Abstract
OBJECTIVE
Despite promising results from studies on mouse models, intranasal insulin failed to prevent or delay the development of type 1 diabetes in autoantibody-positive children with HLA-conferred disease susceptibility. To analyze whether the insulin dose was inadequate to elicit an immunomodulatory response, we compared the changes observed in insulin antibody (IA) affinity and isotypes after treatment with nasal insulin or placebo.
RESEARCH DESIGN AND METHODS
Ninety-five children (47 in the placebo group and 48 in the insulin group of the total of 224 children randomized for the trial) with HLA-conferred susceptibility to type 1 diabetes derived from the intervention arm of the Finnish Type 1 Diabetes Prediction and Prevention study were included in these analyses. Blood samples drawn before or at the beginning of the treatment and after treatment for 3 and 6 months were analyzed for IA affinity and isotype-specific IAs (IgG1–4, IgA, IgM, and IgE).
RESULTS
IgG3- and IgA-IA levels (P = 0.031 and 0.015, respectively) and the number of IgG3-IA–positive subjects (P = 0.022) were significantly higher at 6 months after the initiation of the treatment in the insulin group. No significant differences were observed between the two groups in IA affinity or other IA isotypes.
CONCLUSIONS
The insulin dose administered induced a modest change in the IA isotype profile. The lack of impact of nasal insulin on IA affinity implies that the immune response of study subjects was already mature at the beginning of the intervention.
Numerous studies have demonstrated that the prophylactic administration of insulin via various routes prevents development of autoimmune diabetes in NOD mice and other animal models of type 1 diabetes (1–3). The beneficial effect of insulin is perceived to be attributed to the promotion of immunologic tolerance, alterations in metabolism (i.e., exogenous insulin reducing the metabolic burden of the β-cells), or a combination of both mechanisms (3,4). Despite promising results from pilot studies (5), subcutaneously (6), orally (7), and intranasally (8) administered insulin failed to prevent type 1 diabetes in large clinical trials in humans. Several explanations for these failures have been proposed, including inadequate insulin dose, incorrect timing of the intervention, and inefficiency of insulin administration as a prophylactic measure for human type 1 diabetes.
Increasing affinity of an antibody to the antigen reflects the maturation of the immune response and, thus, could be a valuable tool when assessing the pathogenesis of autoimmune diseases. Accordingly, the affinity of insulin autoantibodies (IAAs) has been proposed to provide a means to differentiate between progressive and nonprogressive or slowly progressive β-cell autoimmunity, because high IAA affinity has been demonstrated to increase the risk of type 1 diabetes in schoolchildren from the general population and in adults and adolescents having first-degree relative(s) with type 1 diabetes (9,10). However, among young children with HLA-conferred susceptibility to type 1 diabetes, IAA affinities were already high at the time of seroconversion, and the affinity failed to differentiate between a progressing and a nonprogressing or slowly progressing disease process (11). Maturation of an immune response is also reflected by changes in the isotype profile of the antibody response. According to a previous study in children with HLA-defined disease predisposition, high titers of IgG1- and IgG3-IAA are associated with increased risk of type 1 diabetes, whereas a weak or failing IgG3 response seems to provide relative protection from the disease (12).
Because the reasons for the failure of the nasal insulin treatment in the prevention of type 1 diabetes remain elusive (8), we decided to characterize its effects on the insulin-specific antibody profiles. Accordingly, we determined the insulin antibody (IA) affinities and isotypes from 95 children who participated in the prevention trial with intranasal insulin (47 in the placebo group and 48 in the insulin group) in the Finnish Type 1 Diabetes Prediction and Prevention (DIPP) Study (8).
RESEARCH DESIGN AND METHODS
The participants in this study were derived from the intervention arm of the Finnish DIPP Study (8). In the DIPP Study, children with HLA-conferred susceptibility to type 1 diabetes were observed from birth for the appearance of diabetes-associated autoantibodies (13). Measurement of islet cell autoantibodies (ICAs) was used as the first step in the autoantibody screening. If a subject seroconverted to ICA positivity or developed diabetes, all his/her previous samples were analyzed also for IAA, glutamic acid decarboxylase (GADA), and islet antigen-2 (IA-2A). Children aged >1 year with persistent positivity for multiple (≥2) autoantibodies were invited into the intervention arm of the DIPP Study comprising a randomized, double–blinded, and placebo–controlled trial with nasally administrated insulin (registered with clinicaltrials.gov, Clinical trial reg. no. NCT0022361) (8). In brief, participants received either recombinant human short-acting insulin (Actrapid in its regular buffer; NovoNordisk, Bagsvaerd, Denmark) or the buffer alone. The insulin dose administered once daily was 1 international unit (IU)/kg, rounded because of practical reasons to multiples of 10 IU (maximum 60 IU per day), divided evenly between the nostrils, and given just before breakfast. The preparations were donated by the manufacturer and packed in metered nasal applicators (VP/100S; Beresol, Gävlinge, Sweden). For the current study, 95 children (47 in the placebo group and 48 in the insulin group) of a total 224 randomized subjects in the original trial (109 in the placebo group and 115 in the insulin group) were selected on the basis of availability of blood samples at 0, 3, and 6 months after the start of the intervention and on testing positive for IAs in at least one of these samples. The baseline characteristics of the study subjects in the current study and those included in the intervention arm of the DIPP Study (8) are presented in Supplementary Table 1.
Laboratory methods
Screening for HLA-DQB1–associated risk genotypes for type 1 diabetes (the high-risk genotype HLA DQB1*02/*0302 and the moderate-risk genotypes HLA DQB1*0302/x; x≠*02, *0301, *0602, or *0603 conferring average risks of 8 and 3%, respectively) (14,15) was performed on cord blood samples by time-resolved triple-label hybridization (16). The INS −23Hph1 polymorphism was analyzed using PCR and a lanthanide-labeled oligonucleotide hybridization method, as described previously (16).
Antibody measurements were performed on serum or plasma samples, depending on availability, ICA with immunofluorescence (17) and IAA (and IA), GADA, and IA-2A with specific radiobinding assays (18–20). The cutoff values for ICA, IAA, GADA, and IA-2A positivity were 2.5 Juvenile Diabetes Foundation units, 3.48, 5.36, and 0.43 relative units (RU), respectively. Cutoff values for the IAA, GADA, and IA-2A assays were based on the 99th percentile of more than 370 healthy Finnish children and adolescents. All initially ICA-positive samples were retested to confirm positivity, as were the samples with IAA, GADA, and IA-2A levels between the 97th and 99.5th percentiles. On the basis of the 2005 Diabetes Autoantibody Standardization Program Workshop, the disease sensitivity values for the IAA, GADA, and IA-2A assays were 58, 82, and 72%, and the disease specificity values were 98, 96, and 100%, respectively.
IAA and IA affinity was measured by radiobinding of 0.159 nmol/L labeled mono125I (TyrA14) human recombinant insulin (Amersham, GE Healthcare, Buckinghamshire, UK; activity 2,000 Ci/mmol) after competition with eight increasing concentrations (between 1.2 × 10−12 and 1.75 × 10−4 mol/L) of unlabeled human recombinant insulin (Roche Diagnostics, Mannheim, Germany). The assay was modified from that described by Achenbach et al. (9). Samples were measured in duplicates, and the total volume per well was 30 μL. After precipitation of the immune complexes, the amount of bound labeled insulin was measured with a liquid scintillation detector (1450 MicroBeta Trilux; Perkin Elmer Life Sciences, Turku, Finland), and the results were given as counts per minute. Values for the half-maximal inhibitory concentration (IC50) and the dissociation constant (Kd) were calculated by using Prism 5.0 (GraphPad Software, Inc., San Diego, CA), and IA affinity was given as the reciprocal of the Kd value (L/mol).
Analyzing high-affinity IA containing samples was not always straightforward. For 21 samples (of 272 samples in total) with high affinities, we had to extrapolate the affinity from the linear correlation between log Kd and log IC50 values (R2 = 0.955, P < 0.001) obtained for high-affinity samples (1010 L/mol < affinity < 1011 L/mol) that could be reliably determined. Samples from one study subject consistently showed characteristics of two-site binding and were eventually excluded from the analysis because of difficulties in determining reliable values, and samples from one subject included in the study were lost before measuring affinity. In addition, samples from three subjects demonstrated unreliable competitive binding curves despite three separate measurements and had to be excluded from the analysis. Despite these adjustments, the balance between the study groups was maintained with 45 subjects in both the placebo and insulin groups.
Isotype- and subclass-specific IAs were analyzed as described previously (12). Briefly, 5 μL serum was incubated with mono125I (TyrA14) human insulin and precipitated with biotinylated isotype- and subclass-specific monoclonal antibodies linked to streptavidin agarose (Pierce and Warriner, Chester, UK). The biotinylated monoclonal anti-human antibodies and anti-rat IgM were obtained from BD PharMingen (San Diego, CA), with the exception of anti-human IgG3, which was from Southern Biotech (Birmingham, AL). The results were expressed as SD scores as defined previously (12), and the cutoff level for positivity was set at an SD score of 3 SD.
Data analysis
SPSS 17.0 statistical software package (SPSS Inc., Chicago, IL) was used for the statistical analysis. The variables analyzed had skewed distributions, and nonparametric tests were primarily used, i.e., Wilcoxon signed rank test for paired variables and Mann–Whitney U test for independent variables. In addition, the χ2 test was used when applicable. Two-tailed statistical significance was set at P < 0.05. With 40 subjects in each group, we would have already had a statistical power of 80% to identify affinity differences of the magnitude similar to that described between risk subjects who later developed type 1 diabetes and those who remained unaffected in previous studies (9,10). Bonferroni correction for multiple comparisons was not applied in the data analysis.
RESULTS
The baseline characteristics of the study subjects are presented in Supplementary Table 2. Mean age and sex distribution were relatively uniform in the placebo and insulin groups. In addition, the median titers and range for diabetes-associated autoantibodies (ICA, IAA, GADA, and IA-2A) at baseline are given. No significant changes in the levels or number of subjects positive for these autoantibodies were seen between the treatment groups before the start of treatment or 3 and 6 months later (data not shown).
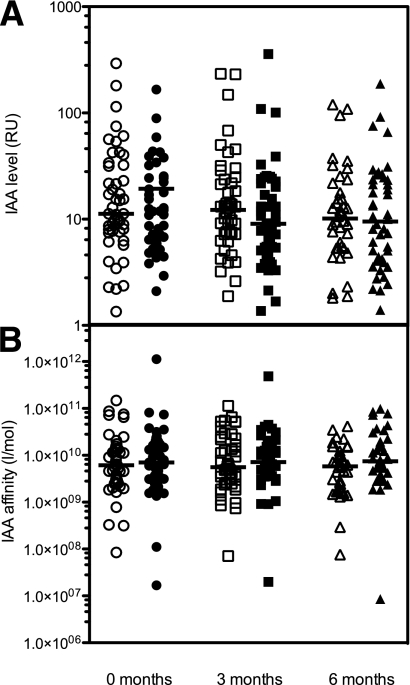
IA levels did not change significantly during the 6-month follow-up (Fig. 1A). More specifically, at the beginning of the treatment with either placebo or insulin, the median IAA levels for placebo and insulin groups were 11.3 RU (range 1.4–293.3) and 9.8 RU (range 0.7–166.0), respectively (P = 0.222). At the second sampling (3 months after the intervention started), median IA levels for placebo and insulin groups were 12.2 RU (range 0.7–233.2) and 9.0 RU (range 1.4–358.4, P = 0.245), respectively, and at 6 months, the median IA level was 10.1 RU (range 0.0–120.1) in the placebo group and 9.5 RU (range 1.4–187.9, P = 0.774) in the insulin-treated group. Even at the beginning of the intervention, the IAA affinities were high in both groups, with a median affinity in the placebo and insulin groups of 6.12 × 109 and 7.01 × 109 L/mol, respectively (P = 0.649). After the administration of placebo or insulin, the IA affinity remained essentially at the same level throughout the 6-month follow-up, and no significant differences between the two groups were evident (Fig. 1B). HLA-conferred risk (mediate vs. high risk) or insulin gene polymorphism (AA, AT, or TT) of the study subjects did not have any significant impact on IA affinity during the intervention (data not shown).
Figure 1.
A: IAA levels in RU. B: IAA affinities in L/mol. The samples drawn before and at ∼3 and 6 months after the start of the intervention are depicted by circles, squares, and triangles, respectively. Open symbols denote children in the placebo group, and filled symbols denote children in the insulin group. Horizontal lines represent medians. Note the logarithmic scale on the y axis.
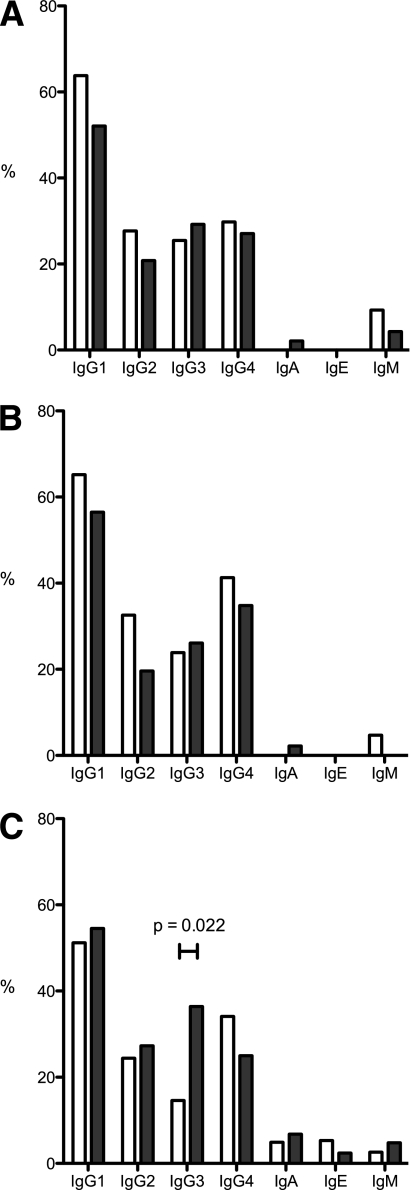
Data on titers of various IA subclasses and isotypes are presented in Table 1. In brief, statistically significant differences between the treatment groups were observed only for IgG3- and IgA-IAs at 6 months when children treated with insulin had higher antibody levels (P = 0.031 and 0.015, respectively). However, the titers of IgA-IA were generally low with only two subjects (4.9%) testing positive for IgA-IA in the placebo group and three subjects (5.9%) testing positive in the insulin group at 6 months after the initiation of the intervention (Fig. 2C, P = 0.704). In contrast, the difference between the placebo and insulin groups remained significant for IgG3-IA when autoantibody positivity was considered. Accordingly, 6 months after beginning the administration of intranasal insulin, 16 children (36.4%) tested positive for IgG3-IA in the insulin group compared with six children (14.6%) in the placebo group (Fig. 2C, P = 0.022). Spaghetti plots illustrating changes in IgG3-IAs for all study subjects positive for IgG3 at some of the three time points are presented in Fig. 3, and the baseline characteristics of these individuals are shown in Supplementary Table 3. In the placebo group, IgG3-IAs decreased in 9 of 14 patients (Fig. 3A), whereas IgG3-IAs increased in 6 of 19 patients in the insulin group (Fig. 3B). Accordingly, part of the observed difference in IgG3-IAs at 6 months was attributed to a decrease in the placebo group but also to a genuine increase in the insulin group. In keeping with previous reports (12), the study subjects who were diagnosed with type 1 diabetes during the intervention had significantly higher IA, IgG1-IA, and IgG3-IA levels at 0, 3, and 6 months, respectively, after the start of the intervention than those who remained nondiabetic (data not shown).
Table 1.
Results from the analyses of IAA isotypes, given as medians (range)
| Placebo group | Insulin group | P | |
|---|---|---|---|
| Median IgG1 titer, SDS (months) | |||
| 0 | 5.5 (0.0–136.1) | 3.2 (0.0–120.5) | 0.470 |
| 3 | 5.9 (0.0–99.3) | 4.2 (0.0–80.8) | 0.361 |
| 6 | 3.4 (0.0–106.8) | 3.4 (0.0–49.5) | 0.470 |
| Median IgG2 titer, SDS (months) | |||
| 0 | 0.5 (0.0–84.9) | 0.4 (0.0–95.3) | 0.639 |
| 3 | 1.0 (0.0–121.3) | 0.7 (0.0–96.3) | 0.465 |
| 6 | 1.2 (0.0–58.3) | 1.2 (0.0–47.2) | 0.893 |
| Median IgG3 titer, SDS (months) | |||
| 0 | 0.3 (0.0–166.9) | 0.5 (0.0–100.1) | 0.849 |
| 3 | 0.3 (0.0–74.9) | 0.1 (0.0–23.6) | 0.844 |
| 6 | 0.0 (0.0–50.3) | 0.3 (0.0–61.5) | 0.031 |
| Median IgG4 titer, SDS (months) | |||
| 0 | 1.2 (0.0–46.8) | 0.7 (0.0–42.7) | 0.714 |
| 3 | 1.4 (0.0–48.6) | 0.7 (0.0–35.0) | 0.614 |
| 6 | 0.7 (0.0–30.4) | 0.6 (0.0–35.4) | 0.957 |
| Median IgA titer, SDS (months) | |||
| 0 | 0.0 (0.0–2.3) | 0.0 (0.0–6.0) | 0.694 |
| 3 | 0.2 (0.0–1.9) | 0.0 (0.0–4.8) | 0.218 |
| 6 | 0.0 (0.0–6.9) | 0.0 (0.0–28.4) | 0.015 |
| Median IgE titer, SDS (months) | |||
| 0 | 0.2 (0.0–2.2) | 0.0 (0.0–2.5) | 0.596 |
| 3 | 0.0 (0.0–2.5) | 0.0 (0.0–2.5) | 0.610 |
| 6 | 0.5 (0.0–6.0) | 0.1 (0.0–3.1) | 0.410 |
| Median IgM titer, SDS (months) | |||
| 0 | 0.0 (0.0–17.8) | 0.0 (0.0–5.3) | 0.194 |
| 3 | 0.0 (0.0–13.5) | 0.0 (0.0–2.8) | 0.401 |
| 6 | 0.0 (0.0–10.7) | 0.2 (0.0–4.5) | 0.428 |
Boldface type indicates significant P values. SDS, SD score.
Figure 2.
Frequencies for positivity of different IAA isotypes in children receiving placebo (□) and insulin (■) intranasally. Statistically significant differences are marked. A: IAA isotypes at baseline. B: IAA isotypes ∼3 months from the start of the treatment. C: IAA isotypes ∼6 months from the start of the treatment.
Figure 3.
IgG3-IA levels in children who tested positive for IgG3 at one of the three time points (0, 3, or 6 months after the initiation of treatment). A: Study subjects receiving the placebo preparation (n = 14). B: Study subjects receiving the insulin preparation (n = 19). Note varying scale on the y axis.
CONCLUSIONS
Several explanations for the failures experienced in clinical trials using insulin as a preventive measure for type 1 diabetes during prediabetes have been proposed. The most obvious one is an inadequate amount of insulin administered for the induction of an immunomodulatory response. In the intervention arm of the DIPP Study, the intranasally delivered insulin dose was chosen to correspond to the approximate daily physiologic insulin need, i.e., 1 unit/kg, when insulin is given parenterally (8). The dose applied was four times the subcutaneously administered dose used in the Diabetes Prevention Trial (6). A blinded crossover trial showed that 1.6 mg (∼46 IU) recombinant insulin administered to the nasal mucosa daily for 10 days and then twice per week for a total of 6 months induced an increase in IA levels compared with placebo (21). We could not confirm this finding because our results indicated no significant changes in IA levels after the initiation of intranasal insulin treatment (Fig. 1A). Variable IA responses to exogenous insulin are probably attributed to the result of differences in patient populations and in the stage of prediabetes among the study subjects. More specifically, Harrison et al. (21) recruited first-degree relatives of patients with type 1 diabetes who tested positive for at least one autoantibody (IAA, GADA, or IA-2A), whereas the inclusion criteria for the intervention arm of the DIPP Study required positivity for at least two autoantibodies. It is possible that the subjects in the current study had a more mature immune response to insulin at the beginning of the intervention and thus did not show any increase in IA levels. However, we demonstrate that the intranasal insulin dose delivered in the DIPP Study did induce a detectable change in IA characteristics and, accordingly, was adequate to elicit a modest immunomodulatory effect. More specifically, insulin treatment increased the titers of IgG3- and IgA-IAs after 6 months of treatment compared with the placebo group (Table 1). However, the levels of IgA-IA were very low in both treatment groups, and when the number of IgA-IA–positive individuals was compared, no significant difference was seen between the two groups. For IgG3-IAs, the observed increase was more convincing. Children in the insulin group were also significantly more often IgG3-IA–positive compared with children receiving the placebo preparation after 6 months of treatment (Fig. 2C).
If the insulin dose is adequate and exerts an immunologic response, the reasons for ineffectiveness in the prevention of type 1 diabetes could be incorrect timing of the intervention during the prediabetic phase, choice of an unresponsive subgroup, or simply the fact that insulin administration during preclinical diabetes does not prevent the clinical disease in humans. On the basis of the present knowledge, it is not possible to definitely rule out any of these options, and it is also possible that the combination of the above explanations contributed to the failure. In the DIPP Study, children with HLA-conferred susceptibility to type 1 diabetes were under close follow-up, and the intervention was started in subjects who tested positive for at least two autoantibodies (ICA, IAA, GADA, and IA-2A). Our analysis shows that, in this population, IAA affinity was already relatively high at the start of the intervention, and no additional maturation of the IA response in terms of increased affinity during the 6-month follow-up was observed. It has been demonstrated that high IAA affinity is associated with increased risk of progression to type 1 diabetes in adults and adolescents having first-degree relative(s) with type 1 diabetes and among schoolchildren from the general population, and, accordingly, would present a marker for more aggressive or advanced insulitis (9,10). Along these lines, it could be argued that, in the DIPP Study, the insulin administration was started too late in the disease process when the immune response to insulin was already mature. On the other hand, the intervention started earlier in relation to initial seroconversion in the DIPP Study than in any previous trial. Previously published data in young children with HLA-conferred susceptibility to type 1 diabetes showed that IAA affinity was already high at the time of seroconversion (11). Accordingly, it is questionable to draw any conclusions about the stage of prediabetes on the basis of IAA affinity among subjects participating in the DIPP Study. Earlier initiation of the treatment, i.e., before the appearance of the first autoantibodies, would raise significant practical and ethical issues because the risk of clinical disease is relatively low before seroconversion to autoantibody positivity, and such an effort would inevitably require a higher number of children to be exposed to insulin treatment.
Supplementary Material
Acknowledgments
This work was supported by grants from the Juvenile Diabetes Research Foundation International (grants 4-1998-274, 4-1999-731, 4-2001-435, 1-2006-267); European Union (grant BMH4-CT98-3314); Novo Nordisk Foundation; Academy of Finland; Special Research Funds for University Hospitals in Finland; Diabetes Research Foundation, Finland; and Sigrid Jusélius Foundation, Finland. No other potential conflicts of interest relevant to this article were reported.
S.J.R. researched the data and wrote the first version of the manuscript. T.H., H.S., and M.K. researched the data. M.K., J.I., and O.S. are the Principal Investigators in the DIPP Study. O.S., M.K., J.I., R.V., H.H., T.S., and K.N.-S. planned and implemented the intervention with intranasal insulin in the DIPP Study. All authors edited the article.
The authors thank the dedicated personnel of the DIPP Study in Turku, Oulu, and Tampere, and the study children and their families for their essential contribution.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc10-1449/-/DC1.
References
- 1.Hancock WW, Polanski M, Zhang J, Blogg N, Weiner HL. Suppression of insulitis in non-obese diabetic (NOD) mice by oral insulin administration is associated with selective expression of interleukin-4 and -10, transforming growth factor-beta, and prostaglandin-E. Am J Pathol 1995;147:1193–1199 [PMC free article] [PubMed] [Google Scholar]
- 2.Daniel D, Wegmann DR. Protection of nonobese diabetic mice from diabetes by intranasal or subcutaneous administration of insulin peptide B-(9-23). Proc Natl Acad Sci U S A 1996;93:956–960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karounos DG, Bryson JS, Cohen DA. Metabolically inactive insulin analog prevents type I diabetes in prediabetic NOD mice. J Clin Invest 1997;100:1344–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowman MA, Campbell L, Darrow BL, Ellis TM, Suresh A, Atkinson MA. Immunological and metabolic effects of prophylactic insulin therapy in the NOD-scid/scid adoptive transfer model of IDDM. Diabetes 1996;45:205–208 [DOI] [PubMed] [Google Scholar]
- 5.Keller RJ, Eisenbarth GS, Jackson RA. Insulin prophylaxis in individuals at high risk of type I diabetes. Lancet 1993;341:927–928 [DOI] [PubMed] [Google Scholar]
- 6.Diabetes Prevention Trial--Type 1 Diabetes Study Group Effects of insulin in relatives of patients with type 1 diabetes mellitus. N Engl J Med 2002;346:1685–1691 [DOI] [PubMed] [Google Scholar]
- 7.Skyler JS, Krischer JP, Wolfsdorf J, et al. Effects of oral insulin in relatives of patients with type 1 diabetes: The Diabetes Prevention Trial—Type 1. Diabetes Care 2005;28:1068–1076 [DOI] [PubMed] [Google Scholar]
- 8.Näntö-Salonen K, Kupila A, Simell S, et al. Nasal insulin to prevent type 1 diabetes in children with HLA genotypes and autoantibodies conferring increased risk of disease: a double-blind, randomised controlled trial. Lancet 2008;372:1746–1755 [DOI] [PubMed] [Google Scholar]
- 9.Achenbach P, Koczwara K, Knopff A, Naserke H, Ziegler AG, Bonifacio E. Mature high-affinity immune responses to (pro)insulin anticipate the autoimmune cascade that leads to type 1 diabetes. J Clin Invest 2004;114:589–597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schlosser M, Koczwara K, Kenk H, et al. In insulin-autoantibody-positive children from the general population, antibody affinity identifies those at high and low risk. Diabetologia 2005;48:1830–1832 [DOI] [PubMed] [Google Scholar]
- 11.Siljander H, Härkönen T, Hermann R, et al. Role of insulin autoantibody affinity as a predictive marker for type 1 diabetes in young children with HLA-conferred disease susceptibility. Diabetes Metab Res Rev 2009;25:615–622 [DOI] [PubMed] [Google Scholar]
- 12.Hoppu S, Ronkainen MS, Kimpimäki T, et al. Insulin autoantibody isotypes during the prediabetic process in young children with increased genetic risk of type 1 diabetes. Pediatr Res 2004;55:236–242 [DOI] [PubMed] [Google Scholar]
- 13.Kimpimäki T, Kupila A, Hämäläinen AM, et al. The first signs of beta-cell autoimmunity appear in infancy in genetically susceptible children from the general population: the Finnish Type 1 Diabetes Prediction and Prevention Study. J Clin Endocrinol Metab 2001;86:4782–4788 [DOI] [PubMed] [Google Scholar]
- 14.Ilonen J, Reijonen H, Herva E, et al. Rapid HLA-DQB1 genotyping for four alleles in the assessment of risk for IDDM in the Finnish population. The Childhood Diabetes in Finland (DiMe) Study Group. Diabetes Care 1996;19:795–800 [DOI] [PubMed] [Google Scholar]
- 15.Nejentsev S, Sjöroos M, Soukka T, et al. Population-based genetic screening for the estimation of type 1 diabetes mellitus risk in Finland: selective genotyping of markers in the HLA-DQB1, HLA-DQA1 and HLA-DRB1 loci. Diabet Med 1999;16:985–992 [DOI] [PubMed] [Google Scholar]
- 16.Sjöroos M, Iitiä A, Ilonen J, Reijonen H, Lövgren T. Triple-label hybridization assay for type-1 diabetes-related HLA alleles. Biotechniques 1995;18:870–877 [PubMed] [Google Scholar]
- 17.Bottazzo GF, Florin-Christensen A, Doniach D. Islet-cell antibodies in diabetes mellitus with autoimmune polyendocrine deficiencies. Lancet 1974;2:1279–1283 [DOI] [PubMed] [Google Scholar]
- 18.Williams AJ, Bingley PJ, Bonifacio E, Palmer JP, Gale EA. A novel micro-assay for insulin autoantibodies. J Autoimmun 1997;10:473–478 [DOI] [PubMed] [Google Scholar]
- 19.Savola K, Bonifacio E, Sabbah E, et al. IA-2 antibodies—a sensitive marker of IDDM with clinical onset in childhood and adolescence. Childhood Diabetes in Finland Study Group. Diabetologia 1998;41:424–429 [DOI] [PubMed] [Google Scholar]
- 20.Savola K, Sabbah E, Kulmala P, Vähäsalo P, Ilonen J, Knip M. Autoantibodies associated with type I diabetes mellitus persist after diagnosis in children. Diabetologia 1998;41:1293–1297 [DOI] [PubMed] [Google Scholar]
- 21.Harrison LC, Honeyman MC, Steele CE, et al. Pancreatic beta-cell function and immune responses to insulin after administration of intranasal insulin to humans at risk for type 1 diabetes. Diabetes Care 2004;27:2348–2355 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.