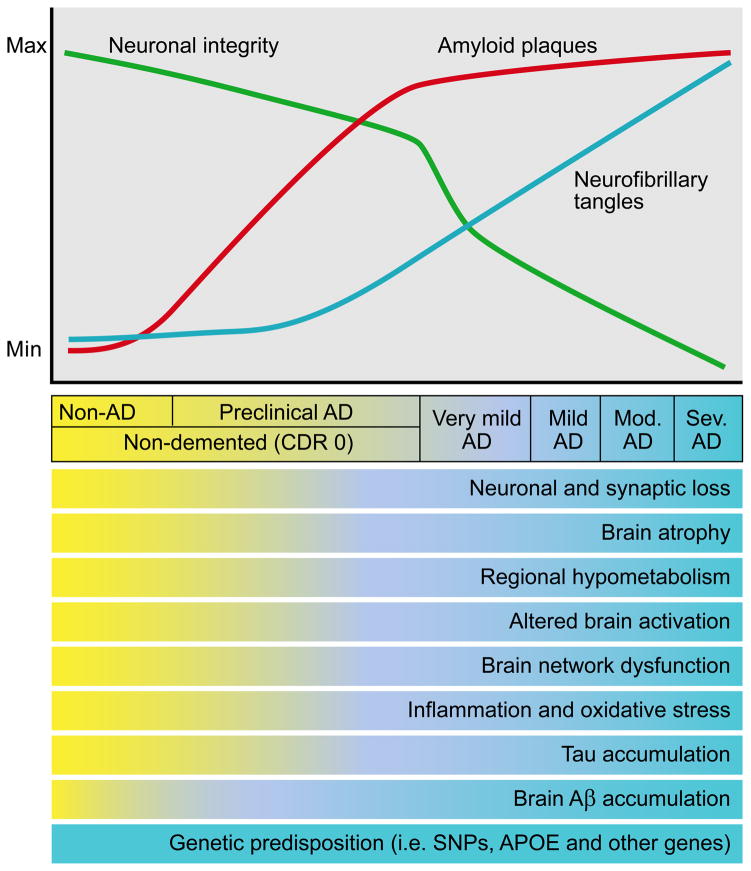
Figure 3.
Model of the time course of biomarker changes that occur in AD in relation to the cognitive and clinical changes. Over time, in cognitively normal people that is going to develop dementia due to AD, one of the first things that occurs is the initiation of Aβ aggregation in the brain in the form of amyloid plaques. Over years, while people are still cognitively normal, amyloid plaques continue to accumulate. At some point, perhaps ~ 5 years prior to any clearcut cognitive decline, tau accumulation begins to increase in the neocortex, inflammation and oxidative stress increase, and brain network connections and metabolism begin to decline. Neuronal and synaptic loss also begins to occur as well as brain atrophy. This period when AD-type pathology is building up yet a person is cognitively normal is termed “preclinical” AD. As these changes continue to accumulate, once there is enough neuronal and synaptic dysfunction as well as cell loss, very mild dementia becomes clinically detectable. At this time, amyloid deposition has almost reached its peak. As dementia worsens to mild, moderate (mod), and severe (sev) stages, there is increasing neurofibrillary tangle formation as well as increasing neuronal and synaptic dysfunction, inflammation, cell death, and brain atrophy. Modified figure reprinted with permission from R. J. Perrin et al., Nature 461, 916–922 (2009).