Abstract
Background:
In earlier days, hormone replacement therapy (HRT) was recommended for menopause symptoms and also gained much popularity. However, the Women's Health Initiative (WHI) studies suggested an increased risk of cardiovascular and Alzheimer's disease. These findings led to a dramatic decrease in hormone therapy (HT) prescriptions all over the world. However, the WHI conclusions remain debatable especially because of contradictory results from antecedent studies. Inspite of these controversies, post-WHI, most gynecologists refrain from prescribing MHT (menopausal hormone replacement therapy, MHT). Furthermore, many Indian gynecologists prefer to prescribe alternative treatments that would help alleviate symptoms and thus avoid HRT. We decided to carry out a survey and document the current opinions regarding indications of HRT and alternative therapies and prescribing practices of Jaipur-based gynecologists.
Objective:
This study was designed to find out the current attitudes and practices of gynecologists (Jaipur) towards management of menopause.
Materials and Methods:
A questionnaire concerning attitudes, management strategies, and use of HT was mailed out to gynecologists, and they are asked to complete the questionnaire. Data were analyzed using the total number of respondents (n = 321). The results were analyzed using a simple percentage method as this was most suitable for this kind of studies.
Results:
From the results, 69.04% gynecologists were currently prescribing MHT. Hot flashes were the most common indication for MHT prescriptions and 78.57% were familiar with controversies surrounding WHI study. Also, 61.9% would consider using MHT for themselves. Alternative therapy was adopted by 83.48% in their prescribing practice. The reason cited by 71% for preferring alternative therapies was that it was safer and less controversial.
Conclusions:
The prescribing practices of Jaipur gynecologists in lieu of ongoing controversies surrounding HT have shifted and now also support alternative therapies for menopause management. In this era of phasic prescriptions, for immediate relief of hot flashes and mood swings, MHT was favored. However, for long-term management of women with poor compliance, alternative therapies were considered a safer option.
Keywords: Gynecologists, menopausal hormone replacement therapy, prescribing practices
INTRODUCTION
Initially, hormone replacement therapy (HRT) was recommended for menopause symptoms and also gained much popularity as the “feminine forever” solution, but since then, has been the subject of much controversy and debate. This can largely be attributed to the highly publicized WHI study regarding the effect of hormone therapy (HT) on the risk for several diseases published in July 2002.[1] Generalized interpretations of the findings may have led many women to discontinue therapy.[2] As a consequence of the confusion surrounding the benefits and risks of HT, many women do not seek pharmacological treatment; instead they either tolerate bothersome symptoms or try alternative therapies.[3]
Menopause occurs at an average age of 51.4 years[4] and by 2020, the number of women aged 51 years or older is expected to be around 50 million. This number is expected to grow substantially over the next 10 years as life expectancy increases.[5]
HT remains the standard treatment for moderate-to-severe vasomotor symptoms, vaginal atrophy symptoms,[6] and osteoporosis. The WHI study suggested an increased risk of cardiovascular and Alzheimer's disease. Earlier, it was mainly contraindicated in women with a history of breast cancer, thromboembolism, and menorrhagia. However, the WHI conclusions remain debatable especially because of contradictory results from antecedent studies.
Inspite of these controversies, it has been observed that post-WHI, most gynecologists refrain from prescribing HRT. Furthermore, many Indian gynecologists prefer to prescribe alternative treatment options that would help alleviate symptoms and thus avoid HRT. Treatment protocol still remains a gray area due to varying attitudes of the gynecologists and degree of patients’ awareness regarding menopause. There are lot of articles in the literature regarding prescribing practices of menopause health practitioners in other countries, but not in the Indian scenario. We decided to carry out a survey and document the current opinions regarding indications of HRT and alternative therapies and prescribing practices of Jaipur-based gynecologists.
MATERIALS AND METHODS
We decided to carry out a survey and document the prescribing practices of Indian (Jaipur-based) gynecologists. A questionnaire concerning attitudes, management strategies, and use of HT was drafted and handouts were prepared. These were made available by us at local continuing medical education (CME's) and workshops at the registration counter. Board certified (Medical Council of India) Jaipur gynecologists were invited to complete the questionnaire. Only one response sheet was allowed for each gynecologist. This procedure was adopted to ensure that all response sheets distributed were duly filled up. A total of 321 gynecologists volunteered to complete the questionnaire, and the same were included in the study.
Respondents were required to fill the number of years they were practicing as gynecologists. The place of work, whether a teaching institute, multispeciality hospital, or a private nursing home/consultation chamber. It was optional for the respondents to mention their own names. The respondents were asked whether they prescribed menopausal hormone replacement therapy (MHT) for menopause symptoms, the indications/contraindications, and awareness of WHI study. A section of questions was devoted to alternative therapies. Personal opinions about the present status of MHT, MHT concerns, and need for further large studies to definitively answer when HT should be used in a clinical setting were sought. In some instances, percentages listed in the table do not add up to 100 because of rounding and/or the acceptance of multiple responses and/or the exclusion of “decline to answer” responses. Data were analyzed using the total number of respondents (n = 321). Results were analyzed using simple percentage method as this was most suitable for this kind of studies.
RESULTS
The majority of respondents (85%) prescribed MHT for menopause symptoms. Of these, 69.04% (n = 221) were currently prescribing HRT [Table 1] and 30.96% were not currently prescribing HRT , among which 16.19% (n = 52) had prescribed this therapy in past. However, 14.95% (n = 48) respondents had never prescribed MHT. Respondents were generally active practitioners and regularly updated themselves with CME's and journals. Of the 321 respondents, 45.23% (n = 145) got their updates from medical books and journals; 59.52% (n = 192) updated themselves by attending CME's; 28.57% (n = 95) by media, and 35.71% (n = 112) used Internet for updating themselves. The total percentage of responses for this question is more than 100 because many gynecologists used more than one means to update themselves.
Table 1.
Data from participating gynecologists in response to the questionnaire
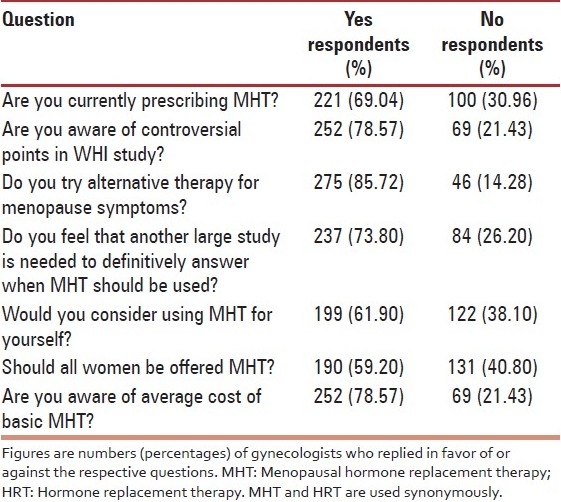
Symptoms related to menopause can include both vaginal atrophy and vasomotor symptoms, which include hot flashes, sleep disturbances, night sweats, anxiety and depression, and mood swings including irritability.[7] Hot flashes are the most common symptom of menopause, occurring in approximately 75% of perimenopausal and postmenopausal women.[8] In our study, 87% of respondents (n = 279) reported that they would prescribe MHT for hot flashes; 72% (n = 231) would prescribe it for mood swings: 84.42% (n = 271) for vaginal atrophy, and 59.81% (n = 192) for osteoporosis prophylaxis [Figure 1]. A desire on the part of the patient to take MHT was also considered as an indication for initiation of therapy by 46% (n = 148). Only 12% felt that they would prescribe MHT for menopause even if the patient personally strongly rejected HT. Regarding contraindications to MHT, all respondents unanimously felt that HRT was contraindicated in deep vein thrombosis, ischemic heart disease, radically treated breast cancer, and radically treated endometrial cancer. Family history of breast cancer was considered a contraindication by 85% and obesity by 15%. When asked about the average cost of basic HRT, 78.57% (n = 252) were aware of the cost while 21.43% (n = 69) were not aware of the average cost.
Figure 1.
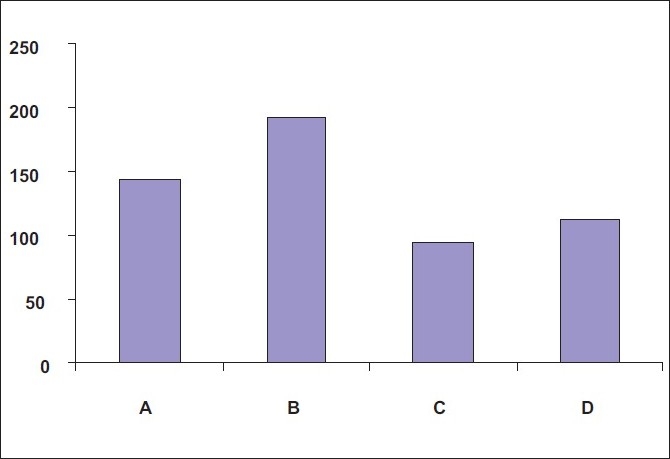
Sources of menopause updates. Figures indicate the number (percentage) of gynecologists who get their updates from the respective source. A = Books; B = CME; C = Magazines; D = Internet
As regards the WHI study, 78.57% (n = 252) of respondents were familiar with the controversial points in the WHI study. Among them, 21.43% reported that they were not aware of the debate surrounding this landmark study. The survey revealed gaps in knowledge on the current research findings in HT. Poor differentiation between results from the estrogen-only treatment arm and the estrogen-plus-progestin treatment arm may account for much of the confusion. Moreover, although initial findings received widespread coverage even in the popular media, less dramatic updates received less attention.[9] When questioned about what concerned them most about MHT, 43% (n = 139) stated inadequate knowledge about present status of HRT and 33% (n = 106) were concerned about the poor safety profile. Poor follow-up and long-term compliance of patients especially in the Indian scenario was the major concern for 24% of the respondents [Figure 2]. Overall 72% (n = 231) had positive current views for MHT, whereas 28% (n = 90) had an overall negative view for MHT.
Figure 2.
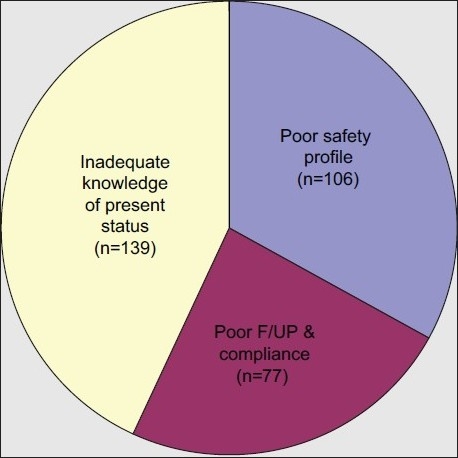
Concerns about MHT. Figures indicate the number of gynecologists who gave the respective reason as their main concern about MHT. MHT = menopausal hormone replacement therapy
Alternative therapy was being adopted in prescribing practice by 83.48% (n = 268). Of all the respondents, 57% (n = 183) used alternative therapies as an adjunct to MHT; 27% (n = 88) used these as the first-line treatment in place of MHT, whereas 16% (n = 50) did not advise alternative therapies to their patients [Figure 3]. The reason sited by 71% (n = 228) of the respondents for preferring alternative therapy was that they felt it was safer and less controversial. Further, 17% (n = 54) preferred it because it was cheaper whereas 12% (n = 38) felt alternative therapies were more effective [Figure 4]. Alternative therapies were felt to be most beneficial in hot flashes by 46% (n = 148). Moreover, 38% respondents (n = 124) felt it was most beneficial in mood swings and 15% (n = 49) felt it to be most beneficial in osteoporosis.
Figure 3.
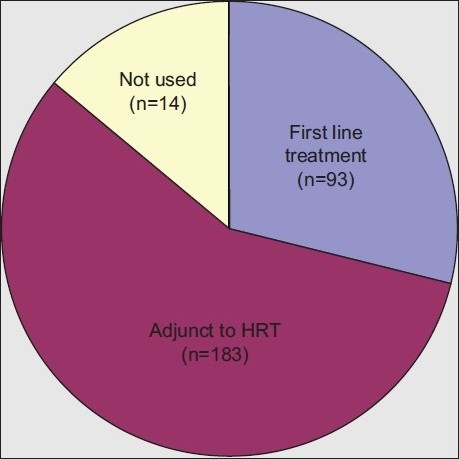
Usage of alternative therapy. Figures indicate the number of gynecologists who use the respective mode for prescribing alternative therapy. HRT = hormone replacement therapy
Figure 4.
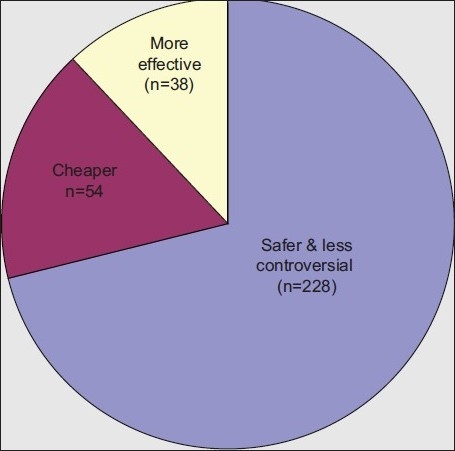
Preference for alternative therapy. Figures indicate the number of gynecologists who gave the respective reason for preferring to prescribe alternative therapy instead of MHT. MHT = menopausal hormone replacement therapy
When attending to a menopause patient in their outpatient clinic, 20.24% (n = 65) said they devoted approximately 5 min for counseling; 59.19% (n = 190) devoted approximately 10 min, and 20.56% (n = 66) devoted more than 10 min for counseling the patient. On an average, 55% (n = 177) respondents felt that percentage of females attending menopause clinic was <50%, whereas 45% (n = 144) felt that surgical menopause composed approximately 50% of the menopause clinic patients. In addition, 59.19% (n = 190) respondents felt that all the patients attending the clinic for menopause-related complaints should be offered MHT for treating the respective problem, whereas 40.80% (n = 131) respondents felt that all such women should not be offered MHT. Interestingly, 61.68% (n = 198) female gynecologists said they would consider using MHT for themselves whereas 38.31% (n = 123) female respondents said they would not use MHT for themselves!
DISCUSSION
The findings of this study in which the most accepted reasons for starting MHT were vasomotor (87%) and urogenital (84.42%) symptoms are consistent with other studies that found vasomotor symptoms to be the most frequently reported symptom among postmenopausal women[9] and the most frequently reported reason for starting MHT.[10] Vasomotor symptoms happen to be the most common presenting complaint and is related to an overall feeling of reduced well-being as earlier reported by a survey of 5213 women aged 39-60 years.[11] Although recent status of MHT indicates osteoporosis to be one of the main indications, only 59.8% felt so in our study. Since prophylaxis for osteoporosis calls for long-term therapy, most gynecologists are wary of prolonged use of MHT post-WHI results.
Previous studies have examined how results from the WHI trials have affected the understanding of the benefits and risks of MHT. Williams et al. studied primary care physicians to assess their understanding of HT as presented in the WHI trials. The results demonstrated that they overestimated the risks associated with HT 67% of the time.[12] Sensationalized coverage of scientific findings can significantly affect prescribing habits and overall acceptance among the general population.[13] This was reflected when prescriptions for HT decreased by 40% after the first WHI data were released.[13] In a country-like India, symptom reporting is affected by factors such as level of education and socioeconomic status. Increasing physician awareness of the different variables that can affect symptom reporting can aid in assessment and determination of treatments.[14] However, till more definitive large-scale trials come up, as indicated by our study and previous studies[15] MHT is being reserved by most gynecologists for treatment of menopause symptoms and not being used as a preventive measure against future complications of heart disease and osteoporosis.
Although most prescribing practices reflect WHI study results, when specifically asked whether they were aware of the WHI study and its controversial points, only 78.57% were aware of the WHI study. This is in contrast to studies reported from abroad stated that 97.2%,[16] 93.6%,[17] and more than 95%,[18] respectively, of gynecologists/physicians were aware of the WHI study.
We found 85% of gynecologists to be prescribing alternative therapies. A study published in 2005[17] showed 18.2% of gynecologists prescribing tibolone or alternative therapies (29.5%). A subsequent study in 2007[19] showed 55.2% gynecologists opting for biphosphonates, tibolone, and SERMS. Further, 46.3% used tranquilizers, isoflavones, and other natural medications for osteoporosis and 71% gynecologists in Jaipur had shifted to alternative therapies because they felt it was safer and less controversial. Similarly, the study carried out in Brazil in 2007[19] showed an increased risk of breast cancer to be the reason for gynecologists not going for MHT in 62.3% cases. Interestingly, it was noted that gynecologists who considered alternative therapies as viable options were more likely to report that they found WHI trial results more convincing.[20] Our study reflected the conclusions drawn by Lukes et al.[21] that risks of long-term HRT outweighed benefits, therefore MHT should not be initiated or continued for primary prevention of coronary heart disease in postmenopausal females.
CONCLUSIONS
Nowadays, MHT is being reserved by majority of gynecologists for treatment of menopause symptoms and not as a preventive measure against future complications of heart disease and osteoporosis. The prescribing practices of gynecologists in Jaipur in lieu of ongoing controversies surrounding HT have shifted and now also support alternative therapies for menopause management. In this era of phasic prescriptions, for immediate relief of hot flashes and mood swings, MHT was favored. However, for long-term management of women with poor compliance, alternative therapy was considered a safer option. We suggest an individualized approach with careful consideration of benefits and risks. Broad-based, multicentric, nationwide surveys are warranted to give the current scenario of menopausal practice in India.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Womens Health Initiative randomized controlled trial. JAMA. 2002;288:321–33. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 2.Ettinger B, Grady D, Tosteson AN, Pressman A, Macer JL. Effect of Womens Health Initiative on women's decision to continue postmenopausal hormone replacement therapy. Obstet Gynecol. 2003;102:1225–32. doi: 10.1016/j.obstetgynecol.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Haimov-Kochman R, Hochner-Celnekier D. Hot flashes revisited: Pharmacological and herbal options for hot flashes management. What does the evidence tell u? Acta Obstet Gynecol Scand. 2005;84:972–9. doi: 10.1111/j.0001-6349.2005.00769.x. [DOI] [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services, Center for Disease Control and Prevention, National Vital Statistics Reports. [Last accessed on 2004 Nov 10];53(6) Available from: http://www.cdc.gov/nchs/data/nvsr/nvsr53/nvsr53-06.pdf . [Google Scholar]
- 5.North American Menopause Society. Menopause Practice. NAMS Clinicians Guide. [Last accessed on 2007]. Available from: http://www.menopause.org/edumaterials/cliniciansguide/cliniciansguidetoc.htm .
- 6.North American Menopause Society. Estrogen and progestogen use in peri- and postmenopausal women: March 2007 position statement of The North American Menopause Society. Menopause. 2007;14:168–82. doi: 10.1097/gme.0b013e31803167ab. [DOI] [PubMed] [Google Scholar]
- 7.Merck Source Medical Encyclopedia. [Last accessed on 2006 Feb 27]. Available from: http://www.mercksource.com/pp/us/cns-hl-adam.jspzQzpgzEzzSzppdocszSzuszSzcnszSzcontentzSzadamSzencyzSzarticlezSz000894zPzhtm .
- 8.Kroenberg R. Hot flashes: Epidemiology and physiology. Ann N Y Acad Sci. 1990;592:52–86. doi: 10.1111/j.1749-6632.1990.tb30316.x. [DOI] [PubMed] [Google Scholar]
- 9.Belchetz PE. Hormonal treatment of postmenopausal women. N Engl J Med. 1994;330:1062–71. doi: 10.1056/NEJM199404143301508. [DOI] [PubMed] [Google Scholar]
- 10.Grady D, Ettinger B, Tosteson AN, Pressman A, Macer JL. Predictors of difficulty when discontinuing postmenopausal hormone therapy. Obstet Gynecol. 2003;102:1233–9. doi: 10.1016/j.obstetgynecol.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 11.Oldenhave A, Jaszmann LJ, Haspels AA, Everaerd WT. Impact of climacteric on well being: A survey based on 5213 women 39-60 years old. Am J Obstet Gynecol. 1993;168:772–80. doi: 10.1016/s0002-9378(12)90817-0. [DOI] [PubMed] [Google Scholar]
- 12.Williams RS, Christie D, Sistrom C. Assesment of the understanding of the risks and benefits of HRT in primary care physicians. Am J Ostet Gynecol. 2005;193:551–8. doi: 10.1016/j.ajog.2005.03.061. [DOI] [PubMed] [Google Scholar]
- 13.Archer DF. Medical decisions regarding hormone therapy for menopausal women are significantly influenced by the media. Pharmacoepidemiol Drug Saf. 2007;16:28–31. doi: 10.1002/pds.1342. [DOI] [PubMed] [Google Scholar]
- 14.Gold EB, Sternfeld B, Kelsey JL, Brown C, Mouton C, Reame N, et al. Relation of demographic and lifestyle factors to symotoms in a multi-racial/ethnic population of women 40-55 years of age. Am J Epidemiol. 2000;152:463–73. doi: 10.1093/aje/152.5.463. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan B, Yogev Y, Orvieto R, Hirsch M, Fisher M, Rabinerson D. Effect of the WHI study on the attitude of Israeli gynecologists to hormonal therapy during menopause. Clin Exp Obstet Gynecol. 2004;31:267–8. [PubMed] [Google Scholar]
- 16.Blümel JE, Castelo-Branco C, Chedraui PA, Binfa L, Dowlani B, Gómez MS, et al. Patients and clinicians’ attitudes after the Women's Health Initiative study. Menopause. 2004;11:57–61. doi: 10.1097/01.GME.0000075503.60230.61. [DOI] [PubMed] [Google Scholar]
- 17.Nassar AH, Abd Essamad HM, Awwad JT, Khoury NG, Usta IM. Gynecologists’ attitudes towards hormone therapy in the post “Women's Health Initiative” study era. Maturitas. 2005;52:18–25. doi: 10.1016/j.maturitas.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Kang BM, Kim MR, Park HM, Yoon BK, Lee BS, Chung HW, et al. Attitudes of Korean clinicians to postmenopausal hormone therapy after the Women's Health Initiative study. Menopause. 2006;13:125–9. doi: 10.1097/01.gme.0000191211.51232.9d. [DOI] [PubMed] [Google Scholar]
- 19.Lazar F, Jr, Costa-Paiva L, Morais SS, Pedro AO, Pinto-Neto AM. The attitude of gynecologists in Sao Paulo, Brazil 3 years after the Women's Health Initiative study.Women's Health Initiative study. Maturitas. 2007;56:129–41. doi: 10.1016/j.maturitas.2006.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Power ML, Anderson BL, Schulki J. Attitudes of obstet- gynecologists towards the evidence from the Women's Health Initiative study hormone therapy trials remain generally skeptical. Menopause. 2009;16:438–41. doi: 10.1097/gme.0b013e31818fc36e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lukes A. Evolving issues in the clinical and managed care settings on the management of menopause following the Women's Health Initiative. J Manag Care Pharm. 2008;14:7–13. doi: 10.18553/jmcp.2008.14.S3-A.7. [DOI] [PMC free article] [PubMed] [Google Scholar]


