Abstract
Study Objectives:
We examined the effects of a cognitive behavioral self-help program (Refresh) to improve sleep, on sleep quality and symptoms of depression among first-year college students.
Methods:
Students in one residence hall (n = 48) participated in Refresh and students in another residence hall (n = 53) participated in a program of equal length (Breathe) designed to improve mood and increase resilience to stress. Both programs were delivered by e-mail in 8 weekly PDF files. Of these, 19 Refresh program participants and 15 Breathe program participants reported poor sleep quality at baseline (scores ≥ 5 on the Pittsburgh Sleep Quality Index [PSQI]). Participants completed the PSQI and the Center for Epidemiological Studies-Depression Scale (CES-D) at baseline and post-intervention.
Results:
Among students with poor sleep (PSQI > 5) at baseline, participation in Refresh was associated with greater improvements in sleep quality and greater reduction in depressive symptoms than participation in Breathe. Among students with high sleep quality at baseline there was no difference in baseline to post-intervention changes in sleep (PSQI) or depressive symptom severity (CES-D).
Conclusions:
A cognitive behavioral sleep improvement program delivered by e-mail may be a cost effective way for students with poor sleep quality to improve their sleep and reduce depressive symptoms. An important remaining question is whether improving sleep will also reduce risk for future depression.
Citation:
Trockel M; Manber R; Chang V; Thurston A; Tailor CB. An e-mail delivered CBT for sleep-health program for college students: effects on sleep quality and depression symptoms. J Clin Sleep Med 2011;7(3):276-281.
Keywords: Insomnia, depression, prevention
College students often have erratic sleep schedules, poor sleep hygiene, and correspondingly poor sleep quality.1 One report suggests that as many as 89% of college students report poor quality sleep.2 Inadequate or poor quality sleep may put students at increased risk for developing unipolar depressive disorders.3–6 In 1989, Ford and Kamerow published data suggesting that poor sleep is a risk factor for subsequent clinical depression and that further research is needed to determine if early recognition and treatment of sleep disturbance can prevent subsequent psychiatric problems.4 Since then, several authors have published empirical evidence indicating disturbed sleep, measured by self-report or with polysomnography6 is a risk factor for subsequent depression.3,5–12
Poor sleep is a predictor of subsequent depression during adolescence,5 and continues to constitute a risk in young3,7 and older adults.11,12 There is a dose response relationship between sleep disturbance in adolescence and subsequent symptoms of depression, with severe sleep disturbance incurring greater risk than moderate disturbance.13 It is therefore important to develop and test the feasibility of potentially cost-effective interventions to improve sleep among adolescents and young adults, which might subsequently be used to determine whether early intervention to improve sleep reverses the progression from disturbed sleep to depressive disorder.
The present study is an important first step toward this important goal. We developed and evaluated the feasibility and short-term efficacy of an intervention to improve sleep in college freshmen and its immediate effects on depressive symptom severity. In addition to addressing disturbed sleep, the intervention also addressed irregular sleep habits because such habits constitute a risk for insomnia and, importantly, there is evidence that day-to-day variations in bed-times and wake-up times by 2 to 4 h is associated with greater severity of symptoms of depression, even among students who regularly obtain ≥ 8 h of sleep.14 Moreover, a recent analysis of risk for depression and suicidal ideation among adolescents suggests having parents who insist on earlier bedtimes is a protective factor, which appears to be partially mediated by sleep duration and perception of getting enough sleep.15 Past research demonstrated that increasing the regularity of times into and out of bed in college students improves sleep, sleepiness, and mood.16
BRIEF SUMMARY
Current Knowledge/Study Rationale: College students often have poor sleep and associated symptoms of depressed mood. The purpose of this study is to test the efficacy of an e-mail delivered self-help program, based on CBT strategies for insomnia, designed for students living in on-campus residence halls.
Study Impact: Results of this quasi-experimental study indicate college students with poor sleep can improve their sleep and reduce symptoms of depression by self-administering a cognitive behavior strategy based program delivered via low-cost electronic media. These findings suggest further program development, implementation, and evaluation may help students improve the quality and regularity of their sleep, and perhaps even help halt or slow the progression from poor sleep to depressive illness.
Cognitive behavioral therapy for insomnia (CBT-I) has been established as an effective treatment for primary insomnia in adults when delivered in person,17–19 as a self-help intervention mailed to participants,20 or delivered via interactive Internet programs.21,22 In addition, a pilot study found that addition of CBT-I to pharmacologic treatment of depression led to improved outcomes in patients with insomnia and Major Depressive Disorder.23 We have therefore adapted CBT-I methods to the special circumstances of college life and to be delivered as a self-help intervention in 8 separate installments via e-mail.
In this report, we present data from a quasi-experimental design study of the effects on sleep quality and symptoms of depressed mood of an e-mail delivered cognitive and behavior strategy based sleep health improvement program, which was delivered to college students living in on-campus residence halls.
METHODS
Participants
We invited all students 18 years of age or older in 2 first-year student residence halls in a large private university to participate in a health promotion program. We presented the study at the first house meeting of the quarter and gave students an opportunity to ask questions and sign informed consent forms to participate in the study. Students were offered one unit of course credit for their participation in the study. The institutional review board approved the study protocol prior to commencement of the study.
Students in one residence hall were invited to participate in an 8-week CBT-I based sleep-health promotion program called Refresh. More than two-thirds (70% [58 of 83]) of eligible students elected to participate in the program. Students in the second residence hall were invited to participate in another health promotion program (called Breathe) designed to help students cope with stress and to improve their emotional health by using skills common to cognitive behavioral therapy (CBT) for depression. Fewer than half (41% [67 of 162]) of eligible students elected to participate in the program.
The baseline sample consisted of 61 women (32 in Refresh and 29 in Breathe) and 64 men (26 in Refresh and 38 in Breathe). Sixty-three (50%) identified themselves as White/Caucasian, 17 (14%) as Latino/Hispanic or Mexican American, and 14 (11%) as Chinese/Chinese American. Fewer than 5 students identified themselves as part of any other single racial or ethnic group, and 9 elected not to answer the question on race/ethnicity. Ninety-nine participating students were 18 years of age at the time they enrolled in the study, and the other 26 were between 19 and 22 years of age.
We sent students a link to online baseline and post-intervention surveys by e-mail, using Survey Monkey. For both baseline and post-intervention data collection, we sent as many as 3 reminder e-mails to students who had not yet responded.
Interventions
Both interventions were delivered in 8 weekly sessions, sent via e-mail messages with attached PDF files. Both programs incorporated vignette examples specific to college students. Students were encouraged to spend 30 min on each session.
The Refresh program has 2 tracks, one for students with poor sleep quality at baseline and a second (attenuated) version of the program for students with no or minimal sleep difficulties. Students were assigned a track based on their score on the Pittsburgh Sleep Quality index (PSQI), using a score > 5 to identify those with poor sleep quality.24 The complete program version for students with poor sleep at baseline, addressed: (1) the physiology of sleep with particular emphasis on circadian rhythms and recommendations for stabilizing circadian rhythm through anchoring wake time; (2) instructions on a time in bed-restriction protocol to consolidate sleep25; (3) relaxation training; (4) mindfulness training; (5) stimulus control strategies26; and (6) cognitive strategies to reduce the impact of maladaptive thoughts about sleep. The program encouraged participants to keep daily sleep logs and implement strategies for improved sleep health. The daily sleep log allowed students to record daily bedtimes, time out of bed, minutes in bed before sleep onset, number of night time awakenings, total minutes spent lying in bed awake during the night, total amount of sleep, number of alcoholic beverages before bedtime, satisfaction with sleep, and degree to which the student felt refreshed in the morning.
The time in bed restriction protocol was a significant portion of the program version for students with poor sleep, beginning with session three. The program first showed students how to self-administer sleep restriction. Students were instructed to compute their average total sleep time over the past week and then instructed to be in bed only as long as their average estimated actual sleep time, plus a margin ≤ 30 minutes. Subsequent program sessions instructed students to add 30 min to their scheduled time in bed if, on average: (a) they were able to fall asleep within 30 min, (b) they spent < 45 min lying in bed at night, and (c) they felt sleepy during most daytime hours.
If students were consistently unable to fall asleep in < 30 min after going to bed or were consistently spending > 45 min per night lying in bed awake, they were asked to review a checklist of strategies to improve sleep presented to them previously in the Refresh program, and to consider adopting one of these strategies. If they had already implemented these strategies, they were encouraged to decrease total time in bed by 30 min per night, to a minimum of 6 h per night if needed.
Students were instructed not to attempt the sleep restriction protocol if they believed any of the following applied to them at baseline: (1) “You have Bipolar Affective Disorder”; (2) “You have a family member with Bipolar Affective Disorder”; (3) “You have had a period of time lasting one week or longer during which you felt euphoric, felt like you had special abilities other people don't have, or felt persistently irritable”; (4) “Within the last 2 months you started a medication to treat depression or anxiety”; (5) “You frequently have trouble staying awake while driving or performing other activities in which drowsiness may have fatal consequences”; (6) “You have a long road trip coming up within the next 3 weeks and you have to be the driver, or you have to perform other activities in which drowsiness may have fatal consequences.”
The attenuated version of the Refresh program developed for students with good sleep quality at baseline included the same content as the full version, except that it did not include instruction on how to self-administer a time in bed restriction protocol to consolidate sleep.
The equal length comparison program, Breathe, was developed to reduce depressive symptoms and improve coping skills for stress. The program integrated concepts and skills from Dialectical Behavior Therapy,27,28 Mindfulness-Based Stress Reduction,29 and Aaron Beck's Cognitive Therapy.30 Specific topics include (1) recognizing and managing difficult emotions, (2) coping with stress, (3) cognitive reframing of negative thoughts, and (4) improving relationships with friends and family. Unlike Refresh, which used cognitive restructuring and mindfulness meditation to address cognitions that interfere with sleep and hyperarousal in bed, Breathe used these strategies to address low mood and general stress.
The Breathe program introduces new treatment components/modules each week, each focused on skill building. These included (1) self-monitoring of stressful events, associated thoughts and emotions, and coping behaviors; (2) challenging automatic negative thoughts; (3) finding solutions to interpersonal conflict; (4) engaging in enjoyable activities; (5) mindfulness meditation; and (6) relaxation. The Breathe program encouraged students to keep daily logs for a variety of self-monitoring tasks relevant to each module and to complete homework (assigned weekly) on topics such as motivation for the behavior change, time management, relaxation, mindfulness meditation, and asking for help.
Measures
The baseline survey included demographic information, the PSQI24 and the Center for Epidemiological Studies-Depression Scale (CES-D).31 Post-treatment measures included the PSQI and the CES-D.
The PSQI includes 19 questions and generates a sleep quality index ranging from 0 to 21. A PSQI score > 5 has good sensitivity and specificity for identifying individuals who are poor sleepers.24
The CES-D measures depressive symptoms in a general population with 20 items on a 0-3 point scale, for a total scale range of 0 to 60. The CES-D has demonstrated good ROC curve performance for detecting college students with clinically significant depression; it has also demonstrated adequate sensitivity and specificity using a cut off score > 15.32
Statistical Analyses
The analyzable sample consisted of all individuals who provided both pre and post measures. We computed change in PSQI and CES-D scores by subtracting baseline scores from post-intervention scores. We then used t-tests for independent samples to test for between-groups differences in PSQI and CES-D score changes from baseline to post-intervention. We also calculated Cohen's d effect sizes for within-group changes from baseline to post intervention on both outcome measures. Separate analyses were conducted for students with high (PSQI > 5) and low (PSQI ≥ 5) baseline sleep quality. We completed analyses using SPSS version 18.0.
RESULTS
Forty-eight of the 58 students (83%) participating in the Refresh program and 53 of 67 students (79%) participating in the Breathe program completed baseline and post-test PSQI and CES-D measures, and thus constitute the sample for this study. The 24 students who began the study but failed to complete one or both post-test measures did not differ significantly in baseline PSQI (4.4 vs. 4.8; t = −0.93; df = 123; p = 0.36), baseline CES-D (11.4 vs. 13.8; t = −1.56; df = 123; p = 0.13), or gender (46% women vs. 50% women; χ2 = 0.11; p = 0.75). Nineteen Refresh program participants and 15 Breathe program participants had poor sleep (PSQI > 5) at baseline. Tables 1 and 2 provide baseline data for students with baseline PSQI scores > 5 (Table 1) and those with lower PSQI scores (Table 2). Among students with PSQI scores > 5 at baseline, there were no statistically significant differences in gender, proportion of white students vs. other racial or ethnic group, or outcome measure (PSQI and CESD) scores at baseline. Among students with lower PSQI scores at baseline, there were statistically significant differences between the intervention groups in the proportion of participants who were women and in average baseline CES-D scores.
Table 1.
Baseline measures by intervention group, for the subgroup of students with PSQI > 5 at baseline
| Refresh, n = 19 M (SD) | Breathe, n = 15 M (SD) | Significance of group difference | |
|---|---|---|---|
| PSQI | 7.7 (1.8) | 7.5 (1.5) | t = 0.38; p = 0.71 |
| CESD | 19.7 (10.4) | 14.7 (8.1) | t = 1.57; p = 0.13 |
| Age | 18.3 (0.4) | 18.6 (1.0) | t = −1.23; p = 0.24 |
| Women* | 0.63 (0.50) | 0.73 (0.46) | X2 = 0.40; p = 0.53 |
| White/Caucasian* | 0.63 (0.50) | 0.53 (0.52) | X2 = 0.33; p = 0.56 |
Mean for categorical variables indicates the proportion of students who identified themselves as part of the specified group.
Table 2.
Baseline measures by intervention group, for the subgroup of students with PSQI ≤ 5 at baseline
| Refresh, n = 29 M (SD) | Breathe, n = 38 M (SD) | Significance of group difference | |
|---|---|---|---|
| PSQI | 3.3 (1.5) | 3.3 (1.2) | t = −0.31; p = 0.76 |
| CESD | 9.7 (5.6) | 13.7 (8.3) | t = −2.23; p = 0.02 |
| Age | 18.1 (0.4) | 18.2 (0.5) | t = −0.40; p = 0.69 |
| Women* | 0.55 (0.51) | 0.29 (0.46) | X2 = 4.70; p = 0.03 |
| White/Caucasian* | 0.48 (0.51) | 0.42 (0.50) | X2 = 0.25; p = 0.62 |
Mean for categorical variables indicates the proportion of students who identified themselves as part of the specified group.
More than half (54%) of the participants who received Refresh reported completing the entire program; the majority (94%) reported completing ≥ 4 of 8 sessions. For the Breathe program, 28% reported completing the entire program and 81% reported completing ≥ 4 of 8 sessions. Among Refresh students with baseline PSQI scores > 5, all but 2 (89%) completed ≥ 7 sessions. The remaining 2 Refresh students with elevated PSQI scores completed ≥ 5 of 8 sessions. Among Breathe students with baseline PSQI scores > 5, a third (33%) completed ≥ 7 sessions, and just over half (53%) completed ≥ 5 weekly sessions. Table 3 provides completion rates—defined as self-report of having completed ≥ 7 of 8 sessions—by baseline sleep category (PSQI > 5 or PSQI ≤ 5), and by program assignment.
Table 3.
Completion rates—defined as self-report of having completed ≥ 7 of 8 sessions—by baseline sleep quality category, and program assignment
| Refresh |
Breathe |
|||
|---|---|---|---|---|
| Total in category | Completers (%) | Total in category | Completers (%) | |
| Baseline PSQI ≤ 5 | 29 | 14 (48%) | 38 | 14 (37%) |
| Baseline PSQI > 5 | 19 | 17 (89%) | 15 | 5 (33%) |
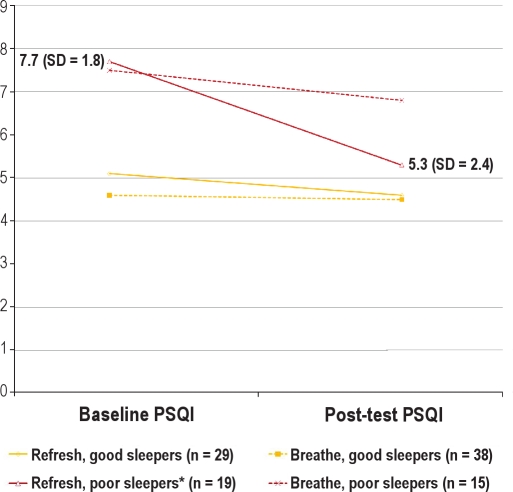
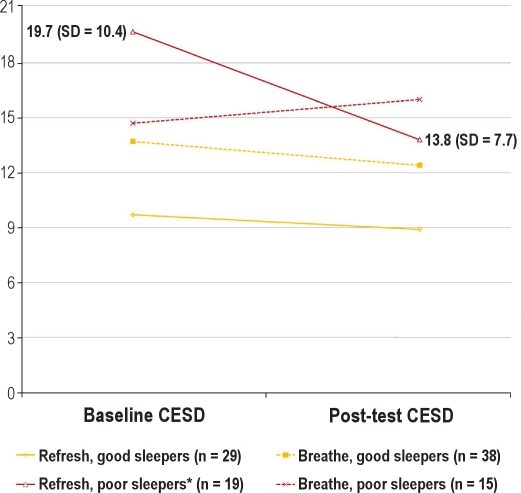
For participants with baseline PSQI scores > 5 (Figure 1), the Refresh intervention was associated with significantly greater reductions (t = −2.25; df = 32; p = 0.034) in PSQI scores (7.68 to 5.26 = −2.42 points; Cohen's d = 1.33) than the Breathe program (7.47 to 6.80 = −0.67 points; Cohen's d = 0.47). The between-group difference in PSQI change = −1.75 points, CI [−3.36 to −0.15]. For participants with baseline PSQI scores > 5, the Refresh program was also associated with significantly greater reductions (t = −2.19; df = 32; p = 0.036) in CES-D scores (19.69 to 13.75 = −5.94 points; Cohen's d = 0.57) than the Breathe program (14.73 to 16.00 = 1.27 points; Cohen's d = 0.16) (Figure 2). The between-group difference in CES-D change was −7.20 points, CI [−14.00 to −0.39]. For participants with baseline PSQI scores ≤ 5, there were no significant differences in pre to post changes in sleep quality or depressive symptom severity between Refresh and Breathe (p = 0.23 for PSQI and p = 0.80 for CES-D).
Figure 1.
Baseline and post-test PSQI scores
*Change is significantly greater than observed in alternative treatment control group
Figure 2.
Baseline and post-test CESD scores
*Change is significantly greater than observed in alternative treatment control group
The average reductions in PSQI scores and CESD scores reported by the 2 participants with baseline PSQI scores > 5 who did not complete ≥ 7 units of the program were 0.00 and 1.00 respectively. The small sample number of participants this group (n = 2) is not sufficient to test the statistical significance of these score reductions compared with average score reductions among participants who completed ≥ 7 of 8 units (n = 17), which were 2.71 and 6.51 for PSQI and CESD scores, respectively.
DISCUSSION
We focus our discussion primarily on findings among students with disturbed sleep at baseline who received the full version of the e-mail delivered self-help program using validated cognitive behavior therapy for insomnia strategies.17–19 The main findings of this study are that, compared to an equal length comparison program, participation in an e-mail delivered self-help CBT-I based program was associated with greater improvements in sleep quality and greater reductions in symptoms of depression among college students with low sleep quality at baseline. This study extends prior findings that self-help CBT-I is effective for adults with insomnia.17–22 Previous adult self-help CBT-I studies have used written materials20 or the Internet.21,22 Our study suggests e-mail delivery of weekly CBT-I based content may be an effective method of helping students with sleep problems improve their sleep.
Most encouraging was our finding that among individuals with poor sleep quality, a sleep enhancement intervention was associated with greater improvement in depressive symptoms than an intervention to improve mood and reduce stress. Our results are consistent with a large body of literature indicating that disturbed sleep constitutes a risk factor for depression3–12 and are consistent with a previous finding that CBT-I improves outcomes among depressed patients receiving antidepressant medication therapy.23 A previous study found that irregular sleep patterns can lead to desensitization of serotonergic receptor systems,33 which suggests a possible biologic mechanism for the relationship between impaired sleep and depressed mood. As our study was conducted with college students, many of whom have irregular sleep schedules, it is possible that the observed improvement in mood is mediated by regularizing the students' sleep schedules. However, we do not have sufficient data to test this hypothesis.
The full version of the program for students with sleep difficulties demonstrated effectiveness. However, we did not find benefit of the sleep-health promotion program in a group of college students with little or no sleep disturbance at baseline. Brown and colleagues found improved sleep quality (PSQI scores) with a single group 30-minute sleep-health education program in a general population college sample.34 It may be that the group of students studied by Brown and colleagues34 had sleep distress at baseline (mean PSQI = 7.3 among intervention group participants and 6.6 among controls) comparable to our sample of students with sleep problems (mean PSQI = 7.7 for Refresh participants and 7.5 for Breathe participants) and different from our group of participants without significant baseline sleep problems (mean PSQI = 3.3 for Refresh participants and 3.5 for Breathe participants). It seems reasonable to expect that students with disturbed sleep at baseline may benefit most from a program designed to help them improve their sleep.
Importantly, among students with baseline sleep difficulties, targeting sleep-health appeared more successful at reducing depressive symptoms than an intervention targeting negative self-talk and coping strategies that are common targets of CBT for depression. Given that poor sleep is a modifiable risk factor for depressed mood,3–12 it is encouraging that targeting sleep-health was also associated with reduction in depressive symptoms. Although we do not have long-term data to directly test the assertion that improving sleep will reduce the risk for a future depressive episode, improving sleep might be an important element in depression prevention interventions for students with sleep problems.
There are limitations of our study that warrant mention. Perhaps the most important limitation is that students were assigned to intervention groups by residence hall, rather than by random assignment. Although this feature in the design reduced the danger of cross-contamination of treatment, it also means we cannot rule out the possibility of systematic differences in students who live in one residence hall versus the other. Among students who did not have significant sleep problems at baseline, the Breathe intervention sample included a greater proportion of women and had higher average baseline symptoms of depression. Although students with poor sleep quality in the control and intervention samples did not differ by a statistically significant margin on key baseline variables, Refresh participants in this group scored 5 points higher on the baseline CESD measure, which is a clinically meaningful difference. Thus we cannot rule out the possibility that the observed intervention group differences could be at least partially explained by regression to the mean among Refresh participants. Quasi-experimental design does not have the same fidelity in internal validity inherent in a randomized clinical trial. Further research using a true experimental design is needed to establish an evidence base for the effectiveness of electronically delivered CBT-I for improving sleep and symptoms of depression among college students with sleep difficulties. Future experimental design research with adequate follow-up time is also needed to determine whether improving sleep will reduce risk of future depression.
Selection of students residing at a highly selective private university may limit the generalizability of our results. Compared to other groups of college students, the students who participated in this study may be more motivated and better able to follow a self-directed program to improve sleep through cognitive and behavioral strategies.
Another limitation of our study is that both sleep quality and depression were each assessed with only one self-report measure. Self-report measures are subject to demand characteristics, which could bias our results. The assessment of participant adherence was limited to self-report of the number of units they had completed. Although limited, these data revealed that a higher proportion of students with poor sleep at baseline completed at least 7 of 8 units, suggesting Refresh is acceptable to a large majority of freshmen with sleep problems.
We cannot determine from our data what, if any, information or intervention may be beneficial for students with no sleep problems. We are also unable to determine from our data whether one or a few components, rather than the whole collection of cognitive and behavior strategies, is associated with observed improvements among students with poor sleep at baseline.
Future research might experiment with intervention tailoring, delivering intervention components that fit students' needs determined by baseline assessment. For example, students with a delayed chronotype may benefit from a module that specifically addresses circadian entrainment, and others may not need it. Most students with insomnia will benefit from combined stimulus control and time-in-bed restriction modules. Although the self-reported number of units completed was very high, we believe future research will also need to evaluate reasons for dropout and consider methods to enhance retention. Perhaps tailored interventions with fewer modules may offer higher adherence without reducing effectiveness, as will adding a motivation enhancement component, though these possibilities await empirical support.
Future research may also determine whether intervention to improve sleep will also improve students' academic performance. Chronic sleep disturbance is strongly associated with short-term cognitive impairments,35 and in adolescents has been linked with subsequent impairment in academic performance.36 College students who report better sleep quality perform better on academic measures than those reporting a poorer quality of sleep,37 and variable sleep schedules, specifically later weekend wake-up times, accounts for significant variance in end-of-term grades.38 Students who obtain less REM sleep than needed may also be less able to integrate and store newly learned information.39,40 Even moderate sleep disturbance has serious implications for neurobehavioral functions, as sleep duration of six hours or less per night for 14 consecutive nights has been shown to produce cognitive performance deficits equivalent to two nights of no sleep.36 Interventions may therefore increase academic performance by improving sleep among students with insomnia and by motivating students without insomnia to allocate sufficient time for sleep.
One attractive feature of the intervention we tested is that electronically delivered practical self-help may be a good fit with the culture of the population for which it was developed. Additional new technologies to deliver self-assessment and self-administration of CBT-I, such as the internet delivery and text messaging offer opportunity for further development of cost-effective and easy to disseminate sleep-health promotion interventions. Iterative sleep-health promotion program development and evaluation research has the potential to help achieve significant gains in well-being of college students by helping them to improve the quality and regularity of their sleep, and may even halt or slow the progression from poor sleep to depressive illness.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This research was conducted at Stanford University. During their initial work on this research, Dr. Trockel and Dr. Chang were funded by an NIMH post-doctoral fellowship grant: T32 5 MH09938-15.
REFERENCES
- 1.Brown FC, Buboltz WC, Jr, Soper B. Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behav Med. 2002;28:33–8. doi: 10.1080/08964280209596396. [DOI] [PubMed] [Google Scholar]
- 2.Buboltz WC, Jr, Brown F, Soper B. Sleep habits and patterns of college students: a preliminary study. J Am Coll Health. 2001;50:131–5. doi: 10.1080/07448480109596017. [DOI] [PubMed] [Google Scholar]
- 3.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 5.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Szklo-Coxe M, Young T, Peppard PE, Finn LA, Benca RM. Prospective associations of insomnia markers and symptoms with depression. Am J Epidemiol. 2010;171:709–20. doi: 10.1093/aje/kwp454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–8. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 8.Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ. Insomnia in young men and subsequent depression. The Johns Hopkins Precursors Study. Am J Epidemiol. 1997;146:105–14. doi: 10.1093/oxfordjournals.aje.a009241. [DOI] [PubMed] [Google Scholar]
- 9.Livingston G, Blizard B, Mann A. Does sleep disturbance predict depression in elderly people? A study in inner London. Br J Gen Pract. 1993;43:445–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Paffenbarger RS, Jr, Lee IM, Leung R. Physical activity and personal characteristics associated with depression and suicide in American college men. Acta Psychiatr Scand Suppl. 1994;377:16–22. doi: 10.1111/j.1600-0447.1994.tb05796.x. [DOI] [PubMed] [Google Scholar]
- 11.Perlis ML, Smith LJ, Lyness JM, et al. Insomnia as a risk factor for onset of depression in the elderly. Behav Sleep Med. 2006;4:104–13. doi: 10.1207/s15402010bsm0402_3. [DOI] [PubMed] [Google Scholar]
- 12.Roberts RE, Shema SJ, Kaplan GA, Strawbridge WJ. Sleep complaints and depression in an aging cohort: A prospective perspective. Am J Psychiatry. 2000;157:81–8. doi: 10.1176/ajp.157.1.81. [DOI] [PubMed] [Google Scholar]
- 13.Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res. 2002;53:561–9. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- 14.Taub JM. Behavioral and psychophysiological correlates of irregularity in chronic sleep routines. Biol Psychol. 1978;7:37–53. doi: 10.1016/0301-0511(78)90041-8. [DOI] [PubMed] [Google Scholar]
- 15.Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, Posner K. Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep. 2010;33:97–106. doi: 10.1093/sleep/33.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manber R, Bootzin RR, Acebo C, Carskadon MA. The effects of regularizing sleep-wake schedules on daytime sleepiness. Sleep. 1996;19:432–41. doi: 10.1093/sleep/19.5.432. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs GD, Pace-Schott EF, Stickgold R, Otto MW. Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison. Arch Intern Med. 2004;164:1888–96. doi: 10.1001/archinte.164.17.1888. [DOI] [PubMed] [Google Scholar]
- 18.Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia:update of the recent evidence (1998-2004) Sleep. 2006;29:1398–414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- 19.Morin CM, Vallieres A, Guay B, et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial. JAMA. 2009;301:2005–15. doi: 10.1001/jama.2009.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morin CM, Beaulieu-Bonneau S, LeBlanc M, Savard J. Self-help treatment for insomnia: a randomized controlled trial. Sleep. 2005;28:1319–27. doi: 10.1093/sleep/28.10.1319. [DOI] [PubMed] [Google Scholar]
- 21.Ritterband LM, Thorndike FP, Gonder-Frederick LA, et al. Efficacy of an Internet-based behavioral intervention for adults with insomnia. Arch Gen Psychiatry. 2009;66:692–8. doi: 10.1001/archgenpsychiatry.2009.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vincent N, Lewycky S. Logging on for better sleep: RCT of the effectiveness of online treatment for insomnia. Sleep. 2009;32:807–15. doi: 10.1093/sleep/32.6.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–95. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 25.Spielman AJ, Saskin P, Thorpy MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep. 1987;10:45–56. [PubMed] [Google Scholar]
- 26.Bootzin RR, Perlis ML. Nonpharmacologic treatments of insomnia. J Clin Psychiatry. 1992;53(Suppl):37–41. [PubMed] [Google Scholar]
- 27.Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Gilford Press; 1993. [Google Scholar]
- 28.Linehan MM. Skills training manual for treating borderline personality disorder. New York: Gilford Press; 1993. [Google Scholar]
- 29.Kabat-Zinn J. New York: Delacorte Press; 1990. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. [Google Scholar]
- 30.Beck AT, Rush AJ, Shaw BF, Emery G. New York: Guilford Press; 1979. Cognitive therapy of depression. [Google Scholar]
- 31.Radloff LS. A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 32.Shean G, Baldwin G. Sensitivity and specificity of depression questionnaires in a college-age sample. J Genet Psychol. 2008;169:281–8. doi: 10.3200/GNTP.169.3.281-292. [DOI] [PubMed] [Google Scholar]
- 33.Roman V, Walstra I, Luiten PG, Meerlo P. Too little sleep gradually desensitizes the serotonin 1A receptor system. Sleep. 2005;28:1505–10. [PubMed] [Google Scholar]
- 34.Brown FC, Buboltz WC, Jr, Soper B. Development and evaluation of the Sleep Treatment and Education Program for Students (STEPS) J Am Coll Health. 2006;54:231–7. doi: 10.3200/JACH.54.4.231-237. [DOI] [PubMed] [Google Scholar]
- 35.Roberts RE, Roberts CR, Duong HT. Chronic insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health. 2008;42:294–302. doi: 10.1016/j.jadohealth.2007.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 37.Howell AJ, Jahrig JC, Powell RA. Sleep quality, sleep propensity and academic performance. Percept Mot Skills. 2004;99:525–35. doi: 10.2466/pms.99.2.525-535. [DOI] [PubMed] [Google Scholar]
- 38.Trockel MT, Barnes MD, Egget DL. Health-related variables and academic performance among first-year college students: implications for sleep and other behaviors. J Am Coll Health. 2000;49:125–31. doi: 10.1080/07448480009596294. [DOI] [PubMed] [Google Scholar]
- 39.Karni A, Tanne D, Rubenstein BS, Askenasy JJ, Sagi D. Dependence on REM sleep of overnight improvement of a perceptual skill. Science. 1994;265:679–82. doi: 10.1126/science.8036518. [DOI] [PubMed] [Google Scholar]
- 40.Smith C, Lapp L. Increases in number of REMS and REM density in humans following an intensive learning period. Sleep. 1991;14:325–30. doi: 10.1093/sleep/14.4.325. [DOI] [PubMed] [Google Scholar]