Abstract
Background
Seniors frequently struggle during the transition home following an acute hospitalization resulting in frequent rehospitalizations. Studies consistently show a lack of comprehension of discharge instructions.
Objectives
To determine the frequency of low cognition at hospital discharge among community dwelling seniors and the changes in cognition that occur one month following hospitalization.
Design
Face-to-face surveys were performed at hospital discharge and one month later in the home of the subject. The Mini-Mental Status Examination (MMSE), Backward Digit Span, and 15 Word Immediate and Delayed Recall Tests were used to evaluate cognition. Low cognition was determined to be a score of less than 25 on the MMSE for subjects with high school education and less than 18 for subjects with less than high school education.
Participants
Two hundred community-dwelling seniors ≥ 70 years, admitted to acute medicine services >24 hours, consenting to their own procedures, not having previously documented cognitive loss, and not admitted for cognitive changes.
Results
Upon hospital discharge, 31.5% of subjects had previously unrecognized low cognition. One month later, 58% of these patients no longer had low cognition (p < 0.001). Of those subjects with low cognition, the MMSE improved by an average of 4 points one month post-discharge. Within the MMSE, subjects experienced significant improvements in the areas of orientation, registration, repetition, comprehension, naming, reading, writing, and calculation.
Conclusion
Low cognition at discharge is common among elderly patients without dementia, and cognition often improves one month post-hospitalization. Seniors may not comprehend discharge instructions, and patient self-management may be better taught as an outpatient following discharge rather than at the time of hospital discharge. Discharge interventions should incorporate screening of seniors for low cognition prior to hospital discharge to provide optimal transitional care.
KEY WORDS: seniors, cognition, post-discharge
INTRODUCTION
Discharge from the hospital to home is a challenging process for seniors. Hospital staff give seniors a tremendous amount of information at discharge including medication changes, dietary restrictions, test results, and home health care plans1. Seniors are expected to understand these and then navigate transportation, obtain new medications, and schedule new appointments following hospitalization.2,3 All these responsibilities place a huge burden on the recovering senior.
Almost one-fifth (19.4%) of hospitalized seniors are rehospitalized within 30 days4. Studies have shown that the transition of older adults from hospital to home is associated with high rates of preventable medication errors, accelerated functional decline, nursing home placement, and mortality 5–9. 10–12, Jencks et al. have estimated that the cost to Medicare of unplanned rehospitalizations was over $17.4 billion in 20044.
Several interventions exist with the goal to reduce rehospitalizations. Project BOOST from the Society of Hospital Medicine focuses on day of hospital discharge with phone call follow-up 2–3 days later13. The Care Transition ProgramTM focuses on empowering seniors and improving their self-management skills with the use of home nurse visits or transition coaches and phone call follow-up.14 Project Re-Engineered Discharge centers on patient education at day of discharge and through phone call 2–3 days later15. All of these interventions concentrate initially on the patient at hospitalization and their obtaining of discharge instructions. While there is post-hospital follow-up either through home visits or phone calls in these interventions, specific data supporting the best timing of this follow-up is lacking.
Current discharge strategies may be ineffective as Jha et al. found that among hospitalized heart failure patients, there was no significant difference in rehospitalization rates between hospitals with complete vs. incomplete discharge documentation16. Calkins et al. showed only 57% of patients reported that they understood their discharge instructions17. Maniaci et al. phoned patients between 4 and 18 days after discharge and found that 86% were aware that they had been prescribed new medications, but fewer could identify the name (64%) of new medications or their dosages (56%) and only 11% could recall being told of any adverse effects, with older patients answering fewer questions correctly (P= 0.02).18 Understanding and recall of discharge instructions may be imperative to the success of seniors avoiding rehospitalization.
Cognition of seniors may be a key factor in the recall of discharge instructions. Studies have shown that seniors who are hospitalized face increased rates of depression, adverse drug events, and decreased physical functioning19–22. Hospitalized seniors are further weakened by sleep deprivation, receiving medications with sedating side effects, undergoing multiple tests, withholding of meals, and the acute illness causing the hospitalization9. These insults impact cognition and multiple studies have shown that cognition is impaired during the hospitalization23,24 Inouye et al. has also shown that many patients hospitalized with cognitive decline had reversibility in one year25.
No prior studies have investigated the frequency of cognitive loss at hospital discharge among seniors returning home. Subsequently, no prior studies have assessed whether cognition improves between hospital discharge and one month following hospitalization. This study aims to longitudinally examine cognitive function among community-dwelling seniors at discharge from an acute hospitalization and one month following hospital discharge.
METHODS
Recruitment of Subjects
The Institutional Review Board of Northwestern University Feinberg School of Medicine approved this study. Research staff recruited consecutive community-dwelling seniors aged 70 and older who were hospitalized to the acute medicine services at Northwestern Memorial Hospital. Accessing the hospital electronic health record, research staff queried admission information and contacted the hospital physician to determine potential subject eligibility. Subjects were excluded if they were (1) blind or had a severe vision problem that could not be corrected with glasses [since vision is needed for completion of the memory tests], (2) unable to consent to their own procedures while hospitalized [which implies known cognitive dysfunction], (3) admitted for mental status changes or cognition issues [since cognition was being tested, we wanted no influences from a previously known medical condition] (4) reliant on a caregiver or home aide services 8 hours or greater per day [which frequently implies a cognitive impairment or answered need for support], (5) expected to have a hospital length of stay of less than 24 hours [due to a logistics], or (6) living outside of a 60 mile radius of the hospital [due to logistics]. Subjects were also excluded if they had documented cognitive loss in the past medical history of their admission history and physical, specifically history of mild cognitive impairment, cognitive disorder, dementia, Alzheimer’s disease, vascular dementia, or memory loss. While hospitalized, patients were also evaluated for delirium using the Confusion Assessment Method (CAM) and excluded if positive26. Patients admitted to the medicine inpatient service are administered the CAM by the nursing staff twice a day with hourly rechecks if there is concern. Nurses have received training on the use of the CAM and are evaluated on their skill as part of their core competencies. Results are recorded in the patient’s Electronic Health Record.
Interviews
Research staff conducted structured in-person surveys of eligible hospitalized subjects within 24 hours prior to hospital discharge (i.e. day of discharge). Surveys were conducted in the private hospital rooms of subjects to maintain confidentiality. Subjects did not receive compensation for their participation. After written informed consent was obtained, research staff began the interview with cognitive testing to reduce the survey burden skewing the cognitive results. Subsequently, the interviewer obtained demographic information from the subject as well as ascertain their availability in one month, support system, medications, and primary care physician. A different research staff member visited subjects in their homes one month following discharge and repeated the below cognitive function testing. All research staff received the same training on administering the cognitive testing. Research staff, who conducted the one month follow-up interviews, were blinded to the prior cognitive testing results obtained in the hospital. The survey lasted between 30–45 minutes.
Cognitive Function Measures
To determine global cognition, research staff used the Folstein Mini Mental Status Examination (MMSE)27 with low cognition being less than 25 for subjects with high school education and less than 18 for subjects with less than high school education. Since discharge instructions require working memory, immediate recall and delayed recall, we performed more intensive cognitive testing in these realms.
To test working memory, we used the backward digit span test where researchers give the subject two digits (i.e. “1-2”) and ask the subject to repeat them backwards (i.e. “2-1). A total of three 2-digit trials are given to the subject. Researchers increase the number of digits (i.e. “1-2-3”) until the subject makes errors on two trials of digits. Working memory low cognition was designated as fewer than three digits (i.e.1-2-3). We chose this level as it is more than two standard deviations below the age-related mean in seniors. The backward digit span has been validated in the literature.25,26
In assessing immediate and delayed recall, we used a validated 15-word list28,29. Research staff read out loud a list of 15 unrelated words to the subjects. For immediate recall, subjects are asked to repeat as many words as they remember immediately after the list is completely read. Immediate recall low cognition was designated as repeating three words or less which is more than two standard deviations below the age-related mean. For delayed recall, research staff asked subjects after 8 minutes to repeat as many words as they remembered. Delayed recall low cognition was designated as repeating one word or less which is more than two standard deviations below the age-related mean28,29.
The three-word registration/recall of the MMSE was performed prior to the initiation of the 15-word list so as to limit recall overlap. There was no overlap of actual words between the 15-word list and the MMSE. The digit backwards test is unique from the MMSE.
Data Analysis
Statistical analysis was performed with the SPSS Statistics 17.0 (SPSS Inc., Chicago, IL). We compared the results of the MMSE, Working Memory, Immediate, and Delayed Memory tests on discharge and one month post discharge from the hospital. We used paired t-tests to compare the changes in cognition on the working memory, immediate, and delayed memory tests. Wilcoxon Ranked Sum was used to analyze the nonparametric results of the MMSE. McNemar test was used to assess the significance of the difference between the MMSE Subtests among the subjects with low cognition on the two time points.
RESULTS
Sample Characteristics
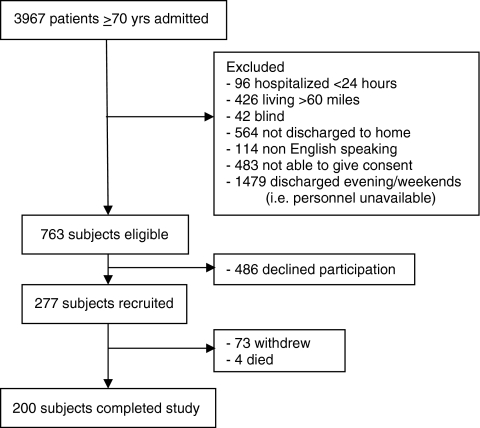
Of the 763 eligible hospitalized seniors, we recruited 277 subjects of which 73 withdrew during the month between tests and 4 died resulting in 200 participants completing both the day of discharge and one month post-discharge testing (Fig. 1) Mean age of the 200 subjects was 79.6 years (range 70–100 yrs, SD 6.4) with 58% female. Subjects identified themselves as 37.5% married, 36% widowed, and 54.0% living alone. On education, the largest group of subjects (36.0%) had some college or were college graduates while 27.5% had attended graduate school. The majority of seniors managed their own medications (84.5%) (Table 1).
Figure 1.
Recruitment.
Table 1.
Characteristics of Study Participants (N = 200)
| Mean Age | 83.0 yrs |
|---|---|
| Female | 57.0% (110) |
| Race | |
| -White | 69.4% (134) |
| -African American | 24.4% (47) |
| -Asian | 2.6% (5) |
| -Hispanic | 2.6% (5) |
| -Other | 1.0% (2) |
| Marital Status | |
| -Married | 35.8% (69) |
| -Never married | 12.4% (25) |
| -Widowed | 37.3% (72) |
| -Divorced | 13.5% (26) |
| Living Arrangement | |
| -Lives alone | 54.4% (105) |
| -Lives with dpouse only | 22.3% (43) |
| -Lives with offspring only | 12.4% (26) |
| -Lives with spouse and offspring | 5.1% (10) |
| Has domeone help with medications | 15.5% (30) |
| -Spouse | 8.0% (16) |
| -Offspring | 4.0% (8) |
| -Visiting nurse/homemaker | 2.5% (6) |
| Education | |
| -8th grade or less | 6.7% (13) |
| -Some high school | 7.8% (15) |
| -High school grad | 23.3% (45) |
| -Some college | 22.3% (43) |
| -College grad | 14.0% (27) |
| - < 4 years grad school | 19.2% (37) |
| - > 4 years grad school | 6.7% (13) |
Subject Retention
Of those subjects who did not complete the one-month follow-up but did complete the day of discharge cognitive testing (n = 126), 37.5% had low cognition on the MMSE which is slightly more than those who completed the study (31.5%). There was no significant difference in race, sex, marital status, and education compared with those who completed the study.
Cognitive Function Testing
MMSE
At hospital discharge, 31.5% (63) of subjects had low cognition on the MMSE (60 high school educated, and 3 less than high school educated). One month following discharge, only 13.5% (27) still had low cognition (p < 0.001). ). 18% of subjects had initially low cognition that improved into the normal range 1 month after discharge, and most subjects (58%) with low cognition improved into the normal range. Among subjects with low cognition (63), we saw a mean improvement of 4 points on the MMSE at one month post-discharge. Specifically, subjects with low cognition had a mean score on the MMSE of 20.56 (range 14–24) at discharge which improved to a mean of 24.57 (range 18–29) at one month post-hospitalization (p < 0.001). Among the MMSE subtests, as expected, orientation showed significant improvements between testing in the hospital and testing one month later in the home. (p < 0.001) However, we also saw significant improvements in task completion, registration, repetition, naming, reading, writing, and calculation (Table 2). Of note, only 54.0% of low cognition subjects were able to complete a three-step task correctly (folding paper, placing in left hand, and handing to interviewer) at discharge; One month later, almost all (98.4%) were able to perform the task correctly.
Table 2.
Scores of MMSE Subtests among Low Cognition Subjects
| Subtests of MMSE (number of items correct) | Day of Discharge | 1 Month Post-Discharge | Significance |
|---|---|---|---|
| Registration | |||
| 1 | 11.1% (7) | 0 | < 0.001 |
| 2 | 20.6% (13) | 3.2% (2) | |
| 3 | 68.3% (43) | 96.8% (61) | |
| Delayed Recall | |||
| 0 | 31.7% (20) | 34.9% (22) | 0.279 |
| 1 | 46.0% (29) | 28.6%(18) | |
| 2 | 15.9% (10) | 25.4% (16) | |
| 3 | 6.3% (4) | 11.1% (7) | |
| Time Orientation | |||
| 1 | 1.6% (1) | 0 | < 0.001 |
| 2 | 6.3% (4) | 1.6% (1) | |
| 3 | 17.5% (11) | 6.3%(4) | |
| 4 | 49.2% (31) | 33.3% (21) | |
| 5 | 25.4% (16) | 58.7% (37) | |
| Place Orientation | |||
| 1 | 1.6% (1) | 0 | < 0.001 |
| 3 | 9.5% (6) | 1.6% (1) | |
| 4 | 27.0% (17) | 6.3% (4) | |
| 5 | 61.9% (39) | 92.1% (58) | |
| Repetition | |||
| 0 | 58.7% (37) | 4.8% (3) | < 0.001 |
| 1 | 41.3% (26) | 95.2% (60) | |
| Comprehension (Ability to follow oral instructions—steps completed correctly) | |||
| 0 | 4.8% (3) | 0 | < 0.001 |
| 1 | 9.5% (6) | 0 | |
| 2 | 31.7% (20) | 1.6% (1) | |
| 3 | 54.0% (34) | 98.4% (63) | |
| Naming | |||
| 0 | 3.2% (2) | 0 | 0.034 |
| 1 | 4.8% (3) | 0 | |
| 2 | 92.1% (58) | 100% (63) | |
| Reading | |||
| 0 | 11.1% (7) | 1.9% (1) | 0.033 |
| 1 | 88.9% (56) | 98.1% (52) | |
| Writing | |||
| 0 | 64.2% (34) | 49.1% (26) | 0.015 |
| 1 | 35.8% (19) | 50.9% (27) | |
| Visual spatial (copy overlapping pentagons) | |||
| 0 | 64.2% (34) | 52.8% (28) | 0.058 |
| 1 | 35.8% (19) | 47.2% (25) | |
| Attention/ Calculations (number of serial subtractions completed) | |||
| 0 | 19.0% (12) | 6.3% (4) | < 0.001 |
| 1 | 11.0% (7) | 9.5% (6) | |
| 2 | 22.2% (14) | 15.9% (10) | |
| 3 | 17.5% (11) | 17.5% (11) | |
| 4 | 3.2% (2) | 7.9% (5) | |
| 5 | 27.0% (17) | 42.9% (27) | |
Working Memory
With the digit backward test, we found that working memory low cognition was present in 35.5% (71) of the subjects. This meant that these subjects were not able to perform on more than two digits (i.e. 1–2, 2–1 only). After one month, 31.5% (63) still had difficulties with working memory (p = 0.014). Working memory among those with low cognition changed marginally but not significantly in one month [from a mean of 1.94 to 2.20 digits, p= 0.15].
Immediate and Delayed Recall
On delayed recall at discharge, 50.0% (100) subjects had low cognition and were not able to remember more than one word from the 15-word list after 8 minutes. One month post-discharge, significant improvements were seen but 34.5% (69) subjects still had difficulties with delayed recall (p < 0.001). With immediate recall, we found that 29.5% (59) subjects had low cognition at hospital discharge. These subjects could only recall three words or less immediately after hearing a 15-word list. At one month post discharge, 25.5% (51) still had difficulties with immediate recall. The change in these results was not significant (p = 0.65).
DISCUSSION
At hospital discharge, almost one third of community-dwelling seniors had previously unrecognized cognitive dysfunction, and cognition significantly improved at one month post-discharge. This transient cognitive impairment poses a threat to both the comprehension and fulfillment of discharge instruction as seniors may not be able to remember their discharge plan when they return home. In our study sample, over half the seniors lived alone in the community and almost 85% managed their own medications.
Seniors with low cognitive function at discharge experienced the largest improvements. On the MMSE, a mean improvement of 4 points was seen one month post-discharge (from 20.56 to 24.57 p < 0.001). As expected, orientation improved when seniors return to their long-standing homes; however, orientation alone did not account for this 4-point increase in MMSE. Significant improvements were present in registration, repetition, comprehension, naming, reading, writing, and calculation. Most notably, seniors struggled with registration and task completion at discharge, skills that are likely important to the successful execution of discharge instructions. One month later, almost all seniors were able to perform exceedingly well on registration and task completion. If seniors are not able to perform task completion at discharge, then the timing of many transition interventions to the day of discharge may not be ideal.
Cognitive loss, hospitalization, and acute illness appear to be tightly interwoven in seniors. To begin with, acute illness frequently affects cognition. With the ensuing hospital admission, seniors cope with more cognitive challenges. Faced with a new environment and remaining bed bound for long periods of time, seniors find orientation in the hospital difficult. While hospitalized, seniors potentially receive medications that sedate or diminish memory. Further affecting memory, hospitalized seniors frequently experience a lack of sleep and reversal of day-night. Vitals are checked in the middle of the night; alarm bells beep throughout the night; hospital roommates snore; patients are called for tests at midnight. To accommodate these nighttime awakenings, naps are encouraged during the day. Subsequently, hospitals discharge patients who are weak, tired, and cognitively impaired.
Our study was limited by several aspects. The population studied was predominantly well educated with over half attending college, graduating from college, or receiving post-graduate education. Since cognition and education are closely linked, the actual frequency of low cognition at discharge may even be higher at hospitals serving patients with less education. Furthermore, half of our study population lived with a spouse or offspring. While 84.5% of our subjects stated that they managed their own medications, we did not collect data on whether their relatives assisted subjects during post-hospitalization in completing the discharge instructions. A number of subjects (n = 127) did not complete the 1 month follow-up but exhibited low cognition at discharge. Low cognition was even higher among this group when compared to those who completed the study (37.5% vs 31.5%). It is unclear if their low cognition at discharge influenced their choice to not continue with the study—either in dissatisfaction with the hospital discharge experience or fear of being institutionalized for continuing low cognition (i.e. placement in nursing home). The problem of low cognition at discharge potentially may be larger than reported.
From a methodological standpoint, limitations existed in that we used fairly basic measures of cognition. More extensive cognitive testing would have given a more thorough cognitive evaluation but made the survey longer and carry a higher burden to the recovering patient. We also did not assess for understanding of discharge instructions. Considering that discharge instructions are given both verbally and in written formats, subjects who struggle with verbal recall may be able to complete a written discharge plan. For this population, creating written discharge instructions that are written simply and targeted to the senior’s health literacy level may be critical. It is also unclear when precisely cognition improves post-hospitalization. We performed cognitive testing at two time points—day of hospital discharge and one month later. A more frequent cognitive testing strategy would have enabled us to determine if patients improved sufficiently at 3, 7, 10, 14, or 21 days. This detail would be helpful in planning discharge interventions to coincide with sufficient cognition in the patient.
From a policy perspective, rapid screening of cognition at hospital discharge may be useful to detect which seniors will require assistance with their discharge plan. Specific discharge interventions can then be targeted to either a relative/caregiver who can assist the patient at home. Caregivers can be educated that the senior’s cognition may be temporarily impaired and may need to be more attentive during the immediate post-hospitalization period. This greater reliance on caregivers in discharge and post-discharge planning may help seniors who are identified with low cognition at discharge. These seniors may also benefit from closer follow-up with their primary care physician to ensure that the discharge plan is being followed and to monitor the cognitive impairment. This tailoring of discharge interventions would decrease the costs to the hospital of initiating sweeping interventions to all discharged seniors.
Ultimately, patient self management may be better taught as an outpatient following discharge and not at the actual hospital discharge itself. Discharge interventions should incorporate screening of seniors for low cognition prior to hospital discharge to provide optimal transitional care.
Acknowledgements
Dr. Lindquist and this study were funded by a grant from the National Institute of Aging (K23AG028439-04). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. Preliminary data for this paper were presented as an abstract at the Society of General Internal Medicine 2010 National Meeting.
Conflict of Interest None disclosed.
References
- 1.Bodenheimer T, Bodenheimer T. Coordinating care–a perilous journey through the health care system. N Engl J Med. 2008;358(10):1064–1071. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 2.Coleman EA. Falling through the cracks: Challenges and Opportunities for Improving Transitional Care for Persons with Continuous Complex Care Needs. J Am Geriatr Soc. 2003;51:549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 3.Chugh A, Williams MV, Grigsby J, et al. Better transitions: improving comprehension of discharge instructions. Front Health Serv Manage. 2009;25(3):11–32. [PubMed] [Google Scholar]
- 4.Jencks SF, Williams MV, Coleman EA, Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 5.Marcantonio ER, McKean S, Goldfinger M, Kleefield S, Yurkofsky M, Brennan TA. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. Am J Med. 1999;107(1):13–17. doi: 10.1016/S0002-9343(99)00159-X. [DOI] [PubMed] [Google Scholar]
- 6.Gillick MR, Serrell NA, Gillick LS. Adverse consequences of hospitalization in the elderly. Soc Sci Med. 1982;16:1033–1038. doi: 10.1016/0277-9536(82)90175-7. [DOI] [PubMed] [Google Scholar]
- 7.Naylor MD. Transitional care of older adults. Annu Rev Nurs Res. 2003;20:127–147. [PubMed] [Google Scholar]
- 8.Coleman EA, Smith JD, Raha D, Min SJ. Posthospital Medication Discrepancies. Arch Intern Med. 2005;165:1842–1847. doi: 10.1001/archinte.165.16.1842. [DOI] [PubMed] [Google Scholar]
- 9.Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219–223. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 10.Gray SL, Mahoney JE, Blough DK. Adverse drug events in elderly patients receiving home health services following hospital discharge. Ann Pharmacother. 1999;33:1147–1153. doi: 10.1345/aph.19036. [DOI] [PubMed] [Google Scholar]
- 11.Chawla S, Pastores SM, Hassan K, et al. ICU admissions after actual or planned hospital discharge: incidence, clinical characteristics, and outcomes in patients with cancer. Chest. 2009;136(5):1257–1262. doi: 10.1378/chest.08-2909. [DOI] [PubMed] [Google Scholar]
- 12.Clemens EL. Multiple perceptions of discharge planning in one urban hospital. Health Soc Work. 1995;20(4):254–261. doi: 10.1093/hsw/20.4.254. [DOI] [PubMed] [Google Scholar]
- 13.Williams MV, Coleman E, Williams MV, Coleman E. BOOSTing the hospital discharge. J Hosp Med (Online) 2009;4(4):209–210. doi: 10.1002/jhm.525. [DOI] [PubMed] [Google Scholar]
- 14.Coleman EA, Smith JD, Frank JC, Min A, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: The care transitions interventions. J Am Geriatr Soc. 2004;52:1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 15.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jha AK, Orav EJ, Epstein AM, Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361(27):2637–2645. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]
- 17.Calkins DR. Davis, R.B., Reiley, P., et al. Patient-Physician Communication at Hospital Discharge and Patients' Understanding of the Postdischarge Treatment Plan. Arch Intern Med. 1997;157:1026–1030. doi: 10.1001/archinte.157.9.1026. [DOI] [PubMed] [Google Scholar]
- 18.Maniaci MJ, Heckman MG, Dawson NL, Maniaci MJ, Heckman MG, Dawson NL. Functional health literacy and understanding of medications at discharge. Mayo Clin Proc. 2008;83(5):554–558. doi: 10.4065/83.5.554. [DOI] [PubMed] [Google Scholar]
- 19.Beers MH, Dang J, Hasegawa J, Tamai IY. Influence of Hospitalization on Drug Therapy in the Elderly. J Am Geriatr Soc. 1989;37:679–683. doi: 10.1111/j.1532-5415.1989.tb02227.x. [DOI] [PubMed] [Google Scholar]
- 20.Forster AJ. Murff, H.J., Peterson, J.F., Gandhi, T.K., Bates, D.W. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 21.Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ Can Med Assoc J. 2004;170(3):345–349. [PMC free article] [PubMed] [Google Scholar]
- 22.Graf C, Graf C. Functional decline in hospitalized older adults. Am J Nurs. 2006;106(1):58–67. doi: 10.1097/00000446-200601000-00032. [DOI] [PubMed] [Google Scholar]
- 23.Hickey A, Clinch D, Groarke EP. Prevalence of cognitive impairment in the hospitalized elderly. Int J Geriatr Psychiatry. 1997;12:27–33. doi: 10.1002/(SICI)1099-1166(199701)12:1<27::AID-GPS446>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 24.Fields SD, MacKenzie CR, Charlson ME, Perry SW. Reversibility of cognitive impairment in medical inpatients. Arch Intern Med. 1986(146):1593–1596. [PubMed]
- 25.Inouye SK, Zhang Y, Han L, Leo-Summers L, Jones R, Marcantonio E. Recoverable cognitive dysfunction at hospital admission in older persons during acute illness. J Gen Intern Med. 2006;21(12):1276–1281. doi: 10.1111/j.1525-1497.2006.00613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Inouye S, Dyck C, Alessi C, Balkin S, Siegal A, Horwitz R. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 27.Folstein MF, Folstein SE, McHugh PR. Mini Mental State: A practical method for grading the cognitive state of patient for the clinician. J Psychiatr Res. 1975;12:196–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 28.Tun PA Lachman ME. Brief Test of Adult Cognition by Telephone (BTACT) Technical Report. Accessed on February 14,2011. Available at http://www.brandeis.edu/departments/psych/lachman/pdfs/techreport.pdf.
- 29.Tun PA Lachman ME. Guidelines on Administration and Scoring of the Brief Test of Adult Cognition by Telephone (BTACT). Accessed on February 14, 2011. Available on http://www.brandeis.edu/departments/psych/lachman/pdfs/btact-admin-scoring.pdf