Abstract
Vertebrate haematopoietic stem cells (HSCs) give rise to a hierarchically organised set of progenitors for erythroid, myeloid, lymphoid and megakaryocyte lineages, and are responsible for lifelong maintenance of the blood system. Dysregulation of the haematopoietic differentiation programme is at the origin of numerous pathologies, including leukaemias. With the discoveries that many transcriptional regulators and signalling pathways controlling blood cell development are conserved between humans and Drosophila melanogaster, the fruit fly has become a good model for investigating the mechanisms underlying the generation of blood cell lineages and blood cell homeostasis. In this review article, we discuss how genetic and molecular studies of Drosophila haematopoiesis can contribute to our understanding of the haematopoietic niche, as well as of the origin and/or progression of haematopoietic malignancies in humans.
Transient and definitive haematopoiesis in mammals and Drosophila
Vertebrate haematopoietic stem cells (HSCs) ensure continuous haematopoietic cell production throughout life. HSCs can be defined by their dual ability to self-renew, thereby maintaining their numbers, and to differentiate into all lineages of the blood and immune system (Dykstra et al., 2007). Blood cells first appear in the mammalian conceptus, in the extraembryonic yolk sac, concomitant with the developing vasculature. These early haematopoietic progenitors are, however, of more limited potency than adult HSCs. In mice, HSCs that confer complete, long-term, multilineage haematopoietic repopulation of irradiated recipient mice first appear at embryonic day (E)10.5 in the aorta-gonad-mesonephros (AGM) region of the embryo body and the placenta, and they seed the fetal liver and the adult bone marrow. There is a rapid and permanent perinatal shift of the entire haematopoietic system to the bone marrow (Mikkola and Orkin, 2006; Dzierzak and Speck, 2008).
The decisions of HSCs to self-renew or differentiate, and to become quiescent or proliferate, are tightly controlled by integrating extrinsic cues provided by the niche. The concept of the niche was coined more than 30 years ago to describe the structural and regulatory microenvironment that sustains long-term renewal of bone marrow HSCs (Schofield, 1978). Recent studies, including the successful detection of HSCs in the bone marrow of live animals by using real-time imaging technology, support the view that there are two subpopulations of HSCs: one that is quiescent [also referred to as dormant, reserved or long-term (LT) HSCs], and the other that is more actively cycling [also referred to as primed, activated or short-term (ST) HSCs] (Wilson et al., 2008; Lo Celso et al., 2009; Xie et al., 2009). Primed HSCs provide ongoing support for the daily normal regeneration of billions of blood cells, whereas dormant HSCs that have maximal, long-term reconstitution potential are mobilised upon bone marrow injury (Wilson et al., 2008; Trumpp et al., 2010).
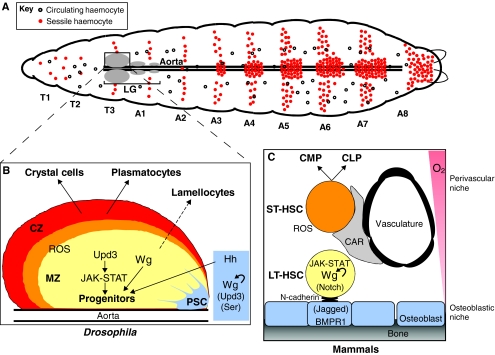
Similarly to vertebrates, Drosophila haematopoiesis occurs in two spatially and temporally distinct phases (Crozatier and Meister, 2007). The Drosophila life cycle comprises an embryonic stage, three larval stages and metamorphosis, which gives rise to an adult. The first embryonic phase provides two types of circulating blood cells (haemocytes) – the plasmatocytes and the crystal cells (see below) – both of which subsist in the larva either in the haemolymph or attached to the inner epidermis in the case of sessile haemocytes (Holz et al., 2003; Honti et al., 2010). The second phase of haematopoiesis takes place in larvae, in a specialised haematopoietic organ known as the lymph gland (LG), which is situated along the anterior part of the dorsal aorta (Lanot et al., 2001) (Fig. 1A). The LG contains haematopoietic progenitors (pro-haemocytes) for three types of functional haemocytes: first, the plasmatocytes, which are monocyte-like cells involved in phagocytosis of apoptotic bodies and pathogens, and, second, the crystal cells, which are required for melanisation, an insect-specific immune and wound-healing response. These two haemocyte types are released in the haemolymph upon dispersal of the LG at the onset of metamorphosis. The LG also gives rise to a third type of haemocyte, the lamellocytes, which are devoted to encapsulation of foreign bodies that are too large to be phagocytosed. Lamellocytes do not differentiate in normal developmental conditions but only in response to specific immune challenges such as wasp parasitism (Rizki and Rizki, 1984; Lanot et al., 2001; Crozatier and Meister, 2007), stress conditions mediated by an increase of reactive oxygen species (ROS) and mutant backgrounds in which their massive proliferation leads to the formation of ‘melanotic tumours’ that result from encapsulation of Drosophila tissue by lamellocytes (see below).
Fig. 1.
Parallels in haematopoiesis between the Drosophila LG and mammalian bone marrow. (A) Schematic representation of a Drosophila third instar larva, illustrating the presence of circulating and sessile haemocytes of embryonic origin, and showing the position of the larval haematopoietic organ (the LG) along the dorsal aorta. T and A refer to thoracic and abdominal segments, respectively, and are numbered along the anterior-posterior axis. (B) The primary lobe of the LG consists of the PSC (blue), the MZ (yellow; containing haemocyte progenitors) and the CZ (red), in which differentiation of plasmatocytes and crystal cells takes place. Lamellocytes only differentiate in response to specific immune threats, at the expense of progenitors. There also exists a population of intermediate progenitors that have left the MZ (found within the orange region). Signalling pathways that are active in the PSC and MZ are indicated. Tightly controlled levels of ROS sensitise haemocyte progenitors to differentiation. Unpaired 3 (Upd3) is one activator of the JAK-STAT pathway, and Serrate (Ser) and Jagged are ligands of the Notch receptor. Their specific roles in the niche remain little understood. (C) Schematic representation of the quiescent LT-HSCs and primed (activated) ST-HSCs and their niches in mammalian bone marrow. Signalling pathways involved in the communication between HSCs and their niches are indicated. Common lymphoid and common myeloid precursors are indicated as CLP and CMP, respectively. Curved arrows indicate cell-autonomous effects within the PSC (B) or in LT-HTCs (C).
The mature Drosophila LG is composed of a pair of anterior (primary) lobes, and several small posterior (secondary) lobes, which contain immature pro-haemocytes. The primary lobes are organised into a medullary zone (MZ) composed of pro-haemocytes, a cortical zone (CZ) containing differentiated haemocytes, and the so-called posterior signalling centre (PSC) (see below for details) (Lebestky et al., 2003; Jung et al., 2005) (Fig. 1B). A pool of mitotically active intermediate progenitors appears at the onset of haemocyte differentiation and accounts for the increasing number of differentiated haemocytes in the mature LG (Krzemien et al., 2010a; Krzemien et al., 2010b). The PSC cells were initially identified by their expression of the Notch ligand Serrate (Ser) (Lebestky et al., 2003). A turning point in the use of Drosophila as a model for haematopoiesis and haematopoietic disorders was the discovery that the PSC plays a key function in controlling larval blood cell homeostasis (Krzemien et al., 2007; Mandal et al., 2007). Specifically, the PSC cells act in a non-cell-autonomous manner to maintain the activity of the Hedgehog (Hh) and JAK-STAT signalling pathways in pro-haemocytes, thereby preserving their multipotent character. This key role of the PSC in supporting Drosophila blood cell homeostasis revealed unanticipated parallels with the HSC niche in mammalian bone marrow (Krzemien et al., 2007; Mandal et al., 2007).
Drosophila as a model to study the haematopoietic niche
The concept that the niche can provide structural and trophic support as well as appropriate signals to regulate stem cell function was first proposed from work on haematopoiesis (Schofield, 1978), but it gained strong experimental and conceptual support from studies in Drosophila germline stem cells (Xie and Spradling, 2000). Recent studies indicate that detailed characterisation of stem-cell–niche interactions will help to understand the pathology of human cancers such as acute myeloid leukaemia (AML) (Box 1). Despite intensive HSC studies in humans and in vertebrate models, characterisation of the HSC niche has progressed slowly, mainly owing to the complex anatomy of bone marrow. Recent data have led to a model in which quiescent and primed stem cells interact with two different microenvironments: the endosteal surface covered by immature osteoblasts (the ‘osteoblastic niche’), which favours long-term quiescence, and the sinusoidal vessels of the central bone marrow (the ‘vascular niche’), which favours proliferation of HSCs (Fig. 1C) (Trumpp et al., 2010). The vessels and endosteal surfaces are intimately entwined within trabecular bone and might play a coordinated and interrelated role, rather than having binary functions.
Box 1. Understanding the hematopoietic niche supports studies of cancer.
Seminal studies of acute myeloid leukaemia (AML), an aggressive malignancy of immature haematopoietic cells in the bone marrow, suggested that AML ‘leukaemic stem cells’ (LSCs) arose from HSCs (Bonnet and Dick, 1997; Reya et al., 2001). This led to the cancer stem cell (CSC) hypothesis that proposed that many human cancers are organised in cellular hierarchies, similar to normal tissues. At the hierarchy apex are multipotent, largely quiescent, long-lived CSCs with self-renewal capacity that sustain disease (Bonnet and Dick, 1997). Investigation of a large number of human AML samples has recently shown that haematopoietic progenitors, rather than HSCs, could be the origin of LSCs. The most important aspect is the ability of LSCs to self-renew, a crucial property of stem cells (Goardon et al., 2011; Majeti and Weissman, 2011). Mouse xenograft models of acute lymphoblastic leukaemia (ALL) recently showed that leukaemic proliferation in bone marrow alters the stromal microenvironment and creates ‘malignant niches’ that out-compete native HSCs. Normal HSCs engaged by the malignant niche exhibit abnormal behaviour, and AML LSCs that home to and engraft within the osteoblastic niche are protected from chemotherapy-induced apoptosis. These findings raise many questions about the nature of the dysfunction of stem and/or progenitor cells and their niche in cancer, as well as related questions about therapy selection and/or intensification (Colmone et al., 2008).
Genetic, transgenic and molecular studies in mice that made use of promoters and inducible systems that are specific to the osteoblastic lineage have uncovered several signalling pathways that are involved in the communication between HSCs and their niche(s) (Table 1 and Fig. 1C). In brief, dormant HSCs and osteoblasts bind via homotypic N-cadherin interactions. Expression of angiopoietin-1 and osteopontin by osteoblasts contributes to both the adhesion of HSCs to the osteoblastic niche and to HSC quiescence (Arai et al., 2004; Nilsson et al., 2005). Enforced expression of the Wnt inhibitor Dickkopf1 in osteoblasts showed that Wnt pathway activation in the niche is required to limit HSC proliferation and thereby to preserve HSC self-renewal capacity and longevity following repeated expansion (Fleming et al., 2008). Parathyroid hormone (PTH) signalling in osteoblasts leads to an increased number of HSCs, probably mediated through high expression levels of the Notch ligand Jagged1 in osteoblasts (Calvi et al., 2003). Conversely, signalling by bone morphogenic proteins (BMPs) controls the number of HSCs by regulating the number of osteoblastic cells (Zhang et al., 2003). Finally, CXC-chemokine ligand 12 (CXCL12) produced by the reticular cells [CXCL12-abundant reticular (CAR) cells] surrounding the sinusoidal endothelial cells is required for maintaining the primed HSC pool. The interconnections between Wnt, PTH, CXCL12 and Notch signalling, however, remain unclear.
Table 1.
Conserved proteins with important roles in haematopoiesis
| Drosophila function | Mammalian function | |
|---|---|---|
| Transcription factors and cofactorsa | ||
| Srp (GATA) | Specification of haemocytes; progenitor maintenance (Lebestky et al., 2000; Lebestky et al., 2003; Tokusumi et al., 2010) | Maintenance of HSCs; lineage commitment; regulation of differentiation (Orkin and Zon, 2008; Braun and Woollard, 2009) |
| Lz (RUNX) | Specification of haemocytes (Lebestky et al., 2000; Lebestky et al., 2003) | Maintenance of HSCs; lineage commitment; regulation of differentiation (Wang et al., 2010) |
| Ush (FOG) | Specification of haemocytes; differentiation of lamellocytes (Lebestky et al., 2000; Sorrentino et al., 2007) | Lineage commitment; regulation of differentiation (Tsiftsoglou et al., 2009) |
| Col (EBF) | Maintenance of PSC cells (Crozatier et al., 2004; Krzemien et al., 2007) | B-cell differentiation; maintenance of the niche (Lin and Grosschedl, 1995; Kieslinger et al., 2010) |
| Antp (HOX) | Formation of the PSC (Jung et al., 2005) | HSC proliferation and self-renewal; myelopoiesis; B lymphopoiesis (Argiropoulos and Humphries, 2007) |
| Signalling pathwaysa | ||
| Notch | Differentiation of crystal cells (Lebestky et al., 2003) | Maintenance of HSCs; haematopoietic regeneration; regulation of differentiation (Weber and Calvi, 2010; Renstrom et al., 2010) |
| Hedgehog | Maintenance of pro-haemocytes (Mandal et al., 2007) | Lineage commitment; regulation of differentiation (Hofmann et al., 2009; Campbell et al., 2008; Gao et al., 2009) |
| Wingless (WNT) | Proliferation of PSC cells; maintenance of pro-haemocytes; differentiation of crystal cells (Sinenko et al., 2009) | Maintenance and proliferation of HSCs; regulation of B- and T-cell differentiation (Grigoryan et al., 2008) |
| JAK-STAT | Maintenance of pro-haemocytes; differentiation of lamellocytes (Krzemien et al., 2007; Harrison et al., 1995; Luo et al., 1995) | HSC renewal during regeneration; lineage commitment (Chung et al., 2006) |
| ROS/FoxO | Maintenance of pro-haemocytes (Owusu-Ansah and Banerjee, 2009) | Maintenance of HSCs; differentiation of erythroid cells (Tothova et al., 2007) |
| Pvf (PDGF/VEGF) | Differentiation of plasmatocytes (Jung et al., 2005) | Maintenance of HSCs (VEGF) (Gerber and Ferrara, 2003) |
Mammalian genetic or functional homologues are shown in parentheses.
Despite the tremendous amount of information gathered from these investigations, our knowledge about the niche and its function remains fragmentary. New approaches are necessary to determine how the integration of different signalling pathways in the niche maintains HSCs. Many transcriptional regulators and signalling pathways involved in haematopoiesis are conserved between humans and Drosophila (Table 1 and Fig. 1B,C). Therefore, the Drosophila PSC, which controls the differentiation of pro-haemocytes in a non-cell-autonomous manner, represents an interesting, genetically tractable model with which to study signal integration and crosstalk during blood cell development.
PSC cells are specified in the embryo by the expression of two transcription factors, the homeotic protein Antennapedia (Antp) and Collier (Col), the Drosophila orthologue of early B-cell factors (EBFs) (Crozatier et al., 2004; Mandal et al., 2007). In the absence of Col activity, the PSC is not specified and larval pro-haemocytes are not maintained, and differentiate prematurely. Mouse EBF2 was recently shown to act in osteoblastic cells and to regulate the maintenance of HSCs, in part by modulating Wnt signalling (Kieslinger et al., 2010). This finding is particularly interesting given that Wingless (Wg; the Drosophila orthologue of Wnt) signalling has been shown to control both the number of PSC cells and the maintenance of pro-haemocytes (Sinenko et al., 2009). PSC cells also express the morphogen Hh, and Hh signalling is required to maintain haemocyte homeostasis in the LG (Mandal et al., 2007). Finally, Ser-mediated Notch signalling from the PSC is required to maintain normal Col expression levels and activity in the PSC (Krzemien et al., 2007) (Fig. 1B). How Hh, Wg, Notch and other signalling outputs are integrated in PSC cells to control JAK-STAT signalling activity in pro-haemocytes and to control blood homeostasis is now being addressed in several laboratories. Our recent studies of the LG have uncovered a previously unidentified mode by which JAK-STAT signalling is regulated, involving a non-signalling dominant-negative form of a cytokine receptor (Makki et al., 2010). Ongoing characterisation and genetic manipulation of PSC function in controlling Drosophila haematopoiesis are thus expected to provide clues as to how the mammalian bone marrow niche controls the balance between HSC self-renewal and differentiation.
ROS levels in regulating haematopoiesis: a Drosophila case
The functional difference between the osteoblastic and vascular niches in mouse bone marrow might be related to oxygen availability: oxygen levels are probably higher in the vascular niche, whereas the LT-HSC osteoblastic niche is hypoxic (Parmar et al., 2007; Simsek et al., 2010). A low-oxygen microenvironment could be essential for the maintenance of HSCs and for their protection from detrimental ROS accumulation (Jang and Sharkis, 2007), whereas a high-oxygen microenvironment could favour proliferation (for a review, see Eliasson and Jonsson, 2010). Notably, the forkhead O (FoxO) transcription factors play essential roles in preserving quiescence and enhancing survival of HSCs in the bone marrow through regulating the response to physiological oxidative stress (Tothova et al., 2007), although how this regulation is exerted remains poorly understood. The distinct metabolism of HSCs [and probably also leukaemic stem cells (Box 1)], which utilise glycolysis instead of mitochondrial oxidative phosphorylation, does indeed reflect their location in a hypoxic niche (Simsek et al., 2010). Notably, quiescent leukaemic cells that reside in the hypoxic endosteum are resistant to radio- and chemotherapy (Ishikawa et al., 2007; Richardson, 2011). The link between ROS levels and HSC survival therefore contributes to understanding the connection between ROS levels in cancer stem cells (Box 1) and the resistance of tumours to radiation (Diehn et al., 2009).
Owusu-Hansa and Banerjee (Owusu-Ansah and Banerjee, 2009) established the role of ROS in the control of Drosophila haematopoiesis, revealing that the accumulation of ROS in the LG is tightly controlled during development. This report showed that ROS levels in pro-haemocytes are an intrinsic factor that sensitises these progenitors to differentiation. Furthermore, they found that there is a tight correlation between FoxO overactivation and the downregulation of Polycomb (an epigenetic silencer) in cells with high ROS levels; this is in agreement with a previous report that showed that repressing the activity of a Polycomb protein provoked abnormal lamellocyte differentiation (Remillieux-Leschelle et al., 2002). Drosophila haematopoiesis is thus an excellent model in which to study the tight developmental control of ROS levels that might play a key role in the transition from HSCs to myeloid progenitors in mammals (Tothova et al., 2007). Similar studies might also be useful for dissecting how signalling via ROS is connected to other signalling pathways, such as the Wg and JAK-STAT pathways required for pro-haemocyte maintenance in the LG (Sinenko et al., 2009; Makki et al., 2010). This would provide a more integrated view of how haematopoiesis is controlled in different environmental conditions.
Using Drosophila to identify new oncogene partners
Drosophila can provide a valuable in vivo screening platform for modifiers, enhancers or suppressors of human oncogenic protein function, as illustrated by studies of AML. The pathogenesis of AML is considered to involve multistep genetic alterations in several genes that predispose or promote leukaemias [for a recent WHO classification, see Dohner et al. (Dohner et al., 2010)]. Analyses of chromosomal translocations in the bone marrow of AML patients have shown that several transcription factors that are crucial for haematopoiesis also play important roles in leukaemogenesis. These include AML1, LMO2, SALL, MLL and SCl/Tal1, all of which are proteins with clearly identified Drosophila orthologues (FlyBase; http://flybase.org/).
The t(8;21) (q22;q22) chromosomal translocation, which creates the AML1-ETO fusion product (see below), is found in ∼12% of AML patients. Under normal conditions, AML1, a RUNX-domain protein, acts as a tissue-specific transcriptional activator at multiple steps during haematopoiesis, whereas ETO (also known as RUNX1T1 and MTG8) functions as a transcriptional repressor. The commonly accepted view is that the AML1-ETO fusion product acts as a constitutive repressor of AML1 protein function and inhibits myeloid differentiation while promoting proliferation of multilineage progenitors. Interestingly, the Drosophila RUNX protein Lozenge is required for the differentiation of crystal cells. Two independent groups expressed human AML1-ETO in Drosophila haemocyte precursors and showed that this results in increased proliferation of circulating progenitors, the formation of ‘melanotic tumours’ or ‘pseudotumours’ and prevention of crystal cell differentiation. Both groups then performed genetic screens to identify modifiers of these blood phenotypes, which could potentially be modulators of the human leukaemogenic protein. One group revealed that mutations in components of the Wnt4-Frizzled and Ca2+ signalling pathways increased AML1-ETO activity (Sinenko et al., 2010). The other group identified eight suppressor candidates, including Calpain B (CalpB), a Ca2+-dependent protease (Osman et al., 2009). Functional analysis of CalpB revealed that it is required to stabilize AML1-ETO in the nucleus. Interestingly, CalpB was also found to interact with AML1-ETO in human cells (Osman et al., 2009), opening up the possibility that it might have a role in regulating leukaemogenesis. This functional study provides proof of principle that expression of human oncogenic factors in Drosophila haemocytes can help to identify core regulatory networks whose dysregulation in humans contributes to the development of leukaemias.
Advantages of Drosophila as a model for haematopoiesis and leukaemias.
Drosophila is amenable to genetic and transgenic manipulations. Homologous recombination and targeted RNAi technologies are routinely used, both in vivo and in cell culture assays. Large collections of mutants and double-stranded RNA (dsRNA) libraries are available.
Drosophila has a very short generation time and is easy to maintain in large populations that are convenient for large-scale genetic screens as well as transcriptome, proteome and interactome analyses.
The genomic sequences of 12 Drosophila species and of several Diptera of medical interest (mosquitoes) are available. This allows a high precision of sequence comparison of coding and regulatory regions between these species and mutants, or of variants within a given species.
The problem of functional redundancy that is often encountered when studying human genes owing to vertebrate genome duplications is minimised in Drosophila.
Drosophila models of leukaemia created by expressing human oncogenic or abnormal proteins can be used to search for new genetic regulators.
As noted above, AML1-ETO expression in Drosophila provokes an increased proliferation of haemocyte precursors and the formation of melanotic tumours or pseudotumours (Osman et al., 2009; Sinenko et al., 2010). Such tumours were previously observed in a gain-of-function mutation affecting the kinase domain of the Hopscotch kinase (Hoptuml mutation), the Drosophila JAK-STAT kinase (Harrison et al., 1995; Luo et al., 1995). Furthermore, misexpression of a dominant-active form of the transcriptional effector of the pathway, STAT92E (STAT92EΔNΔC mutation) also promotes tumorigenesis (Ekas et al., 2010). Together with the key role of JAK-STAT signalling in the maintenance of pro-haemocytes in the LG (Makki et al., 2010), these tumorous phenotypes could be particularly relevant to the study of human leukaemias, because mutations and translocations of JAK genes are associated with a variety of haematopoietic malignancies (Bromberg et al., 1999; Vainchenker et al., 2008; Mullighan et al., 2009). For example, an activating mutation in the human tyrosine kinase JAK2 (JAK2V617F) is responsible for various forms of myeloid leukaemia. Mouse models have confirmed that this mutation causes myeloproliferative neoplasms and has differential effects on HSCs and myeloid progenitor cells (Levine et al., 2005; Mullighan et al., 2009; Mullally et al., 2010). It is therefore possible that the constitutive activity of conserved components of the JAK-STAT pathway can be used in RNAi screens to identify in vivo suppressors of JAK-STAT activity. Such suppressors might have conserved functions in restricting acute lymphoblastic leukaemia (ALL) or AML progression in humans and could provide potential targets for therapeutic intervention.
Conclusions
For the past 30 years, Drosophila melanogaster has been a central model for understanding the genetic and molecular bases of animal development. During this period, new genetic and genomic resources and technologies have been developed that allow tissue-specific knockdown of gene expression, gene replacement and site-specific integration of modified and/or exogenous genes in the Drosophila genome. The recent description of Drosophila haematopoietic stem-like cells and their niche – and the accumulating evidence that many of the basic pathways and processes are also present in vertebrates – establishes Drosophila as a model for studying the genetic aspects of haematopoiesis and haematopoietic disorders.
A new repressible binary expression system for transgene expression, the Q system, has recently been developed (Potter et al., 2010). The combination of the Q system and the previously established GAL4 inducible system will allow the development of strategies for manipulating transgene expression in different cell types in the same fly. This opens the prospect of manipulating gene expression and/or signalling activities in vivo, simultaneously in HSCs and niche cells, and decrypting their reciprocal communication under physiological and pathological conditions. Large-scale screens for melanotic-tumour suppressor genes have already been performed, and new genes and gene networks controlling blood cell homeostasis have been identified (Minakhina and Steward, 2006; Stofanko et al., 2008; Avet-Rochex et al., 2010; Bina et al., 2010; Minakhina and Steward, 2010). On the basis of these pioneering experiments, and the recent demonstration that Drosophila can be used to identify the core regulatory network that contributes to the development of AML (Osman et al., 2009; Sinenko et al., 2010), it is expected that more genetic screens performed in flies will provide novel entries to the study of acute and chronic leukaemias in mammals.
Acknowledgments
We thank Caroline Monod and Cédric Polesello for their comments on the manuscript. Work in the authors’ laboratory is supported by CNRS, University Toulouse III, Ministère de la Recherche (ANR « programme blanc »), ARC (Association pour la Recherche sur le Cancer), AFM (Association Française contre les Myopathies) and FRM (Fondation pour la Recherche Médicale).
Footnotes
COMPETING INTERESTS
The authors declare that they do not have any competing or financial interests.
REFERENCES
- Arai F., Hirao A., Ohmura M., Sato H., Matsuoka S., Takubo K., Ito K., Koh G. Y., Suda T. (2004). Tie2/angiopoietin-1 signaling regulates hematopoietic stem cell quiescence in the bone marrow niche. Cell 118, 149–161 [DOI] [PubMed] [Google Scholar]
- Argiropoulos B., Humphries R. K. (2007). Hox genes in hematopoiesis and leukemogenesis. Oncogene 26, 6766–6776 [DOI] [PubMed] [Google Scholar]
- Avet-Rochex A., Boyer K., Polesello C., Gobert V., Osman D., Roch F., Auge B., Zanet J., Haenlin M., Waltzer L. (2010). An in vivo RNA interference screen identifies gene networks controlling Drosophila melanogaster blood cell homeostasis. BMC Dev. Biol. 10, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bina S., Wright V. M., Fisher K. H., Milo M., Zeidler M. P. (2010). Transcriptional targets of Drosophila JAK/STAT pathway signalling as effectors of haematopoietic tumour formation. EMBO Rep. 11, 201–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnet D., Dick J. E. (1997). Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat. Med. 3, 730–737 [DOI] [PubMed] [Google Scholar]
- Braun T., Woollard A. (2009). RUNX factors in development: lessons from invertebrate model systems. Blood Cells Mol. Dis. 43, 43–48 [DOI] [PubMed] [Google Scholar]
- Bromberg J. F., Wrzeszczynska M. H., Devgan G., Zhao Y., Pestell R. G., Albanese C., Darnell J. E., Jr (1999). Stat3 as an oncogene. Cell 98, 295–303 [DOI] [PubMed] [Google Scholar]
- Calvi L. M., Adams G. B., Weibrecht K. W., Weber J. M., Olson D. P., Knight M. C., Martin R. P., Schipani E., Divieti P., Bringhurst F. R., et al. (2003). Osteoblastic cells regulate the haematopoietic stem cell niche. Nature 425, 841–846 [DOI] [PubMed] [Google Scholar]
- Campbell C., Risueno R. M., Salati S., Guezguez B., Bhatia M. (2008). Signal control of hematopoietic stem cell fate: Wnt, Notch, and Hedgehog as the usual suspects. Curr. Opin. Hematol. 15, 319–325 [DOI] [PubMed] [Google Scholar]
- Chung Y. J., Park B. B., Kang Y. J., Kim T. M., Eaves C. J., Oh I. H. (2006). Unique effects of Stat3 on the early phase of hematopoietic stem cell regeneration. Blood 108, 1208–1215 [DOI] [PubMed] [Google Scholar]
- Colmone A., Amorim M., Pontier A. L., Wang S., Jablonski E., Sipkins D. A. (2008). Leukemic cells create bone marrow niches that disrupt the behavior of normal hematopoietic progenitor cells. Science 322, 1861–1865 [DOI] [PubMed] [Google Scholar]
- Crozatier M., Meister M. (2007). Drosophila haematopoiesis. Cell Microbiol. 9, 1117–1126 [DOI] [PubMed] [Google Scholar]
- Crozatier M., Ubeda J. M., Vincent A., Meister M. (2004). Cellular immune response to parasitization in Drosophila requires the EBF orthologue collier. PLoS Biol. 2, E196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehn M., Cho R. W., Lobo N. A., Kalisky T., Dorie M. J., Kulp A. N., Qian D., Lam J. S., Ailles L. E., Wong M., et al. (2009). Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature 458, 780–783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohner H., Estey E. H., Amadori S., Appelbaum F. R., Buchner T., Burnett A. K., Dombret H., Fenaux P., Grimwade D., Larson R. A., et al. (2010). Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood 115, 453–474 [DOI] [PubMed] [Google Scholar]
- Dykstra B., Kent D., Bowie M., McCaffrey L., Hamilton M., Lyons K., Lee S. J., Brinkman R., Eaves C. (2007). Long-term propagation of distinct hematopoietic differentiation programs in vivo. Cell Stem Cell 1, 218–229 [DOI] [PubMed] [Google Scholar]
- Dzierzak E., Speck N. A. (2008). Of lineage and legacy: the development of mammalian hematopoietic stem cells. Nat. Immunol. 9, 129–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekas L. A., Cardozo T. J., Flaherty M. S., McMillan E. A., Gonsalves F. C., Bach E. A. (2010). Characterization of a dominant-active STAT that promotes tumorigenesis in Drosophila. Dev. Biol. 344, 621–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliasson P., Jonsson J. I. (2010). The hematopoietic stem cell niche: low in oxygen but a nice place to be. J. Cell. Physiol. 222, 17–22 [DOI] [PubMed] [Google Scholar]
- Fleming H. E., Janzen V., Lo Celso C., Guo J., Leahy K. M., Kronenberg H. M., Scadden D. T. (2008). Wnt signaling in the niche enforces hematopoietic stem cell quiescence and is necessary to preserve self-renewal in vivo. Cell Stem Cell 2, 274–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Graves S., Koch U., Liu S., Jankovic V., Buonamici S., El Andaloussi A., Nimer S. D., Kee B. L., Taichman R., et al. (2009). Hedgehog signaling is dispensable for adult hematopoietic stem cell function. Cell Stem Cell 4, 548–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber H. P., Ferrara N. (2003). The role of VEGF in normal and neoplastic hematopoiesis. J. Mol. Med. 81, 20–31 [DOI] [PubMed] [Google Scholar]
- Goardon N., Marchi E., Atzberger A., Quek L., Schuh A., Soneji S., Woll P., Mead A., Alford K. A., Rout R., et al. (2011). Coexistence of LMPP-like and GMP-like leukemia stem cells in acute myeloid leukemia. Cancer Cell 19, 138–152 [DOI] [PubMed] [Google Scholar]
- Grigoryan T., Wend P., Klaus A., Birchmeier W. (2008). Deciphering the function of canonical Wnt signals in development and disease: conditional loss-and gain-of-function mutations of beta-catenin in mice. Genes Dev. 22, 2308–2341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison D. A., Binari R., Nahreini T. S., Gilman M., Perrimon N. (1995). Activation of a Drosophila Janus kinase (JAK) causes hematopoietic neoplasia and developmental defects. EMBO J. 14, 2857–2865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann I., Stover E. H., Cullen D. E., Mao J., Morgan K. J., Lee B. H., Kharas M. G., Miller P. G., Cornejo M. G., Okabe R., et al. (2009). Hedgehog signaling is dispensable for adult murine hematopoietic stem cell function and hematopoiesis. Cell Stem Cell 4, 559–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holz A., Bossinger B., Strasser T., Janning W., Klapper R. (2003). The two origins of hemocytes in Drosophila. Development 130, 4955–4962 [DOI] [PubMed] [Google Scholar]
- Honti V., Csordas G., Markus R., Kurucz E., Jankovics F., Ando I. (2010). Cell lineage tracing reveals the plasticity of the hemocyte lineages and of the hematopoietic compartments in Drosophila melanogaster. Mol. Immunol. 47, 1997–2004 [DOI] [PubMed] [Google Scholar]
- Ishikawa F., Yoshida S., Saito Y., Hijikata A., Kitamura H., Tanaka S., Nakamura R., Tanaka T., Tomiyama H., Saito N., et al. (2007). Chemotherapy-resistant human AML stem cells home to and engraft within the bone-marrow endosteal region. Nat. Biotechnol. 25, 1315–1321 [DOI] [PubMed] [Google Scholar]
- Jang Y. Y., Sharkis S. J. (2007). A low level of reactive oxygen species selects for primitive hematopoietic stem cells that may reside in the low-oxygenic niche. Blood 110, 3056–3063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung S. H., Evans C. J., Uemura C., Banerjee U. (2005). The Drosophila lymph gland as a developmental model of hematopoiesis. Development 132, 2521–2533 [DOI] [PubMed] [Google Scholar]
- Kieslinger M., Hiechinger S., Dobreva G., Consalez G. G., Grosschedl R. (2010). Early B cell factor 2 regulates hematopoietic stem cell homeostasis in a cell-nonautonomous manner. Cell Stem Cell 7, 496–507 [DOI] [PubMed] [Google Scholar]
- Krzemien J., Dubois L., Makki R., Meister M., Vincent A., Crozatier M. (2007). Control of blood cell homeostasis in Drosophila larvae by the posterior signalling centre. Nature 446, 325–328 [DOI] [PubMed] [Google Scholar]
- Krzemien J., Crozatier M., Vincent A. (2010a). Ontogeny of the Drosophila larval hematopoietic organ, hemocyte homeostasis and the dedicated cellular immune response to parasitism. Int. J. Dev. Biol. 54, 1117–1125 [DOI] [PubMed] [Google Scholar]
- Krzemien J., Oyallon J., Crozatier M., Vincent A. (2010b). Hematopoietic progenitors and hemocyte lineages in the Drosophila lymph gland. Dev. Biol. 346, 310–319 [DOI] [PubMed] [Google Scholar]
- Lanot R., Zachary D., Holder F., Meister M. (2001). Postembryonic hematopoiesis in Drosophila. Dev. Biol. 230, 243–257 [DOI] [PubMed] [Google Scholar]
- Lebestky T., Chang T., Hartenstein V., Banerjee U. (2000). Specification of Drosophila hematopoietic lineage by conserved transcription factors. Science 288, 146–149 [DOI] [PubMed] [Google Scholar]
- Lebestky T., Jung S. H., Banerjee U. (2003). A Serrate-expressing signaling center controls Drosophila hematopoiesis. Genes Dev. 17, 348–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine R. L., Wadleigh M., Cools J., Ebert B. L., Wernig G., Huntly B. J., Boggon T. J., Wlodarska I., Clark J. J., Moore S., et al. (2005). Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 7, 387–397 [DOI] [PubMed] [Google Scholar]
- Lin H., Grosschedl R. (1995). Failure of B-cell differentiation in mice lacking the transcription factor EBF. Nature 376, 263–267 [DOI] [PubMed] [Google Scholar]
- Lo Celso C., Fleming H. E., Wu J. W., Zhao C. X., Miake-Lye S., Fujisaki J., Cote D., Rowe D. W., Lin C. P., Scadden D. T. (2009). Live-animal tracking of individual haematopoietic stem/progenitor cells in their niche. Nature 457, 92–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo H., Hanratty W. P., Dearolf C. R. (1995). An amino acid substitution in the Drosophila hopTum-l Jak kinase causes leukemia-like hematopoietic defects. EMBO J. 14, 1412–1420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majeti R., Weissman I. L. (2011). Human acute myelogenous leukemia stem cells revisited: there’s more than meets the eye. Cancer Cell 19, 9–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makki R., Meister M., Pennetier D., Ubeda J. M., Braun A., Daburon V., Krzemien J., Bourbon H. M., Zhou R., Vincent A., et al. (2010). A short receptor downregulates JAK/STAT signalling to control the Drosophila cellular immune response. PLoS Biol. 8, e1000441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal L., Martinez-Agosto J. A., Evans C. J., Hartenstein V., Banerjee U. (2007). A Hedgehog- and Antennapedia-dependent niche maintains Drosophila haematopoietic precursors. Nature 446, 320–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikkola H. K., Orkin S. H. (2006). The journey of developing hematopoietic stem cells. Development 133, 3733–3744 [DOI] [PubMed] [Google Scholar]
- Minakhina S., Steward R. (2006). Melanotic mutants in Drosophila: pathways and phenotypes. Genetics 174, 253–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minakhina S., Steward R. (2010). Hematopoietic stem cells in Drosophila. Development 137, 27–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullally A., Lane S. W., Ball B., Megerdichian C., Okabe R., Al-Shahrour F., Paktinat M., Haydu J. E., Housman E., Lord A. M., et al. (2010). Physiological Jak2V617F expression causes a lethal myeloproliferative neoplasm with differential effects on hematopoietic stem and progenitor cells. Cancer Cell 17, 584–596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullighan C. G., Zhang J., Harvey R. C., Collins-Underwood J. R., Schulman B. A., Phillips L. A., Tasian S. K., Loh M. L., Su X., Liu W., et al. (2009). JAK mutations in high-risk childhood acute lymphoblastic leukemia. Proc. Natl. Acad. Sci. USA 106, 9414–9418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson S. K., Johnston H. M., Whitty G. A., Williams B., Webb R. J., Denhardt D. T., Bertoncello I., Bendall L. J., Simmons P. J., Haylock D. N. (2005). Osteopontin, a key component of the hematopoietic stem cell niche and regulator of primitive hematopoietic progenitor cells. Blood 106, 1232–1239 [DOI] [PubMed] [Google Scholar]
- Orkin S. H., Zon L. I. (2008). Hematopoiesis: an evolving paradigm for stem cell biology. Cell 132, 631–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman D., Gobert V., Ponthan F., Heidenreich O., Haenlin M., Waltzer L. (2009). A Drosophila model identifies calpains as modulators of the human leukemogenic fusion protein AML1-ETO. Proc. Natl. Acad. Sci. USA 106, 12043–12048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owusu-Ansah E., Banerjee U. (2009). Reactive oxygen species prime Drosophila haematopoietic progenitors for differentiation. Nature 461, 537–541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmar K., Mauch P., Vergilio J. A., Sackstein R., Down J. D. (2007). Distribution of hematopoietic stem cells in the bone marrow according to regional hypoxia. Proc. Natl. Acad. Sci. USA 104, 5431–5436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter C. J., Tasic B., Russler E. V., Liang L., Luo L. (2010). The Q system: a repressible binary system for transgene expression, lineage tracing, and mosaic analysis. Cell 141, 536–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remillieux-Leschelle N., Santamaria P., Randsholt N. B. (2002). Regulation of larval hematopoiesis in Drosophila melanogaster: a role for the multi sex combs gene. Genetics 162, 1259–1274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renstrom J., Kroger M., Peschel C., Oostendorp R. A. (2010). How the niche regulates hematopoietic stem cells. Chem. Biol. Interact. 184, 7–15 [DOI] [PubMed] [Google Scholar]
- Reya T., Morrison S. J., Clarke M. F., Weissman I. L. (2001). Stem cells, cancer, and cancer stem cells. Nature 414, 105–111 [DOI] [PubMed] [Google Scholar]
- Richardson R. B. (2011). Stem cell niches and other factors that influence the sensitivity of bone marrow to radiation-induced bone cancer and leukaemia in children and adults. Int. J. Radiat. Biol. 87, 343–359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizki R. M., Rizki T. M. (1984). Selective destruction of a host blood cell type by a parasitoid wasp. Proc. Natl. Acad. Sci. USA 81, 6154–6158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield R. (1978). The relationship between the spleen colony-forming cell and the haemopoietic stem cell. Blood Cells 4, 7–25 [PubMed] [Google Scholar]
- Simsek T., Kocabas F., Zheng J., Deberardinis R. J., Mahmoud A. I., Olson E. N., Schneider J. W., Zhang C. C., Sadek H. A. (2010). The distinct metabolic profile of hematopoietic stem cells reflects their location in a hypoxic niche. Cell Stem Cell 7, 380–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinenko S. A., Mandal L., Martinez-Agosto J. A., Banerjee U. (2009). Dual role of wingless signaling in stem-like hematopoietic precursor maintenance in Drosophila. Dev. Cell 16, 756–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinenko S. A., Hung T., Moroz T., Tran Q. M., Sidhu S., Cheney M. D., Speck N. A., Banerjee U. (2010). Genetic manipulation of AML1-ETO-induced expansion of hematopoietic precursors in a Drosophila model. Blood 116, 4612–4620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorrentino R. P., Tokusumi T., Schulz R. A. (2007). The Friend of GATA protein U-shaped functions as a hematopoietic tumor suppressor in Drosophila. Dev. Biol. 311, 311–323 [DOI] [PubMed] [Google Scholar]
- Stofanko M., Kwon S. Y., Badenhorst P. (2008). A misexpression screen to identify regulators of Drosophila larval hemocyte development. Genetics 180, 253–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokusumi Y., Tokusumi T., Stoller-Conrad J., Schulz R. A. (2010). Serpent, suppressor of hairless and U-shaped are crucial regulators of hedgehog niche expression and prohemocyte maintenance during Drosophila larval hematopoiesis. Development 137, 3561–3568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tothova Z., Kollipara R., Huntly B. J., Lee B. H., Castrillon D. H., Cullen D. E., McDowell E. P., Lazo-Kallanian S., Williams I. R., Sears C., et al. (2007). FoxOs are critical mediators of hematopoietic stem cell resistance to physiologic oxidative stress. Cell 128, 325–339 [DOI] [PubMed] [Google Scholar]
- Trumpp A., Essers M., Wilson A. (2010). Awakening dormant haematopoietic stem cells. Nat. Rev. Immunol.. 10, 201–209 [DOI] [PubMed] [Google Scholar]
- Tsiftsoglou A. S., Vizirianakis I. S., Strouboulis J. (2009). Erythropoiesis: model systems, molecular regulators, and developmental programs. IUBMB Life 61, 800–830 [DOI] [PubMed] [Google Scholar]
- Vainchenker W., Dusa A., Constantinescu S. N. (2008). JAKs in pathology: role of Janus kinases in hematopoietic malignancies and immunodeficiencies. Semin. Cell Dev. Biol. 19, 385–393 [DOI] [PubMed] [Google Scholar]
- Wang C. Q., Jacob B., Nah G. S., Osato M. (2010). Runx family genes, niche, and stem cell quiescence. Blood Cells Mol. Dis. 44, 275–286 [DOI] [PubMed] [Google Scholar]
- Weber J. M., Calvi L. M. (2010). Notch signaling and the bone marrow hematopoietic stem cell niche. Bone 46, 281–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson A., Laurenti E., Oser G., van der Wath R. C., Blanco-Bose W., Jaworski M., Offner S., Dunant C. F., Eshkind L., Bockamp E., et al. (2008). Hematopoietic stem cells reversibly switch from dormancy to self-renewal during homeostasis and repair. Cell 135, 1118–1129 [DOI] [PubMed] [Google Scholar]
- Xie T., Spradling A. C. (2000). A niche maintaining germ line stem cells in the Drosophila ovary. Science 290, 328–330 [DOI] [PubMed] [Google Scholar]
- Xie Y., Yin T., Wiegraebe W., He X. C., Miller D., Stark D., Perko K., Alexander R., Schwartz J., Grindley J. C., et al. (2009). Detection of functional haematopoietic stem cell niche using real-time imaging. Nature 457, 97–101 [DOI] [PubMed] [Google Scholar]
- Zhang J., Niu C., Ye L., Huang H., He X., Tong W. G., Ross J., Haug J., Johnson T., Feng J. Q., et al. (2003). Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425, 836–841 [DOI] [PubMed] [Google Scholar]