Abstract
Although the fields of urban planning and public health share a common origin in the efforts of reformers to tame the ravages of early industrialization in the 19th century, the 2 disciplines parted ways in the early 20th century as planners increasingly focused on the built environment while public health professionals narrowed in on biomedical causes of disease and disability. Among the unfortunate results of this divergence was a tendency to discount the public health implications of planning decisions. Given increasingly complex urban environments and grave health disparities in cities worldwide, urban planners and public health professionals have once again become convinced of the need for inclusive approaches to improve population health and achieve health equity. To make substantive progress, intersectoral collaboration utilizing ecological and systems science perspectives will be crucial as the solutions lie well beyond the control of any single authority. Grounded in the social determinants of health, and with a renewed sense of interconnectedness, dedicated and talented people in government agencies and communities who recognize that our future depends on cultivating local change and evaluating the results can come to grips with the enormous challenge that lies ahead to create more equitable, sustainable, and healthier cities worldwide.
Keywords: Urban planning, Health equity, Social determinants of health, Urban health, Built environment, Public health
Introduction
Students of the city have long understood the importance of social and environmental factors in shaping health inequities (or injustices). Indeed, the fields of public health and urban planning owe their origins, at least in part, to the concerns of urban reformers more than a century ago over how urbanization was affecting the health of impoverished city residents.1,2 Building codes and the widespread adoption of public sewerage are examples of early planning efforts that reduced health inequities.3,4 Nascent public health professionals and urban planners understood that collective action through housing, sanitation, and labor reform was necessary to address unsafe living conditions, impure water, and noxious trades that were manifest in the industrializing slums of the 19th century.5
Today, health inequalities (or disparities) persist within and between populations and by certain measures are widening despite more than a century of both broad-based and targeted public health interventions. As was the case during the Progressive Era (ca. 1890–1920), the social determinants of health and urban planning are again coming to the fore as a framework and a mode for reducing health inequities in urban settings.6–8 Accordingly, governments responsible for enacting public policy are paying increased attention to ecological and systems science perspectives. These models posit that the physical or built environments of communities and the dynamic, complex, adaptive social systems in which they exist are among the important determinants of both individual and population health and wellbeing.9–11 A simplified heuristic of an ecological model is presented as Figure 1, where interventions at lower levels tend to be more effective because they reach broader segments of society and require less individual agency. To obtain the maximum possible sustained public health benefit, it is optimal to implement interventions at each level simultaneously.12
FIGURE 1.
Levels of public health interventions in terms of population health impact and need for individual agency. Source: Adapted from Frieden.12
In 2008, Prevention Institute and Trust for America’s Health convened a multidisciplinary group of government officials, community advocates, and researchers to discuss the role of the US federal government in addressing underlying determinants of health.13 The consensus of the participants was that insufficient resources have been invested in community factors that pertain to the social and physical environment, even as they are influential contributors to poor health outcomes and health inequalities within and between population groups (Table 1).
Table 1.
Community factors in the social and physical environment that affect health
| Place |
| Accessibility and promotion of products: characterized by the availability and promotion of safe, healthy, affordable, culturally appropriate products and services (e.g., food, books and school supplies, sports equipment, arts and crafts supplies, and other recreational items); limited promotion and availability, or lack, of potentially harmful products and services (e.g., tobacco, firearms, alcohol, and other drugs) |
| Maintenance and safety: characterized by a well-maintained, appealing, clean, and culturally relevant visual and auditory environment; actual and perceived safety |
| Parks and open spaces: characterized by safe, clean, accessible parks; parks that appeal to interests and activities across the life span; green space; outdoor space that is accessible to the community; natural/open space that is preserved through the planning process |
| Transportation options: characterized by the availability of safe, reliable, accessible, and affordable methods for transport, including public transit, walking, and bicycling |
| Housing: characterized by safe, affordable, available housing |
| Air, water, and soil: characterized by safe and non-toxic water, soil, indoor and outdoor air, and building materials |
| Arts and culture: characterized by abundant opportunities within the community for cultural and artistic expression and participation |
| People |
| Social networks and trust: characterized by strong social ties among persons and positions, built upon mutual obligations; opportunities to exchange information; the ability to enforce standards and administer sanctions |
| Community engagement and efficacy: characterized by local/indigenous leadership; involvement in community or social organizations; participation in the political process; willingness to intervene on behalf of the common good |
| Norms/expected behaviors and attitudes: characterized by regularities in behavior with which people generally conform; standards of behavior that foster disapproval of deviance; the way in which the environment shapes healthy and unhealthy behaviors |
| Foundation of opportunity |
| Racial/ethnic justice and intergroup relations: characterized by policies and organizational practices that foster equitable opportunities and services for all; positive relations between people of different racial/ethnic, cultural, and religious backgrounds |
| Jobs and local ownership: characterized by local ownership of assets, including homes and businesses; access to investment opportunities, job availability, and the ability to earn a living wage |
| Education: characterized by high-quality and available education, training, and literacy development across the life span for everyone regardless of gender or social standing |
Source: Adapted from Ashley et al.13
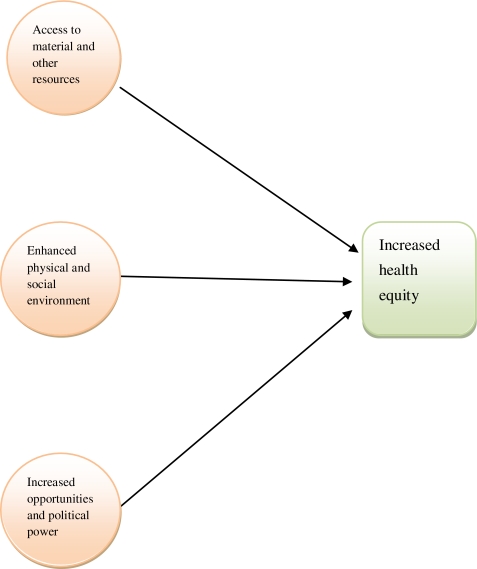
Our particular interest in this paper lies in better understanding how urban planning solutions implemented by local governments may improve health equity.14 Three mechanisms through which this may occur are detailed in the basic schematic presented in Figure 2, as adapted from work by Tsui15 that examined sectoral job training.
FIGURE 2.
Mechanisms for increasing health equity. Source: Adapted from Tsui.15
The first pathway, Access to material and other resources, seeks to undo health inequities that result from the unfair distribution of resources among groups according to, e.g., gender, race/ethnicity, and socioeconomic standing, which lead to unequal burdens of exposures within and across communities (both geographically and socially defined). An example of an urban planning solution to mitigate the negative effects of unequal access to nutritious foods is for local governments to create incentive programs to attract supermarkets and grocery stores to underserved neighborhoods.16
The second pathway, Enhanced physical and social environment, aims to ensure a fairer distribution of community aspects that promote health (or health amenities), as well as community aspects that degrade health (or health disamenities). Among the potentially health-promoting facets of the physical environment are: urban form that facilitates non-motorized forms of travel, such as walking and bicycling; accessibility and affordability of safe housing and community-based health facilities; and parks and other open spaces in close proximity to home, work, and school that engender physical activity and social engagement.6,17 Negative aspects of the physical environment include indoor and outdoor environmental hazards and pollutants, such as lead paint, mold, and particulate emissions, and an overabundance of retail outlets that sell unhealthy food and alcohol.6,13 Because urban planning shapes the physical environment, it influences the spatial distribution of both health amenities and disamenities. Local governments may thus use participatory planning processes that involve socially disadvantaged groups to more fairly distribute health amenities and disamenities, thereby increasing health equity.
The third pathway, Increased opportunities and political power, may be abetted through urban planning efforts instituted by local governments that provide, e.g., safe and affordable transportation options to and from work and school. In concert with other public policies that permit all workers to earn a living wage, and girls and women as well as boys and men to gain quality education and training across the life span, enhanced political power for oppressed populations may result in increased health equity as opportunities and resources that support health are redistributed to underserved groups.
Next, we review the scientific evidence on links between urban planning and public health, with a particular focus on reducing health inequalities through intervening on the social determinants of health. In particular, we consider urban form, food environments, physically active spaces, environmental hazards, and social segregation, sequentially. Our view is expansive in that we examine both purposive policies directed at health disparities as well as urban planning efforts, or the lack thereof, which may have unintentionally influenced health disparities. After each entry, we explicitly cite evidence regarding how efforts to shape the social and physical environment in cities have mitigated or exacerbated health disparities between the “haves” and the “have nots.”
Urban Form
Urban planning is foremost about shaping urban form. Through land use decisions, planners structure the distribution of various entities, e.g., stores, highways, and parks, and the density of the built landscape. Because urban form is thought to influence non-motorized travel, e.g., walking and bicycling, health disparities may result from the unequal distribution of sidewalks and bicycle lanes in communities.
The link between urban form and health has been examined by transportation researchers employing a utility maximization framework that views travel behavior as governed by the set of choices available to individuals. Land use patterns such as density, accessibility, and transportation systems influence the set of available options: e.g., if there is no public transit in a certain locale, it cannot be a transport alternative. The relative attractiveness of available choices also influences the ultimate decision. In areas where walking and bicycling offer appealing alternatives to driving, people may choose non-motorized travel more often than in places where walking and bicycling are dangerous or otherwise prohibitive. This in turn leads to greater physical activity and, given the demonstrated link between physical activity and fitness, improved population health and wellbeing.
Ecological models posit influences simultaneously acting at multiple levels. This may include, e.g., the individual level, such as preferences; the interpersonal level, such as the behavior of one’s peers; and the environmental level, such as the “walkability” of a neighborhood. For example, an individual may be more likely to bicycle to work if a safe, convenient bicycle path is available. Moreover, one person’s decision to commute by bicycle may encourage others to commute by bicycle as they learn about this possibility and it becomes socially acceptable. The utility maximization and ecological perspectives offer similar predictions regarding how the built environment shapes physical activity; a key distinction is that ecological models attach more weight to group-level attitudes and customs toward physical activity.18
In thinking about the relationship between the built environment and health, it is worth noting that—to some extent—individuals choose their built environments. It may be that those who value non-motorized forms of travel choose environments more conducive to walking and bicycling. Handy19 has conceptualized this operating as follows: preference for non-motorized travel influences the choice of neighborhood. The amenability of the chosen neighborhood to non-motorized travel will then work to amplify preferences. This may lead to either more or less physical activity. Handy posits, “for individuals with a high initial preference for [non-motorized travel], the built environment acts as an enabler of such activities and a reinforcer of high preferences or as a constraint on non-motorized travel and a promoter of lower preferences. For individuals with a low initial preference for non-motorized travel, the built environment acts as an encourager of non-motorized travel and a promoter of higher preferences or as a discourager of non-motorized travel and a reinforcer of low preferences.”19 Thus, self-selection is an alternative explanation for why the built environment may be linked to non-motorized travel.
Applying this causal model, we can infer 2 pathways through which the built environment may contribute to health disparities. First, if access to “walkable” or bicycle-friendly neighborhoods is influenced by socioeconomic status, health inequities may be fostered. Moreover, self-selection may be less relevant for disadvantaged populations. “Choosing” a neighborhood of residence assumes a modicum of resources that would allow people to make a selection among different alternatives. For many poor households, affordability may be the overriding criterion that limits their choices to virtually nil. Furthermore, racial/ethnic minorities often face housing discrimination that prevents them from exercising their preferences.20,21 Consequently, although self-selection may explain part of the relationship between the built environment and health, it may be less important for disadvantaged than for advantaged populations.
A second way that the built environment may contribute to health disparities is if socioeconomic groups are differentially affected by the built environment. For example, if more advantaged populations are able to shield themselves from negative environmental impacts on their health whereas disadvantaged populations lack the requisite resources, health inequalities may accrue.
Evidence on Urban Form and Health Equity
A persuasive link between the built environment and non-motorized travel is evident in the peer-reviewed literature.19,22 As concluded by Handy,19 “studies from the travel behavior literature and the physical activity literature provide relatively consistent and convincing evidence of an association between the built environment and physical activity.” Boarnet et al.22 likewise reported that “The results show fairly robust associations between the built environment (or urban design) and walking travel.”
Less certain, however, is the extent to which the documented associations are causal. Overwhelmingly, both the travel and public health literature rely on cross-sectional data to discern relationships between the built environment and physical activity. Recently, researchers have included longitudinal components to their studies to meaningfully address the issue of causality. Here, the evidence is more equivocal. Krizek23 found that when households moved to neighborhoods with different types of urban form, the likelihood of using non-motorized travel remained unaltered. Likewise, Rodriguez et al.24 reported that residents of “walkable” neighborhoods exercised no more frequently than residents of conventional suburbs, although the former walked more, leading the authors to speculate that residents of “walkable” neighborhoods substitute walking for other types of exercise. Research based upon cross-sectional data also supports the notion of an “activity budget,” whereby the total physical activity of individuals is relatively fixed, but environmental factors influence how proclivities for physical activity manifest themselves, i.e., whether to exercise at a gym or bicycle to work. Conversely, Handy et al.25 found that individuals walked more after moving to more “walkable” neighborhoods, even after controlling for individual preferences for different types of neighborhoods.
Thus, the relationship between urban form and health equity is unresolved in the scientific literature, likely because the available evidence is narrow in concept and scale. The types of urban form associated with non-motorized travel, i.e., higher density and “walkability,” are often found in older city neighborhoods.17,26,27 Because of historical patterns of development, it is difficult to draw definitive conclusions from geographically constrained observational studies.
Food Environments
Another way that urban planning may relate to health disparities is through creating or hampering healthy food environments as physical distance may support or hinder healthy eating habits. In urban settings, retail options that provide a wide variety of products, including fresh produce and other nutrient-dense foods, are considered beneficial. In the North American context, this often means large supermarkets. But in less developed countries, global chains may supplant local grocers that carry traditional, nutritious fare. Food environments may also be healthier if there are proximate opportunities to grow vegetables or shop in farmers’ markets. Urban planning may influence food environments through land use decisions that affect the density and location of food outlets, the type of food outlets permitted and sited, and the provision of opportunities for local micro-agriculture.
Because human decisions shape food environments, they are neither evenly nor randomly distributed across space. If proximity to full-service supermarkets correlates with socioeconomic status, it may be difficult for poor households to access fresh produce, thereby contributing to health disparities. Food environments may also foster health disparities if there are differential impacts of location by socioeconomic status. For example, lack of proximity to full-service supermarkets may make it more difficult for poor households to access fresh produce because while affluent households may possess the necessary resources to pay for motorized travel or delivery of fresh produce, poor households may not.
Evidence on Food Environments and Health Equity
According to a recent review, the scientific evidence is inconsistent in demonstrating a link between proximity to healthy food environments and diet and health.17 For example, several studies found that reduced access to supermarkets is associated with poorer diets among certain social groups.28–30 Other studies, however, have failed to demonstrate a link.27,31 Cummins et al.30 employed a quasi-experimental design to compare the diets of residents in a neighborhood that experienced the development of a new supermarket with the diets of residents in a control neighborhood that did not and found little in the way of differences in dietary changes between the residents of the 2 neighborhoods.
While the evidence is mixed on the relationship between food environments and health equity, it does not preclude the possibility that localized food environments contribute to health disparities. It may be that disadvantaged populations are especially vulnerable to or differentially affected by distance from healthy food environments. Part of the reason for the conflicting findings in the literature may be the different contexts in which the research has been conducted. Underscoring this point, studies conducted in North America have consistently found that poor minority neighborhoods have less access to healthy food in the form of full-service supermarkets and an abundance of fast-food restaurants.17,31 Research undertaken elsewhere has been more equivocal, leading to speculation that the hyper-segregated nature of US ghettos makes them especially barren in terms of high-quality food.31 In other advanced industrialized countries, poor minorities are much less spatially segregated, meaning that differences in food environments do not vary across socioeconomic strata as markedly as they do in the United States.32 In addition, governments have intervened more aggressively against market forces outside of the United States in determining the location of food stores, perhaps resulting in more evenly distributed food environments across communities.
In sum, the evidence on the relationship between food environments and health equity is inconsistent, due in part to the differing contexts in which the research has been conducted. In places such as North America where segregation by socioeconomic status and race/ethnicity is stark, access to healthy food environments is uneven, with marginalized groups at a disadvantage.31 Since food environments are more evenly distributed in places where government intervention has been purposeful, urban planning may operate through the shaping of local food environments to reduce health disparities.
Physically Active Places
Recreational physical activity outside of the home may be an important component of health and wellbeing, especially in sedentary societies. Thus, physical proximity to places for walking, running, swimming, or engaging in other forms of exercise become important to the extent that it is more likely for people to engage in these activities. Through land use decisions and infrastructure siting, urban planning affects where fitness facilities may locate and whether or not there are sidewalks for walking and trails or dedicated lanes for bicycling. If these spaces are distributed in such a way that disadvantaged social groups have less access to recreational areas that are perceived of as safe, then urban planning may potentially influence health disparities through this pathway. On the other hand, if a park is viewed as dangerous, it may do little to encourage exercise even for people living right across the street.
Evidence on Physically Active Spaces and Health Equity
The majority of empirical studies conducted to date have reported that proximity to exercise amenities and “walkable” spaces facilitates physical activity, even as a few investigations have failed to demonstrate this link.17,33 Lovasi et al.17 hypothesize that the inconsistency in the literature may be due to the failure to account for the quality of the spaces. For example, if the nearby sidewalks are crumbling and uneven, individuals may not utilize them for walking despite their proximity.
Research on the perceived safety of nearby spaces for physical activity is also mixed, likely because of the variability present among social groups, e.g., as defined by gender and age. Several studies have found that physical and social disorder correlated with worse health outcomes and that certain groups reported fear of crime as the biggest obstacle to exercise,17 but at least one study failed to find this link.34
The evidence on whether exercise-inducing facilities are distributed in an equitable manner, meaning that they are equally accessible to all socioeconomic groups, depends upon the context of the study and the measurement tools employed. In North America, sidewalks and street lighting that facilitate walking do not appear to be distributed in a way that disadvantages impoverished or minority populations, perhaps because these amenities are found in denser urban settings where these groups are concentrated. The reverse is true in less developed countries where impoverished populations often live in areas with little or no infrastructure.35
Whether or not there is a relationship between the socioeconomic status of an area and the availability of exercise facilities depends partly upon how these amenities are defined. The accessibility of indoor exercise spaces closely tracks along socioeconomic gradients as more of them are located in affluent areas. Outdoor exercise facilities, however, are relatively evenly distributed across neighborhoods. This pattern may not be unexpected since indoor exercise facilities are typically expensive to build and maintain and thus are less frequently marketed to disadvantaged populations. In less developed countries where many of the poorest people live in informal settlements, access to both indoor and outdoor exercise facilities is extremely limited.35
Throughout the world, regardless of whether or not perceived or actual measures are used, minority and low-income persons have consistently been found to live in less safe and more disorderly neighborhoods.36 Furthermore, there is reason to believe that the spatial distribution and perceived safety of physically active spaces contributes to health disparities. Because exercise spaces influence activity levels, by carefully considering the siting of these facilities, urban planners may help reduce health inequities.
Environmental Hazards
Environmental hazards in the form of industrial facilities that emit pollutants, hazardous waste facilities, and other point and mobile sources of contaminants have substantial negative impacts on population health.37 Although it is difficult to prove conclusively that proximity to specific environmental hazards leads to specific adverse health outcomes,38 certain studies have demonstrated a link.39 Environmental hazards may contribute to health disparities if they are disproportionately proximate to disadvantaged populations, and there is ample reason to suspect that this may be the case in many locales. Freeman40 first argued that because individuals choose their neighborhoods and those with more resources had more “choice,” the distribution of environmental hazards would likely mirror the distribution of wealth. This thinking is consistent with urban economic models of residential location which posit that disamenities such as hazardous waste facilities are factored into the price of housing units. That is, proximity to disamenities serves to lower the price of housing units, ceterius paribus. Thus, lower priced housing, which is disproportionately occupied by poorer, disadvantaged groups, tends to cluster around environmental disamenities whose residents then suffer the ill consequences of exposures, including disease, disability, and premature death.
Political economy perspectives from urban politics and sociology offer similar predictions with regard to the location of environmental hazards. According to these theories, the urban landscape is shaped by market forces and the decisions of those in authority. Powerful groups will act to ensure that undesirable land uses are located far away from elite interests. Less powerful groups, such as impoverished or subaltern minorities, are thus likely to bear the brunt of decision making.41 There are at least 2 differences, however, between these perspectives. The first is that the political economy perspective focuses more on the original choices made with regard to the siting of environmental hazards. In contrast, the urban economics literature is silent on the siting decisions, only predicting that the surrounding properties will be of lower value. Second, the political economy perspective argues that minorities that are politically weak and segregated, regardless of their class, are disproportionately exposed to environmental hazards.42
Evidence on Environmental Hazards and Health Equity
A burgeoning environmental justice literature over the past few decades has carefully documented the relations among the siting of environmental hazards, race/ethnicity, and social class.43,44 There is near consensus that social class correlates with the location of environmental hazards across time and space. As Downey45 stated in a recent review, “Researchers have found income and poverty to be consistently associated with hazard presence in the expected direction: as environmental hazard presence increases, incomes decrease and poverty rates increase.” Where there have been contradictory findings, a specific environmental hazard has been found to accompany a desirable amenity, such as open space or parkland, or other plausible explanations.46
The evidence on environmental hazards and racial/ethnic minority concentrations, however, is less uniform. While a number of studies have found minorities to be unduly exposed to environmental hazards,47–49 other studies have failed to document a link.46,50 The discrepancy appears to be due to the role that racial/ethnic segregation plays as an intervening variable and the different ways disproportionate exposure to environmental hazards is defined. Segregation physically separates minorities not only from the dominant group but also from desirable amenities that the dominant group prefers. Certain desirable amenities, including those that are related to industrial jobs, also emit pollutants. In such instances, minorities may not be disproportionately proximate to the attendant environmental hazards.45 Certain researchers define differential exposure to environmental hazards only when the hazard was sited after the concentration of minorities already existed.45 But as delineated in the urban economics perspective, minorities (who are disproportionately poor) are expected to move to undesirable areas because the very presence of environmental hazards lowers housing prices.
Despite the mixed evidence with regard to race/ethnicity and proximity to environmental hazards, disparate exposure to environmental hazards is most likely a contributor to health disparities. This conclusion is based upon the following reasoning: the evidence linking exposure to environmental hazards and health is fairly strong; there are theoretical reasons to expect that exposure to environmental hazards is correlated with both race/ethnicity and social class; the published literature consistently demonstrates a link between social class and exposure to environmental hazards; and where the evidence of a link between race/ethnicity and exposure to environmental hazards is equivocal, there are plausible explanations for the unanticipated findings.
Social Segregation
A common theme linking the urban form, food environments, physically active spaces, and environmental hazards literature is the concept that disadvantaged groups are differentially exposed to environmental amenities and disamenities. This assumption hinges on disadvantaged groups being residentially segregated from advantaged groups. If vulnerable populations were evenly dispersed across space, they would not suffer from differential exposures to most environmental hazards.
While the advent of modern communication and transportation technology has further enabled social groups to sort themselves across geographic space, elite groups have long used residential location as a way to distance themselves from disadvantaged groups. Indeed, this pattern has cut across virtually all industrial and post-industrial societies.32,51,52 Historically oppressed groups such as Blacks in the United States and South Africa and ex-untouchable castes in India experience extremely high levels of segregation, but some residential differential between social groups seems to be the norm in every society.32,52,53
Residential segregation thus acts as an intermediary that results in differential exposures to urban form, food environments, physically active spaces, and environmental hazards and consequently contributes to health disparities. But residential segregation also concentrates disadvantage and serves to further exacerbate inequities. According to this perspective, being disadvantaged and having disadvantaged neighbors is worse than being disadvantaged in isolation.
Wilson54 inspired much of the theorizing by social scientists about the mechanisms through which the social organization of a neighborhood may affect the life chances of poor residents. Broadly speaking, these mechanisms are categorized as theories of social structure36,55 and include myriad ways that neighbors influence behavior. The notion of peer effects is especially common in the popular imagination. For instance, in neighborhoods where many teenagers join sports teams, there is pressure on all teenagers to engage in these activities. In addition to the influence of peers, the wider community has a voice in shaping the behavior of residents through the process of collective socialization. Adults serve as role models whose behavior sets norms for youngsters to follow. Moreover, adults acting as “old heads” provide wisdom and advice to youths in the neighborhood.56 The social standing of adults in the neighborhood affects the way youths are collectively socialized. In communities where the adults have been marginalized by the wider society, the only trailblazing that adults can offer may lead to “dead end jobs” or “beating the system.” In some cases, the youths, sensing the marginalization of the adults, may decide to ignore their advice, blazing their own paths.
Whereas notions of peer effects and collective socialization seem most pertinent to minors, social networks have the potential to influence the life chances of adults as well. Social networks refer to the relationships people have with one another and, in the province of neighborhood effects, the nature of those ties in the immediate community. These networks are sources of social satisfaction, providing love, friendship, and a sense of belonging. But social networks also play a role in upward mobility by providing sources of information about accessing jobs, services, and other important resources.57 Once again, better-off neighbors are an advantage in that they offer ties that are more “leverageable,” that is, ties that foster upward mobility or offer access to important social and economic resources. For example, employed neighbors are more likely to have information about employment than unemployed neighbors. Likewise, a neighbor with an important position in the local school system has the potential to assist in extracting the best possible education from the system. Poorer neighbors may provide important social ties, but they may be less likely to possess the sort of resources that lead to upward mobility. In this way, social networks in poorer neighborhoods may be less advantageous than those in more affluent neighborhoods.
Evidence on Segregation and Health Equity
Although the exact mechanisms are unclear, the empirical evidence is for the most part consistent with the interpretation that better-off neighbors are an advantage in a segregated neighborhood. The most convincing evidence derives from the Moving to Opportunity (MTO) experiment where public housing residents were randomly assigned to a control group (families retained their public housing unit and received no new assistance), a section 8 comparison group (families received the standard counseling and voucher subsidy for use in the private market), or an experimental group (families received special relocation counseling and a voucher usable only in a low-poverty neighborhood).58 Among the documented health-related findings were positive impacts on physical and mental health for adult women and adolescent girls, including lower levels of obesity for the experimental group and reduced depression and anxiety for both experimental and section 8 comparison group movers.58 The findings of the MTO experiment are consistent with quasi-experimental research on neighborhood effects.59 Unfortunately, however, adolescent boys seemed to have not benefited at all from moving to better neighborhoods in the MTO experiment.58
Intersectoral Urban Health Interventions
Healthy urban planning means planning for people in cities.60 It promotes the idea that the city is much more than buildings, streets, and open spaces; it is a dynamic social space, the health of which is closely linked to that of its residents.60 This perspective is especially consonant with efforts to utilize urban planning to promote health equity.
Moreover, the major public health problems of the 21st century are dynamic, complex, and interconnected, and will require cooperation and partnership to address the enormous and persistent social disparities in health that exist within and across groups.61 While systems science has much intuitive appeal in collaborating across sectors, it is also increasingly endorsed by authoritative US public health bodies, including the Institute of Medicine,62 the National Institutes of Health,10 and the Centers for Disease Control and Prevention63 as an approach that merits further development. Midgley64 offers a methodology for systemic intervention that: (1) emphasizes the need to explore stakeholder values and boundaries; (2) challenges marginalization; and (3) draws upon a wide range of methods to create a flexible and responsive systems science practice. Accordingly, it complements other participatory intervention approaches such as community-based participatory research65 and health impact assessment66 that are gaining support in both urban planning and public health circles.
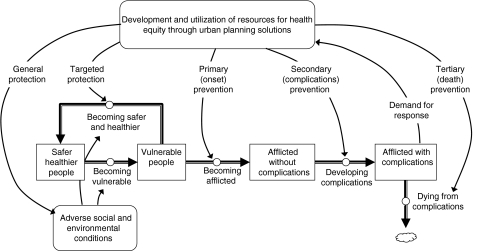
Figure 3 provides a broad view of urban planning solutions to achieve health equity and the spectrum of possible responses using a system dynamics stock and flow diagram.67
FIGURE 3.
A broad view of urban planning solutions to achieve health equity and the spectrum of possible responses. Rectangles represent the stocks of people; thick arrows with circles represent flows of people; thinner arrows indicate causal influence; rounded rectangles indicate multidimensional concepts. Source: Adapted from Homer and Hirsch.67
Our purpose in introducing systems science as another possible approach in addressing health inequities is to emphasize the importance of bringing the best science to bear on this major challenge. Triangulating a number of approaches, e.g., community-based participatory research,65 health impact assessment,66 and systems science,10,11,64,67 may prove to be optimal in the long term. And finally, while it has been stated before, it is vital to emphasize that open and participatory processes involving local authorities and vulnerable populations which give the latter a voice in decisions about infrastructure and public services that affect their lives may offer the best hope for success.68
References
- 1.Melosi MV. The Sanitary City: Urban Infrastructure in America from Colonial Times to the Present. Baltimore: Johns Hopkins University Press; 2000. [Google Scholar]
- 2.Porter D. Health, Civilization and the State: A History of Public Health from Ancient to Modern Times. New York: Routledge; 1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garb M. Health, morality, and housing: the “tenement problem” in Chicago. Am J Public Health. 2003;93(9):1420–1430. doi: 10.2105/AJPH.93.9.1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peterson J. The impact of sanitary reform upon American urban planning, 1840–1890. J Soc Hist. 1979;13(1):83–103. doi: 10.1353/jsh/13.1.83. [DOI] [PubMed] [Google Scholar]
- 5.Fairchild AL, Rosner D, Colgrove J, Bayer R, Fried LP. The exodus of public health: what history can tell us about its future. Am J Public Health. 2010;100(1):54–63. doi: 10.2105/AJPH.2009.163956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008. [DOI] [PubMed] [Google Scholar]
- 7.Our Cities, Our Health, Our Future: Acting on Social Determinants for Health Equity in Urban Settings. Report to the WHO Commission on Social Determinants of Health from the Knowledge Network on Urban Settings. Kobe: World Health Organization; 2008. [Google Scholar]
- 8.Boarnet MG. Planning’s role in building healthy cities: an introduction to the special issue. J Am Plann Assoc. 2006;72(1):5–9. doi: 10.1080/01944360608976719. [DOI] [Google Scholar]
- 9.Northridge ME, Sclar E, Biswas P. Sorting out the connections between the built environment and health: a conceptual framework for navigating pathways and planning healthy cities. J Urban Health. 2003;80:556–568. doi: 10.1093/jurban/jtg064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mabry PL, Olster DH, Morgan GD, Abrams DB. Interdisciplinarity and systems science to improve population health: a view from the NIH Office of Behavioral and Social Sciences Research. Am J Prev Med. 2008;35:211–224. doi: 10.1016/j.amepre.2008.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meadows DH. Thinking in Systems: A Primer. White River Junction: Chelsea Green Publishing; 2008. [Google Scholar]
- 12.Frieden T. A framework for public health action: health impact pyramid. Am J Public Health. 2010;100(4):590–595. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ashley L, Mikkelsen L, Cohen L. Restructuring Government to Address Social Determinants of Health. Oakland, CA: Prevention Institute and Trust for America’s Health; 2008. http://www.preventioninstitute.org/index.php?option=com_jlibrary&view=article&id=77&Itemid=127. Accessed July 20, 2010.
- 14.Schulz A, Northridge ME. Social determinants of health: implications for environmental health promotion. Health Educ Behav. 2004;31(4):455–471. doi: 10.1177/1090198104265598. [DOI] [PubMed] [Google Scholar]
- 15.Tsui EK. Sectoral job training as an intervention to improve health equity. Am J Public Health. 2010;100(4):S88–S94. doi: 10.2105/AJPH.2009.181826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Institute of Medicine. Local Government Actions to Prevent Childhood Obesity. Washington, DC: Institute of Medicine of the National Academies; 2009. http://www.iom.edu/Reports/2009/ChildhoodObesityPreventionLocalGovernments.aspx. Accessed July 20, 2010. [PubMed]
- 17.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31(1):7–20. doi: 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- 18.Day K. Active living and social justice: planning for physical activity in low-income, Black and Latino communities. J Am Plann Assoc. 2006;72(1):88–99. doi: 10.1080/01944360608976726. [DOI] [Google Scholar]
- 19.Handy S. Critical assessment of the literature on the relationships among transportation, land use, and physical activity. Resource paper for TRB Special Report 282: Does the Built Environment Influence Physical Activity? Examining the Evidence, written by the Transportation Research Board and Institute of Medicine Committee on Physical Activity, Health, Transportation, and Land Use; 2005. http://onlinepubs.trb.org/onlinepubs/archive/downloads/sr282papers/sr282Handy.pdf. Accessed July 20, 2010.
- 20.Sorry It’s Gone: Testing for Racial Discrimination in the Private Rental Sector, a General Investigation. London: Commission for Racial Equality; 1990. [Google Scholar]
- 21.Yinger J. Closed Doors, Opportunities Lost: The Continuing Costs of Housing Discrimination. New York: Russell Sage; 1995. [Google Scholar]
- 22.Boarnet MG, Greenwald M, McMillan TE. Walking, urban design, and health: toward a cost-benefit analysis framework. J Plann Educ Res. 2008;27(3):341–358. doi: 10.1177/0739456X07311073. [DOI] [Google Scholar]
- 23.Krizek KJ. Residential relocation and changes in urban travel: does neighborhood-scale urban form matter? J Am Plann Assoc. 2003;69(3):265–281. doi: 10.1080/01944360308978019. [DOI] [Google Scholar]
- 24.Rodriguez DA, Khattak AJ, Evenson KR. Can new urbanism encourage physical activity? Comparing a new urbanist neighborhood with conventional suburbs. J Am Plann Assoc. 2006;72(1):43–54. doi: 10.1080/01944360608976723. [DOI] [Google Scholar]
- 25.Handy S, Cao X-Y, Mokhtarian PL. Self-selection in the relationship between the built environment and walking: empirical evidence from northern California. J Am Plann Assoc. 2006;72(1):55–74. doi: 10.1080/01944360608976724. [DOI] [Google Scholar]
- 26.Lee C. Environment and active living: the roles of health risk and economic factors. Am J Health Promot. 2007;21(4):293–304. doi: 10.4278/0890-1171-21.4s.293. [DOI] [PubMed] [Google Scholar]
- 27.Lovasi GS, Bader M, Quinn J, Weiss C, Neckerman K, Rundle A. Neighborhood safety, aesthetics and body mass index in New York City. Obes. 2008;16(S1):S249. [Google Scholar]
- 28.Laraia BA, Siega-Riz AM, Kaufman JS, Jones SJ. Proximity of supermarkets is positively associated with diet quality index for pregnancy. Prev Med. 2004;39(5):869–875. doi: 10.1016/j.ypmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 29.Rose D, Richards R. Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public Health Nutr. 2004;7(8):1081–1088. doi: 10.1079/PHN2004648. [DOI] [PubMed] [Google Scholar]
- 30.Cummins S, Petticrew M, Higgins C, Findlay A, Sparks L. Large scale food retailing as an intervention for diet and health: quasi-experimental evaluation of a natural experiment. J Epidemiol Community Health. 2005;59(12):1035–1040. doi: 10.1136/jech.2004.029843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cummins S, Macintyre S. Food environments and obesity—neighbourhood or nation? Int J Epidemiol. 2006;35(1):100–104. doi: 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- 32.Musterd S. Social and ethnic segregation in Europe: levels, causes, and effects. J Urban Aff. 2005;27(3):331–348. doi: 10.1111/j.0735-2166.2005.00239.x. [DOI] [Google Scholar]
- 33.Krizek KJ, El-Geneidy A, Thompson K. A detailed analysis of how an urban trail system affects cyclists’ travel. Transp. 2007;34(5):611–624. doi: 10.1007/s11116-007-9130-z. [DOI] [Google Scholar]
- 34.Eyler AA, Matson-Koffman D, Young DR, et al. Quantitative study of correlates of physical activity in women from diverse racial/ethnic groups: the Women’s Cardiovascular Health Network Project—summary and conclusions. Am J Prev Med. 2003;25(3 Suppl 1):93–103. doi: 10.1016/S0749-3797(03)00170-3. [DOI] [PubMed] [Google Scholar]
- 35.Fry S, Cousins B, Olivola K. Health of Children Living in Urban Slums in Asia and the Near East: Review of Existing Literature and Data. Washington, DC: US Agency for International Development; 2002. http://www.ehproject.org/PDF/Activity_Reports/AR109ANEUrbHlthweb.pdf. Accessed July 20, 2010.
- 36.Ellen IH, Turner M. Do Neighborhoods Matter and Why? In: Goering JM, Feins JD, editors. Choosing a Better Life? Evaluating the Moving to Opportunity Social Experiment. Washington: The Urban Institute Press; 2003. pp. 313–338. [Google Scholar]
- 37.Kjellstrom T, Friel S, Dixon J, et al. Urban environmental health and health equity. J Urban Health. 2007;84(3 Suppl):i86–i97. doi: 10.1007/s11524-007-9171-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Institute of Medicine, Committee on Environmental Justice, Health Sciences Policy Program, Health Sciences Section. Toward Environmental Justice: Research, Education, and Health Policy Needs. Washington, DC: the National Academies Press; 1999. http://www.nap.edu/openbook.php?isbn=0309064074. Accessed July 20, 2010.
- 39.Ritz B, Yu F, Fruin S, Chapa G, Shaw GM, Harris JA. Ambient air pollution and risk of birth defects in southern California. Am J Epidemiol. 2002;155(1):17–25. doi: 10.1093/aje/155.1.17. [DOI] [PubMed] [Google Scholar]
- 40.Freeman AM. Distribution of Environmental Quality. In: Kneese V, Bower BT, Baltimore MD, editors. Environmental Quality Analysis: Theory and Methods in the Social Sciences. Baltimore: Johns Hopkins University Press; 1972. pp. 243–278. [Google Scholar]
- 41.Logan JRM, Luskin H. Urban Fortunes: The Political Economy of Place. Berkeley: University of California Press; 1987. [Google Scholar]
- 42.Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Cambridge: Harvard University Press; 1993. [Google Scholar]
- 43.Olden K. Impact of environmental justice investments. Am J Public Health. 2009;99(11):S484. doi: 10.2105/AJPH.2009.176602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morrison DS. Rallying point: Charles Lee’s long-standing career in environmental justice. Am J Public Health. 2009;99(11):S508–S510. doi: 10.2105/AJPH.2009.178590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Downey L. US metropolitan-area variation in environmental inequality outcomes. Urban Stud. 2007;44(5–6):953–977. doi: 10.1080/00420980701256013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wartenberg D, Greenberg MR, Harris G. Environmental justice: a contrary finding for the case of high-voltage electric power transmission lines. J Expo Sci Environ Epidemiol. 2010;20(3):237–244. doi: 10.1038/jes.2009.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ash M, Fetter TR. Who lives on the wrong side of the environmental tracks? Evidence from the EPA’s risk-screening environmental indicators model. Soc Sci Q. 2004;85(2):441–462. doi: 10.1111/j.0038-4941.2004.08502011.x. [DOI] [Google Scholar]
- 48.Pastor M, Sadd JL, Morello-Frosch R. Reading, writing, and toxics: children’s health, academic performance, and environmental justice in Los Angeles. Environ Plann, C Gov Policy. 2004;22(2):271–290. doi: 10.1068/c009r. [DOI] [Google Scholar]
- 49.Mohai P, Lantz PM, Morenoff J, House JS, Mero RP. Racial and socioeconomic disparities in residential proximity to polluting industrial facilities: evidence from the Americans’ Changing Lives Study. Am J Public Health. 2009;99(Suppl 3):S649–S656. doi: 10.2105/AJPH.2007.131383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bowen W. An analytical review of environmental justice research: what do we really know? Environ Manage. 2002;29(1):3–15. doi: 10.1007/s00267-001-0037-8. [DOI] [PubMed] [Google Scholar]
- 51.Massey DS. Ethnic residential segregation: a theoretical synthesis and empirical review. Sociol Soc Res. 1985;69(3):315–350. [Google Scholar]
- 52.Huttman ED, Blauw W, Saltman J. Urban Housing Segregation of Minorities in Western Europe and the United States. Durham: Duke University Press; 1991. [Google Scholar]
- 53.Dupont V. Socio-spatial differentiation and residential segregation in Delhi: a question of scale? Geoforum. 2003;35(2):157–175. doi: 10.1016/j.geoforum.2003.08.003. [DOI] [Google Scholar]
- 54.Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago: University of Chicago Press; 1987. [Google Scholar]
- 55.Jencks C, Mayer SE. The Social Consequences of Growing Up In a Poor Neighborhood. In: Lynn LE, McGeary MGH, editors. Inner City Poverty in the United States. Washington: The National Academies Press; 1990. [Google Scholar]
- 56.Anderson E. Code of the Street: Decency, Violence, and the Moral Life of the Inner City. New York: W.W. Norton; 1999. [Google Scholar]
- 57.Kleit RG. The role of neighborhood social networks in scattered-site public housing residents’ search for jobs. Hous Policy Debate. 2001;12(3):541–573. [Google Scholar]
- 58.Popkin S. New Findings on the Benefits and Limitations of Assisted Housing Mobility. Washington: Urban Institute; 2008. [Google Scholar]
- 59.Ellen IG, Turner MA. Does neighborhood matter? Assessing recent evidence. Hous Policy Debate. 1997;8(4):833–866. [Google Scholar]
- 60.Barton H, Tsourou C. Healthy Urban Planning. New York: Routledge; 2000. [Google Scholar]
- 61.Northridge ME. Integrating public health across sectors. Am J Public Health. 2010;100(2):200. doi: 10.2105/AJPH.2009.185926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Plsek P. Appendix B: Redesigning Health Care with Insights from the Science of Complex Adaptive Systems. In: Crossing the Quality Chasm: A New Health System for the 21st Century. Committee on Quality of Health Care in America, Institute of Medicine. Washington, DC: the National Academies Press; 2001. http://www.nap.edu/openbook.php?isbn=0309072808. Accessed July 20, 2010.
- 63.Gerberding JL. Protecting health—the new research imperative. JAMA. 2005;294:1403–1406. doi: 10.1001/jama.294.11.1403. [DOI] [PubMed] [Google Scholar]
- 64.Midgley G. Systemic intervention for public health. Am J Public Health. 2006;96(3):466–472. doi: 10.2105/AJPH.2005.067660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Minkler M. Linking science and policy through community-based participatory research to study and address health disparities. Am J Public Health. 2010;100(4):S81–S87. doi: 10.2105/AJPH.2009.165720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dannenberg AL, Bhatia R, Cole BL, Heaton SK, Feldman JD, Rutt CD. Use of health impact assessment in the U.S.: 27 case studies, 1999–2007. Am J Prev Med. 2008;34(3):241–256. doi: 10.1016/j.amepre.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 67.Homer JB, Hirsch GB. System dynamics modeling for public health: background and opportunities. Am J Public Health. 2006;96(3):452–458. doi: 10.2105/AJPH.2005.062059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Garau P, Sclar ED, Carolini GY, lead authors for the UN Millenium Project Task Force on Improving the Lives of Slum Dwellers. A Home in the City. London, UK: United Nations Development Programme; 2005.