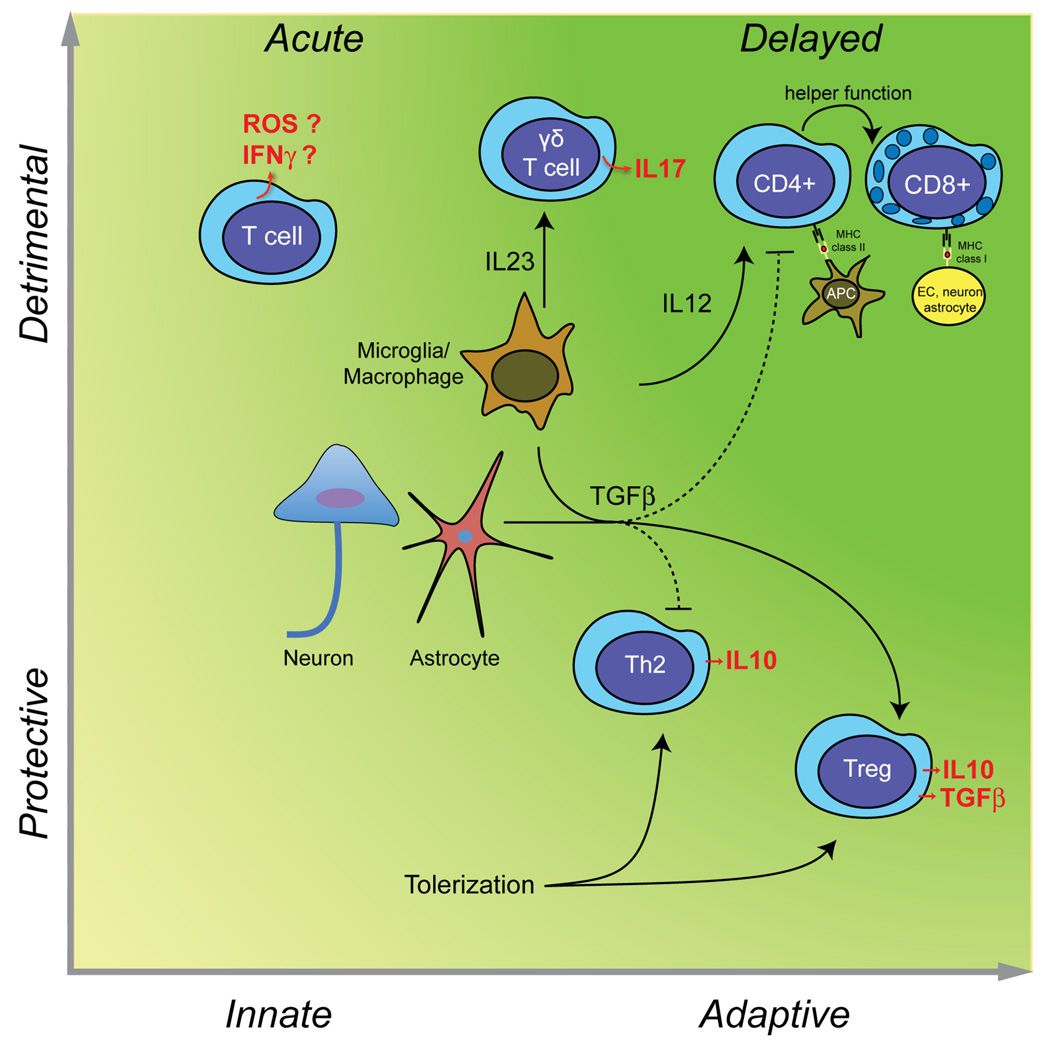
Figure 3. Deleterious and beneficial roles of T cells in stroke.
In the acute phase of cerebral ischemia, unprimed T cells contribute to tissue damage in an antigen independent manner (innate immunity), possibly through IFNγ151 and ROS152 (left upper quadrant). γδT cells, activated by IL-23 released from microglia/macrophages, produce the cytotoxic cytokine IL-17 and contributes to acute ischemic brain injury41. However, T cells can also be protective. TGFβ produced by neurons, glia, or macroglia/macrophages promotes the development of Treg cells secreting the protective cytokine IL-10 and inhibits Th1 and Th2 responses. Treg cells are protective in models of cerebral ischemia42. Induction of mucosal tolerance with CNS antigens produces an adaptive response, which leads to the establishment of autoreactive Th2 cells producing IL-1048 and Treg cells producing IL-10 and TGFβ107,141 is highly protective in experimental stroke (right lower quadrant). As discussed in the text, there is no evidence that adaptive immunity contributes to acute ischemic brain injury. However, weeks and months after stroke, autoreactive CD4+ and CD8+ T cells targeting CNS antigens could develop (right upper quadrant). The resulting cell death could play a role in the delayed brain damage and atrophy that occurs after stroke83.