Abstract
Aim:
Garlic is available as an over-the-counter herbal supplement and is known to have antiplatelet properties. Because of scarcity of clinical data regarding the safety of concomitant use of garlic supplements and anticoagulants, we tried to evaluate the effects of coadministration of single and multiple doses of garlic and cilostazol on platelet aggregation.
Materials and Methods:
The study was a randomized, open label, placebo-controlled, crossover study of type II diabetic patients, where 14 patients were enrolled and 10 completed the study. The patients were administered 600 mg aged garlic extract, 100 mg cilostazol, 600 mg aged garlic extract, and cilostazol or placebo for seven days as per prior randomization schedule. Blood samples for platelet aggregation and bleeding time and clotting time were collected before and 2, 4, and 6 hours after single-dose drug administration and after seven days of treatment.
Results:
After single- and multiple-dose administration of garlic, there was a significant inhibition of platelet aggregation at 2 hours, whereas with cilostazol, the inhibition was significant at all the three time points tested, with 4 hours showing maximum inhibition. Coadministration of garlic and cilostazol in single and multiple doses for seven days did not produce any significant change in the antiplatelet activity of the individual drugs.
Conclusions:
Coadministration of aged garlic extract and cilostazol did not enhance the antiplatelet activity compared with individual drugs. Large randomized trials are needed to further evaluate the possible interaction of garlic in higher doses and in combination with other antiplatelet activity drugs.
Keywords: Cilostazol, garlic, platelet aggregation
Introduction
In recent years, there has been resurgence in the use of herbal therapies, and they are becoming increasingly popular in general population. Millions of people today use herbal therapies along with prescription and nonprescription medications. The size of the worldwide market of herbal medicines is estimated to be around US$100 billion and this market is expected to reach US$2 500 billion by the year 2010. These products are available to consumers as over-the-counter items in various forms of preparations and doses.[1] Several factors contribute to the increased use of herbal products: namely, easy accessibility, perception of herbs as safe alternate treatment, desire for self medication, and lesser cost.
Recently, with increasing use of herbal drugs, there have been concerns regarding the safety of these products, in particular the potential interaction of these drugs with conventional drugs. Certain herbal supplements can cause potentially dangerous side effects when taken with prescription drugs. The use of alternative therapy is mostly not supervised by practitioners resulting in increased harm to the patients, especially if they are using herbal and prescription medicines that have latent interactions. These interactions can go unnoticed until a patient is hurt or a serious life-threatening event has occurred. It has been documented that as many as 31% of patients use herbal supplements concurrently with the prescribed conventional drugs, and 70% of them do not report the use of these products to their healthcare providers.[1] Despite the widespread use of herbal drugs, documented herb-drug interactions are sparse. Knowledge of at least commonly occurring or anticipated interactions between herbal supplements and conventional drugs are need of the hour.
Cilostazol is a type III phosphodiesterase inhibitor used for the management of peripheral arterial disease (PAD). It is an antithrombotic agent that inhibits platelet aggregation and increased vasodilatation; the antiplatelet activity of cilostazol is 10 to 30 times more potent than aspirin.[2] Patients with type 2 diabetes are at risk of or have PAD associated with dyslipidemia and are known to take the medications for the same.
Garlic is a commonly used herbal medicine intended to lower cholesterol. It has antiplatelet activity and other pharmacological properties. The antiplatelet activity of garlic is well documented.[3,4] Diabetes mellitus is a major risk factor for cardiovascular disease. It mostly affects the microcirculation. Increased adhesion of platelets is known to potentiate thrombus formation in microcirculation. Cilostazol is indicated in peripheral vascular disease. Antiplatelet agents are commonly used prophylactically to prevent cardiovascular complications. There is a possibility that the diabetic patients may be using garlic as a herbal therapy along with the prescribed cilostazol. Thus, there is a possibility that concurrent use of garlic and cilostazol may potentiate the antiplatelet activity and may cause prolongation of bleeding time, hence increasing the risk of hemorrhage. The present study was conducted to evaluate the pharmacodynamic interactions of garlic with cilostazol, after single- and multiple-dose administration in diabetic patients. The primary objective of the study was to detect any significant change in platelet aggregation from baseline on administration of single and multiple doses of garlic, cilostazol, and their combination. More than 20% change in platelet aggregation from baseline was considered to be a positive response. Secondary objective was to detect any changes in coagulation and hemodynamic parameters.
Materials and Methods
The present study was conducted in the Department of Clinical Pharmacology and Therapeutics of Nizam's Institute of Medical Sciences, Hyderabad. The study was approved by the Institutional Ethics Committee and all the participants gave written informed consent before the start of any study-related procedures.
Study Design
It was a randomized open-label, placebo-controlled, crossover study. A total of 14 subjects were enrolled into the study and 10 completed the study. To avoid confounding factors known to affect antiplatelet activity, the following exclusion criteria were applied: severe uncontrolled hyperglycemia (HbA1C > 11%), uncontrolled hypertension, cardiac arrhythmia, congestive heart failure, evidence of hepatic and renal impairment or any other serious chronic disease requiring active treatment, subjects hypersensitive to the study drugs, chronic smokers or alcoholics, history of gastrointestinal surgery that could interfere with absorption of study drug, and treatment with any other herbal supplements, lipid-lowering drugs, and antiplatelet drugs in last 4 weeks. All the subjects were on stable dose of their antidiabetic medication for the past three months.
After an overnight fast and 12 hours after the last antidiabetic medication dose, subjects were randomized in a 4-way crossover design to receive either 600 mg of garlic, 100 mg of cilostazol, 600 mg garlic + 100 mg cilostazol, or placebo, once daily for 7 days as per the randomization table. Blood samples for platelet aggregation were taken immediately before (0 hours) and 2, 4, and 6 hours after the drug treatment on first day. Vital parameters were measured at 0 and 6 hours, and bleeding time was measured at 0, 2, 4, and 6 hours. Similarly, subjects were housed on day six and the same procedure as on day one was applied on day 7 also. Two weeks washout period was allowed between each treatment, after which they were crossed over to the other treatment arm as per the prior randomization schedule.
Measurement of platelet aggregation was done by using a dual-channel platelet aggregometer (Chronolog) by the turbidimetric method, using adenosine diphosphate (ADP) 10 μg. Nine milliliters of blood was collected from the antecubital vein in a polypropylene test tube containing 1 ml of sodium citrate. The aggregometer was switched on about 30 minutes before the test to allow the heating block to warm up to 37° C. Platelet-rich plasma (PRP) was prepared by centrifuging blood at 110 g for 15 minutes. Platelet-poor plasma was then prepared from the remaining blood by centrifuging at 2 400 g for 20 minutes. PRP (0.5 ml) was taken into a small cuvette and stir bar was added and placed in platelet aggregometer. The transmission was set to zero on the chart recorder. PRP was allowed to warm to 37° C for 2 minutes and then 2.5 μl of the platelet-aggregating solution containing 10 μmol of ADP was added. The change in absorbance was recorded until the response reached a plateau or for 6 minutes, whichever was earlier. Bleeding time was measured by Ivy's method.
Subjects were allowed to leave the department after 8 hours on each study day (Day 1 and Day 7), if there were no side effects. Any side effects reported were recorded on the case record form.
Statistical Analysis
Data are represented as mean ± standard deviation. Repeated measures of ANOVA, paired and unpaired t test were used to compare the effects of treatment within the group and between the groups. The level of significance was set at 0.05 with a power of 90%. Being a pilot study with cross-over design, 14 subjects were screened.
Results
In the present study, a total of 14 diabetic patients were screened over one month, of which three were excluded because of abnormal laboratory investigations. One patient left the study due to personal reasons; hence, 10 patients completed the study. The demographic details of all the patients are given in Table 1. All the patients had similar baseline characteristics, dose of antidiabetic drugs, and duration of diabetes mellitus. The results of inhibition in platelet aggregation with 10 μg ADP, after single dose of 600 mg of garlic, 100 mg of cilostazol, combination of 600 mg of garlic and 100 mg of cilostazol, and placebo are summarized in Table 2. At baseline, day 1 (0 hours), there was no significant difference in platelet aggregation in the four treatment groups. Single-dose administration of garlic produced a significant inhibition of platelet aggregation, which was maximum at 2 hours as compared with 4 and 6 hours (75.00 ± 18.36% at 0 hours vs 47.25 ± 11.23% at 2 hours, P<0.001; 56.25 ± 21.70% at 4 hours, P<0.01; and 65.00 ± 16.69 at 6 hours). Cilostazol when administered in a single dose showed significant inhibition of platelet aggregation at 2, 4, and 6 hours; however, the maximum inhibition was seen at 4 hours (72.25 ± 6.13% vs 40.25 ± 4.78%, P<0.001). Coadministration of garlic and cilostazol showed inhibition in platelet aggregation that was similar to those obtained with cilostazol alone. In placebo group, the platelet aggregation at 2, 4, and 6 hours was comparable with baseline [Figure 1a]. Further, when compared to baseline, there was no statistically significant change in bleeding time and other hemodynamic parameters with both the treatment arms.
Table 1.
Demographic details of all the patients
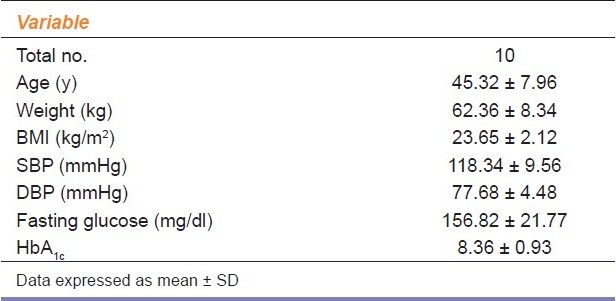
Table 2.
Maximum platelet aggregation percentage with adenosinediphosphate (10μmol) after single dose administration
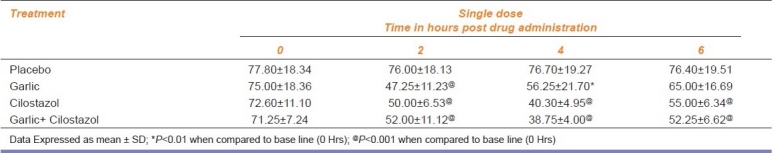
Figure 1a.
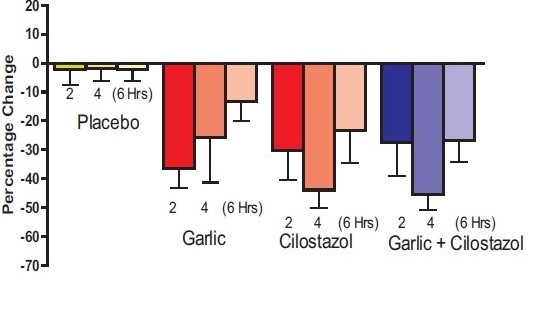
% age decrease in platelet aggregation (DAY-1) b: % age decrease in platelet aggregation (DAY-7)
Similarly, seven days of treatment with garlic produced maximum inhibition of platelet aggregation at 2 hours (83.00 ± 15.45% vs 56.80 ± 17.85%, P<0.001), the effect persisted at 4 hours also (83.00 ± 15.45% vs 66.80 ± 19.27%, P<0.01). However, the inhibition in platelet aggregation seen at 6 hours was not statistically significant. Cilostazol also showed a significant inhibition in platelet aggregation at 2, 4, and 6 hours, with maximum inhibition occurring at 4 hours when compared with baseline (78.33 ± 17.24% vs 45.33 ± 13.65%, P<0.001). Administration of garlic and cilostazol combination daily for seven days produced significant inhibition in platelet aggregation at all the time points, with maximum inhibition at 4 hours (75.20 ± 4.60% vs 42.80 ± 10.08%, P<0.001) [Table 3]. Similar to single-dose, multiple-dose treatment with combination did not produce any additive effect on platelet aggregation and data were comparable with that of cilostazol given alone [Figure 1b]. There was no significant change in bleeding time in any of the treatment arms. Furthermore, there was no significant change in any of the hemodynamic parameters evaluated.
Table 3.
Maximum platelet aggregation percentage with adenosine diphosphate (10μmol) after multiple dose administration
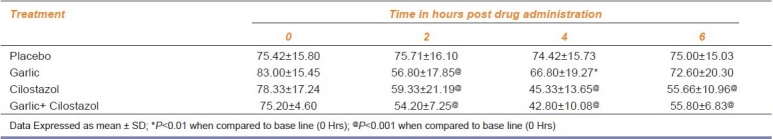
Figure 1b.
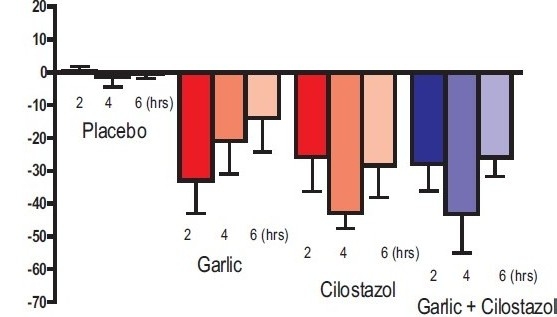
% age decrease in platelet aggregation (DAY-7)
Discussion
In the present study, we have evaluated the effects of administration of single and multiple doses of garlic and cilostazol alone and in combination on platelet aggregation. Both single-dose and multiple-dose administration of 600 mg of garlic produced significant inhibition of platelet aggregation induced by 10 μmol of ADP at 2 hours, and the effect sustained till 4 hours. Cilostazol has shown to inhibit platelet aggregation at all the three time points studied; however, the maximum inhibition was seen at 4 hours. Coadministration of garlic and cilostazol did not produce any significant change in platelet aggregation when compared with cilostazol alone.
There have been several reports of inhibition of platelet aggregation by garlic in healthy human male subjects.[3,5–7] Rahman and Billington conducted a 13-week study; the authors reported that dietary supplementation with 5 ml aged garlic extract/day significantly reduced the extent and rate of platelet aggregation at concentrations of ADP up to 10 μmol/l.[8] In another study conducted by Legnani et al., it was demonstrated that platelet aggregation induced by ADP and collagen was significantly inhibited by ingestion of garlic. The inhibition seen was significant at 2 and 4 hours after garlic ingestion, further platelet aggregation values were significantly lower after 7 and 14 days of garlic treatment.[3] In a study involving patients with increased risk of juvenile ischemic attack, Kiesewetter et al. demonstrated that daily ingestion of 800 mg of powdered (in the form of coated tablets) for 4 weeks led to a significant inhibition of the pathologically increased ratio of circulating platelet aggregates and of spontaneous aggregation. The ratio of circulating platelet aggregates decreased by 10.3% and spontaneous platelet aggregation by 56.3%.[4] Similarly, in our study with diabetic patients, significant inhibition of platelet aggregation was seen at 2 and 4 hours, with single and multiple doses. The results of our study are in accordance with these earlier reports. Several authors have demonstrated that garlic contains several chemical compounds that inhibit in vitro platelet aggregation,[9–11] such as Ajoene. Ajoene is not a genuine compound of garlic, but is formed in the human body from allicin after garlic intake. The antiplatelet effect induced by garlic and its extracts seems to be dose related, particularly under fasting condition,[12,13] and has been attributed to inhibition of thromboxane synthesis[14,15] or altered properties of platelet membrane.[9] In fresh garlic, Alliin is the major natural compound, with only a slight activity on platelet aggregation. Alliinase, an enzyme released when garlic is crushed, converts Alliin to Allicin that seems to be a more aggregation inhibitor. After garlic intake, condensation of Allicin induces formation of Ajoene, probably the most potent antiplatelet product of garlic. Ajoene may also be obtained by maceration of garlic oil or by alcoholic extraction. Apitz-Castro et al. have reported that Ajoene inhibits the binding of Von Willebrand Factor (vWF) and fibrinogen to GPIIb/IIIa,[16] thus exerting a potent inhibitory effect on platelet-vessel wall interaction. Thus, Ajoene inhibition of platelet aggregation seems to be mediated by a mechanism involving the vWF and fibrinogen receptors of the platelet membrane without interfering with the major metabolic pathways subsequently responsible for platelet aggregation.
With single- and multiple-dose administration of cilostazol, there was a significant reduction in platelet aggregation at all the time points tested. The results obtained in our study are in accordance with the earlier published reports of antiplatelet activity of cilostazol.[17] Coadministration of single and multiple doses of garlic and cilostazol did not enhance the inhibition of platelet aggregation of either cilostazol or garlic. The maximum inhibition of platelet aggregation with combination therapy was seen at 4 hours, with the combination similar to cilostazol alone. The results of our study show that there is no pharmacodynamic interaction between garlic and cilostazol; this is clearly indicated by the results, whereby the antiplatelet activity of neither the garlic nor cilostazol was effected by the presence of other drug.
Although there are reports of antiplatelet activity of garlic in healthy human subjects, to the best of our knowledge, this is the first study conducted in which we have studied the effects of garlic supplementation on platelet inhibition in diabetic patients. Furthermore, the interaction of garlic with cilostazol was also studied. The possible drawbacks of our study include a small sample size. Also, we have tested platelet aggregation with only one platelet-aggregating agent.
In conclusion, there is no possible pharmacodynamic interaction on antiplatelet activity of garlic and cilostazol administered at dose of 600 and 100 mg, respectively, at single dose and multiple doses given for seven days. However, the interaction at higher doses and for longer duration needs to be evaluated.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Abebe W. Herbal medication: Potential for adverse interactions with analgesic drugs. J Clin Pharm Ther. 2002;27:391–401. doi: 10.1046/j.1365-2710.2002.00444.x. [DOI] [PubMed] [Google Scholar]
- 2.Beebe HG, Dawson DL, Cutler BS, Herd JA, Strandness DE, Jr, Bortey EB, et al. A new pharmacological treatment for intermittent claudication: Results of a randomized, multicenter trial. Arch Intern Med. 1999;159:2041–50. doi: 10.1001/archinte.159.17.2041. [DOI] [PubMed] [Google Scholar]
- 3.Legnani C, Frascaro M, Guazzaloca G, Ludovici S, Cesarano G, Coccheri S. Effects of a dried garlic preparation on fibrinolysis and platelet aggregation in healthy subjects. Arzneimittelforschung. 1993;43:119–22. [PubMed] [Google Scholar]
- 4.Kiesewetter H, Jung F, Jung EM, Mroweitz C, Koscielny J, Wenzel E. Effect of garlic on platelet aggregation in patients with increased risk of juvenile ischaemic attack. Eur J Clin Pharmacol. 1993;45:333–6. doi: 10.1007/BF00265950. [DOI] [PubMed] [Google Scholar]
- 5.Bordia A, Verma SK, Srivastava KC. Effect of garlic on platelet aggregation in humans: A study in healthy subjects and patients with coronary artery disease. Prostaglandins Leukot Essent Fatty Acids. 1996;55:201–5. doi: 10.1016/s0952-3278(96)90099-x. [DOI] [PubMed] [Google Scholar]
- 6.Lawson LD, Ransom DK, Hughes BG. Inhibition of whole blood platelet-aggregation by compounds in garlic clove extracts and commercial garlic products. Thromb Res. 1992;65:141–56. doi: 10.1016/0049-3848(92)90234-2. [DOI] [PubMed] [Google Scholar]
- 7.Steiner M, Lin RS. Changes in platelet function and susceptibility of lipoproteins to oxidation associated with administration of aged garlic extract. J Cardiovasc Pharmacol. 1998;31:904–8. doi: 10.1097/00005344-199806000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Rahman K, Billington D. Dietary supplementation with aged garlic extract inhibits ADP-induced platelet aggregation in humans. J Nutr. 2000;130:2662–5. doi: 10.1093/jn/130.11.2662. [DOI] [PubMed] [Google Scholar]
- 9.Apitz-Castro R, Cabrera S, Cruz MR, Ledezma E, Jain MK. Effects of garlic extract and of three pure components isolated from it on human platelet aggregation, arachidonate metabolism, release reaction and platelet ultrastructure. Thromb Res. 1983;32:155–69. doi: 10.1016/0049-3848(83)90027-0. [DOI] [PubMed] [Google Scholar]
- 10.Apitz-Castro R, Escalante J, Vargas R, Jain MK. Ajoene, the antiplatelet principle of garlic, synergistically potentiates the antiaggregatory action of prostacyclin, forskolin, indomethacin and dypiridamole on human platelets. Thromb Res. 1986;42:303–11. doi: 10.1016/0049-3848(86)90259-8. [DOI] [PubMed] [Google Scholar]
- 11.Mohammad SF, Woodward SC. Characterization of a potent inhibitor of platelet aggregation and release reaction isolated from allium sativum (garlic) Thromb Res. 1986;44:793–806. doi: 10.1016/0049-3848(86)90025-3. [DOI] [PubMed] [Google Scholar]
- 12.Bordia A. Effect of garlic on human platelet aggregation in vitro. Atherosclerosis. 1978;30:355–60. doi: 10.1016/0021-9150(78)90129-6. [DOI] [PubMed] [Google Scholar]
- 13.Boullin DJ. Garlic as a platelet inhibitor. Lancet. 1981;1:776–7. doi: 10.1016/s0140-6736(81)92644-1. [DOI] [PubMed] [Google Scholar]
- 14.Makheia AN, Vanderhoek JY, Bailey JM. Inhibition of platelet aggregation and thromboxane synthesis by onion and garlic. Lancet. 1979;1:781. doi: 10.1016/s0140-6736(79)91239-x. [DOI] [PubMed] [Google Scholar]
- 15.Vanderhoek JY, Makheja AN, Bailey JM. Inhibition of fatty acid oxygenases by onion and garlic oils.Evidence for the mechanism by which these oils inhibit platelet aggregation. Biochem Pharmacol. 1980;29:3169–73. doi: 10.1016/0006-2952(80)90581-x. [DOI] [PubMed] [Google Scholar]
- 16.Apitz-Castro R, Jain MK, Bartoli F, Ledezma E, Ruiz MC, Salas R. Evidence for direct coupling of primary agonist-receptor interaction to the exposure of functional IIb-IIIa complexes in human blood platelets.Results from studies with the antiplatelet compound ajoene. Biochim Biophys Acta. 1991;1094:269–80. doi: 10.1016/0167-4889(91)90086-d. [DOI] [PubMed] [Google Scholar]
- 17.Aruna D, Naidu MU. Pharmacodynamic interaction studies of Ginkgo biloba with cilostazol and clopidogrel in healthy human subjects. Br J Clin Pharmacol. 2007;63:333–8. doi: 10.1111/j.1365-2125.2006.02759.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


