Abstract
Background
Little information is available on depressive symptom change in persons with stroke.
Objectives
Provide estimates of change in depressive symptoms and determine how depressive symptom change influences recovery of functional status.
Design
Prospective cohort study.
Setting
Eleven in-patient medical rehabilitation facilities located across the U.S.
Participants
544 persons with a first-time stroke.
Measurements
General linear regression model estimates assessed associations between depressive symptom change and functional status 3 and 12 months post discharge.
Results
The majority of persons with stroke were aged 75 and older, white, female and married. The most prevalent stroke type was ischemic. Non-depressed patients at discharge who reported fewer symptoms 12-months later had an adjusted functional status score of 108.2. This compared to adjusted functional status scores of 104.6 for those non-depressed at discharge with increasing symptoms over the 12-month follow-up, 100.3 for those depressed at discharge with fewer symptoms over the 12-month follow-up, and 88.0 for those depressed at discharge with more symptoms over the 12-month follow-up.
Conclusion
Tracking depressive symptom change in hospital and post discharge is clinically relevant and an important component of patient care and recovery of functional status.
Keywords: Stroke, Depression, Functional Status
INTRODUCTION
Depression is a frequent complication of stroke. A recent review and meta-analysis1 of community, hospital and rehabilitation based studies found one-third of stroke survivors experience depression at some point during the acute, medium and long-term phases of recovery. Other studies2–4 report the highest rates of depression in the initial months following stroke with a gradient of decline over 12–24 months.
Reported differences in rates of depression post-stroke raise the question of whether there is a need to more precisely track change in depression status among those classified as either depressed or non-depressed post stroke. A focus on depressive symptoms and change in depressive symptoms post-stroke may provide insight about the possibility and time course of recovery, help set therapeutic goals and plan for appropriate care in-hospital and post discharge. Also, a more precise understanding of patterns of depressive symptom change could help predict improvement in functional status. Some investigations have documented the negative and significant impact depression has on recovery of functional ability post stroke,5, 6 whereas others report non-significant associations.7, 8
In the current study, we examined 544 persons with a first time stroke admitted to an in-patient medical rehabilitation facility. Objectives of the study were to provide estimates of depression at time of discharge from in-patient medical rehabilitation and at 3 and 12 months post-discharge, assess change in depression status (e.g., depressed to non-depressed), change in depressive symptoms and how change in depressive symptoms influences recovery of functional status.
METHODS
Source of Data
Data came from the Stroke Recovery in Underserved Populations database, an observational follow-up study of persons with first time stroke who received care at an inpatient medical rehabilitation facility in 2005–2006. A total of 11 inpatient medical rehabilitation facilities were included in the study. The facilities were located across diverse regions of the country including California, Florida, Iowa, Illinois, Kentucky, New Jersey, New York (2), Texas (2), and Washington, DC. Operating bed sizes ranged from 12 to 155 (median bed size = 78). All 11 facilities were accredited by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO); and all but one facility was accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF).
Data Collection
Sociodemographic and clinical measures were collected within 72 hours of discharge from the inpatient medical rehabilitation facility and at 3 and 12 months post-discharge. Nursing staff at the medical rehabilitation facility collected discharge information, and nurse researchers using telephone interview collected post-discharge information. Discharge and follow-up interviews were conducted in Spanish or English. Previous studies have documented the reliability and concurrent validity of collecting clinical information, including functional status, using post-discharge telephone interview by trained research nurses.9, 10
Study Population
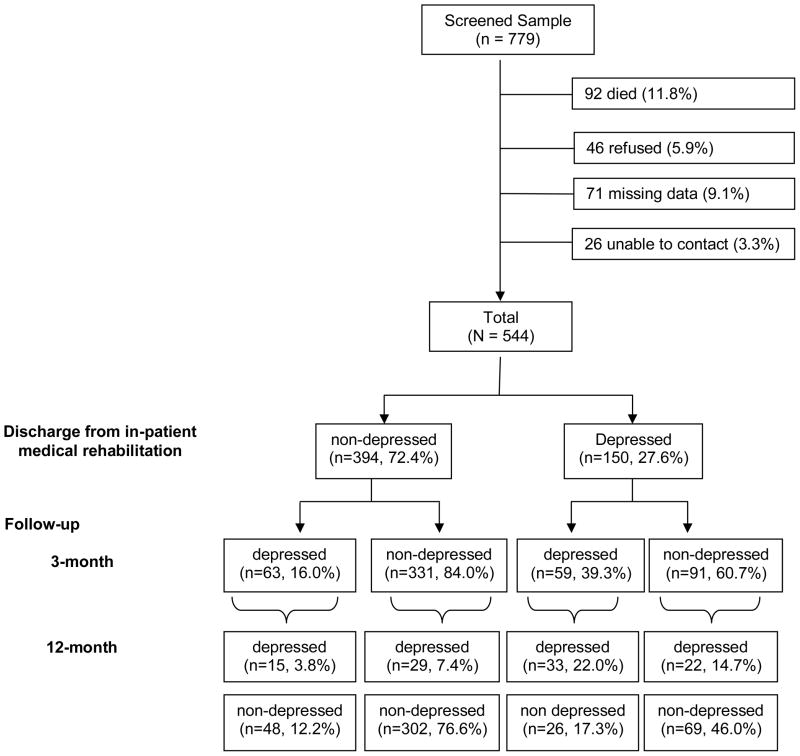
Patients eligible for study inclusion were admitted between April, 2005 and October, 2006 to an inpatient medical rehabilitation facility with a diagnosis of a first time stroke (ICD-9 codes 430–438) and aged 65 years or older of either gender. Patients were screened for cognitive appropriateness by nursing staff, regarding their ability to respond to basic questions about orientation to person, place, and time. A total of 779 patients aged 65 and older were eligible for study (Figure 1). Of these, 544 had complete information at all interview time points, 92 died, 46 refused the 3 or 12 month follow-up interview and 26 could not be contacted post-discharge. An additional 71 persons were removed because of missing data on measures of interest. To evaluate the potential bias of those excluded from the study, we tested for significant differences across sociodemographic and clinical measures. After reviewing these measures, we did not identify significant differences between persons included in the study and those excluded by gender, race, education, marital status, body involvement, comorbidity, type of stroke, length of stay, pain ratings, or in-patient rehabilitation facility. Persons included in the study were significantly more likely to be younger and better educated. Central and local ethical committee approval was sought and obtained. Consent was obtained at the time of the discharge interview.
Figure 1.
Depression status at discharge, and 3 and 12 months post discharge.
Measures
Depression
A 20-item Center for Epidemiologic Studies-Depression (CES-D) scale11 was used to determine depression status and symptom change at discharge and 3 and 12 months post discharge. Responses were scored on a four-point scale (0–3) and ranged from 0 (rarely or none of the time) to 3 (most of the time). Summing the responses created a depression summary score ranging from 0 to 60, with higher scores indicating more depressive symptoms. The CES-D scale was used as a continuous and categorical measure (0 – 15 and ≥ 16), according to previously established criteria.11 A score ≥16 on the CES-D scale is suggestive of clinically significant depression.12 The reliability and validity of the CES-D scale has been established.11, 13–15
Depressive symptom change was determined by subtracting discharge CES-D score from the 3 and 12 month CES-D follow up score, respectively. The categorical discharge CES-D score together with the 3 and 12 month continuous depressive change score was used to create a four level depression measure: 1) non-depressed at discharge and fewer symptoms at follow up; 2) non-depressed at discharge and more symptoms at follow up; 3) depressed at discharge and fewer symptoms at follow up; and 4) depressed at discharge and more symptoms at follow up.
Covariates
Sociodemographic and clinical measures were included as covariates in the statistical models described below. Sociodemographic characteristics included age (65–95), gender, marital status, (married vs. unmarried), race/ethnicity (white vs. black or Hispanic) and education (< high school vs. ≥ high school). Clinical measures included a summary comorbidity scale (myocardial infarction, diabetes, arthritis, kidney disease, and cancer), length of hospital stay, pain rating (0 – 10), stroke type (ischemic, hemorrhagic, or other), body involvement (right, left, bilateral or no paresis) and prior history of depression (ICD-9 code 296.2 (major depressive episode–single), 296.3 (major depressive episode–recurrent), 311 (depressive disorder not otherwise specified)).
Outcome
Functional status was assessed by the Inpatient Rehabilitation Facilities–Patient Assessment Instrument (IRF-PAI). The IRF-PAI is a 54-item instrument used to assign medical rehabilitation inpatients to a case-mix group. The case-mix group determines prospective reimbursement for medical rehabilitation by the Centers for Medicare and Medicaid Services (CMS).16–18 The functional status items in the IRF-PAI are from the Functional Independence Measure (FIM) instrument, a standardized measure including 18 items covering six domains: self-care, sphincter control, transfer, locomotion, communication, and social cognition.19 All 18 items are scored into one of seven levels of function, ranging from complete dependence (level 1) to complete independence (level 7). Total FIM ratings have a potential range of 18 to 126, where higher scores indicate greater functional independence. Total FIM ratings can be grouped into Motor and Cognition ratings. Motor ratings contain self-care, sphincter control, mobility, and locomotion items, and Cognition ratings contain communication and social cognition items.19 Ratings for the motor subscale ranges from 9 to 91, and for the cognition subscale from 5 to 35. The reliability, validity, and responsiveness of the FIM instrument have been widely investigated.19–21 The reliability (intraclass correlation coefficient) of the Total FIM and of its domains has consistently been found to be > 0.85.20, 21
Statistical Analysis
We compared discharge sociodemographic and clinical measures stratified by depression status using means (SD) for continuous measures and χ2 test for categorical measures. We calculated the proportion of persons classified as depressed and those non-depressed at discharge and 3 and 12 months post-discharge. Chi-square test was used to compare sociodemographic and clinical measures in persons who reported fewer depressive symptoms from discharge to 3 and 12 month follow up with those who reported more depressive symptoms.
Unadjusted and adjusted general linear regression model estimates were used to assess associations between a 4-level depression measure and Total FIM score and Motor and Cognition FIM score at 3 and 12 months post discharge. Adjusted models sequentially controlled for potentially confounding sociodemographic and clinical factors. Statistical analyses were performed using SAS software, version 9.2 (SAS Institute, Cary, NC). All reported P values were two-sided and results were considered statistically significant at the P < 0.05.
RESULTS
Of the 544 persons included in the analysis, most were aged 75 and older, white, female and married (Table 1). Less than half had an educational level below high school. The most prevalent stroke type was ischemic, followed by hemorrhagic and other stroke. A similar percentage of persons with stroke had left or right body involvement. A large majority reported ≥ 1 comorbidity and the average length of stay was 20.4 (SD 9.5) days. Non-significant differences in sociodemographic and clinical measures were found between the depressed and non-depressed at discharge with the exception of pain ratings (p < 0.04), which were higher among those classified as depressed (CES-D score ≥ 16).
Table 1.
Discharge characteristics of persons with stroke by depression status.
| Characteristic | Total sample N = 544 n (%) |
Non-depressed N = 394 n (%) |
Depressed N = 150 n (%) |
p-value |
|---|---|---|---|---|
| Age | .62 | |||
| 65–74 | 223 (41.0) | 159 (40.4) | 64 (42.7) | |
| 75 and above | 321 (59.0) | 235 (59.6) | 86 (57.3) | |
| Education | .90 | |||
| < High School | 130 (23.9) | 99 (25.1) | 31 (20.7) | |
| ≥ High School | 414 (76.1) | 295 (74.9) | 119 (79.3) | |
| Sex | .30 | |||
| Male | 249 (45.8) | 175 (44.4) | 74 (49.3) | |
| Female | 295 (54.2) | 219 (55.6) | 76 (50.7) | |
| Ethnicity/Race | .20 | |||
| White | 430 (79.0) | 306 (77.7) | 124 (82.7) | |
| Nonwhite | 114 (21.0) | 88 (22.3) | 26 (17.3) | |
| Marital status | .19 | |||
| Married | 287 (52.8) | 201 (51.0) | 86 (57.3) | |
| Unmarried | 257 (47.2) | 193 (49.0) | 64 (42.7) | |
| Type of stroke | .49 | |||
| Ischemic | 425 (78.1) | 310 (78.7) | 115 (76.7) | |
| Hemorrhagic | 70 (12.9) | 52 (13.2) | 18 (12.0) | |
| Other | 49 (9.0) | 32 (8.1) | 17 (11.3) | |
| Impairment group | .76 | |||
| Left-body | 218 (40.1) | 158 (40.1) | 60 (40.0) | |
| Right-body | 218 (40.1) | 155 (39.3) | 63 (42.0) | |
| Other | 108 (19.9) | 81 (20.6) | 27 (18.0) | |
| Comorbidity | .59 | |||
| None | 10 (1.8) | 8 (2.0) | 2 (1.3) | |
| 1 or more | 534 (98.2) | 386 (98.0) | 148 (98.7) | |
| Pain | .04 | |||
| None | 479 (88.1) | 354 (89.9) | 125 (83.3) | |
| Any | 65 (11.9) | 40 (10.2) | 25 (16.7) | |
| Total FIMa | < 0.01 | |||
| mean (SD) | 81.1 (22.4) | 83.6 (21.6) | 74.3 (23.3) | |
| Motor FIMb | < 0.01 | |||
| mean (SD) | 56.3 (17.5) | 58.2 (16.9) | 51.5 (18.3) | |
| Cognition FIMc | < 0.01 | |||
| mean (SD) | 24.7 (7.2) | 25.4 (7.0) | 22.8 (7.6) | |
| Previous Depression | .03 | |||
| No | 480 (88.2) | 355 (90.1) | 125 (83.3) | |
| Yes | 64 (11.8) | 39 (9.9) | 25 (16.7) |
Total FIM scores for the sample ranged from 18–122
Motor FIM scores for the sample ranged from 13–89
Cognition FIM scores for the sample ranged from 5–35
Prior to stroke, 11.8% (n = 64) of the sample had a clinical diagnosis of depression. At discharge, 27.6% (n = 150) were identified as depressed (Figure 1). The general trend over the next 12 months was toward recovery of depression. At three months post discharge, 22.4% (n = 122) were classified as depressed and at 12 months, 18.2% (n = 99) (p = 0.01). Similar trends in depression recovery were found when adjustments were made by age (p = 0.01), gender (p = 0.01) and racial/ethnic group (p = 0.01).
Of those classified as depressed at discharge, 33 (22.0%) remained depressed 3 and 12 months later, while 69 (46.0%) were reclassified as non-depressed at both follow up time points (Figure 1). The remainder (n = 48) moved in and out of depression. Twenty-six (17.3%) were depressed at 3 months but non-depressed at 12 months, while 22 (14.7%) were non-depressed at 3 months but depressed at 12 months. Of the 394 persons identified as non-depressed at discharge, 302 (76.6%) remained non-depressed at 3 and 12 months. Only a small percentage (3.8%) was reclassified as depressed at both follow up time points. Of the remaining 77 persons, 29 (7.3%) were non-depressed at 3 months but depressed at 12 months, and 48 (12.2%) were depressed at 3 months and non-depressed at 12 months.
Mean Total FIM score for those classified as depressed at discharge was 74.32 (SD 23.3), and increased by about 20 points to 94.1 (SD 24.4) at 3 months. At 12 months, Total FIM score was 94.7 (SD 26.7). Mean Total FIM score for those classified as non-depressed at discharge was 83.6 (SD 21.6) and increased to 106.4 (SD 18.9) at 3 months. As with the depressed group, few gains in Total FIM score (107.3, SD 19.7) were noted at 12 months.
General linear model estimates and associated standard errors (SE) were calculated to summarize the relative benefits of being non-depressed at discharge and reporting fewer depressive symptoms at the 3 and 12 month follow up (Table 2). Parameter estimates showed this group to have a 3 month Total FIM score that was 2.9, 7.2 and 13.0 points greater than those categorized as non-depressed at discharge and reporting more depressive symptoms (p = 0.07), depressed at discharge and reporting fewer depressive symptoms (p < 0.01 ), and depressed at discharge and reporting more depressive symptoms (p < 0.01 ), respectively (Model 1). After adjustment for sociodemographic (Model 2) and clinical (Model 3) measures, similar trends of association were found. Other significant variables (p < 0.05) included Total discharge FIM score, race/ethnicity, type of stroke, comorbidity, and length of stay. At 12 months, those non-depressed at discharge who reported fewer depressive symptoms over the follow up period had fully adjusted Total FIM score that was 3.6 (p = 0.06), 7.9 (p < 0.01) and 20.2 (p < 0.01) points greater than those in the other 3 depression categories. Other significant variables (p < 0.05) included Total discharge FIM score, type of stroke, and length of stay.
Table 2.
Linear regression of Total FIM score at 3 and 12 months by depression status at discharge.
| 3 months | 12 months | |||||
|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | Model 1a | Model 2b | Model 3c | |
| b (SE) | b (SE) | b (SE) | b (SE) | b (SE) | b (SE) | |
| Non depressed at discharge, fewer symptomsd | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Non depressed at discharge, more symptoms | −2.9 (1.59) | −1.2 (1.58) | −1.0 (1.55) | −4.7 (1.87)* | −4.3 (1.89)* | −3.6 (1.88) |
| Depressed at discharge, fewer symptoms | −7.2 (1.88)* | −6.5 (1.83)* | −5.8 (1.80)* | −8.5 (2.20)* | −8.9 (2.20)* | −7.9 (2.19)* |
| Depressed at discharge, more symptoms | −13.0 (3.22)* | −12.7 (3.14)* | −11.7 (3.11)* | −21.4 (4.15)* | −20.4 (4.17)* | −20.2 (4.13)* |
| Total FIM at discharge | 0.7 (0.03)* | 0.7 (0.03)* | 0.6 (0.03)* | 0.6 (0.03)* | 0.6 (0.03)* | 0.5 (0.04)* |
| Age (≥ 75 vs. < 75) | −0.2 (1.25) | −0.3 (1.24) | −2.4 (1.56) | −2.0 (1.57) | ||
| Education (≥ 12 vs. <12) | 1.1 (1.44) | 0.7 (1.44) | 2.7 (1.81) | 2.8 (1.81) | ||
| Sex (female vs. male) | −0.2 (1.22) | −1.0 (1.29) | −0.9 (1.53) | −2.2 (1.63) | ||
| Race (white vs. nonwhite) | 8.6 (1.54)* | 9.3 (1.53)* | 2.5 (1.92) | 2.9 (1.91) | ||
| Marital status (married vs. unmarried) | −1.5 (1.29) | −1.3 (1.64) | ||||
| History of depression (yes vs. no) | −3.4 (1.90) | −2.9 (2.38) | ||||
| Type of stroke | ||||||
| Hemorrhagic vs. ischemic | 3.4 (1.89) | 7.7 (2.39)* | ||||
| Other vs. ischemic | −5.9 (2.12)* | −5.18 (2.69) | ||||
| Impairment group | ||||||
| Right vs. left | 0.8 (1.34) | −0.3 (1.69) | ||||
| Other vs. left | −1.5 (1.71) | −3.1 (2.16) | ||||
| Comorbidity (≥ 1 vs. none) | −2.9 (1.47)* | −3.2 (1.84) | ||||
| Pain (any vs. none) | −1.8 (1.91) | 0.7 (2.38) | ||||
| Length of stay (days) | −0.2 (0.07)* | −0.2 (0.09)* | ||||
| R-square (P-value) | 0.54 (< 0.01) | 0.57 (<0.01) | 0.59 (<0.01) | 0.39 (<0.01) | 0.40 (<0.01) | 0.43 (<0.01) |
adjusted for Total FIM score at discharge
adjusted for total FIM score at discharge, and age, education, sex, and race
adjusted for total FIM score at discharge, and age, education, sex, race, and marital status, history of depression, type of stroke, impairment group, comorbidity, pain, and length of stay
3-month Total FIM score for models 1–3: 106.8,105.7 & 105.4; 12-month Total FIM score for models 1–3: 108.9,108.8 & 108.2
p < 0.05
Parameter estimates were calculated separately for Motor and Cognition FIM at 3 and 12 months. In the fully adjusted model, those non-depressed at discharge who reported fewer symptoms at 3 months had Motor FIM scores that were 1.2 points greater than those non-depressed at discharge and reporting more depressive symptoms (p = 0.32), 4.7 points greater than depressed at discharge and reporting fewer depressive symptoms (p < 0.01), and 8.5 points greater than depressed at discharge and reporting more depressive symptoms (p < 0.01). At 12 months, the difference in Motor FIM between the non-depressed at discharge who reported fewer symptoms and the other three groups was 3.4 (p = 0.03), 6.8 (p < 0.01) and 14.1 (p < 0.01) points, respectively. In the fully adjusted model examining Cognition FIM at 3 months, the non-depressed at discharge who reported fewer symptoms had cognition scores that were 0.2 (p = 0.64), 1.4 (p < 0.01) and 3.4 (p < 0.01) points greater the other three groups. At 12 months, the difference was 0.3 (p = 0.59), 1.5 (p < 0.01) and 6.4 (p < 0.01) points.
DISCUSSION
The current study examined trends and change in depression status in persons aged 65 and older with a first time stroke. This information was used to determine associations with functional status over a 12 month follow up after discharge from in-patient medical rehabilitation. To increase the clinical applicability of our findings, we used ICD-9 codes to identify persons with stroke and prior history of depression. Our main findings can be summarized as follows. In accordance with the results of most prior studies,22–25 we showed rates of depression were greatest in the acute phases of recovery and declined over the subsequent 12 months. In an early study looking at trends in depression post stroke, Robinson et al.25 reported depression prevalence rates of 18.5% in a hospital or rehabilitation setting and 9.1% in a community setting. More recently, Aben et al.22 reported the highest rates of depression in the month following stroke with decreases over the next 12 months.
Although most patients recovered from their depression, a considerable minority reported more symptoms over the 12 month follow up and about a quarter of the sample neither consistently improved nor worsened, which underscores the dynamic nature of depression following stroke. When we tested for individual differences between those who recovered from their depression and those who did not, no statistically significant sociodemographic or clinical differences were found with the exception of race/ethnicity, education and marital status. It was unlikely that differences in depression status were due to variation in management of care across rehabilitation facilities. All facilities were JCAHO accredited (and all but one, CARF accredited) and mean Total FIM scores at discharge were similar across all eleven facilities. This finding indicates persons with stroke are potentially at risk for late on-set depression and suggest the need for continued and on-going mental health screenings among those initially classified as non-depressed.
In considering the effects of depression on functional status, we created a 4-level depression measure to examine change in function 3 and 12 months post discharge. Overall, those identified as non-depressed at discharge and reported fewer symptoms at follow up showed greater improvement in functional status than those in the other 3 groups. Previous reports on the depression-functional status association have been varied. Differences in findings may be due to factors including time to assessment, and definition and methods used to classify individuals as depressed. It may also reflect how persons with depression are followed. Past studies have classified individuals as either depressed or non-depressed. In the current study we focused on change in depressive symptoms, which allowed us to track individual patterns of change and examine associations with functional status. Functional status is clearly an important measure of post stroke recovery and provides clinicians with an objective means to track patient progress during hospitalization and post discharge. In persons with stroke, Granger et al.26 observed an inverse gradient of association, where each 1-point increase in Total FIM score decreased the need for assistance from another person to complete basic activities of daily living by about 2.2 min. Carter et al.16 recently reported that an average increase of 1 FIM point was associated with a 3% reduction in the expected cost of inpatient rehabilitation care. Early recognition and management of depressive symptom change in persons with stroke represents an important challenge in the effort to improve health outcomes and facilitate functional independence.
Our analysis has some limitations. First, we did not have information on anti-depressant use post stroke. In a recent review of the literature, anti-depressant use post stroke ranged from 0% in the first weeks to 31% 2 years post-stroke.27 Second, although our data were collected across diverse geographic regions, patients were not randomly selected and may not be representative of all persons with stroke. Third, because interhospital variability exists in the type and quality of care delivered by medical rehabilitation providers, the selected facilities participating in this study may not reflect the rehabilitation experience at other facilities. Nevertheless, the study did include JCAHO- and CARF-accredited facilities, which set guidelines and standards. Strengths of the study included the large sample of persons from distinct regions with a first time stroke, the use of ICD-9 codes, and the collection of outcomes using reliable and widely respected instruments (e.g., CES-D).
In summary, our goal was to assess change in depression post stroke and examine its association with functional status. This goal is important in view of continued advances in medical technology, improved therapeutics, and changing demographics that have resulted in increased stroke prevalence due to an improved likelihood of stroke survival and a growing elderly population.28, 29 Our findings provide a baseline with which to compare future patterns and change in depression with other outcomes important to health care professionals, researchers, and stroke survivors. The value of collecting information on depression and symptoms of depression post stroke is that it not only assesses what the person may feel about their current health status, but it may also predict whether these individuals seek on-going treatment or therapy, or perhaps more importantly, whether they consider themselves to be successfully coping with their stroke and related functional limitations.
Acknowledgments
Sponsor’s Role: The funding organizations had no role no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Funding sources: This research was supported by funding from the National Institutes of Health and the National Institute of Aging for G. Ostir (R01-AG024806 & K01-HD046682), and National Center for Medical Rehabilitation Research for I. Berges (R03-HDO05821-01).
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions:
Ostir - study concept and design, acquisition of subjects, data, analysis, interpretation of data, and preparation of manuscript
Berges - interpretation of data and preparation of manuscript
Ottenbacher A. - data, analysis and interpretation
Ottenbacher K. - data, analysis, interpretation and preparation of manuscript
Dr. Ostir had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Hackett ML, Yapa C, Parag V, et al. Frequency of depression after stroke: A systematic review of observational studies. Stroke. 2005;36:1330–1340. doi: 10.1161/01.STR.0000165928.19135.35. [DOI] [PubMed] [Google Scholar]
- 2.Burvill PW, Johnson GA, Jamrozik KD, et al. Prevalence of depression after stroke: The Perth Community Stroke Study. Br J Psychiatry. 1995;166:320–327. doi: 10.1192/bjp.166.3.320. [DOI] [PubMed] [Google Scholar]
- 3.Herrmann N, Black SE, Lawrence J, et al. The Sunnybrook Stroke Study: A prospective study of depressive symptoms and functional outcome. Stroke. 1998;29:618–624. doi: 10.1161/01.str.29.3.618. [DOI] [PubMed] [Google Scholar]
- 4.Robinson RG. Poststroke depression: Prevalence, diagnosis, treatment, and disease progression. Biol Psychiatry. 2003;54:376–387. doi: 10.1016/s0006-3223(03)00423-2. [DOI] [PubMed] [Google Scholar]
- 5.Chemerinski E, Robinson RG, Kosier JT. Improved recovery in activities of daily living associated with remission of poststroke depression. Stroke. 2001;32:113–117. doi: 10.1161/01.str.32.1.113. [DOI] [PubMed] [Google Scholar]
- 6.Robinson RG, Murata Y, Shimoda K. Dimensions of social impairment and their effect on depression and recovery following stroke. Int Psychogeriatr. 1999;11:375–384. doi: 10.1017/s1041610299005992. [DOI] [PubMed] [Google Scholar]
- 7.Andersen G, Vestergaard K, Riis JO, et al. Dementia of depression or depression of dementia in stroke? Acta Psychiatr Scand. 1996;94:272–278. doi: 10.1111/j.1600-0447.1996.tb09860.x. [DOI] [PubMed] [Google Scholar]
- 8.Verdelho A, Henon H, Lebert F, et al. Depressive symptoms after stroke and relationship with dementia: A three-year follow-up study. Neurology. 2004;62:905–911. doi: 10.1212/01.wnl.0000115107.66957.8c. [DOI] [PubMed] [Google Scholar]
- 9.Smith PM, Illig SB, Fiedler RC, et al. Intermodal agreement of follow-up telephone functional assessment using the Functional Independence Measure in patients with stroke. Arch Phys Med Rehabil. 1996;77:431–435. doi: 10.1016/s0003-9993(96)90029-5. [DOI] [PubMed] [Google Scholar]
- 10.Segal ME, Gillard M, Schall RR. Telephone and in-[erson proxy agreement between stroke patients and caregivers for the functional independence measure 1. Am J Phys Med Rehabil. 1996;75:208–212. doi: 10.1097/00002060-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 12.McDowell I, Newell C. Measuring Health: A Guide to Rating Scales and Questionnaires. 2. New York: Oxford University Press; 1996. [Google Scholar]
- 13.Miller TQ, Markides KS, Black SA. The factor structure of the CES-D in two surveys of elderly Mexican Americans. J Gerontol B Psychol Sci Soc Sci. 1997;52B:S259–S269. doi: 10.1093/geronb/52b.5.s259. [DOI] [PubMed] [Google Scholar]
- 14.Roberts RE. Reliability of the CES-D Scale in different ethnic contexts. Psychiatry Res. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- 15.Watson LC, Pignone MP. Screening accuracy for late-life depression in primary care: A systematic review. J Fam Pract. 2003;52:956–964. [PubMed] [Google Scholar]
- 16.Carter GM, Relles DA, Buchanan JL, et al. Project memo (Final 31 Aug 95–3 Jul 97) Santa Monica, CA: RAND Corp; 1997. A classification system for inpatient rehabilitation patients: A review and proposed revisions to the Functional Independence Measure-Function Related Groups. (NTIS Order Number PB98-105992.) [Google Scholar]
- 17.Stineman MG, Hamilton BB, Granger CV, et al. Four methods for characterizing disability in the formation of function related groups. Arch Phys Med Rehabil. 1994;75:1277–1283. [PubMed] [Google Scholar]
- 18.Stineman MG, Escarce JJ, Goin JE, et al. A case-mix classification system for medical rehabilitation. Med Care. 1994;32:366–379. doi: 10.1097/00005650-199404000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Ottenbacher KJ, Hsu Y, Granger CV, et al. The reliability of the functional independence measure: A quantitative review. Arch Phys Med Rehabil. 1996;77:1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton BB, Laughlin JA, Fiedler RC, et al. Interrater reliability of the 7-level functional independence measure (FIM) Scand J Rehabil Med. 1994;26:115–119. [PubMed] [Google Scholar]
- 21.Sands LP, Landefeld CS, Ayers SM, et al. Disparities between black and white patients in functional improvement after hospitalization for an acute illness. J Am Geriatr Soc. 2005;53:1811–1816. doi: 10.1111/j.1532-5415.2005.53517.x. [DOI] [PubMed] [Google Scholar]
- 22.Aben I, Verhey F, Strik J, et al. A comparative study into the one year cumulative incidence of depression after stroke and myocardial infarction. J Neurol Neurosurg Psychiatry. 2003;74:581–585. doi: 10.1136/jnnp.74.5.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andersen G, Vestergaard K, Ingemann-Nielsen M, et al. Risk factors for post-stroke depression. Acta Psychiatr Scand. 1995;92:193–198. doi: 10.1111/j.1600-0447.1995.tb09567.x. [DOI] [PubMed] [Google Scholar]
- 24.Morrison V, Pollard B, Johnston M, et al. Anxiety and depression 3 years following stroke: Demographic, clinical, and psychological predictors. J Psychosom Res. 2005;59:209–213. doi: 10.1016/j.jpsychores.2005.02.019. [DOI] [PubMed] [Google Scholar]
- 25.Robinson RG, Starr LB, Kubos KL, et al. A two-year longitudinal study of post-stroke mood disorders: Findings during the initial evaluation. Stroke. 1983;14:736–741. doi: 10.1161/01.str.14.5.736. [DOI] [PubMed] [Google Scholar]
- 26.Granger CV, Cotter AC, Hamilton BB, et al. Functional assessment scales: A study of persons after stroke. Arch Phys Med Rehabil. 1993;74:133–138. [PubMed] [Google Scholar]
- 27.Hackett ML, Anderson CS, House A, et al. Interventions for treating depression after stroke. Cochrane Database Syst Rev. 2008:CD003437. doi: 10.1002/14651858.CD003437.pub3. [DOI] [PubMed] [Google Scholar]
- 28.American Heart Association. Heart Disease and Stroke Statistics- 2007 Update. Dallas, Texas: American Heart Association; 2007. [Google Scholar]
- 29.Kelly PJ, Stein J, Shafqat S, et al. Functional recovery after rehabilitation for cerebellar stroke. Stroke. 2001;32:530–534. doi: 10.1161/01.str.32.2.530. [DOI] [PubMed] [Google Scholar]