Abstract
Objective:
Nonadherence to antidepressants has been reported to range widely from 10% to 60%. Most adherence studies focus on persistence of use and do not include prescriptions that are not picked up by the patient. The objectives of this study were to determine the rate of unfilled antidepressant prescriptions as well as to identify factors associated with failure to fill these prescriptions.
Method:
This retrospective study used administrative and pharmacy data from a mid-Atlantic managed care organization serving 3.3 million medical members and 1.2 million pharmacy members. Electronic prescriptions for citalopram, duloxetine, sertraline, and venlafaxine sent to pharmacies from July 1, 2007, to June 30, 2009, were matched to pharmacy claims to determine the rate of unfilled antidepressant prescriptions. Patients were ≥18 years of age and had continuous pharmacy coverage from July 1, 2006, to July 31, 2009. Logistic regression was used to assess whether clinical and demographic factors were associated with unfilled electronic prescriptions.
Results:
There were 557 electronically prescribed antidepressants for 267 patients. The rate of unfilled electronic prescriptions was 13.1%, which affected 19.9% of patients. Electronic prescriptions for new users of the antidepressant were 5 times more likely to be unfilled (odds ratio [OR]=5.13; 95% CI, 2.66–9.91; P<.001) than those for previous users. Antidepressant prescriptions for patients aged 18–34 years were most likely to be unfilled (OR=3.72; 95% CI, 1.81–7.67; P<.001).
Conclusions:
Nonadherence to antidepressants is a significant problem with one-fifth of patients never receiving their electronically prescribed antidepressant. Prescriptions for patients without a previous antidepressant claim and aged 18–34 years were least likely to be filled. Interventions targeting patients who fail to fill their antidepressant prescription are needed.
Major depressive disorder is the leading cause of disability in US adults aged 15–44 years and will become the second leading cause of death worldwide by 2020.1,2 Despite being a significant public health problem, depression is underreferred, underdiagnosed, and undertreated.3 Undertreated depression is associated with poorer outcomes in chronic medical diseases such as osteoporosis, diabetes, heart disease, certain cancers, and chronic obstructive pulmonary disease.4–7
Depression is commonly seen in the primary care setting, and the American College of Preventive Medicine recommends that primary care providers screen all adults for depression.8 In the United States, antidepressant use almost doubled from 1996 to 2005.9 Antidepressant medications are used for all severities of depression, and nonadherence to antidepressant therapy has been cited as a main cause of treatment failure.2,10 Many methods used to study adherence, including pharmacy claims analysis, only measure use by users and overlook patients who fail to fill their antidepressant when prescribed.11 First-fill adherence studies in specific patient populations found that 8% of antidepressant prescriptions remain unfilled in US military pharmacies, and 5.4% of Medicare patients report that they do not fill or refill an antidepressant.12,13 In clinical practice, the rate of failure to obtain the first-fill of an antidepressant is largely unknown.
With the recent increase in the use of electronic prescribing across practice settings, a new method to study adherence is available. This study seeks to determine the rate of failure to fill electronically prescribed prescriptions for antidepressants, as well as to understand the factors associated with failure to fill these prescriptions.
Clinical Points
♦Rates of nonadherence to antidepressant therapy are high and may contribute to treatment failure: 1 in 5 patients had ≥ 1 unfilled electronically prescribed prescription for an antidepressant.
♦Patients who are younger and treatment-naive are more likely to be nonadherent to antidepressant medications than older patients and previous users.
♦Clinicians may use data from electronic prescribing records to detect patients who are nonadherent to therapy and conduct outreach.
METHOD
This retrospective study used administrative and pharmacy data from a mid-Atlantic managed care organization (MCO) serving 3.3 million medical members and 1.2 million pharmacy members. To be eligible for inclusion, patients had to have at least 1 electronically prescribed citalopram, duloxetine, sertraline, or venlafaxine prescription between July 1, 2007, and June 30, 2009. These 4 antidepressants were chosen because they were among the top 10 medications paid by the MCO in the first quarter of 2009. There were no restrictions (prior authorizations, step-therapy requirements) that limited access to these antidepressants. During the study period, all medications were available in the generic form except for duloxetine and venlafaxine extended release, which were only available as brand-name formulations.
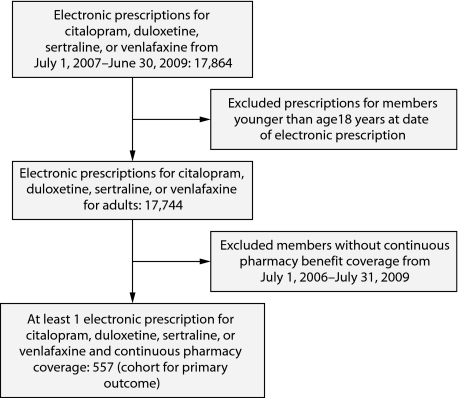
A query of the MCO pharmacy claims database identified all prescription claims (not necessarily electronic) for each of the 4 antidepressants from July 1, 2006, through July 31, 2009 (Figure 1). Patients and their prescription claims were excluded if the patient was younger than age 18 years on the date of the electronic prescription or if the patient did not have continuous enrollment in the same pharmacy benefit plan from July 1, 2006, through July 31, 2009.
Figure 1.
Flowchart for Identification of the Electronic Prescription Cohort
In addition, all antidepressant pharmacy claims within the year prior to the date of the electronic prescription were obtained. For each electronically prescribed antidepressant, it was determined whether the patient was naive to antidepressant therapy, had received another antidepressant within the preceding 12 months, or had received the same antidepressant previously.
The pharmacy claims dataset contained the following fields: unique deidentified patient number, patient age (on date of fill), patient sex, prescription number, date filled, drug name, drug strength, claim number, claim status, claim status description, quantity, copayment, and number of paid days supplied.
Electronic prescriptions were compared to pharmacy claims, and each prescription was categorized as “filled” or “unfilled.” A filled prescription represented one that was approved by the MCO for coverage and was picked up by the patient. Prescriptions designated as unfilled were considered to have not been picked up by the patient and served as a proxy for first-fill nonadherence. A prescription was unfilled if it was “voided,” “denied,” or had no corresponding claim.
A voided claim meant that the prescription had originally been approved by the MCO for coverage, but was later voided by the pharmacist because the patient did not pick up the prescription. This category served as a proxy for patient-directed nonadherence, as the patient was able to obtain the prescription, but failed to do so. Denied claims represent prescriptions that were not approved for coverage by the MCO. This may have occurred if there was inappropriate prescribing (drug interaction, dose too high) or insufficient patient information (ie, no doctor identification, incorrect patient date of birth) that caused the claim to be blocked through insurance processing. Electronic prescriptions had no corresponding claim if the pharmacy did not process the claim through insurance. This may have occurred in several of the following scenarios: the prescription was sent to the wrong pharmacy, and no one followed up to see if the patient received the prescription; the patient never used the pharmacy, so the pharmacist did not have the patient's insurance, and the patient never returned to the pharmacy; the patient paid out of pocket; or the patient did not know that a prescription was sent by the provider.
Outcome Measures
The primary outcome was the percentage of unfilled, first-fill electronic antidepressant prescriptions. To calculate this number, the numerator was the number of unfilled electronic prescriptions, while the denominator was the overall number of electronically prescribed antidepressant prescriptions in the cohort. The secondary outcome measures examined the clinical and demographic factors that increased the likelihood that the electronically prescribed antidepressant was unfilled. Factors of age category, sex, type of insurance coverage, history of antidepressant use, class of antidepressant, and prescriber type were evaluated to determine the relationship with first-fill.
All data conformed to Health Insurance Portability and Accountability Act patient privacy standards, and the University of Maryland Baltimore Institutional Review Board fully approved the research protocol.
Statistical Analysis
Statistical analysis included descriptive statistics such as percentages for discrete variables (eg, sex) and calculations of means and standard deviations for continuous variables (eg, age). Univariate analyses using χ2 tests examined the correlation between clinical and demographic (eg, sex, age) characteristics and filled prescription rates. Binomial logistic regression was used to assess whether there were any predictors of the failure rate. Statistical significance was set at an accepted α of P<.05.
RESULTS
Prescription Cohort
There were 557 electronic prescriptions for 267 patients that met the study criteria (Table 1, Figure 1). There were 2.84 times more prescriptions for females than males. Data showed that 14.7% of prescriptions were for patients who were naive to particular prescribed electronic antidepressant (ie, no paid claim for same prescribed antidepressant filled within last 12 months of electronic prescription date), and 9.9% of prescriptions were for patients who were naive to all antidepressants (ie, no paid antidepressant claim within last 12 months of electronic prescription date) and the majority. Of the electronically prescribed antidepressants, 76.8% were prescribed by primary care physicians; 15.3% were prescribed by other health care providers including practitioners and specialty providers like cardiologists, rheumatologists, neurologists, gynecologists, and gastroenterologists; and 7.9% were prescribed by psychiatrists. The majority (43.4%) of prescriptions were prescribed for patients enrolled in a health management organization.
Table 1.
Demographics and Clinical Characteristics of Prescription and Patient Cohorts
| Variable | Cohort |
| Unique patients, n | 267 |
| Sex, n (%) | |
| Female | 196 (73.4) |
| Male | 71 (26.6) |
| Age at date of first electronic prescription, mean (SD), y | 51.5 (14.1) |
| Age range (minimum–maximum), y | 20–97 |
| Age range breakdown, n (%), y | |
| 18–34 | 34 (12.7) |
| 35–49 | 78 (29.2) |
| 50–64 | 118 (44.2) |
| ≥65 | 37 (13.9) |
| No. of unique electronic prescriptions | 557 |
| Prescription breakdown, no. (%) | |
| Citalopram | 63 (11.3) |
| Duloxetine | 113 (20.3) |
| Sertraline | 209 (37.5) |
| Venlafaxine | 172 (30.9) |
| Prescription breakdown by class, no. (%) | |
| Serotonin-norepinephrine reuptake inhibitor | 272 (48.8) |
| Selective serotonin reuptake inhibitor | 285 (51.2) |
| Prescription breakdown by sex, no. (%) | |
| Female | 412 (74.0) |
| Male | 145 (26.0) |
| Previous therapy (within 1 y prior to date of electronic prescription), no. (%) | |
| New to all antidepressants | 55 (9.9) |
| Another antidepressant only | 27 (4.8) |
| Electronically prescribed antidepressant | 475 (85.3) |
| Type of health plan, no. (%) | |
| Health management organization | 217 (39.0) |
| Preferred provider organization | 204 (36.6) |
| Medicare Part D | 72 (12.9) |
| Indemnity | 64 (11.5) |
| Type of prescriber, no. (%) | |
| Primary care | 428 (76.8) |
| Psychiatrist | 44 (7.9) |
| Other | 85 (15.3) |
Primary Outcome
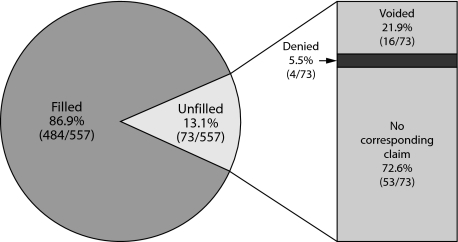
Of the 557 electronic antidepressant prescriptions, 63 were for citalopram, 113 for duloxetine, 209 for sertraline, and 172 for venlafaxine (Table 1). Also, 13.1% (73/557) were categorized as unfilled, and of the unfilled prescriptions, 21.9% (16/73) were voided, 72.6% (53/73) were no corresponding claim, and 5.5% (4/73) were denied (Table 2, Figure 2).
Table 2.
Rates of Filled and Unfilled Electronically Prescribed Antidepressants
| Variable | Cohort |
| Prescriptionsa | |
| Filled, no. (%) | 484 (86.9) |
| Unfilled, no. (%) | 73 (13.1) |
| Denied, no. (% of unfilled) | 4 (5.5) |
| Voided, no. (% of unfilled) | 16 (21.9) |
| No corresponding claim, no. (% of unfilled) | 53 (72.6) |
| Patientsb,c | |
| Filled, n (%) | 238 (89.1) |
| Unfilled, n (%) | 53 (19.9) |
| Denied, n (% of unfilled) | 4 (7.5) |
| Voided, n (% of unfilled) | 15 (28.3) |
| No corresponding claim, n (% of unfilled) | 34 (64.2) |
557 prescriptions.
267 patients.
Numbers of filled plus unfilled patients are greater than 100%, as 23 patients had both filled and unfilled prescriptions.
Figure 2.
All Electronic Antidepressant Prescriptions
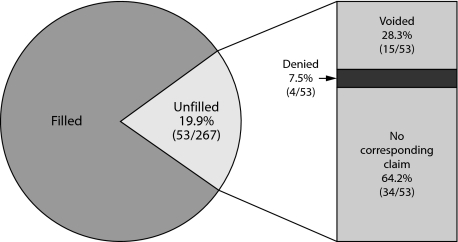
Of the 267 patients, 19.9% (53/267) had at least 1 unfilled prescription. This group consisted of 28.3% (15/53) of patients who were able to obtain their prescription (ie, claim classified as voided) but did not (Table 2, Figure 3).
Figure 3.
Electronic Antidepressant Prescription Rates for Patients (N = 267)
Secondary Outcomes
Demographic, prescription, and insurance coverage characteristics were compared among “filled” and “unfilled” prescriptions (Table 3). Univariate analyses revealed statistically significant differences for age, previous antidepressant use, and type of insurance coverage. No significant differences in prescription outcome were seen by patient sex, antidepressant medication class (serotonin-norepinephrine reuptake inhibitor vs selective serotonin reuptake inhibitor), and prescriber type (primary care vs psychiatrist vs other) (Table 3).
Table 3.
Univariate χ2 Analysis of Filled and Unfilled Electronically Prescribed Prescriptionsa
| Variable | Filled (484) | Unfilled (73) | P |
| Age, yb | .0005 | ||
| 18–34 | 53 (11.0) | 20 (27.4) | |
| 35–49 | 127 (26.2) | 19 (26.0) | |
| 50–64 | 232 (47.9) | 23 (31.5) | |
| ≥65 | 72 (14.9) | 11 (15.1) | |
| Sexc | .15 | ||
| Male | 131 (27.1) | 14 (19.2) | |
| Female | 353 (72.9) | 59 (80.8) | |
| Prior antidepressant history (within 1 y prior to electronic prescription date)d | < .0001 | ||
| Naive to all antidepressants | 34 (7.0) | 21 (28.8) | |
| Previous therapy with other antidepressant only | 23 (4.8) | 4 (5.5) | |
| Previous therapy with electronically prescribed antidepressant | 427 (88.2) | 48 (65.8) | |
| Class of electronically prescribed antidepressante | .55 | ||
| Serotonin-norepinephrine reuptake inhibitor | 250 (51.7) | 35 (47.9) | |
| Duloxetine | 98 (39.2) | 15 (42.9) | |
| Venlafaxine | 152 (60.8) | 20 (57.1) | |
| Selective serotonin reuptake inhibitor | 234 (48.3) | 38 (52.1) | |
| Citalopram | 55 (23.5) | 8 (21.1) | |
| Sertraline | 179 (76.5) | 30 (78.9) | |
| Type of health planf | .032 | ||
| Health management organization | 203 (41.9) | 14 (19.1) | |
| Preferred provider organization | 186 (38.4) | 18 (24.7) | |
| Medicare Part D | 33 (6.8) | 39 (53.4) | |
| Indemnity | 62 (12.8) | 2 (2.7) | |
| Prescriber typeg | .43 | ||
| Primary care | 376 (77.7) | 52 (71.2) | |
| Psychiatrist | 72 (14.9) | 13 (17.8) | |
| Other | 36 (7.4) | 8 (11.0) | |
All data are presented as no. (%).
χ21=17.7815.
χ21=2.0497.
χ21=34.1929.
χ21=0.349.
χ21=8.7745.
χ21=0.2787.
Statistically significant factors from univariate analyses were included in the logistic regression model (Table 4). The independent factors affecting risk of failure to fill electronically prescribed antidepressant medication were patient age and history of antidepressant use. Antidepressants for patients who were naive to electronically prescribed antidepressants were about 5 times more likely to be unfilled when compared to those for patients naive to particular antidepressants (OR=5.13; 95% CI, 2.66–9.91; P<.001). Electronic prescriptions for patients aged 18–34 years were more likely to be “unfilled” (OR=3.72; 95% CI, 1.81–7.67; P<.001) compared to antidepressants for patients aged 50–64 years. Type of health insurance coverage was not independently associated with failure to fill electronically prescribed antidepressants.
Table 4.
Binomial Logistic Regression Analysis: Predictors of Failure to Fill Antidepressant Prescription
| Variable | Statistic | |
| Odds Ratio (95% CI) | P | |
| Age, ya | ||
| 18–34 | 3.72 (1.81–7.67) | <.001 |
| ≥65 | 2.22 (0.94–5.23) | .069 |
| 35–49 | 1.75 (0.88–3.50) | .11 |
| 50–64* | 1 | |
| Previous therapy (within 1 y prior to electronic prescription date)b | ||
| Naïve to all antidepressants | 5.13 (2.66–9.91) | <.001 |
| Previous therapy with other antidepressant only | 1.21 (0.39–3.7) | .74 |
| Previous therapy with electronically prescribed antidepressant* | 1 | |
| Type of health planc | ||
| Indemnity | 3.07 (0.59–15.90) | .18 |
| Health management organization | 2.91 (0.57–14.80) | .20 |
| Preferred provider organization | 1.84 (0.36–9.56) | .47 |
| Medicare Part D* | 1 | |
χ23=13.3981.
χ22=23.8269.
χ23=3.6303.
Reference category=1.
DISCUSSION
Poor adherence to antidepressants has been well documented, but many of these studies excluded patients who never filled their first antidepressant prescription.14–18 We found that 19.9% of patients did not receive their first-fill electronically prescribed antidepressant. In the few studies that have examined first-fill for antidepressants, rates of 4.2%–15% have been reported.12,13,19
New users of antidepressants are a vulnerable group at high risk of being undertreated. Antidepressants for patients who did not have a previous fill within the past year were 5 times more likely to be unfilled. New users may continue to be undertreated, as they are more likely to be nonadherent and also discontinue therapy earlier.19,20 One study observed that treatment-naive patients were 2 times more likely than treatment-experienced patients to prematurely discontinue their antidepressants within the first 30 days.20
Younger patients aged 18–34 years were most likely to have an unfilled prescription out of all age categories. Adherence is of greater concern in this age group, as the mean age of major depression onset and the highest rates of depression occur within this age group.21,22
Past studies have identified successful ways to encourage adherence. A simple question about current or future nonadherence by the clinician may be useful to identify sources of nonadherence and trigger appropriate interventions.23 Simple and specific educational messages easily integrated into primary care visits have also been shown to improve adherence to antidepressant therapy.24 For example, Lin et al24 found that patient adherence increased during the first month of therapy when physicians inquired about patients’ prior antidepressant experience, informed patients of how to take their antidepressant and when to expect noticeable effects, and told patients to continue taking medication even if feeling better and to not stop taking the antidepressant without checking with them. Collaborative care programs that involve nonmedical specialists to augment primary care and care management delivered by primary care clinicians, psychiatrists, psychologists, or nonclinician health educators have also been shown to be effective in improving depression outcomes and medication adherence.25,26
Recognition of patients who do not adhere to medications is complicated by the lack of accurate and affordable objective measures suitable for widespread implementation.27 It is likely that prescribers are unaware of those patients who do not receive their prescriptions since 24% of patients who discontinue antidepressants prematurely fail to inform their physicians.28 Our study utilized electronic prescribing, which may be a useful way to systematically detect and inform prescribers of patients’ nonadherence. A study comparing electronic prescribing records to community pharmacy–dispensing records concluded that adherence problems could be detected if e-pharmacy networks allowed physician practices to match dispensing against prescriptions.29 The authors recommend using electronic prescribing data to enhance chronic care management on a case-by-case basis by physicians to prompt discussion of adherence issues with patients.
Limitations
As a retrospective study, there are several limitations. Only 4 electronically prescribed antidepressants were studied, and these may not be fully representative of all antidepressant medications. Also, patients were not required to have a diagnosis of depression and could be using antidepressants for other indications. The rate of unfilled prescriptions may be greater in uninsured populations or insured populations with gaps in coverage, as these groups are more likely to have unfilled prescriptions.30 The requirement of 3 years of continuous pharmacy coverage limited the study population, and a rolling continuous coverage requirement may have allowed a bigger study cohort.
Furthermore, receiving a prescription does not mean that the patient took the medication as prescribed. This methodology required patients to fill their prescriptions through insurance, and some prescriptions may be paid by cash due to the availability of low-price generics offered by pharmacies. However, unfilled rates were similar for antidepressants when generics were available and when they were not, so, we do not believe this to be a significant limitation, as there was no apparent impact. Also, patients may have filled samples and therefore did not fill their prescriptions, or there may have been a miscommunication between the prescriber and patient as to which pharmacy to send electronic prescriptions. The interpretations of the logistic regression analysis may be limited, as it does not account for dependency of prescriptions for the same patient. However, the primary result of the rate of unfilled prescriptions uses descriptive statistics, which is unaffected by the logistic model. Finally, we did not ascertain the reasons behind patients failing to receive their first-fill antidepressant, and this is an area that requires further research.
CONCLUSION
About one-fifth of patients never receive their antidepressant electronic prescriptions, even though a quarter of these prescriptions are approved for coverage by insurance. Patients aged 18–34 years and new users of prescribed antidepressants are at higher risk for failure to receive their antidepressant prescription. Electronic prescription systems are able to notify clinicians when patients fail to obtain their prescription medication and can target interventions to improve first-fill rates for antidepressants; however, these systems are currently underutilized.
Drug names: citalopram (Celexa, Lexapro, and others), duloxetine (Cymbalta), sertraline (Zoloft and others), venlafaxine (Effexor and others).
Disclosure of off-label usage: The authors have determined that, to the best of their knowledge, no investigational information about pharmaceutical agents that is outside US Food and Drug Administration−approved labeling has been presented in this article.
Financial disclosure: Dr Cooke has served as a consultant to AstraZeneca and Novartis; has received grant/research support from Novartis and Pfizer; has served on the speakers board of and received honoraria from Pfizer; and is a stock shareholder in Pfizer. Drs Xing, DiPaula, and Lee have no personal affiliations or financial relationships with any commercial interest to disclose relative to the article.
Funding/support: None reported.
Acknowledgment: The authors would like to thank Xiaolin Xing, PhD, Fairfax, Virginia, for statistical support. Dr Xing reports no conflicts of interest relevant to the subject of this article.
Footnotes
CME Background
Articles are selected for credit designation based on an assessment of the educational needs of CME participants, with the purpose of providing readers with a curriculum of CME articles on a variety of topics throughout each volume. Activities are planned using a process that links identified needs with desired results.
To obtain credit, read the material and go to PSYCHIATRIST.COM to complete the Posttest and Evaluation online.
CME Objective
- Use electronic pharmacy data to identify patients who do not fill antidepressant prescriptions and provide targeted interventions for nonadherence
Accreditation Statement
The CME Institute of Physicians Postgraduate Press, Inc., is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit Designation
The CME Institute of Physicians Postgraduate Press, Inc., designates this educational activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Date of Original Release/Review
This educational activity is eligible for AMA PRA Category 1 Credit through January 31, 2014. The latest review of this material was December 2010.
Financial Disclosure
All individuals in a position to influence the content of this activity were asked to complete a statement regarding all relevant personal financial relationships between themselves or their spouse/partner and any commercial interest. The CME Institute has resolved any conflicts of interest that were identified. In the past 3 years, Larry Culpepper, MD, MPH, Editor in Chief, has been a consultant and a member of the advisory boards for AstraZeneca, Cephalon, Forest, Pfizer, Wyeth, Eli Lilly, Takeda, Merck, Neurocrine, sanofi, Bristol-Myers Squibb, and Otsuka and has been a member of the speakers panels for Forest, Wyeth, and Pfizer. No member of the CME Institute staff reported any relevant personal financial relationships. Faculty financial disclosure appears at the end of the article.
REFERENCES
- 1.World Health Organization. The World Health Report 2001: mental health: new understanding. new hope. http://www.who.int/whrAccessed February 20, 2010.
- 2.World Health Organization. The World Health Report 2004: changing history, annex table 3: burden of disease in DALYs by cause, sex, and mortality stratum in WHO regions, estimates for 2002. http://www.who.int/whr/2004/en/09_annexes_en.pdfAccessed September 15, 2010.
- 3.Rihmer Z. Can better recognition and treatment of depression reduce suicide rates? a brief review. Eur Psychiatry. 2001;16(7):406–409. doi: 10.1016/s0924-9338(01)00598-3. [DOI] [PubMed] [Google Scholar]
- 4.Brody B.L., Gamst A.C., Williams R.A., et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology. 2001;108(10):1893–1900. doi: 10.1016/s0161-6420(01)00754-0. discussion 1900–1901. [DOI] [PubMed] [Google Scholar]
- 5.Bogner H.R., Morales K.H., Post E.P., et al. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT) Diabetes Care. 2007;30(12):3005–3010. doi: 10.2337/dc07-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lichtman J.H., Bigger J.T., Jr., Blumenthal J.A., et al. American Heart Association Prevention Committee of the Council on Cardiovascular Nursing; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Epidemiology and Prevention; American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research; American Psychiatric Association. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118(17):1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 7.de Voogd J.N., Wempe J.B., Koëter G.H., et al. Depressive symptoms as predictors of mortality in patients with COPD. Chest. 2009;135(3):619–625. doi: 10.1378/chest.08-0078. [DOI] [PubMed] [Google Scholar]
- 8.Nimalasuriya K., Compton M.T., Guillory V.J. Prevention Practice Committee of the American College of Preventive Medicine. Screening adults for depression in primary care: a position statement of the American College of Preventive Medicine. J Fam Pract. 2009;58(10):535–538. [PubMed] [Google Scholar]
- 9.Olfson M., Marcus S.C.National patterns in antidepressant medication treatment Arch Gen Psychiatry 2009668848–856.. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association Practice Guideline for the Treatment of Patients With Major Depressive Disorder (revision): American Psychiatric Association. Am J Psychiatry. 2000;157(4 suppl):1–45. [PubMed] [Google Scholar]
- 11.Vik S.A., Maxwell C.J., Hogan D.B. Measurement, correlates, and health outcomes of medication adherence among seniors. Ann Pharmacother. 2004;38(2):303–312. doi: 10.1345/aph.1D252. [DOI] [PubMed] [Google Scholar]
- 12.Esposito D., Schone E., Williams T., et al. Prevalence of unfilled prescriptions at military pharmacies. J Manag Care Pharm. 2008;14:553–560. doi: 10.18553/jmcp.2008.14.6.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy J., Tuleu I., Mackay K. Unfilled prescriptions of Medicare beneficiaries: prevalence, reasons, and types of medicines prescribed. J Manag Care Pharm. 2008;14(6):553–560. doi: 10.18553/jmcp.2008.14.6.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bull S.A., Hunkeler E.M., Lee J.Y., et al. Discontinuing or switching selective serotonin-reuptake inhibitors. Ann Pharmacother. 2002;36(4):578–584. doi: 10.1345/aph.1A254. [DOI] [PubMed] [Google Scholar]
- 15.Dunn R.L., Donoghue J.M., Ozminkowski R.J., et al. Selective serotonin reuptake inhibitor antidepressant prescribing in primary care in the United Kingdom: a longitudinal analysis. Prim Care Psychiatry. 1998;4:141–148. [Google Scholar]
- 16.Fairman K.A., Drevets W.C., Kreisman J.J., et al. Course of antidepressant treatment drug type, and prescriber's specialty. Psychiatr Serv. 1998;49(9):1180–1186. doi: 10.1176/ps.49.9.1180. [DOI] [PubMed] [Google Scholar]
- 17.Akincigil A., Bowblis J.R., Levin C., et al. Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Med Care. 2007;45(4):363–369. doi: 10.1097/01.mlr.0000254574.23418.f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sirey J.A., Meyers B.S., Bruce M.L., et al. Predictors of antidepressant prescription and early use among depressed outpatients. Am J Psychiatry. 1999;156(5):690–696. doi: 10.1176/ajp.156.5.690. [DOI] [PubMed] [Google Scholar]
- 19.van Geffen E.C., Gardarsdottir H., van Hulten R., et al. Initiation of antidepressant therapy: do patients follow the GP's prescription? Br J Gen Pract. 2009;59(559):81–87. doi: 10.3399/bjgp09X395067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vanelli M., Coca-Perraillon M. Role of patient experience in antidepressant adherence: a retrospective data analysis. Clin Ther. 2008;30(9):1737–1745. doi: 10.1016/j.clinthera.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 21.Hasin D.S., Goodwin R.D., Stinson F.S., et al. Epidemiology of major depressive disorder: results from the National Epidemiology Survey on Alcoholism and Related Disorders. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 22.Office of Applied Studies. (2007). Results from the 2007 National Survey on Drug Use and Health: National findings. DHHS Publication. 2009 http://oas.samhsa.gov/NSDUH/2k7NSDUH/2k7results.cfm#Ch8. Accessed June 30, 2009. [Google Scholar]
- 23.Rickles N.M., Svarstad B.L. Relationships between multiple self-reported nonadherence measures and pharmacy records. Res Social Adm Pharm. 2007;3(4):363–377. doi: 10.1016/j.sapharm.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Lin E.H., Von Korff M., Katon W., et al. The role of the primary care physician in patients’ adherence to antidepressant therapy. Med Care. 1995;33(1):67–74. doi: 10.1097/00005650-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Gilbody S., Bower P., Fletcher J., et al. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 26.Williams JW Jr, Gerrity M., Holsinger T., et al. Systematic review of multifaceted interventions to improve depression care. Gen Hosp Psychiatry. 2007;29(2):91–116. doi: 10.1016/j.genhosppsych.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Bucci K.K., Possidente C.J., Talbot K.A. Strategies to improve medication adherence in patients with depression. Am J Health Syst Pharm. 2003;60(24):2601–2605. doi: 10.1093/ajhp/60.24.2601. [DOI] [PubMed] [Google Scholar]
- 28.Demyttenaere K., Enzlin P., Dewé W., et al. Compliance with antidepressants in a primary care setting, 1: beyond lack of efficacy and adverse events. J Clin Psychiatry. 2001;62(suppl 22):30–33. [PubMed] [Google Scholar]
- 29.Mabotuwana T., Warren J., Harrison J., et al. What can primary care prescribing data tell us about individual adherence to long-term medication? comparison to pharmacy dispensing data. Pharmacoepidemiol Drug Saf. 2009;18(10):956–964. doi: 10.1002/pds.1803. [DOI] [PubMed] [Google Scholar]
- 30.Schoen C., DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health Serv Res. 2000;35(1 pt 2):187–206. [PMC free article] [PubMed] [Google Scholar]