Abstract
Azithromycin is an azalide that acts by binding to the 50S ribosomal subunit of susceptible microorganisms and interfering with microbial protein synthesis. Azithromycin is also noted by anti-inflammatory and immunomodulatory activity. AzaSite® (Inspire Pharmaceuticals, Inc, Durham, NC) is azithromycin ophthalmic solution, 1% formulated in polycarbophil (the aqueous mucoadhesive polymer contained in DuraSite®) that delivers high and prolonged azithromycin concentrations in a variety of ocular tissues, including the conjunctiva, cornea and particularly the eyelid. AzaSite was approved by the Food and Drug Administration (FDA) in the US in 2007, for the treatment of bacterial conjunctivitis caused by susceptible isolates. This article aims to evaluate the peer-reviewed published scientific literature and to define well-established uses of AzaSite eye drops in the field of ocular infections.
Keywords: azithromycin, AzaSite, DuraSite
Introduction
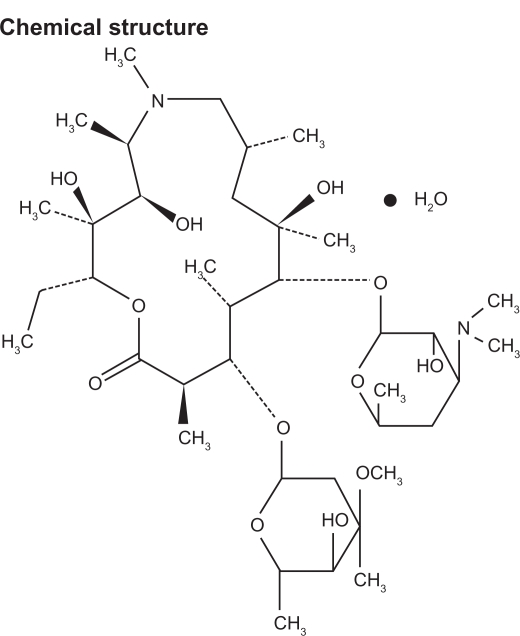
Azithromycin is an azalide, a subclass of macrolide antibiotics (Figure 1). AzaSite® (Inspire Pharmaceuticals, Inc, Durham, NC) is azithromycin ophthalmic solution, 1% formulated in polycarbophil (the aqueous mucoadhesive polymer contained in DuraSite®) that delivers the active drug to ocular surface tissues, over a period of time in a controlled fashion.1 Azithromycin is one of the few antibiotic classes that achieve therapeutic concentrations in the eye lids. The combination of inherent anti-inflammatory properties along with the high and prolonged tissue concentrations1,2 suggest that azithromycin ophthalmic solution, 1% has potential to serve as a treatment option for patients experiencing a wide range of conditions associated with the lid margin and ocular surface. AzaSite has been widely used by the ophthalmologists for various different indications in the field of ocular surface diseases.
Figure 1.
The chemical structure of the azithromycin molecule.
Antimicrobial and anti-inflammatory action of azithromycin
Azithromycin exhibits a broad spectrum activity against Gram-positive, Gram-negative, and atypical bacteria, by binding to the 50S ribosomal subunit of susceptible microorganisms and interfering with microbial protein synthesis. In 2007, the first ophthalmic formulation of azithromycin was approved by the Food and Drug Administration (FDA) in the US for the treatment of bacterial conjunctivitis caused by susceptible isolates (Table 1).3 Azithromycin has potency up to four times higher than erythromycin against Haemophilus influenza and Neisseria gonorrhea.4 Azithromycin is particularly effective against the intracellular organism Chlamydia trachomatis, the main cause of preventable blindness in developing countries, which affects the conjunctiva and lids.5
Table 1.
Antimicrobial activity of azithromycin
| Azithromycin has been shown to be efficacious on the following ocular pathogens: |
| Hemophilus influenzae |
| Staphylococcus aureus |
| Streptococcus mitis group |
| Streptococcus pneumoniae |
| CDC coryneform group G (efficacy studied in fewer than 10 infections) |
| Azithromycin has shown in vitro minimum inhibitory concentrations of equal or less against most (≥90%) of isolates of the following ocular pathogens: |
| Chlamydia pneumoniae |
| Chlamydia trachomatis |
| Legionella pneumophila |
| Moraxella catarrhalis |
| Mycoplasma hominis |
| Mycoplasma pneumoniae |
| Neisseria gonorrhoeae |
| Peptostreptococcus species |
| Streptococci (Groups C, F, G) |
| Streptococcus pyogenes |
| Streptococcus agalactiae |
| Ureaplasma urealyticum |
| Viridans group streptococci. |
A large body of preclinical and clinical observations has shown that azithromycin has anti-inflammatory and immunomodulatory properties independent of its antibacterial effect by virtue of its ability to inhibit the synthesis of proinflammatory mediators and cytokines by monocytes and epithelial cells, suppress the NF-κB signal transduction pathway, inhibit matrix metalloproteinases 2 and 9, promote expression of the anti-inflammatory cytokine IL-10, and inhibit the migration of inflammatory cells.6–11 In vitro studies indicate that azithromycin is highly concentrated within polymorphonuclear leukocytes, which gravitate by chemotactic mechanisms to sites of infection. The high intracellular concentration of azithromycin in inflammatory fluids of abscesses supports the observation of concentration-dependent killing of bacteria and prolonged persistent effects in tissues.1 In the setting of a murine model of surgically induced corneal inflammation, topical AzaSite twice daily led to significant suppression of corneal inflammation at the molecular and cellular levels (ie, significant decrease in messenger RNA expression levels of IL-1β, TNF-α and ICAM-1 in the cornea, and corneal leukocyte infiltration), although no anti-angiogenic effects were seen.12
The azithromycin ophthalmic solution, 1% (AzaSite®)
Given the hydrophobic nature of azithromycin, the aqueous ophthalmic preparations are not stable at room temperature. On the other hand, DuraSite is a polycarbophil (polymer of polyacrylic acid) bio-adhesive support matrix that allows longer persistence of the active compound on the eye surface, by forming hydrogen bonds with glycosaminoglycans in mucus. It releases the neutral, anionic and cationic small molecules that it binds with over a period of time in a controlled fashion.13 When a drop of AzaSite is applied to the ocular surface, the polymer returns to a gel state, which limits its loss through reflex tearing and naso-lacrimal drainage. Thus, the azithromycin formulation in DuraSite stays in contact with the ocular surface, delivering the drug over a period of hours,14 increasing the overall bioavailability of azithromycin.2 This property facilitates topical delivery of azithromycin and offers the benefit of a less-frequent dosing regimen. Additionally, in vitro studies have shown that the killing spectrum of 1% azithromycin in DuraSite appeared to be enhanced compared to the solution without DuraSite.15 DuraSite was found to play a greater role in the inhibition of staphylococcal biofilm formation by AzaSite, compared to azithromycin which only had a moderate inhibitory effect.16 In a clinical trial, 1% azithromycin in DuraSite eliminated 82% of Staphylococcus aureus, including some species that were considered resistant to azithromycin.17
Pharmacokinetics of azithromycin
Following oral administration, azithromycin is characterized by high-tissue distribution and prolonged elimination half-life, with relatively low plasma levels.18,19 It is taken up mainly by phagocytic cells and fibroblasts. During active phagocytosis, large concentrations of azithromycin are released directly to the site of infection.20,21 Plasma concentrations of azithromycin decrease in a polyphasic pattern, with an average terminal half-life of elimination of 68 hours.22
Studies that examined the ocular pharmacokinetics following oral administration of azithromycin in rabbits23,24 and in human subjects undergoing cataract surgery,25 revealed high drug concentrations in the tissues (ie, cornea, conjunctiva, iris, ciliary body) in contrast to relatively low concentrations in fluids (ie, vitreous humor and aqueous humor). This unique ocular distribution of azithromycin provides the rationale for the effectiveness of single administration oral azithromycin for the treatment of trachoma.5
Ocular pharmacokinetics after ocular administration was studied on 120 pigmented rabbits that were equally assigned to two groups (ie, 1% azithromycin formulated with the polymer polycarbophil (AzaSite) vs azithromycin ophthalmic solution without polycarbophil.).2 Each group received a single 30 μL eye drop of drug, which was deposited onto the center of the cornea. Peak concentrations of azithromycin in the tear film, conjunctiva and cornea with the 1% azithromycin with polycarbophil formulation were between 5- and 12-fold higher than those observed without polycarbophil; which persisted for the duration of the observation (ie, 7 days), indicating that the polycarbophil formulation increased the bioavailability of azithromycin. Additionally, the exposure of azithromycin measured as the area under curve (AUC) in the tear film following a single instillation was 3016 μg*h/g in the polycarbophil-containing formulation and 155 μg*h/g in the formulation without polycarbophil, representing a 19.5-fold increase of exposure for the formulation with polycarbophil. Consistent with the tendency of azithromycin to distribute preferentially in the tissues, the levels of azithromycin observed in the aqueous humor following ocular administration of both formulations were relatively low. The exposure of azithromycin in the eyelids 6 days after the last instillation in the multiple administration study was more than 2-fold higher than that observed in the conjunctiva. It was concluded that azithromycin may potentially be used in the treatment of ocular surface disorders that require chronic suppressive antibiotic treatment with or without anti-inflammatory effects. Following the FDA-approved dosing regimen for the treatment of bacterial conjunctivitis (ie, one drop twice a day for 2 days, followed by one drop per day for 5 days),3 clinically meaningful concentrations of azithromycin in the conjunctiva, cornea, and eyelids were observed as early as 1 hour after the first administration and the level of azithromycin remained high for up to 6 days after the end of treatment, providing therapeutic antibacterial levels of the drug.2
In the same study, an additional 156 pigmented rabbits received a 30 μL eye drop in the right eye following the FDA-approved dosing regimen for the treatment of bacterial conjunctivitis. Azithromycin was absorbed rapidly; and the peak concentrations continued to increase from dose-to-dose in the conjunctiva, cornea and eyelids throughout the 7-day treatment period, while trough concentrations stabilized within the first 2–3 days of dosing. The AUC(144–288 h) after the last dose was 4.2-fold greater in conjunctiva, 19.6-fold greater in cornea, and 13.3-fold greater in aqueous humor compared to AUC(0–144 h) after a single dose.2
Another study on the pharmacokinetic properties of a 1.5% azithromycin ophthalmic formulation in a medium chain triglyceride oil formulation in rabbits also reported high levels of drug concentration in the cornea and conjunctiva in contrast to relatively low levels in the aqueous humor after single and multiple administrations. In that study, the maximal concentrations of azithromycin achieved in all tissues were lower than those reported using the mucoadhesive polycarbophil formulation.26
A Phase IV, open-label, randomized, multicenter study designed to evaluate the pharmacokinetic properties in humans (Inspire Pharmaceuticals, Inc, Study 041-103) revealed that following single and multiple (twice daily for two days and once daily for the next 5 days) administration of azithromycin ophthalmic solution, 1%, the Cmax for aqueous humor was 0.053 μg/mL, but the Cmax for conjunctiva was over 10,000-fold higher, at 559.7 μg/g of tissue, indicating a substantial accumulation in conjunctiva. Total exposure to azithromycin, as measured by the AUC values, was also substantially greater for conjunctiva than for aqueous humor.27 In another study performed in humans who were scheduled to undergo cataract surgery and received AzaSite in the FDA-approved dosing regimen for bacterial conjunctivitis, conjunctival biopsies taken at the time of surgery were examined. The conjunctival concentrations of azithromycin above the minimum inhibitory concentration required for inhibition of growth of 90% of tested bacterial isolates were found approximately 24 hours after the last dose. The concentration of azithromycin was maintained more than 300 μg/mL after 7 days of therapy, with levels persisting above 50 μg/g for 5 days after stopping the drug.28 These results suggested that the drug penetrates into ocular surface tissues in high concentrations and persists in therapeutic concentrations for several days after therapy is discontinued, unlike the fluoroquinolones that partition readily in aqueous solution.28 Similarly in another open-label, active-controlled trial in healthy adult volunteers, after a single instillation of AzaSite into healthy human conjunctiva, azithromycin tissue concentrations peaked at 30 minutes after administration and remained high at therapeutic concentrations at 24 hours.29 In contrast, other studies have demonstrated that, when azithromycin in aqueous solution without DuraSite was administered topically, the concentrations of azithromycin in ocular surface tissues were negligible.2
Recently, the pharmacokinetics of a 2% ocular solution of azithromycin in DuraSite (AzaSite Xtra™) was analysed in forty-two male pigmented rabbits.30 Twenty-four hours after administration of a single drop, corneal and conjunctival concentrations exceeded the minimum inhibitory concentration breakpoint for the most common causative pathogens of bacterial conjunctivitis by 3.5- and 5.8-fold, respectively; whereas the plasma levels were four to five orders of magnitude lower than ocular tissue levels.
Safety profile and tolerability
Azithromycin ophthalmic solution has been studied at concentrations from 0.2% to 1% in a 14-day ocular toxicity study with four times daily dosing, and at 1% in two 30-day ocular toxicity studies with twice daily dosing in rabbits. No evidence of overt toxicity was observed in any study, by ophthalmoscopic or histopathological evaluation, as indicated by a lack of corneal degeneration, necrosis, inflammation, or edema.27 Cytoplasmic microvacuolation, most likely a manifestation of phospholipidosis, has been observed in corneal tissue sections. This was fully reversible after 60 days of posttreatment recovery. In rabbits treated with azithromycin 3% formulated in DuraSite twice daily for 30 days, focal corneal cloudiness of minimal grade was observed which was slowly reversible, and was not associated with corneal mineralization or other histopathological changes indicative of toxicity. Focal corneal cloudiness was not observed at concentrations of ≤2% in any study.
Azithromycin did not cause gene mutations in bacterial or mammalian cells in vitro, and did not cause chromosomal aberrations in human lymphocytes in vitro or mouse bone marrow cells in vivo.31 It has been used in adult and pediatric populations for over 10 years with no known association with carcinogenicity.27 No evidence of impaired fertility or teratogenicity was determined in mice or rats that received oral doses of ≤200 mg/kg/day.32
In the clinical trials, the azithromycin ophthalmic solution, 1% was reported to be well tolerated. The most frequently reported ocular adverse reaction reported in clinical trials involving subjects undergoing cataract surgery or subjects with blepharitis was eye irritation, which occurred in approximately 1%–2% of patients. Other adverse reactions associated with the use of AzaSite were reported in less than 1% of patients and included: burning, stinging and irritation upon instillation, contact dermatitis, corneal erosion, dry eye, dysgeusia, nasal congestion, ocular discharge, punctate keratitis, and sinusitis.27 On the other hand, in a subject-masked, randomized, active and placebo-controlled study that compared perceptions of subjects with normal ocular health for two antibiotic ophthalmic drops in contralateral eyes, moxifloxacin 0.5% ophthalmic solution (Vigamox®, Alcon Laboratories, Inc, Fort Worth, TX) was rated more comfortable and acceptable with less blurring than azithromycin 1% in DuraSite, in both adult and pediatric populations. Ocular adverse events (redness, irritation, stinging, burning, dryness, itching and chemosis) were observed in 18 (17.3%) eyes receiving azithromycin and one (1%) eye receiving moxifloxacin.33
The adverse effect levels for the neurological and cardiovascular safety studies were determined as 35,000 times and 350 times, respectively, the maximum intended daily clinical dose of 1% azithromycin ophthalmic solution (0.0286 mg/kg for a 70 kg human).27 At the plasma concentrations found with the instillation of AzaSite (in the ng/mL range), no arrhythmogenic effects or Q-T interval prolongation were observed.34
For the polycarbophil polymer (DuraSite), ocular topical administration at 0.6% and 1.3% concentrations to albino rabbits three times a day for at least 52 weeks was reported to elicit no evidence of ocular or systemic toxicity.27 However, in another randomized, masked, placebo-controlled animal study, DuraSite medications injected into the anterior chamber were found to induce acute inflammatory reaction with direct toxic effect and acute glaucoma by trabecular meshwork blockage.35
Ophthalmic uses of AzaSite®
Bacterial conjunctivitis
Azithromycin 1% in DuraSite (AzaSite) is the only FDA-approved topical formulation of azithromycin available and marketed in the US. Azithromycin has been shown to be efficacious on the most common bacterial pathogens of infective conjunctivitis (ie, Staphylococcus aureus, Haemophilus influenzae, Streptococcus pneumoniae) (Table 1).36 It is indicated for the treatment of bacterial conjunctivitis,37 with the recommended dosing regimen of one drop in the affected eye twice daily (8–12 hours apart) for the first 2 days, then one drop once daily for the next 5 days. Randomized controlled trials on AzaSite for the treatment of bacterial conjunctivitis are summarized in Table 2.3,15,33,38–42
Table 2.
Randomized controlled trials on azithromycin ophthalmic solution, for the treatment of bacterial conjunctivitis*
| Author | Quality | Number of patients (age range) | Indication | Dosage of azithromycin eye drop | Result |
|---|---|---|---|---|---|
| Abelson15 | Clinical efficacy | 159 patients received 1% azithromycin, 157 patients received 0.3% tobramycin (1 to 83 years old) | Clinically diagnosed bacterial conjunctivitis | bid on days 1 and 2, qd on days 3 to 5 | Clinical resolution 79.9% with AzaSite®, 78.3% with tobramycin; bacterial eradication 88.1% with AzaSite®, 94.3% with tobramycin at day 6 or 7 |
| Abelson3 | Clinical efficacy | 130 patients received 1% azithromycin, 149 patients received vehicle (1 to 96 years old) | Clinically diagnosed bacterial conjunctivitis | bid on days 1 and 2, qd on days 3 to 5 | Clinical resolution 63.1% with AzaSite®, 49.7% with vehicle; bacterial eradication 88.5% with AzaSite®, 66.4% with vehicle at day 6 or 7 |
| Abelson, Unpublished38 | Clinical efficacy | 685 patients (age not available) | Clinically diagnosed bacterial conjunctivitis | bid on days 1 and 2, qd on days 3 to 5 | Clinical resolution and bacterial eradication were significantly better in patients who received 1% azithromycin compared to patients who received vehicle |
| Heller, Unpublished39 | Safety and tolerability | 685 patients (1 to 96 years old) | Clinically diagnosed bacterial conjunctivitis | bid on days 1 and 2, qd on days 3 to 5 | 12% of patients had at least one adverse event in both groups of patients who received 1% azithromycin and who received vehicle |
| Protzko40 | Safety and tolerability | 343 patients received 1% azithromycin, 367 patients received 0.3% tobramycin (1 to 96 years old) | Clinically diagnosed bacterial conjunctivitis | bid on days 1 and 2, qd on days 3 to 5 | The most common adverse events were eye irritation, conjunctival hyperemia and worsening of bacterial conjunctivitis were observed in 1.1 to 1.9% of patients who received azithromycin and 1.1 to 2.1% of patients who received tobramycin. The rates of microbial eradication and bacterial infection recurrence were same in both groups. |
| Granet33 | Safety and tolerability | 84 subjects received 0.5% moxifloxacin and contralateral 1% azithromycin, 21 subjects received 0.5% moxifloxacin and contralateral placebo, 20 subjects received 1% azithromycin and contralateral placebo (≥9 years old) | Healthy subjects | One drop only | Moxifloxacin was rated more comfortable and acceptable with less blurring than azithromycin. Redness, irritation, stinging, burning, dryness, itching and chemosis were observed in 17.3% of eyes receiving azithromycin and 1% of eyes receiving moxifloxacin |
| Cochereau41 | Clinical efficacy and safety | 524 patients received 1.5% azithromycin, 519 patients received 0.3% tobramycin (4 days old to 87 years old) | Clinically diagnosed bacterial conjunctivitis | bid for 3 days | Clinical resolution 87.8% with azithromycin, 89.4% with tobramycin on day 9; bacterial eradication 85.2% with azithromycin, 83.8% with tobramycin at day 3, and 92.8% vs 94.6% at day 9, respectively. Treatment related minor adverse events (ie, burning, foreign body sensation, discharge) were noted in 3 patients in azithromycin group and 1 patient in tobramycin group |
| Bremond-Gignac42 | Clinical efficacy and safety | 73 patients received 1% azithromycin, 77 patients received 0.3% tobramycin (4 to 17 years old) | Clinically diagnosed bacterial conjunctivitis | bid for 3 days | Clinical resolution 80% with AzaSite®, 81.8% with tobramycin on day 9; bacterial eradication 94.1% with AzaSite®, 76.2% with tobramycin at day 3. Itching, burning, stinging were noted in 1 patient in azithromycin group and 2 patients in tobramycin group. |
Notes:
Table modified from McLean S, Sheikh A. Effectiveness, tolerability and safety of azithromycin 1% in DuraSite® for acute bacterial conjunctivitis. Patient Prefer Adherence. 2010;4:69–76.
In a randomized, vehicle-controlled, double-blind, multicenter clinical study in which patients were dosed in the FDA-approved dosing regimen, azithromycin ophthalmic solution, 1% was found to be superior to vehicle on days 6–7 in patients with a confirmed clinical diagnosis of bacterial conjunctivitis.3 Clinical resolution was achieved in 63.1% (82/130) of patients treated with azithromycin ophthalmic solution, compared to 49.7% (74/149) in patients that received the vehicle. The bacterial eradication rates were 88.5% and 66.4% in the AzaSite and vehicle groups, respectively. Furthermore, in a multicenter, randomised, investigator-masked study in adults and children with purulent bacterial conjunctivitis, azithromycin 1.5% (Azyter®, Laboratoires Thea, Clermont-Ferrand, France) for 3 days was found to be noninferior to tobramycin 0.3% for 7 days, for clinical and bacteriological cure. Moreover, more azithromycin than tobramycin patients presented an early clinical cure at day 3 (29.8% vs 18.6%). The safety profiles and tolerability of the two drugs were comparable.41
In another Phase III, parallel-group, controlled clinical trial that studied the efficacy of the 1% azithromycin in DuraSite for the resolution of signs and symptoms in participants with acute bacterial conjunctivitis, a regimen of 7 drops of 1% azithromycin in DuraSite was found to be equally effective as 20 drops of tobramycin (65% more drops). In that study, AzaSite was found to eradicate pathogens that are resistant to azithromycin in vitro, erythromycin, and fluoroquinolones, which suggested that systemic breakpoints may not be broadly applicable to ocular surface infections.15 A report from the active-controlled trial (clinicaltrials.gov NCT00105469) comparing the clinical and bacterial resolution rates in 710 patients with subjects aged 1 year or older, showed that the microbial eradication and clinical cure rates were equivalent for azithromycin 1% in DuraSite twice a day on days 1 and 2, followed by once daily on days 3 to 5 and tobramycin 0.3% four times daily for 5 days. Upon analysis of tolerability, azithromycin was found to be just as comfortable as tobramycin or vehicle.40 Similar results were also reported in a multicenter, randomized, investigator-masked study that compared six drops of azithromycin 1.5% eye drops (Azyter) with thirty-six drops of tobramycin 0.3% in 1043 patients with purulent bacterial conjunctivitis.43
A recent multicenter, randomized, investigator-masked, parallel-group study that included 150 children and adolescents of 4–17 years old found greater bacteriologic cure with azithromycin 1.5% eye drops (Azyter) twice daily for 3 days, compared to tobramycin 0.3% every two hours for 2 days, then four times daily for 5 days. Clinical cure was obtained faster with azithromycin compared to tobramycin (48% vs 27.3% on day 3, respectively) although similar overall cure rates were observed (80% vs 81.8% on day 9, respectively). Azithromycin treatment also eradicated bacteria that were defined as resistant, using classical antibiogram.42
Blepharitis and dry eye
Blepharitis is a chronic disorder producing inflammation of the anterior and posterior lid margin, with involvement of skin, mucocutaneous junction, and meibomian glands. It can also affect the conjunctiva, tear film, and corneal surface in advanced stages and may be associated with dry eye disease. It has also been suggested that chronic blepharitis may have an inflammatory etiology,44 in addition to bacterial infection.45 It is the resulting inflammation of the conjunctiva and cornea that are believed to cause the painful symptoms experienced by the patient and, in severe cases, can impair vision.46
Given the role of bacteria as one of the possible etiological determinants of blepharitis,45 it is believed that azithromycin ophthalmic solution, 1% could provide therapeutic benefit for this indication. The combination of anti-inflammatory properties along with the high and prolonged tissue concentrations suggest that azithromycin ophthalmic solution, 1% has potential to serve as a novel treatment option for patients experiencing signs and symptoms of blepharitis.2,47 Additionally, the altered ordering of the meibum lipids and resultant alteration of phase transition temperature seen in meibomian gland dysfunction was shown to be restored toward normal after topical azithromycin treatment, as shown by Fourier transform infrared spectroscopy.48
In a 2-week study comparing the efficacy of topical Aza-Site combined with warm compresses to warm compresses alone for the treatment of posterior blepharitis, the extent of lid margin redness, meibomian gland plugging, and quality of meibomian gland secretions improved statistically significantly in patients in the azithromycin group but not in patients in the warm compress-only group.49 In a multicenter study that randomized patients with moderate-to-severe blepharitis to warm compresses-only or warm compresses and topical 1% azithromycin for a 4-week course of treatment, the efficacy of azithromycin was rated as excellent or good in 70% of patients in the azithromycin group, compared with only 48% in the compress-only group at the end of treatment period. The improvements achieved in the azithromycin group persisted as long as 2 weeks after therapy had concluded.50 Similarly, in an open-label study of patients with moderate-to-severe blepharitis that evaluated changes in the signs and symptoms of anterior and posterior blepharitis after a treatment period of 4 weeks with AzaSite in the absence of warm compresses or eye scrubs, patient-rated symptom scores and investigator-rated assessment of the clinical signs of blepharitis were significantly improved from baseline levels. The improvement persisted for 4 weeks posttreatment.51
An open-label study conducted in patients with meibomian gland dysfunction also revealed that azithromycin 1.0% ophthalmic solution twice a day for 2 days, then every evening for a total of 30 days was effective in achieving significant improvement in the signs and symptoms associated with posterior blepharitis.52 In that study, vision-related function, ocular symptoms and environmental triggers were significantly improved after only 2 weeks of treatment, as shown by the reduction of the Ocular Surface Disease Index.
On the other hand, a multicenter, randomized, investigator-masked and active-controlled study (clinicaltrials. gov NCT01102244) enrolled 122 adult patients with moderate-to-severe blepharitis/blepharoconjunctivitis, randomized to tobramycin/dexamethasone ophthalmic suspension 0.3%/0.05% four times daily for 14 days or azithromycin ophthalmic solution 1% twice daily for 2 days followed by once daily for 12 days. The combination of tobramycin/dexamethasone provided faster inflammation relief compared to azithromycin, with a statistically significant lower mean total signs and symptoms score at Day 8.53
Recently, two Phase II, randomized, double-masked, placebo-controlled studies of different lengths (2 and 4 weeks, respectively) have been completed (clinicaltrials. gov NCT00894530 and NCT00892970), in which the primary outcome measure was eyelid margin erythema. Another study evaluated the effects of oral doxycycline100 μg twice daily for 2 months, oral essential fatty acids 1000 μg/day for 2 months, or topical AzaSite once daily for 1 month in expressing meibomian gland secretions before and after treatment in subjects with meibomian gland dysfunction and/or dry eye disease (clinicaltrials.gov NCT00803452).47
Trachoma
The World Health Organization recommends the SAFE strategy (ie, Surgery, Antibiotics, Facial cleanliness, Environmental improvement),54 with a goal of eliminating trachoma, the leading cause of infectious blindness worldwide,5,55 by year 2020. Azithromycin, having intracellular accumulation and long tissue half-life properties and high efficacy against Chlamydia trachomatis, represents an ideal antibiotic for this indication.
Although oral azithromycin was shown to treat trachoma effectively,56 an eye-drop formulation without the systemic side effects of oral administration would be beneficial in the treatment of this potentially blinding disease. In a randomised, controlled, double-masked, double-dummy, noninferiority explanatory study, azithromycin 1.5% eye drops (Azyter) twice daily for 2 or 3 days were noninferior to World Health Organization’s reference treatment, azithromycin single 20 mg/kg oral dose for the treatment of trachoma in children.57 Likewise, an epidemiological study that was carried out in the Republic of Cameroon revealed that after two topical mass treatments 1 year apart, which involved one instillation of azithromycin 1.5% in both eyes twice daily for 3 consecutive days, lead to reduction of active forms of trachoma 1 year after the second treatment, from 31.5% to 3.1% (ie, a total reduction of 90%) in a population of children between 1 and 10 years.58,59
Conclusion
Current literature supports the efficacy and safety of topical azithromycin ophthalmic 1% solution DuraSite (AzaSite) in the treatment of various ocular surface disorders, particularly bacterial conjunctivitis, blepharitis and dry eye. The combination of anti-inflammatory properties along with high and prolonged tissue concentrations, particularly in the lid margin and ocular surface due to polycarbophil (the aqueous mucoadhesive polymer contained in DuraSite) suggest that azithromycin ophthalmic solution, 1% has potential to serve as a treatment option for patients experiencing a wide range of conditions associated with the lid margin and ocular surface. Treatment of trachoma with topical azithromycin ophthalmic 1% solution is also encouraging.
Footnotes
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Amsden GW. Advanced-generation macrolides: tissue directed antibiotics. Int J Antimicrob Agents. 2001;18(Suppl 1):S11–S15. doi: 10.1016/s0924-8579(01)00410-1. [DOI] [PubMed] [Google Scholar]
- 2.Akpek EK, Vittitow J, Verhoeven RS, et al. Ocular surface distribution and pharmacokinetics of a novel ophthalmic 1% azithromycin formulation. J Ocul Pharmacol Ther. 2009;25(5):433–439. doi: 10.1089/jop.2009.0026. [DOI] [PubMed] [Google Scholar]
- 3.Abelson MB, Heller W, Shapiro AM, et al. Clinical cure of bacterial conjunctivitis with azithromycin 1%: vehicle-controlled, double-masked clinical trial. Am J Ophthalmol. 2008;145(6):959–965. doi: 10.1016/j.ajo.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 4.Retsema J, Girard A, Schelkly W, et al. Spectrum and mode of action of azithromycin (CP-62,993), a new 15-membered-ring-macrolide with improved potency against gram-negative organisms. Antimicrob Agents Chemother. 1987;31(12):1939–1947. doi: 10.1128/aac.31.12.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.West SK. Azithromycin for control of trachoma. Community Eye Health. 1999;12(32):55–56. [PMC free article] [PubMed] [Google Scholar]
- 6.Ianaro A, Ialenti A, Maffia P, et al. Anti-inflammatory activity of macrolide antibiotics. J Pharmacol Exp Ther. 2000;292(1):156–163. [PubMed] [Google Scholar]
- 7.Piacentini GL, Peroni DG, Bodini A, et al. Azithromycin reduces bronchial hyperresponsiveness and neutrophilic airway inflammation in asthmatic children: a preliminary report. Allergy Asthma Proc. 2007;28(2):194–198. doi: 10.2500/aap.2007.28.2958. [DOI] [PubMed] [Google Scholar]
- 8.Howe RA, Spencer RC. Macrolides for the treatment of Pseudomonas aeruginosa infections? J Antimicrob Chemother. 1997;40(2):153–155. doi: 10.1093/jac/40.2.153. [DOI] [PubMed] [Google Scholar]
- 9.Hoffmann N, Lee B, Hentzer M, et al. Azithromycin blocks quorum sensing and alginate polymer formation and increases the sensitivity to serum and stationary-growth-phase killing of Pseudomonas aeruginosa and attenuates chronic P. aeruginosa lung infection in Cftr(−/−) mice. Antimicrob Agents Chemother. 2007;51(10):3677–3687. doi: 10.1128/AAC.01011-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amsden GW. Anti-inflammatory effects of macrolides – an underappreciated benefit in the treatment of community-acquired respiratory tract infections and chronic inflammatory pulmonary conditions? J Antimicrob Chemother. 2005;55(1):10–21. doi: 10.1093/jac/dkh519. [DOI] [PubMed] [Google Scholar]
- 11.Jacot JL, Jacot TA, Sheppard JD, et al. Evaluation of MMP 2/9 modulation by AzaSite and DuraSite in human corneal epithelial cells and bovine corneal endothelial cells in vitro. Poster presented at The Association for Research in Vision and Ophthalmology (ARVO) 2008 Annual Meeting; 2008 Apr 28; Fort Lauderdale, FL. abstract 1985. [Google Scholar]
- 12.Sadrai Z, Hajrasouliha AR, Chauhan S, Saban DR, Dastjerdi MH, Dana R. Effect of topical azithromycin on corneal innate immune response. Invest Ophthalmol Vis Sci. 2011;52(5):2525–2531. doi: 10.1167/iovs.10-5658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bowman L, Si E, Pang J, Archibad R, Friedlaender M. Development of a topical polymeric mucoadhesive ocular delivery system for azithromycin. J Ocul Pharmacol Ther. 2009;25(2):133–139. doi: 10.1089/jop.2008.0066. [DOI] [PubMed] [Google Scholar]
- 14.Bowman LM, Si E, Pang J, Friedlaender M. Development of a commercial eye drop formulation of azithromycin. Poster presented at The Association for Research in Vision and Ophthalmology (ARVO) 2007 Annual Meeting; 2007 May 6–10; Fort Lauderdale, FL. e-Abstract 772. [Google Scholar]
- 15.Abelson M, Protzko E, Shapiro A, Garces-Soldana A, Bowman L, 1% azithromycin in DuraSite Clinical Study Group A randomized trial assessing the clinical efficacy and microbial eradication of 1% azithromycin ophthalmic solution vs tobramycin in adult and pediatric subjects with bacterial conjunctivitis. Clin Ophthalmol. 2007;1(2):177–182. [PMC free article] [PubMed] [Google Scholar]
- 16.Wu EC, Kowalski RP, Romanowski EG, Mah FS, Gordon YJ, Shanks RM. AzaSite® inhibits Staphylococcus aureus and coagulase-negative Staphylococcus biofilm formation in vitro. J Ocul Pharmacol Ther. 2010 Dec;26(6):557–562. doi: 10.1089/jop.2010.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harper DG, Chen CE, Friedlaender MH. Controlled comparison of two fluorometholone formulations in the antigen challenge model of allergic conjunctivitis. CLAO J. 1995;21(4):256–260. [PubMed] [Google Scholar]
- 18.Liu P, Allaudeen H, Chandra R, et al. Comparative pharmacokinetics of azithromycin in serum and white blood cells of healthy subjects receiving a single-dose extended-release regimen versus a 3-day immediate-release regimen. Antimicrob Agents Chemother. 2007;51(1):103–109. doi: 10.1128/AAC.00852-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schentang JJ, Ballow CH. Tissue-directed pharmacokinetics. Am J Med. 1991;91(3A):5S–11S. doi: 10.1016/0002-9343(91)90394-d. [DOI] [PubMed] [Google Scholar]
- 20.Gladue RP, Snider ME. Intracellular accumulation of azithromycin by cultured human fibroblasts. Antimicrob Agents Chemother. 1999;34(6):1056–1060. doi: 10.1128/aac.34.6.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gladue RP, Bright GM, Isaacson RE, Newborg MF. In vitro and in vivo uptake of azithromycin (CP-62,993) by phagocytic cells: possible mechanism of delivery and release at sites of infection. Antimicrob Agents Chemother. 1989;33(3):277–282. doi: 10.1128/aac.33.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rapp RP. Pharmacokinetics and pharmacodynamics of intravenous and oral azithromycin: enhanced tissue activity and minimal drug interactions. Ann Pharmacother. 1998;32(7–8):785–793. doi: 10.1345/aph.17299. [DOI] [PubMed] [Google Scholar]
- 23.Karcioglu ZA, Ahmed WS, Raines D, El-Yazigi A. Pharmacokinetics of azithromycin rabbit lacrimal glands and conjunctiva. Ophthalmic Res. 1999;31(1):47–52. doi: 10.1159/000055512. [DOI] [PubMed] [Google Scholar]
- 24.O’Day DM, Head FS, Foulds G, Robinson RD, Williams TE, Ferraina RA. Ocular pharmacokinetics of orally administered azithromycin in rabbits. J Ocul Pharmacol. 1994;10(4):633–641. doi: 10.1089/jop.1994.10.633. [DOI] [PubMed] [Google Scholar]
- 25.Tabbara KF, Al-Kharashi SA, Al-Mansouri SM, et al. Ocular levels of azithromycin. Arch Ophthalmol. 1998;116(12):1625–1628. doi: 10.1001/archopht.116.12.1625. [DOI] [PubMed] [Google Scholar]
- 26.Amar T, Caillaud T, Elena P. Ocular pharmacokinetic study following single and multiple azithromycin administrations in pigmented rabbits. Curr Eye Res. 2008;33(2):149–158. doi: 10.1080/02713680701860499. [DOI] [PubMed] [Google Scholar]
- 27.Inspire Pharmaceuticals, Inc; Raleigh, NC: Nov 12, 2009. Investigator’s Brochure, Azithromycin Ophthalmic Solution 1%, ed 2.0. [Google Scholar]
- 28.Stewart WC, Crean CS, Zink RC, Brubaker K, Haque R, Hwang DG. Pharmacokinetics of azithromycin and moxifloxacin in human conjunctiva and aqueous humor during and after the approved dosing regimens. Am J Ophthalmol. 2010;150:744–751. doi: 10.1016/j.ajo.2010.05.039. [DOI] [PubMed] [Google Scholar]
- 29.Torkildsen G, O’Brien TP. Conjunctival tissue pharmacokinetic properties of topical azithromycin 1% and moxifloxacin 0.5% ophthalmic solutions: a single-dose, randomized, open-label, active-controlled trial in healthy adult volunteers. Clin Ther. 2008;30(11):2005–2014. doi: 10.1016/j.clinthera.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 30.Si PC, Cheung PS, Bowman L, Hosseini K. Ocular pharmacokinetics of Azasite Xtra – 2% azithromycin formulated in a DuraSite delivery system. Curr Eye Res. 2009;34(6):485–491. doi: 10.1080/02713680902919532. [DOI] [PubMed] [Google Scholar]
- 31.Amacher DE, Ellis JH, Joyce AJ, et al. Preclinical toxicology studies with azithromycin: genetic toxicology evaluation. Mutat Res. 1993;300:79–90. doi: 10.1016/0165-1218(93)90125-w. [DOI] [PubMed] [Google Scholar]
- 32.Stadnicki SW, Kessedijan M, Stadler J, Tachibana M. Preclinical reproductive and teratology studies with azithromycin. Oyo Yakuri/Pharmacometrics. 1996;51:85–95. [Google Scholar]
- 33.Granet D, Lichtenstein SJ, Onofney B, Katz JA. An assessment of the tolerability of moxifloxacin 0.5% compared to azithromycin 1.0% in DuraSite. Clin Ophthalmol. 2007;1(4):519–525. [PMC free article] [PubMed] [Google Scholar]
- 34.Ohtani H, Taninaka C, Hanada E, et al. Comparative pharmacodynamic analysis of Q-T interval prolongation induced by the macrolides clarithromycin, roxithromycin, and azithromycin in rats. Antimicrob Agents Chemother. 2000;44(10):2630–2637. doi: 10.1128/aac.44.10.2630-2637.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ness PJ, Mamalis N, Werner L, et al. An anterior chamber toxicity study evaluating Besivance, AzaSite, and Ciprofloxacin. Am J Ophthalmol. 2010;150(4):498–504. doi: 10.1016/j.ajo.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 36.Seal DV, Barrett SP, McGill JI. Aetiology and treatment of acute bacterial infection of the external eye. Br J Ophthalmol. 1982;66:357–360. doi: 10.1136/bjo.66.6.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Durham, NC: inspire Pharmaceuticals; 2008. AzaSite [package insert] [Google Scholar]
- 38.Abelson M, Heller W. Efficacy of azithromycin 1% eye drops vs vehicle as first line therapy for bacterial conjunctivitis. 2006. Unpublished study the Cochrane Register of Controlled Trials (CENTRAL). ID CN00634804.
- 39.Heller W, Abelson M, Group TAS Safety and tolerabiltiy of azithromycin 1% eye drops as anti-infective therapy for bacterial conjunctivitis. Unpublished study for the Cochrane Register of Controlled Trials (CENTRAL). Study ID CN 00634521.
- 40.Protzko E, Bowman L, Abelson M, Shapiero A, Group TACS Phase 3 safety comparisons for 1% azithromycin in polymeric mucoadhesive eye drops versus 0.3% tobramycin eye drops for bacterial conjunctivitis. Invest Ophthalmol Vis Sci. 2007;48(8):3425–3429. doi: 10.1167/iovs.06-1413. [DOI] [PubMed] [Google Scholar]
- 41.Cochereau I, Meddeb-Ouertani A, Khairallah M, et al. 3-day treatment with azithromycin 1.5% eye drops versus 7-day treatment with tobramycin 0.3% for purulent bacterial conjunctivitis: multicentre, randomised and controlled trial in adults and children. Br J Ophthalmol. 2007;91(4):465–469. doi: 10.1136/bjo.2006.103556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bremond-Gignac D, Mariani-Kurkdjian P, Beresniak A, et al. Efficacy and safety of azithromycin 1.5% eye drops for purulent bacterial conjunctivitis in pediatric patients. Pediatr Infect Dis J. 2010;29(3):222–226. doi: 10.1097/INF.0b013e3181b99fa2. [DOI] [PubMed] [Google Scholar]
- 43.Robert PY, Bourcier T, Meddeb-Ouertani A, et al. [Efficacy assessment of azithromycin 1.5% eye drops versus tobramycin 0.3% on clinical signs of purulent bacterial conjunctivitis] J Fr Ophtalmol. 2010;33(4):241–248. doi: 10.1016/j.jfo.2010.01.005. French. [DOI] [PubMed] [Google Scholar]
- 44.Seal DV, McGill JI, Jacobs P, Liakos GM, Goulding NJ. Microbial and immunological investigations of chronic non-ulcerative blepharitis and meibomianitis. Br J Ophthalmol. 1985;69(8):604–611. doi: 10.1136/bjo.69.8.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smith RE, Flowers CW. Chronic blepharitis: a review. CLAO J. 1995;21(3):200–207. [PubMed] [Google Scholar]
- 46.McDermott AM, Perez V, Huang AJ, et al. Pathways of corneal and ocular surface inflammation: a perspective from the cullen symposium. Ocul Surf. 2005;3(Suppl 4):S131–S138. doi: 10.1016/s1542-0124(12)70238-0. [DOI] [PubMed] [Google Scholar]
- 47.Luchs J. Azithromycin in DuraSite for the treatment of blepharitis. Clin Ophthalmol. 2010;4:681–688. doi: 10.2147/opth.s6370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Foulks GN, Borchman D, Yappert M, Kim SH, McKay JW. Topical azithromycin therapy for meibomian gland dysfunction: clinical response and lipid alterations. Cornea. 2010;29(7):781–788. doi: 10.1097/ICO.0b013e3181cda38f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Luchs J. Efficacy of topical azithromycin ophthalmic solution 1% in the treatment of posterior blepharitis. Adv Ther. 2008;25(9):858–870. doi: 10.1007/s12325-008-0096-9. [DOI] [PubMed] [Google Scholar]
- 50.Trattler WB, Kuhn KL, Haque R, Zink RC, Sall KN, Luchs J. Topical azithromycin improves blepharitis signs and symptoms. Presented at The American Society of Cataract and Refractive Surgery; 2009 Apr 3–8; San Francisco, CA. [Google Scholar]
- 51.Haque RM, Torkildsen GL, Brubaker K, et al. Multi-center, open-label study evaluating the efficacy of azithromycin ophthalmic solution 1% on the signs and symptoms of subjects with blepharitis. Cornea. 2010;29(8):871–877. doi: 10.1097/ICO.0b013e3181ca38a0. [DOI] [PubMed] [Google Scholar]
- 52.Opitz DL, Tyler KF. Efficacy of azithromycin 1% ophthalmic solution for treatment of ocular surface disease from posterior blepharitis. Clin Exp Optom. 2011;94(2):200–206. doi: 10.1111/j.1444-0938.2010.00540.x. [DOI] [PubMed] [Google Scholar]
- 53.Torkildsen GL, Cockrum P, Meier E, Hammonds WM, Silverstein B, Silverstein S. Evaluation of clinical efficacy and safety of tobramycin/dexamethasone ophthalmic suspension 0.3%/0.05% compared to azithromycin ophthalmic solution 1% in the treatment of moderate to severe acute blepharitis/blepharoconjunctivitis. Curr Med Res Opin. 2011;27(1):171–178. doi: 10.1185/03007995.2010.539603. [DOI] [PubMed] [Google Scholar]
- 54.Mariotti SP, Prüss A, World Health Organization . 2001. The safe strategy. Preventing trachoma. A guide for environmental sanitation and improved hygiene; pp. 1–36. WHO/PBD/GET/00.7/ Rev 1. [Google Scholar]
- 55.Resnikoff S, Pascolini D, Etya’ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–851. [PMC free article] [PubMed] [Google Scholar]
- 56.Tabbara KF, Abu-El-Asrar A, Al-Omar O, Choudhury AH, Al-Faisal Z. Single dose azithromycin in the treatment of trachoma. A randomized controlled study. Ophthalmology. 1996;103(5):842–846. doi: 10.1016/s0161-6420(96)30605-2. [DOI] [PubMed] [Google Scholar]
- 57.Cochereau I, Goldschmidt P, Goepogui A, et al. Efficacy and safety of short duration azithromycin eye drops versus azithromycin single oral dose for the treatment of trachoma in children: a randomised, controlled, doublemasked clinical trial. Br J Ophthalmol. 2007;91(5):667–672. doi: 10.1136/bjo.2006.099275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Amza A, Goldschmidt P, Einterz E, et al. Elimination of active trachoma after two topical mass treatments with azithromycin 1.5% eye drops. PLoS Negl Trop Dis. 2010;4(11):e895. doi: 10.1371/journal.pntd.0000895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huguet P, Bella L, Einterz EM, Goldschmidt P, Bensaid P. Mass treatment of trachoma with azithromycin 1.5% eye drops in the Republic of Cameroon: feasibility, tolerance and effectiveness. Br J Ophthalmol. 2010;94(2):157–160. doi: 10.1136/bjo.2009.161513. [DOI] [PMC free article] [PubMed] [Google Scholar]