Abstract
Background/Aims
Endoscopic extraction of bile duct stones is difficult and often complicated in patients with a Billroth II gastrectomy. We evaluated a simpler technique to achieve an adequate ampullary opening for the removal of choledocholithiasis using endoscopic papillary large balloon dilation (EPLBD) combined with a guidewire-assisted needle-knife papillotomy.
Methods
Sixteen patients who had a Billroth II gastrectomy were included in this study. Following placement of the guidewire in the bile duct, a precut incision was made over the guidewire with a needle knife sphincterotome inserted alongside the guidewire. Balloon dilation of the ampullary orifice was gradually performed.
Results
Needle knife papillotomy over the guidewire with subsequent EPLBD was successful in all patients. Complete stone removal was achieved in 15 (93.7%) patients in 1 session. However, 1 (6.3%) patient required mechanical lithotripsy with an additional procedure for complete ductal clearance, and there was 1 case of minor bleeding following the EPLBD. There were no cases of pancreatitis or perforation.
Conclusions
EPLBD followed by guidewire-assisted needle-knife papillotomy appears to be a useful method with few technical difficulties and a low risk of complications for the removal of bile duct stones in patients with prior Billroth II gastrectomy.
Keywords: Precut, Large balloon dilation, Billroth II gastrectomy
INTRODUCTION
Endoscopic stone removal is an established method of treatment for bile duct stones. However, it is often complicated in patients who have undergone Billroth II gastrectomy because the inverted direction of the ampulla of Vater in the endoscopic view makes selective cannulation of the bile duct more difficult. Furthermore, differently designed sphincterotomy knives or special techniques are required to enable an endoscopic sphincterotomy (EST) in the up-down (6 o'clock) direction.1-10 Currently, the most widely used technique is the needle knife papillotomy over an antecedently-inserted plastic stent into the bile duct.10 Compared to standard EST in patients with normal anatomy, all available techniques require more time-consuming and dangerous procedures, and are associated with a higher rate of procedure-related complications.11 Even with these methods, it is difficult to make an adequate sphincterotomy incision and to achieve ampullary widening sufficient to remove the bile duct stones.12
Recently, endoscopic papillary large balloon dilation (EPLBD) combined with limited EST (EPLBD+EST) has been reported to be effective and safe for the removal of common bile duct (CBD) stones.5,13 Although this method has had promising results, EST is still a problematic procedure in patients with prior Billroth II gastrectomy. We described a simpler technique to achieve adequate ampullary opening by using EPLBD combined with guidewire-assisted needle knife papillotomy, which was a modification of biliary endoprosthesis-guided needle knife papillotomy, in patients with Billroth II gastrojejunostomy.
MATERIALS AND METHODS
From April 2006 to September 2009, therapeutic ERCP was performed in 37 patients with common duct stones who had previously undergone Billroth II gastrectomy. Of the total 37 patients, 2 patients who failed to reach ampulla or to make selective cannulation of bile duct, 1 patient who had the size of stone less than 10 mm and 18 patients who underwent endoscopic biliary drainage procedure to control acute cholangitis were excluded. Sixteen patients with successful selective biliary cannulation who did not perform biliary endoprosthesis were included in this study. The indication of EPLBD combined with guidewire-assisted precut papillotomy for the treatment of choledocholithiasis in patients with Billroth II gastrectomy is the patients who size of CBD was more than 10 mm.
The mean age of the 16 patients was 69.7±7.9 (range, 55 to 83) years and the male to female ratio was 10:6. In cases of thrombocytopenia (<50,000/µL) or prolongation of the prothrombin time (>3 seconds), ERCP was postponed until the coagulation parameters were normalized. If the patients were taking anticoagulant or antiplatelet agents, all medicines were discontinued at least 5 days before ERCP. The study protocol was approved by the Institutional Review Board at our center.
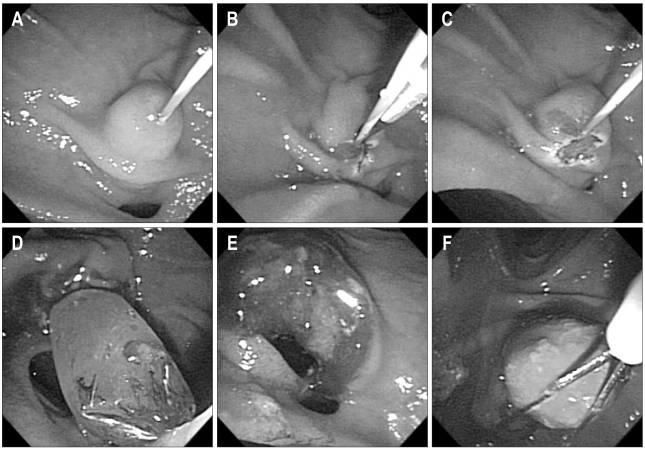
The procedure was performed with an Olympus side-viewing endoscope (TJF-160; Olympus Co., Tokyo, Japan) under conscious sedation with a combination of midazolam and meperidine. A new catheter with a straight tip was used for diagnostic ERCP to facilitate cannulation of the CBD. When selective biliary cannulation was successful, a 0.035 inch guidewire was inserted into either one of the main intrahepatic ducts through the diagnostic catheter. Once the guidewire was placed in the hepatic duct, the guidewire was left in the proximal biliary tree as the diagnostic catheter was removed (Fig. 1). Subsequently, we inserted a needle knife sphincterotome (TW 1/23; Medizin-Technische-Werkstte, Endoskopie, Wesel, Germany) alongside the guidewire and a precut incision was made over the guidewire. The precutting was usually made from papillary orifice to the point between the proximal hooding fold and major horizontal fold. Once the precut papillotomy was done, the guidewire kept left in the proximal biliary tree and the dilating balloon (CRE balloon; Boston Scientific Microvasive, Cork, Ireland) was advanced over the guidewire and was positioned in the middle of the balloon across the ampullary orifice. Under endoscopic and fluoroscopic guidances, the balloon was then inflated gradually with diluted contrast media until the waist on the balloon disappeared. We chose balloons between 12 mm and 18 mm in diameter, according to the size of the stone, but not exceeding 2 mm over the diameter of the distal CBD for safety. We maintained the ballooning for 10 to 60 seconds after notching of the balloon disappeared. Either stone retrieval baskets or balloon-tipped catheters were used to extract CBD stones after EPLBD, and mechanical lithotripsy was attempted to fragment the stone if the stone was too big to remove at once. A biliary drainage procedure was done to prevent cholangitis when incomplete stone removal was suspected at the end of the procedure.
Fig. 1.
With precutting made along the prepositioned guidewire (A, B), a small incision of the papilla is made (C). Adequate ampulla widening is achieved with subsequent endoscopic papillary large balloon dilation (D, E). The common bile duct stone is removed with a stone retrieval basket (F).
To assess the efficacy and safety of this technique, the number and size of CBD stones, the number of ERCP sessions for complete stone removal, and complications after ERCP were evaluated. When there were no stones on cholangiogram after stone extraction, we defined that the stone was removed completely. Technical success was defined that successful stone removal was accomplished after selective biliary cannulation. Post-ERCP pancreatitis was defined by the development of abdominal pain with serum amylase levels higher than three times of the upper normal limit and post-ERCP hyperamylasemia by the elevation of serum amylase without abdominal pain. Post-ERCP bleeding was defined as significant hemorrhage requiring endoscopic hemostasis. Minor bleeding was defined as endoscopic bleeding that stopped spontaneously.
RESULTS
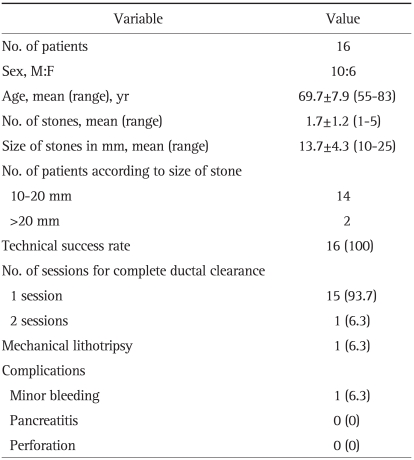
Needle knife precutting over a guidewire and subsequent EPLBD were successful in all patients, although there were some technical difficulties to control the needle knife papillotome precisely because the guidewire itself hindered the movement of the needle knife papillotome. The mean size of the stones was 13.7±4.3 (range, 10 to 25) mm. The mean number of stones was 1.7±1.2 (range, 1 to 5) (Table 1). The size of the balloon used for EPLBD was 12 mm in 7 patients, 15 mm in 3 patients, and 18 mm in 6 patients. The balloon inflation time was 33.7±17.4 (range, 10 to 60) seconds. Complete stone removal was achieved in 15 (93.7%) patients with 1 session. Only 1 (6.3%) patient required mechanical lithotripsy and an additional procedure for complete ductal clearance. One of the 16 patients had minor bleeding after the ERCP. Perforation or cholangitis associated with EPLBD was not observed. Hyperamylasemia was observed in 4 patients, none of whom developed acute pancreatitis.
Table 1.
Results of EPLBD Combined with Guidewire-Assisted Precut Papillotomy in Patients with Billroth II Gastrectomies
Data are presented as mean±SD (range) or number (%).
DISCUSSION
Ampullary widening is an essential part of the endoscopic removal of bile duct stones and most commonly performed by EST, and in part by endoscopic balloon dilatation (EBD). In patients with prior Billroth II gastrectomy, however, EST is often a complicating procedure and various techniques and specially designed instruments have been developed to facilitate EST. The opposite direction of the sphincteromy incision and angulations of the distal CBD makes the procedure more challenging and necessitates higher endoscopic skills and experiences.14 An adequate EST incision to allow stone removal requires a more demanding procedure and accompanies a higher risk of acute complications, such as bleeding, perforation, or pancreatitis, regardless of all available methods.
Although EBD, an alternative to EST, was reported to be effective and relatively easy to perform.12 EBD was not usually recommended for the treatment of choledocholithiasis because there was a potential risk of life threatening pancreatitis which was presumably related with the obstruction of the pancreatic orifice or direct pancreatic damage due to balloon compression.15 In addition, ampullary opening made by EBD was usually too small to remove larger stones, so mechanical lithotripsy was required more frequently.12,14
Recently, EPLBD+EST has shown encouraging therapeutic outcomes and safety with a lower risk of complications.5,13,14,16-18 The risk of pancreatitis related to EPLBD may be prevented because the obstruction of the pancreatic orifice is alleviated by antecedent EST. In previous studies concerning EPLBD+EST, the risk of pancreatitis, bleeding, and perforation were nearly absent. Our study again demonstrated that this technique is an effective method to remove bile duct stones and can be performed safely without serious complications.
EPLBD+EST is relatively easy to perform compared to full length EST in patients with normal anatomy. However, this procedure is still complicated in patients with Billroth II anastomosis because antecedent EST is required and difficult to perform. We noticed that only a small incision is sufficient for performing EPLBD+EST and found possibilities that this small incision can be done with a needle knife over a guidewire instead of a biliary endoprosthesis. In practice, we experienced some difficulties in controlling a needle knife papillotome over the guidewire and it was dangerous to perform full incision because the guidewire itself interfered with the movement of the needle knife. However there were no problems to make small incisions necessary for EPLBD+EST and the procedure time was similar to endoprosthesis guided precutting.
The most important and difficult step in our technique is selective cannulation of the bile duct. To facilitate biliary cannulation in Billroth II gastrectomy, we used a new catheter with a straighter end and in some cases used guidewire technique. Other problems with this method included difficulties in handling the needle knife because meticulous control of the needle knife was not possible due to interference of the guidewire. Thus, a full incision of the papilla with this method should be avoided because it is technically difficult and dangerous.
In conclusion, needle knife papillotomy over a guidewire in patients with Billroth II gastrectomy seems to be a useful alternative to biliary endoprosthesis-guided EST for performing a minimal incision of the papilla. When this technique is combined with EPLBD, adequate ampullary widening to remove bile duct stones can be obtained with little technical difficulties and a low risk of complications.
References
- 1.Al-Kawas FH, Geller AJ. A new approach to sphincterotomy in patients with Billroth II gastrectomy. Gastrointest Endosc. 1996;43:253–255. doi: 10.1016/s0016-5107(96)70328-0. [DOI] [PubMed] [Google Scholar]
- 2.Hintze RE, Veltzke W, Adler A, Abou-Rebyeh H. Endoscopic sphincterotomy using an S-shaped sphincterotome in patients with a Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:74–78. doi: 10.1055/s-2007-1004078. [DOI] [PubMed] [Google Scholar]
- 3.Itoi T, Shinohara Y, Takeda K, et al. A novel technique for endoscopic sphincterotomy when using a percutaneous transhepatic cholangioscope in patients with an endoscopically inaccessible papilla. Gastrointest Endosc. 2004;59:708–711. doi: 10.1016/s0016-5107(04)00170-1. [DOI] [PubMed] [Google Scholar]
- 4.Kim MH, Lee SK, Lee MH, et al. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29:82–85. doi: 10.1055/s-2007-1004080. [DOI] [PubMed] [Google Scholar]
- 5.Kim GH, Kang DH, Song GA, et al. Endoscopic removal of bileduct stones by using a rotatable papillotome and a large-balloon dilator in patients with a Billroth II gastrectomy (with video) Gastrointest Endosc. 2008;67:1134–1138. doi: 10.1016/j.gie.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 6.Koo HC, Moon JH, Choi HJ, et al. The utility of a multibending endoscope for selective cannulation during ERCP in patients with a Billroth II gastrectomy (with video) Gastrointest Endosc. 2009;69:931–934. doi: 10.1016/j.gie.2008.10.053. [DOI] [PubMed] [Google Scholar]
- 7.Lee YT. Cap-assisted endoscopic retrograde cholangiopancreatography in a patient with a Billroth II gastrectomy. Endoscopy. 2004;36:666. doi: 10.1055/s-2004-814558. [DOI] [PubMed] [Google Scholar]
- 8.Nakahara K, Horaguchi J, Fujita N, et al. Therapeutic endoscopic retrograde cholangiopancreatography using an anterior oblique-viewing endoscope for bile duct stones in patients with prior Billroth II gastrectomy. J Gastroenterol. 2009;44:212–217. doi: 10.1007/s00535-008-2299-x. [DOI] [PubMed] [Google Scholar]
- 9.Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS. Cap-assisted ERCP in patients with a Billroth II gastrectomy. Gastrointest Endosc. 2007;66:612–615. doi: 10.1016/j.gie.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 10.van Buuren HR, Boender J, Nix GA, van Blankenstein M. Needle-knife sphincterotomy guided by a biliary endoprosthesis in Billroth II gastrectomy patients. Endoscopy. 1995;27:229–232. doi: 10.1055/s-2007-1005676. [DOI] [PubMed] [Google Scholar]
- 11.Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007;22:1210–1213. doi: 10.1111/j.1440-1746.2006.04765.x. [DOI] [PubMed] [Google Scholar]
- 12.Bergman JJ, van Berkel AM, Bruno MJ, et al. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19–26. doi: 10.1067/mge.2001.110454. [DOI] [PubMed] [Google Scholar]
- 13.Espinel J, Pinedo E. Large balloon dilation for removal of bile duct stones. Rev Esp Enferm Dig. 2008;100:632–636. doi: 10.4321/s1130-01082008001000006. [DOI] [PubMed] [Google Scholar]
- 14.McHenry L, Lehman G. Difficult bile duct stones. Curr Treat Options Gastroenterol. 2006;9:123–132. doi: 10.1007/s11938-006-0031-6. [DOI] [PubMed] [Google Scholar]
- 15.Disario JA, Freeman ML, Bjorkman DJ, et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291–1299. doi: 10.1053/j.gastro.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 16.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 17.Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39:958–961. doi: 10.1055/s-2007-966784. [DOI] [PubMed] [Google Scholar]
- 18.Misra SP, Dwivedi M. Large-diameter balloon dilation after endoscopic sphincterotomy for removal of difficult bile duct stones. Endoscopy. 2008;40:209–213. doi: 10.1055/s-2007-967040. [DOI] [PubMed] [Google Scholar]