Abstract
Background
In a pilot study, two-dimensional (2-D) CT assessment of posterior wall fracture fragments predicted hip stability with small fracture fragments and instability for large fracture fragments.
Questions/purposes
To confirm the previous findings, we determined whether there is sufficient observer consistency and accuracy to predict hip stability in posterior wall acetabular fractures for this CT assessment method and assessed its ease of clinical use.
Methods
We selected 10 fractures having variable characteristics with known clinical outcome and created three study participant groups, based on level of training, for evaluation. Each observer reviewed the CT scans from the 10 fractures and applied the method in two separate sessions, the second after at least a 1-month washout period.
Results
Participants reported subjective ease in using the method, averaging 5 minutes (range, 3–11 minutes) for each assessment. Intraobserver and interobserver reliability were both greater than 0.80 regardless of the level of experience. Although sensitivity was 90%, specificity was only 61% after comparison with examination under anesthesia (EUA). Inappropriate nonoperative treatment would have occurred in 6% of cases and inappropriate operative treatment in 16%.
Conclusions
This method for assessing hip instability is reliable, reproducible, and easy to learn and use. However, as a diagnostic tool in the clinical setting, it is useful only for fractures involving greater than 50% of the posterior wall owing to limited accuracy. For fractures less than 50%, EUA should be performed to determine hip stability.
Introduction
Posterior wall fractures are common and comprise approximately 25% of all acetabulum fractures [9]. These fractures may be treated nonoperatively if there is a congruous and stable hip [16, 20]. After initial successful closed reduction confirmed by plain radiographs in the emergent setting, 2-D CT is obtained for a more detailed evaluation of morphologic features of the fracture [3, 5, 6, 8, 11, 16]. Studies using 2-D CT-derived-criteria indicate, in general, posterior wall fractures involving less than 20% of the posterior wall are stable and able to withstand physiologic loads, whereas those involving greater than 40% to 50% are unstable, leaving a wide range of posterior wall fractures classified as indeterminate [3, 5, 13]. Therefore, the radiographic findings of subluxation of the hip or involvement greater than 50% of the posterior wall seen on CT are signs of hip instability and indications for operative repair [2, 3, 5, 13, 21].
Examination of the hip by dynamic stress fluoroscopic imaging obtained with the patient under general anesthesia (EUA) has been used as a clinical measure of dynamic stability and congruence of the hip and advocated to assess the need for operative treatment [13–17, 19–21]. Posterior subluxation, as evidenced by a widening medial clear space or loss of joint parallelism, is indicative of dynamic hip instability [2, 5, 13–15, 17–21], and EUA is considered the gold standard for diagnosis of dynamic hip stability status [4, 13, 18, 19]. However, EUA has not attained general clinical use status, and CT assessment of fragment size and position is thought to be able to identify clinically unstable hips requiring operative fixation [3, 5, 13].
Several investigators have described measurement methods based on 2-D CT to calculate a percentage of posterior wall involvement [3, 5, 13]. Moed et al. [13] recently reported a method that uses aspects of previous techniques. This method provides a percentage of maximal posterior wall involvement, with fractures involving less than 20% considered stable, fractures involving greater than 50% unstable, and the remaining 20% to 50% indeterminate [13]. As opposed to the other methods, the high specificity, sensitivity, and positive predictive value of the method described by Moed et al. [13] make it a superior assessment tool to aid in preoperative evaluation of these injuries. However, the evaluations were obtained only by one observer [13]. Therefore, the important considerations of interobserver and intraobserver variability have not been determined [13]. In addition, Moed et al. [13] commented on the potential difficulties in the technical aspects of making the CT measurements. Therefore, the teachability and potential for clinical application have not been assessed.
We therefore determined whether there is sufficient observer consistency to predict hip stability status in posterior wall acetabular fractures for this method and assessed its ease of clinical use. Specifically we examined the (1) ease of use; (2) observer reliability; (3) sensitivity and specificity compared with EUA with risk of incorrect predictions; and (4) potential errors in measurement.
Materials and Methods
We selected 10 patients with displaced posterior wall fractures having varying fracture characteristics and known hip stability status. These patients with isolated unilateral posterior wall (OTA 62-A1) [10] acetabular fractures had undergone dynamic stress fluoroscopy EUA to determine hip stability as described by Grimshaw and Moed [4] and Moed et al. [13]. The use of EUA identified four stable hips and six unstable hips. The mean patient age at the time of injury was 25.5 years (range, 17–53 years). All patients were male and nine of the 10 had a right-sided injury. The patients having the four stable hips had been treated nonoperatively and followed for a minimum of 2 years, showing excellent radiographic appearance and clinical function to verify the EUA-determined stable diagnosis. The six unstable hips were treated by open reduction and internal fixation.
All fractures involved the posterior wall. However, one had a slightly oblique fracture orientation with a posterosuperior location (Fig. 1), and three had associated nondisplaced transverse fractures, visible as a completely nondisplaced fracture line on the CT sections, one of which involved less than 2 mm of marginal impaction of the posterior wall. This variability in morphologic features of the fracture, which was not addressed in the study by Moed et al. [13], was selected to better approximate the clinical setting. The fracture with the marginal impaction was determined by EUA to be stable and the other three were unstable. The posterosuperior fracture with the oblique orientation was selected to evaluate this fracture type, which is thought to be at increased risk for hip instability regardless of fracture size [7]. To otherwise eliminate the indeterminate group from the classification of the system described by Moed et al. [13] as a potential confounding variable, one of us (BRM) screened the fractures to include only those predicted to be stable (involving less than 20% of the posterior wall) or unstable (involving greater than 50%) by this CT method. Therefore, all four EUA-determined stable fractures were thought to involve less than 20% of the posterior wall and five of the six EUA-determined unstable fractures were thought to involve greater than 50% of the posterior wall. The posterosuperior fracture was thought to involve less than 20% of the wall by our screening measurement.
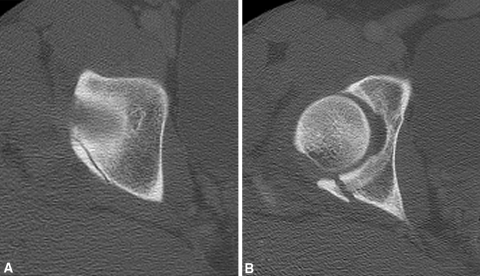
Fig. 1A–B.
Selected axial CT sections of a wall fracture having an oblique orientation and a posterosuperior location show (A) the superior extent and oblique orientation of the fracture and (B) the level of the greatest size of the posterior wall fracture fragment.
Three study participant observer groups were created for comparison based on level of training. These included an attending level (three traumatologists who perform acetabular fixation), a senior resident level (three Postgraduate Year 5 residents), and a junior resident level (three Postgraduate Year 2 residents). Each participant reviewed the 10 CT scans (Round 1) and applied the measurement method described by Moed et al. [13]. The CT images were reviewed for a second time after at least a 1-month washout period to assess intraobserver reliability (Round 2). The 10 fractures with nine observers and two rounds provided 180 predictions, which were predetermined to be more than adequate for statistical analysis.
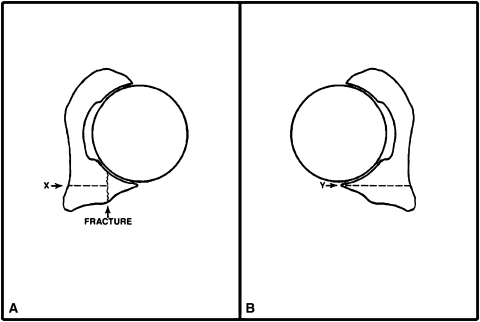
As noted previously, the method of CT assessment of hip stability described by Moed et al. [13] provides a percentage of posterior wall involvement and suggests that hip stability status can be predicted: fractures involving less than 20% are predicted to be stable, fractures involving greater than 50% are considered unstable, and the remaining 20% to 50% are of indeterminate stability. For this system, the observer must identify the largest percentage of posterior wall fracture involvement. A ratio is made comparing the size of the fracture fragment to the intact contralateral wall depth at an equivalent axial cut level. Performing accurate measurements may be complicated by fracture fragment comminution, translation, and displacement. For this reason a subtraction method is used to determine the true fracture fragment size (Fig. 2). The observer must repeat measurements at multiple CT image section levels to ensure that the greatest percentage of posterior wall fracture involvement is identified, which then is used to determine the hip stability classification.
Fig. 2A–B.
The diagrams illustrate the measurement method. (A) The approximate mediolateral dimension (depth) of the smallest remaining intact posterior wall measured to the medial extent of the quadrilateral plate (X) is determined at the level of the greatest size of the posterior wall fracture fragment. (B) The percentage of fragment size is calculated from the ratio of the estimated depth of the fractured segment to the intact matched contralateral acetabular depth measured to the medial extent of the quadrilateral plate (Y) at a level comparable to that used for measurement of the fracture fragment. Y − X divided by Y multiplied by 100 provides the percentage. (Modified and reprinted with permission from Moed BR, Ajibade DA, Israel H. Computed tomography as a predictor of hip stability status in posterior wall fractures of the acetabulum. J Orthop Trauma. 2009;23:7–15.)
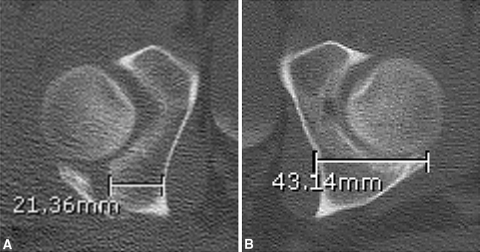
Before reviewing the CT studies, each participant was provided with a copy of the article by Moed et al. [13], which explains and illustrates the measurement technique. In addition, each participant was taken through a case example (Fig. 3) using our institution’s digital CT software. All CT scans were obtained using a General Electric LightSpeed Plus (General Electric Corp, Waukesha, WI, USA) with 2.5-mm slice thickness. Measurements where made using the integrated ruler function in the Synapse® PACS system (FUJIFILM Medical Systems USA, Inc, Stamford, CT, USA). Accordingly, the participants were asked to classify each hip as stable, indeterminate, or unstable. The understanding was that a classification of stable would be an indication for nonoperative treatment and that a classification of either indeterminate or unstable would be an indication for open reduction and internal fixation. The participants were not told how many fractures were stable or unstable as determined by EUA. They also were not told the fractures were thought either to involve less than 20% of the posterior wall or to involve greater than 50% of the posterior wall.
Fig. 3A–B.
A clinical example of the measurement method is shown. (A) Measurement of the smallest remaining intact posterior wall is 21.36 mm and (B) the contralateral equivalent uninjured wall measurement is 43.14 mm. This was confirmed by tracing an overlay. This calculation is performed for measures obtained at multiple levels to ensure the largest percentage of wall involvement is obtained. The calculation is completed as follows: percent wall involvement = {(43.14 − 21.36)/(43.14)} × 100 = 50.5%, indicating “unstable.” This CT example was used as part of the participant instructions and was not one of the 10 cases used in the study.
Teachability and ease of clinical use were assessed through recording of the time required for completing each prediction, rounded up to the nearest minute, and having the participants answer a two-question survey at the completion of the study. These two questions, which were skewed toward obtaining an adverse response to the technique, were graded on a 7-point Likert scale (Appendix 1).
Participant measurements, level of training, and time for completion were recorded and evaluated. Interobserver and intraobserver reliability were assessed by using an interclass correlation coefficient (ICC) reported as a measure from 0 to 1, with 0 representing no agreement and 1 being perfect agreement [1]. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated by defining a stable hip (nonoperative treatment) as the healthy state and an unstable (or indeterminate) hip (operative treatment) as the unhealthy state. All statistical analyses were performed using SPSS® 15.0 software (SPSS Inc, Chicago, IL, USA).
Results
All study participants reported subjective ease in learning and using the CT measurement method. All participants responded that they either strongly disagreed or disagreed with each of the two survey statements (Appendix 1). Time to complete each hip stability assessment averaged 5 minutes (range, 3–11 minutes) and there were no differences within or among (p > 0.8) the participant groups.
The interobserver reliability scores revealed this classification system to be reliable for users at all experience levels, with an overall interobserver reliability of 0.90. The classification system also was reproducible, with an overall intraobserver reliability of 0.94. There were no differences in interobserver or intraobserver reliability as a function of experience level (Table 1).
Table 1.
Interobserver and intraobserver reliability as a measure of experience level
| Experience level | Interclass correlation coefficient | |
|---|---|---|
| Intraobserver | Interobserver | |
| Junior | 0.91 | 0.94 |
| Senior | 0.96 | 0.94 |
| Attending | 0.93 | 0.83 |
| Overall | 0.94 | 0.90 |
Of the total of 180 predictions, there were 12 incorrect stable versus unstable predictions. Eleven of these were predictions of stability for unstable hips as determined by EUA. There was only one prediction of instability for a stable hip as determined by EUA. Indeterminate predictions comprised 47 of the 180 total possible predictions. There were 27 indeterminate predictions for stable hips as determined by EUA. The remaining 20 indeterminate predictions were for unstable hips as determined by EUA. Overall, these predictions would have resulted in a recommendation for inappropriate nonoperative treatment in 6% (11/180) of cases and a recommendation for inappropriate operative treatment in 16% (28/180). Therefore, overall as compared with EUA, the participant’s ability to use their CT predictions to determine appropriate treatment had a sensitivity of 90% and specificity of only 61%. Positive predictive value was 78% and negative predictive value was 80%. By excluding the indeterminate interpretations (as would be the situation if this method were used as a screening method to select only those with these indeterminate interpretations for EUA), the predictions were differentially affected. The recommendation for inappropriate operative treatment decreased to less than 1% (1/133). However, the recommendation for inappropriate nonoperative treatment increased to 8% (11/133).
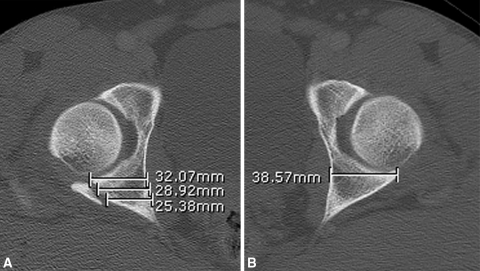
Examination of the individual responses revealed that potentially clinically important errors made by the participants were limited to the four posterior wall fractures having special features. The fracture that included a nondisplaced transverse fracture and a posterior wall with less than 2 mm of marginal impaction was stable by EUA but was predicted to be either unstable or indeterminate by all participants. For the two additional fractures that had a nondisplaced transverse component, which were unstable by EUA, one participant interpreted one to be stable in Round 1 and both to be stable in Round 2. All other participants classified these fractures as unstable. For the one posterosuperior wall fracture with an oblique fracture line, which was unstable by EUA, four of the nine participants predicted the hip to be stable in both rounds. All remaining participants interpreted the CT as indeterminate (Fig. 4).
Fig. 4A–B.
The images show the potential measurement variabilty for the posterosuperior wall fracture with an oblique orientation shown in Fig. 1. Depending on the selected position for measurement, (A) the three different measurements shown (B) when compared with the uninjured contralateral hip indicate 17%, 25%, or 34% posterior wall involvement, which would correspond to a stable or an indeterminate prediction. The hip was unstable by EUA.
Discussion
Some investigators have described methods of predicting hip stability based on the size of the posterior wall fracture fragment as determined by 2-D CT [3, 4, 12, 20]. Moed et al. [13] recently compared hip stability status predictions using the method described by Calkins et al. [3], the method described by Keith et al. [5], and an alternative method [13]. The alternative method showed improved results, 100% positive predictive value, and zero incorrect predictions when compared with EUA and was the only reliable technique predictive of hip stability for small fracture fragments and instability for large fracture fragments [13]. However, that study did not evaluate the interobserver and intraobserver variability, the ease of the method’s clinical use, or potential areas for measurement errors. Consequently, the authors cautioned against the use of this CT technique as the sole screening tool for determination of hip stability status, instead recommending the use of EUA [13]. Therefore, in the current study we sought to determine ease of use, and whether there is sufficient observer consistency and accuracy to predict hip stability in posterior wall acetabular fractures for this CT assessment method.
We acknowledge limitations to our study. First, the entire range of posterior wall fracture geometry could not possibly be included. However, we included a broad representative sample of fractures including variables that commonly would be seen in the clinical setting, such as marginal impaction, an oblique fracture line and an associated nondisplaced transverse fracture line. Second, our series included only 10 posterior wall fracture CT scans. Although a larger number of cases would have enlarged the data set, it is doubtful that it would have altered the results or improved the study. The 10 fractures with nine observers and two rounds provided 180 predictions, which were predetermined to be more than adequate for statistical analysis, including the calculation of ICC [1]. Third, there is a possibility that the method was applied incorrectly by one or more of the participants. We believe we avoided this problem by providing a copy of the original article describing the method [13] and providing individual instruction using a separate case example outlining the method step by step (Fig. 3). Fourth, associated hip dislocation, a variable thought to indicate hip instability, was not addressed in this study. However, none of the previous investigators has considered hip dislocation as part of the CT evaluation protocol. In addition, associated hip dislocation is reportedly not an important risk factor for residual instability of the hip [4].
Our findings suggest orthopaedic clinicians at all levels of training can quickly, easily, and reliably accomplish the task. The participants universally reported they would not have any difficulty using this technique in their clinical practice. We found no comparable data evaluating the physician’s ability to use the published CT methods for assessing hip stability.
We found no differences with respect to level of training and all coefficients were greater than 0.80 (Table 1). For an evaluation of this type, these results indicate a high degree of consistency in the observations [1]. Therefore, our findings indicate that the method described by Moed et al. [13] provides consistent data. Again, we found no published data evaluating the intraobserver and interobserver reliability for any of the published CT methods for assessing hip stability.
Our evaluation of sensitivity and specificity compared with EUA along with the risk of incorrect predictions identified a problem with clinical application of this CT assessment tool. Inappropriate operative (16% of cases) and nonoperative (6% of cases) treatments have error rates too great to recommend its unlimited clinical use. One could argue that unnecessary surgery on a posterior wall fracture should still result in good hip function, similar to that described for open reduction and internal fixation of any posterior wall fracture [9, 14–17]. However, this surgery is not without risks [12]. Perhaps more importantly, an incorrect prediction of stability and subsequent nonoperative treatment for an actually unstable hip would likely lead to recurrent subluxation or frank dislocation and poor hip function associated with early arthritic changes. Eliminating stable and indeterminate findings from consideration, and thereby limiting this CT method to screen only for those injuries defined as unstable (fracture fragment > 50%), is the only situation (with < 1% incorrect predictions) in which this technique can be applied reasonably to the clinical setting.
We attempted to evaluate potential errors in measurement, another aspect of CT assessment that previously has not been evaluated. Our examination of the individual responses revealed that the clinically important errors made by the participants were limited to four posterior wall fractures having special features commonly found in fractures of the posterior wall of the acetabulum [12, 14, 17]. It generally has been thought posterior wall fractures with a more superior location pose such a risk, as such fractures involving less than 20% of the articular surface may be unstable. The posterosuperior fracture in this study illustrates this point. Nondisplaced transverse fracture lines and the presence of a marginally impacted fragment appeared to adversely affect the observers’ accuracy. Although in this method the observer is instructed to discount these nondisplaced fracture lines, one of the observers produced a measurement smaller than the actual posterior wall involvement, yielding a smaller percentage and an incorrect prediction of hip stability status. Therefore, these fracture lines make it difficult to determine the actual posterior wall involvement for measurement purposes. However, as previously noted, these secondary fracture lines commonly occur in the clinical setting.
This CT method for assessing hip instability is reliable, reproducible, and easy to learn and use, which would seem to support its general use as an appropriate screening tool for hip stability status. However, this technique of using a static 2-D tool to evaluate a dynamic 3-D structure is too inaccurate to be used clinically. We believe EUA should remain the gold standard in determining dynamic hip stability status after posterior wall fractures [4]. CT nonetheless can serve a limited role as a diagnostic tool in the clinical setting, being useful to determine as unstable only those fractures found to involve greater than 50% of the posterior wall. Fractures involving less than 50% of the posterior wall require EUA to determine hip stability status.
Acknowledgments
We thank Heidi Israel PhD for assistance with the statistical analysis. We thank John A. Boudreau MD, Cody B. Bellard MD, Jaret M. Butler MD, Lisa K. Cannada MD, Jason D. Cobb MD, James M. Jackman DO, Jessica C. McMichael MD, Christopher D. Mudd MD, and Kevin J. Quigley MD for reading the CT scans.
Appendix
Appendix 1. Posttest questionnaire
Instructions: Using the following 7-point scale, please place the number on the blank before each item that best describes how much you agree with each statement.
Strongly Disagree
Disagree
Slightly Disagree
Neutral
Slightly Agree
Agree
Strongly Agree
_________ 1. It was very difficult to master this technique of CT assessment of posterior wall fracture fragment size as a predictor of hip stability status.
_________ 2. I would have difficulty using this technique in the clinical situation.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Altman DG. Practical Statistics for Medical Research. New York, NY: Chapman and Hall; 1991. [Google Scholar]
- 2.Baumgaertner MR. Fractures of the posterior wall of the acetabulum. J Am Acad Orthop Surg. 1999;7:54–65. doi: 10.5435/00124635-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Calkins MS, Zych G, Latta L, Borja FJ, Mnaymneh W. Computed tomography evaluation of stability in posterior fracture dislocation of the hip. Clin Orthop Relat Res. 1988;227:152–163. [PubMed] [Google Scholar]
- 4.Grimshaw CS. Moed BR: Outcome of posterior wall fractures of the acetabulum treated nonoperatively after diagnostic screening with dynamic stress examination under anesthesia. J Bone Joint Surg Am. 2010;92:2792–2800. doi: 10.2106/JBJS.J.00112. [DOI] [PubMed] [Google Scholar]
- 5.Keith JE, Jr, Brashear HR, Jr, Guilford WB. Stability of posterior fracture-dislocations of the hip: quantitative assessment using computed tomography. J Bone Joint Surg Am. 1988;70:711–714. [PubMed] [Google Scholar]
- 6.Kellam JF, Messer A. Evaluation of the role of coronal and sagittal axial CT scan reconstructions for the imaging of acetabular fractures. Clin Orthop Relat Res. 1994;305:152–159. doi: 10.1097/00003086-199408000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Kregor PJ, Stover M. Acetabular fractures. In: Stannard JP, Schmidt AH, Kregor PJ, editors. Surgical Treatment of Orthopaedic Trauma. New York, NY: Thieme; 2007. pp. 470–521. [Google Scholar]
- 8.Lang JE, Cothran RL, Pietrobon R, Olson SA. Observer variability in assessing articular surface displacement in acetabular fractures using a standardized measurement technique. J Surg Orthop Adv. 2009;18:9–12. [PubMed] [Google Scholar]
- 9.Letournel E, Judet R. Fractures of the Acetabulum. New York, NY: Springer; 1993. [Google Scholar]
- 10.Marsh JL, Slongo TF, Agel J, Broderick SJ, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 11.Martinez CR, Di Pasquale TG, Helfet DL, Graham AW, Sanders RW, Ray LD. Evaluation of acetabular fractures with two- and three-dimensional CT. Radiographics. 1992;12:227–242. doi: 10.1148/radiographics.12.2.1561413. [DOI] [PubMed] [Google Scholar]
- 12.Moed BR: Posterior Wall Acetabular Fractures: Diagnosis, Treatment, and Results. American Academy of Orthopaedic Surgeons: Orthopaedic Knowledge Online. Available at: http://www5.aaos.org/oko/description.cfm?topic=TRA026. Accessed February 23, 2009.
- 13.Moed BR, Ajibade DA, Israel H. Computed tomography as a predictor of hip stability status in posterior wall fractures of the acetabulum. J Orthop Trauma. 2009;23:7–15. doi: 10.1097/BOT.0b013e31818f9a5c. [DOI] [PubMed] [Google Scholar]
- 14.Moed BR, Carr SE, Gruson KI, Watson JT, Craig JG. Computed tomographic assessment of fractures of the posterior wall of the acetabulum after operative treatment. J Bone Joint Surg Am. 2003;85:512–522. doi: 10.2106/00004623-200303000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Moed BR, Carr SE, Watson JT. Open reduction and internal fixation of posterior wall fractures of the acetabulum. Clin Orthop Relat Res. 2000;377:57–67. doi: 10.1097/00003086-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Moed BR, Spoonamore MJ. Management of acetabular fractures. In: Bulstrode C, Buckwalter JA, Carr A, Fairbank J, Marsh L, Wilson-MacDonald J, Bowden G, eds. Oxford Textbook of Orthopedics and Trauma. Oxford, UK: Oxford University Press; 2002:2182–2201.
- 17.Moed BR, WillsonCarr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002;84:752–758. doi: 10.2106/00004623-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Starr AS, Moed BR. Acetabular fractures: definitive treatment and expected outcomes. In: Baumgaertner MR, Tornetta P 3rd, editors. OKU Trauma 3. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2005. pp. 271–280. [Google Scholar]
- 19.Tornetta P., 3rd Non-operative management of acetabular fractures: the use of dynamic stress views. J Bone Joint Surg Br. 1999;81:67–70. doi: 10.1302/0301-620X.81B1.8805. [DOI] [PubMed] [Google Scholar]
- 20.Tornetta P., 3rd Displaced acetabular fractures: indications for operative and nonoperative management. J Am Acad Orthop Surg. 2001;9:18–28. doi: 10.5435/00124635-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Vailas JC, Hurwitz S, Wiesel SW. Posterior acetabular fracture-dislocations: fragment size, joint capsule, and stability. J Trauma. 1989;29:1494–1496. doi: 10.1097/00005373-198911000-00007. [DOI] [PubMed] [Google Scholar]