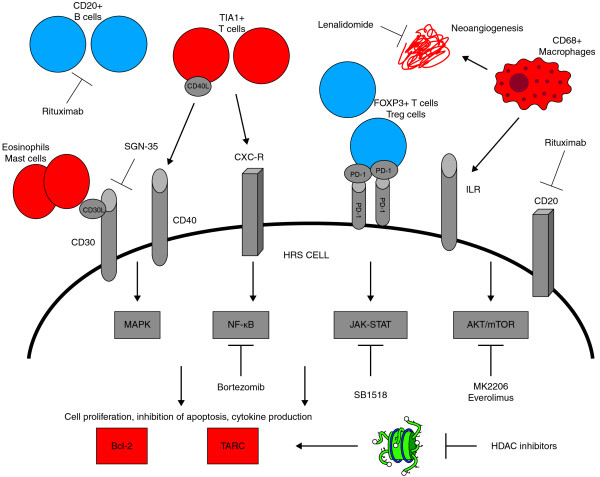
Figure 1.
Prognostic factors, pathways, and potential therapeutic targets involved in the pathogenesis of classical Hodgkin lymphoma. Prognostic factors associated with good outcome are shown in blue, and prognostic factors associated with poor outcome are shown in red.
This figure shows the most important prognostic factors involved in the pathogenesis of cHL, with particular attention to the role of tumor microenvironment, the main activated intracellular signaling pathways and potential targets for therapies. CD 20+ B cells and FOXP3 + T regulatory cells in the tumor microenvironment, are associated with good outcome, whereas CD 68+ macrophages, TIA1+ T cells and MAST cells are associated to poor prognosis. Also the expression of the antiapoptotic protein bcl-2 in HRS cells and increased plasma levels of the chemokine TARC have been related to worse prognosis. Notably the activation of intracellular signalling pathways mediated by autocrine and paracrine cytokine loops, leads to increased expression of bcl-2 and TARC production. The engagement of surface receptors such as CD 30, CD 40, CD 20, IL-R, CXC-R by their ligands, leads to the activation of the oncogenic NF-kB, JAK-STAT, AKT- mTOR and MAPK pathways. A number of drugs that selectively inhibit these targets are currently under clinical investigation.
Bcl-2, B-cell lymphoma 2; FOXP3, forkhead box P3; HDAC, histone deacetylase; HRS, Hodgkin and Reed-Sternberg; ILR, interleukin receptor; JAK, Janus kinase; MAPK, mitogen activated protein kinase; mTOR, mammalian target of rapamycin; NF, nuclear factor; PD-1, programmed death 1; PDL1, programmed death 1 ligand 1; TARC, thymus and activation-regulated chemokine; TIA1, cytotoxic granule-associated RNA-binding protein; Treg, regulatory T cell.