Abstract
Average risk of acquiring HIV infection after a percutaneous exposure to HIV infected blood is 0.3%. Post exposure prophylaxis (PEP) for HIV refers to a set of comprehensive services to prevent HIV infection in exposed individuals where the exposure can be occupational/ non occupational and a provision of short term (28 days) antiretroviral drugs are given depending on the risk assessment. It also includes counselling and relevant laboratory investigations after taking informed consent of the exposed person and source. PEP inhibits the replication of the initial inoculum of virus and thereby prevents establishment of chronic HIV infection, and is best effective when initiated within 2 hours but certainly within 72 hours. Present communication deals with the registry of 278 cases of PEP from Gujarat in terms of various determinants, their status and the outcome in terms of HIV sero positivity.
Keywords: Antiretroviral drugs, health care personals, HIV, post exposure prophylaxis
INTRODUCTION
Post exposure prophylaxis (PEP) is a medical response to prevent transmission of pathogens after potential exposure and refers to comprehensive management instituted to minimize the risk of infection following potential exposure to blood-borne pathogens (HIV, HBV, HCV). It includes first aid, counselling, risk assessment, relevant laboratory investigations based on the informed consent of the exposed person and source and depending on the risk assessment, the provision of short term (28 days) of antiretroviral drugs, along with follow-up evaluation.[1,2]
Healthcare personals (HCP) are defined as person paid/ unpaid working in healthcare settings and are potentially exposed to infectious materials such as blood, tissue, specific body fluids, medical supplies/ equipment or environmental surfaces contaminated with these substances are constantly exposed to occupational hazards through exposure of per-cutaneous injury (Needle stick or cut with sharps, contact with the mucus membrane of eyes or mouth of an infected person, contact with non-intact skin (particularly when exposed skin is chapped, abraded, or afflicted with dermatitis or contact with blood or other potentially infectious body fluids).[2,3]
One of the most common yet dreaded hazards in healthcare facilities is the needle stick injury. Globally, 1 million healthcare workers annually suffer from needle stick injuries. Of these, 100 are infected with diseases such as hepatitis B, hepatitis C, and HIV. Centre for Disease Control (CDC) and National AIDS Control Organization (NACO) recommend PEP for workers with needle stick injuries.[4,5] PEP for HIV exposure is best when started within golden period of <2 hours and there is little benefit after 72 hours. The prophylaxis needs to be continued for 28 days. PEP is available as either basic regimen (2 Nucleoside Reverse Transcriptase Inhibitor (NRTI)) or expanded regimen (2NRTI and 1 PI drugs). NACO recommend Zidovudine/ Stavudine + Lamivudine (basic regimen) and Zidovudine + Lamivudine + Lopinavir/ Ritonavir (expanded regimen), and make efforts to ensure its free of cost availability at all Anti Reteroviral Therapy Centers (ARTCs) and Integrated Counseling & Testing Centers (ICTCs). Availability of limited literatures in Indian context about PEP usage and outcome in HIV care settings necessitated the present study.[6–8]
MATERIALS AND METHODS
PEP record registry as per the NACO guidelines is maintained at all ARTCs, which is coordinated by Gujarat State AIDS Control Society in the prescribed format. Present study includes data from 14 ARTCs. Out of these, data on PEP was available from 11 centres – Civil Hospital, Ahmadabad 91 (32.7%), followed by Sir T hospital, Bhavnagar 60 (21.6%), PDU Medical College, Rajkot 31 (11.2%), SSG Hospital, Vadodara 28 (10.1%), New Civil Hospital Surat 27 (9.71%), GG Hospital, Jamnagar 14 (5.03%), SMIMER, Surat 7 (2.52%), MG Hospital, Surendranagar 6 (2.16%), VS Hospital and Civil Hospital, Junagadh each accounting for 5 (1.8%) and District Hospital, Mahesana 4 (1.44%). Till date, no HCP has approached ARTC at Palanpur, Himmatnagar, and Reliance Surat for PEP.
Study design and period
It is a prospective study carried over a period from October 2008 to August 2010.
Inclusion criteria
Any HCP in government/ private sector in occupational settings having directly/ indirectly exposed to needle stick injuries of a known/ unknown source comprised the study material.
RESULTS
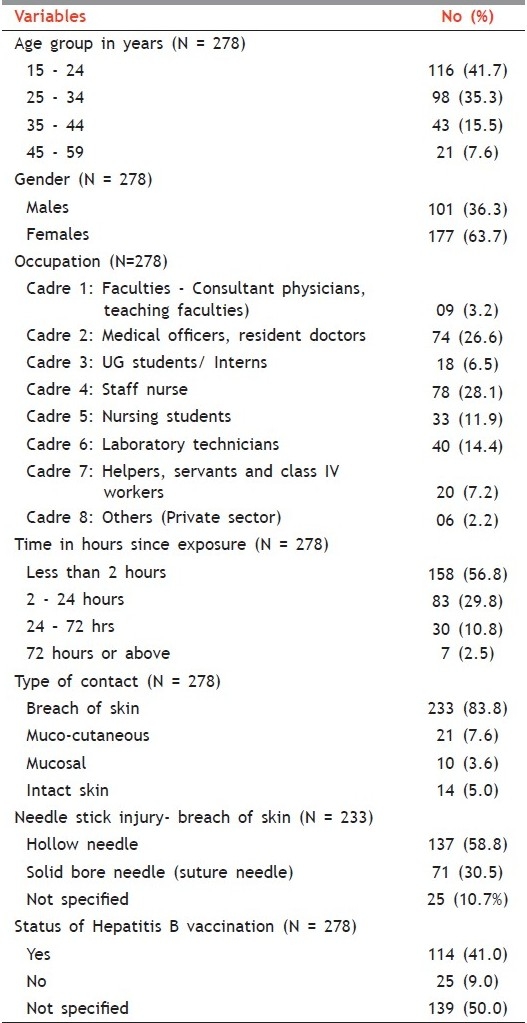
A total of 278 cases in HCP at various cities in Gujarat were analyzed and out of them, 101 (36.3%) were males and 177 (63.7%) females with male to female ratio of 0.57:1. Majority (54.68%) of exposed HCP comprised of staff nurse and resident doctors/ medical officers followed by laboratory technicians and nursing students (26.26%). Majority of exposed HCPs (56.8%) came within 2 hours followed by 29.8% between 2 and 24 hours. Needle stick injury was the commonest injury accounting for 75.9% of cases, with majority of them exposed to hollow bore needle (64.93%) [Table 1].
Table 1.
Demographic profile of healthcare personals
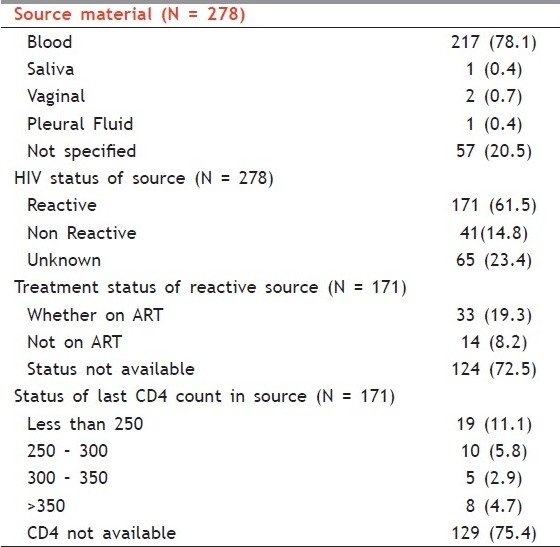
Correct information regarding the type of contact was elicited in 221 (79.5%) cases. Of these, 217 (98.2%) had contact with blood, (including 1 having contact with blood and vaginal secretions), followed by 2 cases (0.9%) of contact with vaginal secretion, and 1 (0.5%) each of contact with saliva and pleural fluid [Table 2]. Exposure wise majority of them had mild exposure (65.1%), followed by moderate (25.9%) and severe (9.0%) cases. Regarding first aid steps taken after exposure, most common response was wash the affected site with either water or soap and water (66.9 %) followed by application of sprit/ alcohol/ antiseptics (14.7%) and “tried to squeeze the affected site” (7.9%).
Table 2.
Status of source
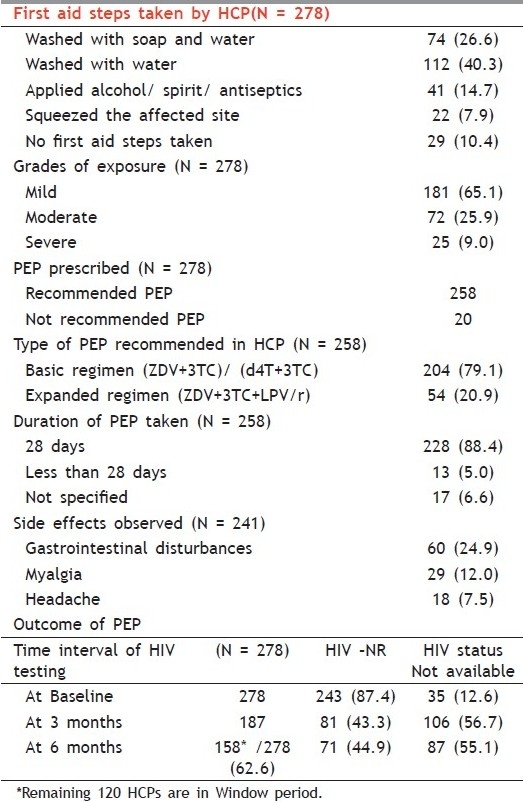
Baseline HIV status: Out of 278 HCP, baseline HIV test was done in 243 (87.4%), and all were HIV Non reactive (NR). Remaining 35 did not turn up for HIV testing. As per NACO guidelines, HIV testing is also done at 3 months, but in the study only 81 (43.3%) out of 187 due for 3 months testing turned out and all were non reactive. Confirmatory HIV test at 6 months could be done in 71 (44.9%) out of 158 cases due for 6 monthly testing. Rest 87 (55.06%) cases did not turn up for follow-up at 6 months. All 71 cases were non reactive. Another 120 cases are in the window period. Till date, no case of HIV reactivity has been observed in this study [Table 3].
Table 3.
Steps taken and outcome in the exposed healthcare personals
DISCUSSION
Per cutaneous inoculation (by needle or other instrument that pierces the skin) carries a low risk of HIV transmission of around 0.3% (95% CI 0.2 to 0.5);[9] our study also did not report any HIV case.
Majority of people (63.7%) in this study who suffered occupational injuries were females. Male: female ratio whether in PLHIV or patients on ART show a male dominance, whereby the male female ratio is around 2:1. This study shows a female vulnerability in healthcare settings, which needs to be targeted through training of HCP with special emphasis on female employee (staff nurses, technicians, and helpers). Proportions of staff nurses (28.1%), medical officers (26.6%), and laboratory technicians (14.4%) in our study were high when compared with 19%, 18%, and 10%, respectively, by Baheti et al. They all being highly vulnerable for increased risk for acquiring blood borne HIV exposures in care settings in India.[8,10]
PEP is the cost-effective measurements in low and middle income countries in HIV care settings for HCP getting exposed to infectious materials.[10] While 120 out of 278 are still in the window period; rest who could be tested were found non reactive. This may be due to the timely institution of effective PEP. It may not be true in all cases as 25 HCP had severe exposure and for another 30 we are unsure whether they took it for required 28 days or not. The fact that majority of them (55–57%) do not come for repeat testing is a worrying aspect. Staff still have the fear of stigmatization and afraid to know their HIV status, more so at the facility where they are working. All healthcare units should ensure to have adequate staff counselling and education about risk of infection after occupational exposure. Policies and procedures should be in place and the staff should be aware about the actions to be taken in the event of occupational exposure.
However, one encouraging fact was that most of the HCP (85%) exposed to occupational exposure had their baseline HIV test done, all being HIV non reactive. It is important that once PEP started, it should be taken for full duration of 28 days. More than 94% respondents who were prescribed the PEP took it for full 28 days. Rest discontinued it for the side effects to PEP regimen. Adverse effects due to PEP should be treated with core concern to continue PEP. Detailed counselling is required in such cases for better mental preparation for post PEP outcome as well.
HCPs should be educated to report occupational exposures immediately after the occurrence, particularly because hepatitis B vaccine and HIV - PEP is most effective if administered soon after the exposure. Exposed HCP of all cadres must be aware of the standard instructions for access to urgent advice of occupational exposure and the fact that HIV testing should be done at the baseline level and after the completion of the PEP at interval of 3 and 6 months to confirm the HIV status of exposed HCP.[2]
Equally important for the HCP is to know how to minimize the injuries and about the round the clock availability of PEP, expected adverse events, and the strategies for managing them. It must be noted that PEP is not cent percent effective in preventing HIV seroconversion,[11] Therefore, PEP cannot be considered to replace the universal precautions and avoiding occupational injuries. Persons who take PEP and are under follow up for 6 months should abstain from any high risk behaviour activity and not donate blood.[12] Although preventing blood exposures is the primary means of preventing occupationally acquired blood borne diseases, appropriate post-exposure management is an important element of workplace safety. The study highlights the need of standardized protocols for management of exposure to blood borne pathogens. It also reflects the need for safe working environment in all hospitals. There is a need to report, investigate and follow-up needle stick injuries. Drugs for PEP for HIV should be available 24 hours readily in hospitals for immediate use by HCPs.
This study indicates the need to reinforce knowledge regarding various aspects of occupational PEP to health care personals especially those associated with nursing (staff nurse, nursing students), Resident doctors and Laboratory technicians. Another study from Ahmadabad[13] has shown that by regular sensitization and universal precaution workshops increase the awareness among HCPs for reducing HIV infection risk and transmission and prevention through PEP.
Success of entire program depends up on (1) making PEP drugs available everywhere, (2) making the staff informed about avoiding injuries, following universal precautions and preparing them to take PEP as and when indicated with its all associated procedures.
Acknowledgments
We acknowledge our sincere thanks to all the ART centres of Gujarat State for their kind cooperation and providing valuable data.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Sharma A, Marfatiya YA, Ghiya R. Post-exposure prophylaxis for HIV. Indian J Sex Trans Dis and AIDS. 2007;28:2. [Google Scholar]
- 2.Management of Occupational exposure including Post exposure prophylaxis for HIV. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India; 2009. National AIDS Control Organization. [Google Scholar]
- 3.Antiretroviral Therapy Guidelines for HIV-infected Adults and Adolescents including Post-exposure Prophylaxisnone. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India; 2008. National AIDS Control Organization. [Google Scholar]
- 4.Kapila K, Gupta RM, Chopra GS. Post-exposure Prophylaxis: What Every Health Care Worker Should Know. Med JArmed Forces India. 2008;64:3. doi: 10.1016/S0377-1237(08)80106-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC. Updated US Public Health Service guidelines for the management of occupational exposures to HIV and recommendations for post-exposure prophylaxis. MMWR Morb Mortal Wkly Rep. 2005;54:1–24. [PubMed] [Google Scholar]
- 6.Wig N. HIV: Awareness of management of occupational exposure in health care workers. Indian J Med Sci. 2003;57:192–8. [PubMed] [Google Scholar]
- 7.Scoular A, Watt AD, Watson M, Kelly B. Knowledge and attitudes of hospital staff to occupational exposure to blood borne viruses. Commun Dis Public Health. 2000;3:247–9. [PubMed] [Google Scholar]
- 8.Baheti AD, Tullu MS, Lahiri KR. Awareness of Health Care Workers Regarding Prophylaxis for Prevention of Transmission of Blood-Borne Viral Infections in Occupational Exposures. Al Ameen J Med Sci. 2010;3:79–83. [Google Scholar]
- 9.Cardo DM, Culver DH, Ciesielski CA, Srivastava PU, Marcus R, Abiteboul D, et al. A case - control study of HIV seroconversion in health care workers after percutaneous exposure. N Engl J Med. 1997;337:1485–90. doi: 10.1056/NEJM199711203372101. [DOI] [PubMed] [Google Scholar]
- 10.Gupta A, Anand S, Sastry J, Krisagar A, Basavaraj A, Bhat SM, et al. High risk for occupational exposure to HIV and utilization of post-exposure prophylaxis in a teaching hospital in Pune, India. BMC Infect Dis. 2008;21:142. doi: 10.1186/1471-2334-8-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young TN, Arens FJ, Kennedy GE, Laurie JW, Rutherford G. Antiretroviral post-exposure prophylaxis (PEP) for occupational HIV exposure. Cochrane Database Syst Rev. 2007;24:CD002835. doi: 10.1002/14651858.CD002835.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merchant RC, Keshavarz R. Human immunodeficiency virus postexposure prophylaxis for adolescents and children. Paediatrics. 2001;108:38. doi: 10.1542/peds.108.2.e38. [DOI] [PubMed] [Google Scholar]
- 13.Shah A, Kavina B, Prajapati S, Purohit H, Shevkani M, Derasari U, et al. Service Outcome of Antiretroviral Post-Exposure Prophylaxis (PEP) For Occupational HIV Exposure among Health Care Personnel. Retrovirology. 2010;7:75. [Google Scholar]


