [19].
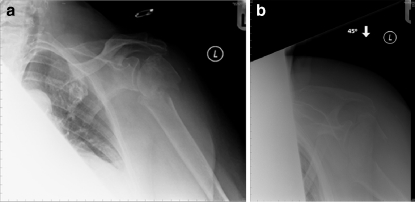
Fig. 2.
a, b Radiographs of left shoulder in a 70-year-old lady showing four-part proximal humeral fracture
Statistical analysis was performed using the software Medcalc (Version 10.1, Mariakerke, Belgium). Results were evaluated with the Mann-Whitney U test and the null hypothesis was rejected if the p value was <0.05 which was regarded significant. The mean and median values and 95% confidence intervals (CI) are presented in the tables.
Results
In our study, 32 patients were available for follow-up with a mean follow up of 25.3 months (range 12–48 months). There were eight males and 24 females, with a mean age of 72.2 years (range 53–89 years). Table 1 illustrates the clinical details and results of the 32 patients.
Table 1.
Clinical details and results
| Patient number | Age (y) | Gender | Follow-up (mo) | Fracture type | Cuff | Radiograph | SST | UCLA | ASES | Active FF |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 89 | F | 24 | 3 | Deficient | Sublux | 6 | 23 | 71.7 | 60 |
| 2 | 73 | M | 12 | 4 | Deficient | None | 8 | 27 | 73.3 | 60 |
| 3 | 67 | F | 12 | 4 | Good | None | 8 | 27 | 75 | 60 |
| 4 | 53 | M | 24 | 4 | Good | Sublux | 9 | 30 | 85 | 90 |
| 5 | 84 | F | 24 | D + 4* | Deficient | None | 8 | 27 | 78.3 | 90 |
| 6 | 78 | F | 36 | 4 | Deficient | Sublux | 6 | 13 | 43.3 | 60 |
| 7 | 78 | M | 36 | 4 | Good | None | 10 | 31 | 85 | 90 |
| 8 | 64 | F | 24 | 4 | Deficient | None | 10 | 31 | 83.3 | 130 |
| 9 | 69 | F | 12 | D + 4 | Deficient | None | 3 | 7 | 23.3 | 20 |
| 10 | 63 | F | 36 | 4 | Good | None | 10 | 35 | 83.3 | 160 |
| 11 | 69 | M | 14 | 4 | Deficient | Sublux | 8 | 20 | 56.6 | 100 |
| 12 | 76 | M | 36 | D + 4 | Deficient | None | 8 | 25 | 66.6 | 90 |
| 13 | 71 | F | 30 | 4 | Good | Sublux | 7 | 27 | 55 | 50 |
| 14 | 64 | M | 37 | D + 4 | Good | Sublux | 11 | 26 | 71.6 | 120 |
| 15 | 76 | M | 12 | 4 | Deficient | None | 10 | 32 | 86.6 | 130 |
| 16 | 83 | F | 12 | 4 | Deficient | None | 9 | 26 | 70 | 100 |
| 17 | 64 | F | 30 | 4 | Good | None | 10 | 28 | 73.3 | 90 |
| 18 | 62 | F | 24 | 4 | Deficient | None | 5 | 23 | 60 | 110 |
| 19 | 78 | F | 24 | D + 4 | Deficient | None | 7 | 14 | 48.3 | 45 |
| 20 | 79 | F | 12 | D + 4 | Deficient | None | 5 | 16 | 58.3 | 50 |
| 21 | 55 | F | 24 | 3 | Deficient | None | 7 | 28 | 73.3 | 60 |
| 22 | 64 | F | 34 | 4 | Good | Sublux | 8 | 29 | 71.6 | 70 |
| 23 | 76 | F | 24 | 3 | Deficient | None | 8 | 28 | 76.6 | 120 |
| 24 | 54 | F | 30 | 4 | Good | None | 8 | 31 | 75 | 100 |
| 25 | 76 | F | 36 | 3 | Deficient | None | 8 | 28 | 75 | 110 |
| 26 | 86 | F | 30 | 4 | Deficient | None | 7 | 25 | 58.3 | 90 |
| 27 | 75 | F | 48 | 4 | Deficient | None | 8 | 30 | 68.3 | 90 |
| 28 | 75 | F | 24 | 4 | Deficient | None | 9 | 30 | 81.6 | 120 |
| 29 | 84 | M | 12 | 4 | Deficient | None | 4 | 13 | 41.6 | 50 |
| 30 | 65 | F | 30 | 4 | Good | Sublux | 4 | 25 | 70 | 90 |
| 31 | 87 | F | 24 | 4 | Deficient | Sublux | 5 | 23 | 60 | 60 |
| 32 | 76 | F | 24 | D + 4 | Deficient | Sublux | 4 | 17 | 53.3 | 60 |
D + 4 four-part fracture dislocation, SST simple shoulder test, UCLA University of California Los Angeles shoulder end result assessment, ASES American Shoulder and Elbow Society shoulder index, active FF active forward flexion
Twenty-six patients (81%) were living independently prior to their injury, while one patient was dependent and the remaining five were receiving some assistance. At their final follow-up visit, 18 patients (56%) were completely independent; two were completely dependent, while 12 patients required assistance at home.
Twelve of the 32 patients had no significant past medical history while the other 20 patients had significant medical history varying from pulmonary disease, ischemic heart disease, diabetes, Parkinsonism and depression. Two patients were on treatment for osteoporosis prior to the injury. Twenty-six patients were non-smokers. Twelve patients denied any alcohol intake, 18 claimed only social intake while two claimed excessive alcohol intake before their injury. A summary of the functional outcome is presented in Table 2.
Table 2.
Functional outcome
| Outcome measure | Mean | Median | 95% CI | Range |
|---|---|---|---|---|
| Active forward flexion in degrees | 85.1° | 90° | 60–100° | 20–160° |
| Simple shoulder test (out of 12) | 7.4 | 8 | 7–8 | 3–11 |
| UCLA shoulder end result assessment (out of 35) | 24.8 | 27 | 23.4–28 | 7–35 |
| ASES shoulder index (out of 100) | 67.2 | 71.6 | 60–75 | 23–86 |
Pain At the final follow-up, 84% of patients had either no pain (18 patients) or only mild pain with heavy activity (nine patients). Four patients (12.5%) complained of pain after light activity and one had continuous pain that required regular analgesia.
Movements Mean active forward elevation was 85.1° (range 20–160°). Six patients had active forward elevation of more than 120° and another 13 patients had 90–120° of active forward elevation (59%). Twelve patients had forward elevation between 45–90° and one patient regained only 20° forward elevation.
Function Only one patient stated normal function after hemiarthroplasty. Fourteen patients claimed to have slight restriction or restriction with the overhead activities. Six patients were able to perform household activities, driving and shopping, and eight could only perform activities of daily living and light work. Another three claimed only light activities and one patient was unable to use her shoulder.
Strength Five patients had normal strength (Medical Research Council (MRC) grade 5). Thirteen had strength against resistance (MRC grade 4). Ten patients could lift their arm against gravity but not against resistance (MRC grade 3) while three could only lift their arm when the gravity was eliminated (MRC grade 2). Flickering of the muscles was present in only one patient (MRC grade 1).
Patient satisfaction Twenty-six patients (81%) were satisfied with their outcome from the surgery. Six patients remained unsatisfied with their outcome, out of these, three were independent and the other three were partially dependent in their activities prior to the injury. However, five of them were dependent at the last follow up. No significant comorbidities were noticed in them.
Radiographs Images taken one year after surgery revealed superior migration of the prosthesis in ten patients; however, no dislocation was seen. The rest of the 22 patients had no evidence of instability or impingement on the radiographs. There was no significant difference in the ASES index, UCLA score, SST and active forward elevation between patients who had postoperative superior prosthetic head migration and those who had normal radiographs.One patient had lesser tuberosity displacement and showed anterior subluxation. However, she had had another fall three months after the surgery. She refused to have further surgical intervention to address this complication. Apart from this patient, radiographs of the other 31 patients revealed union of the tuberosities (Fig. 3). None of the radiographs at the last follow-up revealed any radiolucent lines, cement fractures or migration of the stem nor was ectopic bone formation seen in our series.
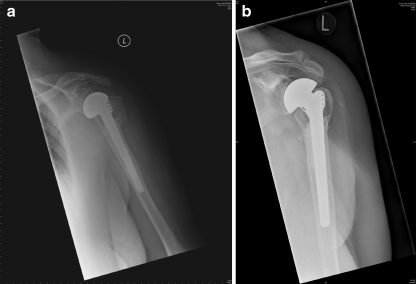
Fig. 3.
Postoperative radiographs. Immediate postoperative (a) and at two-years follow-up (b) showing good position of prosthesis and satisfactory healing of tuberosities
Table 3 demonstrates outcomes in different subsets of patients. No statistically significant difference was seen in gender, age and radiological appearance. However, the quality of the rotator cuff had significant impact on the functional outcome. There were ten patients with good quality cuff while in the rest of the 22 patients the rotator cuff was deficient. There were significant differences in ASES scores (P = 0.05), UCLA score (P = 0.01) and SST (P = 0.04) between patients who had good quality cuff and those with lack of integrity of the rotator cuff.
Table 3.
Outcome in different sub groups of patients
| Measure | Mean ASES (95% CI) | Mean UCLA (95% CI) | Mean SST (95% CI) | Mean active FF (95% CI) |
|---|---|---|---|---|
| Female (n = 24) | 70.8 (58.3–75) | 27 (23–28.5) | 7.5 (5.9–8) | 90 (60–100) |
| Male (n = 8) | 72.4 (45.8–86.1) | 26.5 (14.9–31) | 8.5 (5.1–10.7) | 90 (52.8–127) |
| p value | 0.42 | 0.74 | 0.07 | 0.51 |
| >70 years (n = 19) | 68.3 (55.2–76.4) | 26 (17.3–28) | 8 (6–8) | 90 (60–99.3) |
| <70 years (n = 13) | 73.3 (59.6–83.3) | 28 (22.6–31) | 8 (4.8–10) | 90 (60–121.1) |
| p value | 0.33 | 0.25 | 0.33 | 0.21 |
| Deficient cuff (n = 22) | 67.4 (56.9–74.6) | 25 (17.6–28) | 7.5 (5.2–8) | 90 (60–107.8) |
| Good cuff (n = 10) | 74.1 (68.3–85) | 28.5 (25.8–31) | 8.5 (6.6–10.1) | 90 (58.8–124.4) |
| p value | 0.05 | 0.01 | 0.04 | 0.56 |
| Normal X-ray (n = 22) | 73.3 (61.4–77.9) | 27.5 (25–30) | 8 (7–9) | 90 (60–110) |
| Superior migration (n = 10) | 65 (52.1–73.1) | 24 (16.5–29.1) | 6.5 (4–9.2) | 65 (58.8–102.2) |
| p value | 0.12 | 0.12 | 0.21 | 0.29 |
SST simple shoulder test, UCLA University of California Los Angeles shoulder end result assessment, ASES American Shoulder and Elbow Society shoulder index, active FF active forward flexion
The Mann-Whitney U test was used to test for significance (p value)
Complications One case of superficial infection was seen in our series which was treated with oral antibiotics. No case of deep infection, deep venous thrombosis or myocardial infarction was seen. Preoperatively, one patient had axillary nerve neurapraxia while incomplete brachial plexus injury was seen in another. Both of these injuries improved with time. None of the patients required revision surgery.
Discussion
Hemiarthroplasty for proximal humeral fracture is performed with the aim to restore normal biomechanics, achieve adequate range of movement and to provide a painless functional joint to the patients [7]. It is a technically demanding procedure that requires restoration of the humeral height, anatomical reconstruction of the tuberosities and fixation of the stem in correct retroversion [11]. Preoperative patient selection and postoperative rehabilitation are important factors affecting the outcome [3, 6]. Zyto et al. [19] mentioned that median forward elevation was 70° among their 27 patients. In their series of 20 patients, Anjum et al. [20] reported that four patients claimed to have moderate pain after the hemiarthroplasty and the median forward elevation and abduction was around 60°. Prakash et al. [21] stated that among their 22 patients mean forward flexion was 93° and the pain relief was the most predictable outcome. The mean active forward elevation in our report was 85.1°, which is comparable to other studies.
Tuberosity fixation is one of the key elements of reconstruction, as well as outcome [6, 11, 12, 22]. Boileau et al. [11], in their series, noticed a tuberosity migration rate of 23%, with a nonunion rate of 17%. Subsequently, they changed their postoperative mobilisation technique to delayed mobilisation. Demirhan et al. [23] had around 27% greater tuberosity displacement rate. Prakash et al. [21] reported greater tuberosity had displaced in 12.5% of their patients. Although, 96% tuberosity union was reported by Mighell et al. [12]. In our series, we did not have any greater tuberosity migration and only one lesser tuberosity displacement. We adopted delayed mobilisation (as Boileau et al. [11] had done) which may explain our good results; however, it could also be due to our tuberosity fixation technique or the implant used. This study cannot determine the importance of these other factors.
Goldman et al. [24], in their series of 22 patients, described that hemiarthroplasty can give reasonable pain relief in the shoulder; however, functional outcome and range of movement cannot be predicted. Most of the studies report patient satisfaction rate of approximately 80% after hemiarthroplasty [3, 12, 20, 21, 23]. This high patient satisfaction rate despite reduced range of movement and function could be due to reasonable pain relief following hemiarthroplasty. In our series, 81% patients were completely satisfied with their outcome and 84% patients had either no pain or only mild pain with heavy activity.
In our series, there was no significant difference in functional outcome, after the shoulder hemiarthroplasty for proximal humeral fractures, between different ages, genders or superior subluxation. Similar results were reported by Demirhan et al. [23] in their study of 32 cases and by Mighell et al. [12] in a study of 72 patients. However, Boileau et al. [11], in a study of 66 patients, found increased greater tuberosity migration and poor outcome in women over 75 years of age. They had patients of wide age range (31–85 years) which may have had an effect on their results. In our study however, the youngest patient was 53 years old.
Gronhagen et al. [25], in a study of 46 patients, mentioned poor functional outcome in patients with rotator cuff deficiency following shoulder hemiarthroplasty for comminute proximal humeral fractures. However, they did not show any statistical difference. Our study is the first to show a statistically significant difference in functional outcome between patients with good quality rotator cuff and those with deficient cuff (Table 3).
Some of the strengths of our study include the length of the follow-up, that none of our patients were lost to follow-up, and that all the patients were operated upon by the same surgeon, received the same implant and had a similar postoperative rehabilitation. We acknowledge the weakness of our study that a small cohort of patients was included, but in spite of this our series showed comparative results to other studies.
In conclusion, our results show that shoulder hemiarthroplasty using the Comprehensive® Fracture stem (Biomet, Inc., Warsaw, IN) is reliable in providing pain free shoulder after such a serious and disabling injury as reported by others using different implants [3, 12, 20, 21, 23]. We showed that the outcome after the hemiarthroplasty is independent of age, gender or superior subluxation of the humeral head but is directly correlated to the quality of the rotator cuff. This might justify the use of a different prosthesis in such a situation; however, this is a topic for further research.
Contributor Information
Nasir Shah, Email: nasir110@btinternet.com.
Hafiz J. Iqbal, Email: hafjavaid@yahoo.com
References
- 1.Lind T, Kroner K, Jensen J. The epidemiology of fractures of the proximal humerus. Arch Orthop Trauma Surg. 1989;108–5:285–287. doi: 10.1007/BF00932316. [DOI] [PubMed] [Google Scholar]
- 2.Iannotti JP, Ramsey ML, Williams GR, Jr, Warner JJ. Nonprosthetic management of proximal humeral fractures. Instr Course Lect. 2004;53:403–416. [PubMed] [Google Scholar]
- 3.Hawkins RJ, Angelo RL. Displaced proximal humeral fractures. Selecting treatment, avoiding pitfalls. Orthop Clin North Am. 1987;18–3:421–431. [PubMed] [Google Scholar]
- 4.Stableforth PG. Four-part fractures of the neck of the humerus. J Bone Joint Surg Br. 1984;66:104–108. doi: 10.1302/0301-620X.66B1.6693466. [DOI] [PubMed] [Google Scholar]
- 5.Darder A, Darder A, Jr, Sanchis V, Gastaldi E, Gomar F. Four-part displaced proximal humeral fractures: operative treatment using Kirschner wires and a tension band. J Orthop Trauma. 1993;7:497–505. doi: 10.1097/00005131-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Compito CA, Self EB, Bigliani LU. Arthroplasty and acute shoulder trauma. Reasons for success and failure. Clin Orthop Relat Res. 1994;307:27–36. [PubMed] [Google Scholar]
- 7.Kontakis G, Koutras C, Tosounidis T, Giannoudis P. Early management of proximal humeral fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg Br. 2008;90:1407–1413. doi: 10.1302/0301-620X.90B11.21070. [DOI] [PubMed] [Google Scholar]
- 8.Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 9.Shrader MW, Sanchez-Sotelo J, Sperling JW, Rowland CM, Cofield RH. Understanding proximal humerus fractures: image analysis, classification, and treatment. J Shoulder Elbow Surg. 2005;14:497–505. doi: 10.1016/j.jse.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 10.Frankle MA, Ondrovic LE, Markee BA, Harris ML, Lee WE. Stability of tuberosity reattachment in proximal humeral hemiarthroplasty. J Shoulder Elbow Surg. 2002;11:413–420. doi: 10.1067/mse.2002.126098. [DOI] [PubMed] [Google Scholar]
- 11.Boileau P, Krishnan SG, Tinsi L, Walch G, Coste JS, Mole D. Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2002;11:401–412. doi: 10.1067/mse.2002.124527. [DOI] [PubMed] [Google Scholar]
- 12.Mighell MA, Kolm GP, Collinge CA, Frankle MA. Outcomes of hemiarthroplasty for fractures of the proximal humerus. J Shoulder Elbow Surg. 2003;12:569–577. doi: 10.1016/S1058-2746(03)00213-1. [DOI] [PubMed] [Google Scholar]
- 13.Agorastides I, Sinopidis C, El Meligy M, Yin Q, Brownson P, Frostick SP. Early versus late mobilization after hemiarthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2007;16(Suppl):S33–S38. doi: 10.1016/j.jse.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 14.Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed] [Google Scholar]
- 15.Lippitt SB, Harryman DT, Matsen FA (1993) A practical tool for evaluating function: The simple shoulder test. In Matsen FA, Fu FH, Hawkins RJ (eds) The shoulder: A balance of mobility and stability. American Academy of Orthopaedic Surgeons, Rosemont, IL, pp 519–529
- 16.Cook KF, Roddey TS, Olson SL, et al. Reliability by surgical status of self-reported outcomes in patients who have shoulder pathologies. J Orthop Sports Phys Ther. 2002;32:336–346. doi: 10.2519/jospt.2002.32.7.336. [DOI] [PubMed] [Google Scholar]
- 17.Wallace WA, Hellier M. Improving radiographs of the injured shoulder. Radiography. 1983;49:229–233. [PubMed] [Google Scholar]
- 18.Torrens C, Martinez-Diaz S, Ruiz A, et al. Assessment of radiolucent lines in cemented shoulder hemi-arthroplasties: study of concordance and reproducibility. Int Orthop. 2009;33(1):165–169. doi: 10.1007/s00264-007-0452-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zyto K, Wallace WA, Frostick SP, Preston BJ. Outcome after hemiarthroplasty for three- and four-part fractures of the proximal humerus. J Shoulder Elbow Surg. 1998;7:85–89. doi: 10.1016/S1058-2746(98)90215-4. [DOI] [PubMed] [Google Scholar]
- 20.Anjum SN, Butt MS. Treatment of comminuted proximal humerus fractures with shoulder hemiarthroplasty in elderly patients. Acta Orthop Belg. 2005;71:388–395. [PubMed] [Google Scholar]
- 21.Prakash U, McGurty DW, Dent JA. Hemiarthroplasty for severe fractures of the proximal humerus. J Shoulder Elbow Surg. 2002;11:428–430. doi: 10.1067/mse.2002.126615. [DOI] [PubMed] [Google Scholar]
- 22.Sperling JW, Cuomo F, Hill JD, Hertel R, Chuinard C, Boileau P. The difficult proximal humerus fracture: tips and techniques to avoid complications and improve results. Instr Course Lect. 2007;56:45–57. [PubMed] [Google Scholar]
- 23.Demirhan M, Kilicoglu O, Altinel L, Eralp L, Akalin Y. Prognostic factors in prosthetic replacement for acute proximal humerus fractures. J Orthop Trauma. 2003;17:181–188. doi: 10.1097/00005131-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Goldman RT, Koval KJ, Cuomo F, Gallagher MA, Zuckerman JD. Functional outcome after humeral head replacement for acute three- and four-part proximal humeral fractures. J Shoulder Elbow Surg. 1995;4:81–86. doi: 10.1016/S1058-2746(05)80059-X. [DOI] [PubMed] [Google Scholar]
- 25.Gronhagen CM, Abbaszadegan H, Revay SA, Adolphson PY. Medium-term results after primary hemiarthroplasty for comminute proximal humerus fractures: a study of 46 patients followed up for an average of 4.4 years. J Shoulder Elbow Surg. 2007;16:766–773. doi: 10.1016/j.jse.2007.03.017. [DOI] [PubMed] [Google Scholar]