Abstract
Purpose
Exercise is associated with a decrease in bone mineral density under certain conditions. One potential mechanism is increased bone resorption due to an exercise-induced increase in parathyroid hormone (PTH), possibly triggered by dermal calcium loss. The purpose of this investigation was to determine whether calcium supplementation either before or during exercise attenuates exercise-induced increases in PTH and C-terminal telopeptide of type I collagen (CTX; a marker of bone resorption).
Methods
Male endurance athletes (n=20) completed three 35-km cycling time trials under differing calcium supplementation conditions: 1) 1000 mg calcium 20 minutes before exercise and placebo during, 2) placebo before and 250 mg calcium every 15 minutes during exercise (1000 mg total), or 3) placebo before and during exercise. Calcium was delivered in a 1000 mg/L solution. Supplementation was double-blinded and trials were performed in random order. PTH, CTX, bone-specific alkaline phosphatase (BAP; a marker of bone formation), and ionized calcium (iCa) were measured before and immediately after exercise.
Results
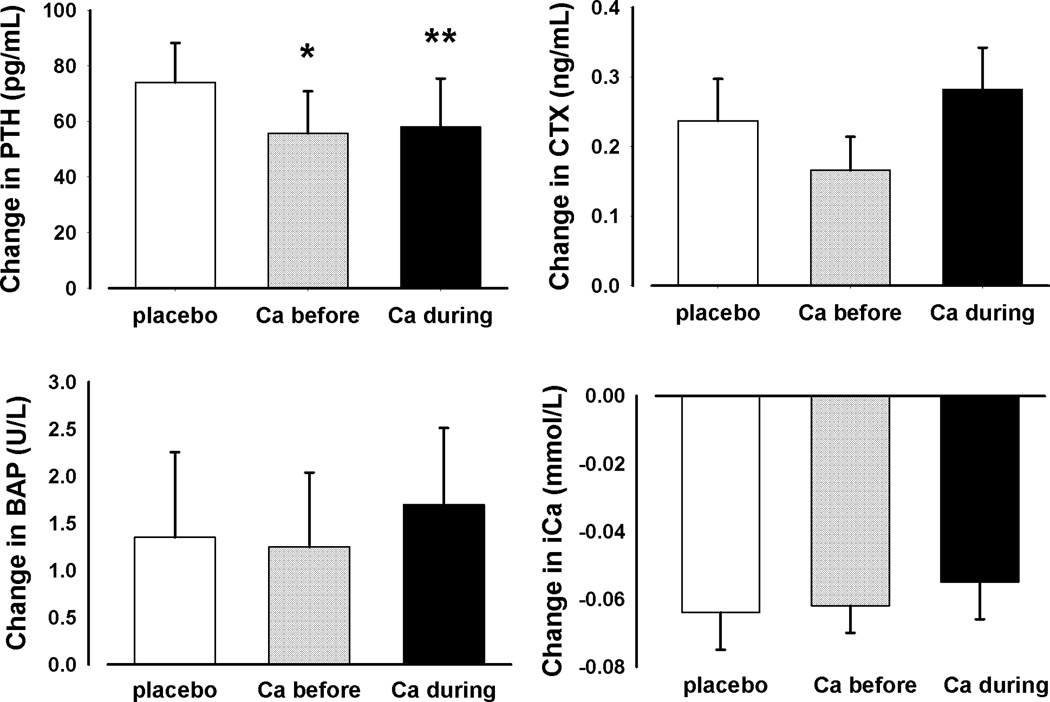
CTX increased and iCa decreased similarly in response to exercise under all test conditions. When compared to placebo, calcium supplementation before exercise attenuated the increase in PTH (55.8 ± 15.0 vs. 74.0 ± 14.2; mean ± SE; p=0.04); there was a similar trend (58.0 ± 17.4; p=0.07) for calcium supplementation during exercise. There were no effects of calcium on changes in CTX, BAP, and iCa.
Conclusions
Calcium supplementation before exercise attenuated the disruption of PTH. Further research is needed to determine the effects of repeated increases in PTH and CTX on bone (i.e., exercise training), and whether calcium supplementation can diminish any exercise-induced demineralization.
Keywords: Exercise, Parathyroid hormone, Bone Markers, Cycling
Exercise is recommended for both the prevention and treatment of low bone mineral density (BMD). Although cross-sectional studies typically show that athletes have higher BMD values than nonathletes (18), competitive cyclists have been found in some studies to have lower BMD levels than other athletes, such as runners (15). It has been thought that the relatively low BMD in cyclists reflects their participation in a weight-supported, rather than a weight-bearing, activity. However, it seems unlikely that this would explain why BMD levels of cyclists are lower than in sedentary individuals (11). BMD was recently shown to decrease in male cyclists over a one-year period of training and competition (2). In that study, total hip BMD decreased by 1.5% over one year, a rate comparable to the accelerated bone loss seen during early menopause. This suggests that, under certain condition, exercise can have detrimental effects on bone health. However, the mechanisms responsible for exercise-induced bone loss remain unknown.
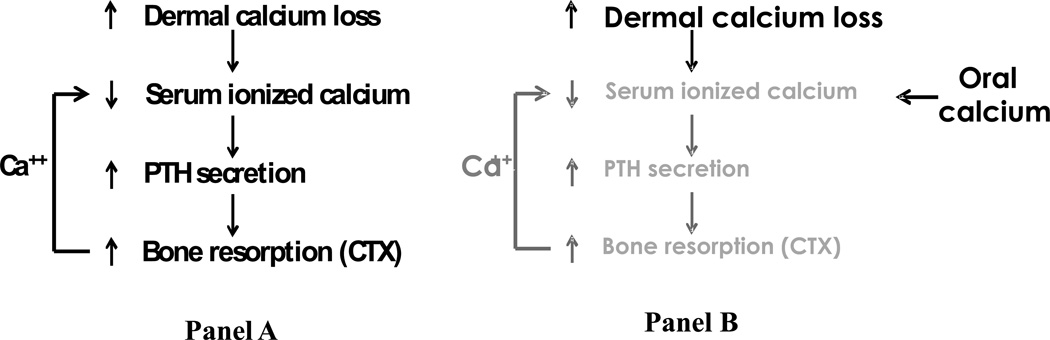
A disruption of calcium homeostasis during exercise is a potential mediator of bone loss, as shown in the conceptual model (Figure 1, panel A). One hypothesis is that prolonged or excessive sweating during exercise triggers metabolic responses that acutely activate bone resorption and, when this occurs repetitively (i.e., exercise training), could lead to bone loss. Accordingly to this model, calcium loss through sweating activates a cascade of events. Because sweat is derived from plasma, sweat losses with exercise would be predicted to trigger a decline in serum ionized calcium (iCa). Because serum calcium levels are vigorously defended, even a small decrease would trigger an increase in serum parathyroid hormone (PTH), which is a potent stimulator of bone resorption. The mobilization of calcium from the skeleton protects against a further decline in serum calcium.
Figure 1.
Conceptual model showing the pathway by which exercise-induced disruptions of calcium homeostasis may trigger a decrease in BMD (Panel A), and the possible attenuation of bone resorption by supplemental calcium (Panel B; PTH, parathyroid hormone; CTX, C-terminal telopeptide of type I collagen; Ca++, calcium).
Although this working model remains hypothetical, there is evidence that steps in the model are operative during exercise. Sweating during exercise has been found to cause a significant dermal calcium loss (1;7) and several studies have found an increase in PTH in response to various modes and durations of exercise (1;4;8;19). There is also limited evidence that C-terminal telopeptide of type I collagen (CTX), which is a systemic biomarker of osteoclast-mediated bone resorption, increases acutely in response to relatively intense exercise (4;8).
If our working model is correct, this raises the question of whether providing supplemental calcium before or during exercise could prevent the decline in serum calcium levels and the resulting release of PTH and activation bone resorption. To our knowledge, the timing of calcium supplementation relative to exercise as a means to attenuate increases in PTH and CTX (Figure 1, panel B) has been examined in only one previous study (4). In that study, exercise-induced increases in PTH and CTX were significantly attenuated when a calcium-enriched beverage was consumed before and during exercise. Although administering high-calcium water for 1 hour before and during exercise was effective in minimizing the activation of calcium homeostatic mechanisms, it may be a challenging strategy for athletes to adopt routinely during training. The purpose of the present study was to evaluate separately the effects of calcium supplementation before or during exercise when compared to placebo on exercise-induced increases in PTH and CTX. We hypothesized that both supplementation strategies would be more effective than placebo in minimizing increases in PTH and CTX in response to exercise. The findings of this study could aid in the design of future prospective studies of the effects of calcium supplementation and exercise on changes in BMD.
Methods
Subjects
Twenty healthy adult male road cyclists and triathletes participated in the study. Exclusion criteria included hyperparathyroidism, vitamin D deficiency, thyroid dysfunction, abnormal liver or kidney function, and routine use of medications known to affect bone or calcium metabolism (e.g., thiazide diuretics, bisphosphonates, oral steroids). Subjects were amateur athletes competing at the state to international level. The study was approved by the Colorado Multiple Institutional Review Board. Each subject gave informed written consent prior to study participation.
Experimental protocol
Participants performed exercise bouts on four separate days. Maximal aerobic power (VO2max) was measured at the first exercise visit. The three subsequent bouts of exercise were 35-kilometer time trials (35-km TT) performed under different conditions of calcium supplementation. We estimated that this exercise bout would take approximately 60 minutes to complete. Time trials of this duration have reported CVs of 3.4% (5). All bouts were performed on an electronically-braked Velotron cycle ergometer (RacerMate, Seattle, WA). Participants were instructed to avoid strenuous exercise the day before and the day of all testing.
VO2max
Subjects performed an incremental exercise test on the cycle ergometer. Subjects began exercising at 50 watts (W) and resistance was increased by 50 W every two minutes up to 200 W. Thereafter, resistance was increased 25 W every 2 minutes until volitional fatigue. Fractions of carbon dioxide and oxygen in exhaled air were measured continuously using a TruMax 2400 metabolic cart (ParvoMedics, Sandy UT). Data were averaged over 60-second intervals to determine VO2max.
35 Kilometer Time Trials
On separate days, subjects performed three 35-km TTs on the cycle ergometer. These bouts were separated by at least two days to allow for recovery, but not more than seven days. We estimated that it would take 50–60 minutes to cycle this distance. This duration of intense exercise has been previously shown to disrupt calcium homeostasis (4;8). A computer display provided subjects with gearing, current and average speed, cadence, grade, and distance. Subjects were instructed to complete each TT as quickly as possible. For purposes of standardization, no outside encouragement was offered during the TT and subjects were not allowed to listen to music. Blood samples were obtained through a peripheral venous catheter at the beginning of the exercise bout, every 15 minutes during exercise, and immediately upon completion. To control for diurnal variation in PTH, a given subject performed all 35-km TTs at the same time of day. Participants were instructed to consume the same foods and beverages prior to each of the TTs to standardize dietary calcium within an individual subject. Indirect calorimetry was not performed during the TTs.
Calcium supplementation
Study beverages included a calcium-free sports beverage (placebo) and a calcium-fortified sports beverage containing 1000 mg of calcium per liter (Aquamin Soluble, marine-derived multi-mineral complex containing calcium citrate malate compound; Marigot Ltd, Cork, Ireland). The placebo and calcium-fortified beverages were otherwise matched for pH, electrolytes, carbohydrate, and taste. Under one test condition, participants consumed 1000 mL of the fortified beverage 20 minutes prior to exercise and 250 mL of the placebo beverage at 0, 15, 30, and 45 minutes of the exercise bout. For the second test condition, subjects consumed 1000 mL of placebo prior to exercise and four 250 mL doses during exercise. For the third condition, subjects consumed the placebo solution at all time points. Both of the calcium supplemented conditions provided a total of 1000 mg of calcium. The three test conditions were administered in a double-blinded, counter-balanced order.
Sweat collection
Sweat was collected during the 35-km TT exercise bouts using a previously developed patch technique (12). Briefly, 42 mm filter paper discs were placed on the skin under an occlusive Parafilm dressing (Structure Probe, West Chester, PA). Patches were applied to each forearm, the upper chest, and below the scapula. These areas were cleaned with deionized water and then dried. Patches were secured using non-permeable tape. Sweat was collected for two 20-minute intervals: the first 20 minutes of exercise and minutes 30–50. The four patches from each time point were placed in a single vial and weighed. The weights of the vial and patches were obtained prior to application. Cesium sulfate (2 mL of 0.75 mol/L) was added to the vials to elute the sweat from the patches. Calcium chloride (4 mL of 5.4 mg/dL) was also added to ensure the resulting solution had a calcium concentration above the detectable limit of 2 mg/dL. The sweat calcium concentration was then calculated from the calcium concentration of this solution by volume and mass balance. Nude, dry body weight was measured before and after each exercise bout. Weight change, corrected for the weight of fluid consumed and any voided urine, was used as an index of sweat loss. The specific gravity of sweat was taken to be 1.00 g/mL. Total dermal calcium loss during the 35-km TT bouts was estimated from the sweat calcium concentration and total sweat loss.
Analyses
Serum PTH was measured using a dual-site immunoassay for intact PTH (Diagnostic Products, Los Angeles, CA); intra- and inter-assay coefficients of variation (CVs) were 6.3 and 8.6%, respectively; the sensitivity of this assay was 3 pg/mL. Sweat calcium was measured using ion-specific electrodes (LXI 725; Beckman-Coulter, Fullerton, CA). Intra- and inter-assay CVs were 3.0 and 4.5%, respectively. Serum ionized calcium was measured using an iSTAT analyzer (Abbott Point of Care Inc, Princeton, NJ) with a manufacturer-reported CV 1.1% and sensitivity of 0.25 mmol/L. CTX was measured by an ELISA (Nordic Bioscience Diagnostics, Herlev, Denmark). Bone-specific alkaline phosphatase (BAP) was also measured by an ELISA (Quidel Corporation, San Jose, CA). In our lab, the intra-assay CVs for BAP and CTX were 7.5±7.1% and 6.2±4.4%, respectively, and inter-assay CVs were 11.5±9.5% and 20.5±11.3%, respectively. Sensitivities for the CTX and BAP assays were 0.020 ng/mL and 0.7 U/L respectively. All CTX and BAP samples were batched and run in duplicate. BMD was measured by a Discovery dual-energy X-ray absorptiometer (Hologic, Waltham, MA). In our lab, CVs for hip and spine BMD measurements ranged from 0.8–1.9%. pH was also measured using the iSTAT analyzer (reported CV 0.08%).
Adjustment for hemoconcentration
Changes in PTH, iCa, CTX, and BAP were correct for changes in plasma volume according to the methods of Van Beaumont et al. (21). Raw hematocrit (Hct) readings were first multiplied by the factor (0.96 × 0.91) to correct for trapped plasma and convert venous to whole-body Hct. Changes in Hct from before (Hct1) to after (Hct2) exercise and the initial concentration (C1) were then used to calculate the expected concentration (CE) based on fluid shifts alone: CE = [Hct2(100 − Hct1)/Hct1(100 − Hct2] × C1. The measured concentration after exercise (C2) was then corrected for CE to yield the Hct-corrected post-exercise concentration (C2’): C2’ = C2 − (CE − C1).
Statistical Analysis
The primary outcomes were the changes in PTH, BAP, and CTX from before to after exercise. The determination of whether the outcomes were different among the three exercise conditions was based on a maximum likelihood repeated measures model. Pre- and post-exercise values of PTH, BAP, CTX, and iCa within a treatment arm were compared with paired t tests. Unless otherwise stated, data are reported as means ± SD. All analyses were performed using SAS 9.1 (SAS Institute Inc., Cary NC). The study was sized to detect a 20 pg/mL attenuation in the pre-post exercise difference in serum PTH due to the administration of calcium using a paired t test, assuming a SD of the difference of 30 pg/mL, with 80% power at the 0.05 level. The expected effect of calcium supplementation on change in serum PTH was based on a study by Guillemant et al. (4) and the estimate of the SD of the difference was based on the standard deviation of change in PTH in response to exercise in one of our studies that involved less-intense exercise, where the average change and standard deviation of change in serum PTH was 29 ±30 pg/mL (1). Spearman correlation coefficients were calculated to explore for relationships between estimated dermal calcium loss and PTH and CTX.
Results
Six subjects (30%) were found to have a total hip or lumbar spine T-score ≤ −1.0 (Table 1). Nine subjects had insufficient 25-hydroxyvitamin D concentrations (i.e., below 30 ng/mL), but none was deficient (i.e., below 20 ng/mL). There was no effect of calcium supplementation on cycling performance time (59 ± 5, 60 ± 6, and 59 ± 5 minutes for placebo, calcium before, and calcium during, respectively). There were no significant differences in baseline Hct values (Table 2). Hct increased similarly under all test conditions.
Table 1.
Subject characteristics (n=20)
| Variable | Mean ± SD |
|---|---|
| Age (yr) | 37.0 ± 7.6 |
| Weight (kg) | 75.7 ± 8.8 |
| Height (m) | 1.80 ± 0.06 |
| Total hip BMD (g/cm2) | 1.043 ± 0.106 |
| Total hip T-score | 0.07 ± 0.71 |
| L1-L4 BMD (g/cm2) | 1.030 ± 0.132 |
| Lumbar spine T-score | −0.56 ± 1.20 |
| VO2max (mL/kg/min) | 53.0 ± 7.3 |
| Years of cycling competition | 6.0 ± 6.5 |
| Serum 25-hydroxyvitamin D (ng/mL) | 32.7 ± 9.2 |
Table 2.
Serum concentrations of PTH, CTX, BAP, iCa, and Hb before and after exercise.
| Condition | ||||
|---|---|---|---|---|
| Variable | Placebo | Ca before | Ca during | |
| PTH (pg/mL) | before | 51.44 ± 4.58 | 44.13 ± 4.27 | 54.80 ± 5.57 |
| after | 125.47 ± 16.14 | 99.89 ± 16.61 | 112.81 ± 20.06 | |
| afteradj | 121.54 ± 16.01 | 96.19 ± 16.47 | 108.01 ± 20.04 | |
| change | 74.03 ± 14.22* | 55.77 ± 15.03*† | 58.01 ± 17.43*‡ | |
| changeadj | 70.10 ± 14.18* | 52.06 ± 15.01*† | 53.21 ± 17.48*‡ | |
| CTX (ng/mL) | before | 0.59 ± 0.05 | 0.68 ± 0.05 | 0.60 ± 0.05 |
| after | 0.82 ± 0.09 | 0.85 ± 0.07 | 0.88 ± 0.07 | |
| afteradj | 0.77 ± 0.08 | 0.79 ± 0.07 | 0.82 ± 0.07 | |
| change | 0.24 ± 0.06* | 0.17 ± 0.05* | 0.28± 0.06* | |
| changeadj | 0.19 ± 0.06* | 0.11 ± 0.05* | 0.23 ± 0.06* | |
| BAP (U/L) | before | 23.60 ± 1.40 | 21.98 ± 1.53 | 22.35 ± 1.42 |
| after | 24.95 ± 1.71 | 23.23 ± 1.51 | 24.04 ± 1.51 | |
| afteradj | 24.95 ± 1.71 | 21.62 ± 1.49 | 21.96 ± 1.40 | |
| change | 1.35 ± 0.90 | 1.25 ± 0.79 | 1.69 ± 0.82 ** | |
| changeadj | −0.40 ± 0.93 | −0.36 ± 0.72 | −0.38 ± 0.86 | |
| iCa (mmol/L) | before | 1.20 ± 0.01 | 1.24 ± 0.01 | 1.21 ± 0.01 |
| after | 1.14 ± 0.01 | 1.17 ± 0.01 | 1.16 ± 0.01 | |
| afteradj | 1.05±0.01 | 1.08±0.01 | 1.05±0.01 | |
| change | −0.06 ± 0.01* | −0.06 ± 0.01* | −0.06 ± 0.01* | |
| changeadj | −0.16 ± 0.02* | −0.16 ± 0.01* | −0.17 ± 0.02* | |
| Hct (%) | before | 44.80 ± 0.53 | 44.85 ± 0.63 | 44.65 ± 0.63 |
| after | 46.80 ± 0.51 | 46.90 ± 0.54 | 47.05 ± 0.58 | |
| change | 2.00 ± 0.36* | 2.05 ± 0.59* | 2.40 ± 0.24* | |
Values are means ± SE.
Pre- vs post-exercise, *p < 0.01,
p=0.05;
change different from placebo, † p≤0.04,
p=0.07.
PTH, parathyroid hormone; CTX, C-terminal telopeptide of type I collagen; BAP, bone-specific alkaline phosphatase; iCa, ionized calcium; Hb, hemoglobin; Ca, calcium; adj, adjusted for hemoconcentration.
There were no significant differences in pre-exercise values of PTH, CTX, BAP, or iCa across test conditions (Table 2). PTH and CTX increased and iCa decreased under all test conditions (p<0.05) irrespective of adjustment for hemoconcentration. Calcium supplementation before exercise attenuated the increase in PTH relative to placebo (p=0.04; Figure 2); when adjusted for hemoconcentration this difference remained significant (p=0.05). There was a similar response for calcium supplementation during exercise vs. placebo but the difference was not significant (p=0.07 unadjusted and hemoconcentration adjusted). Any calcium supplementation (before or during exercise) attenuated the exercise-induced increase in PTH (p=0.02 unadjusted; p=0.03 adjusted).
Figure 2.
Unadjusted changes in parathyroid hormone (PTH; upper left), C-terminal telopeptide of type I collagen (CTX; upper right), bone-specific alkaline phosphatase (BAP; lower left), and ionized calcium (iCa; lower right) in response to exercise under varying calcium (Ca) supplementation strategies. Values are mean ± SEM. * different from placebo, p=0.04; ** different from placebo, p=0.07.
There were no significant effects of calcium before or during exercise on changes in CTX or iCa, although the smallest increases in CTX occurred when calcium was ingested before exercise. BAP increased during the condition when calcium was provided during exercise (p=0.05). However, the increase in BAP was no longer significant when adjusted for hemoconcentration (p=0.66). Additionally, the increase in BAP when calcium was provided before exercise was not statistically different from that observed under the other conditions.
Dermal calcium loss was estimated at 120.4 ± 101.3 mg (n=19), 147.4 ± 61.0 mg (n=18), and 137.2 ± 83.8 mg (n=20) for placebo, calcium before, and calcium during exercise respectively. Complete sweat calcium data were not available because three of the samples had calcium concentrations below the detection threshold of 2 mg/dL. There were no significant differences in estimated calcium losses among the test conditions. There were no significant correlations between estimated dermal calcium loss and changes in PTH, CTX, or BAP under any test condition. Sweat loss as estimated by weight loss was −1.5 ± 0.1 kg under all three conditions. There were no differences in ambient temperature (mean 22°C) or humidity (mean 33%) among the test conditions. No subjects voided urine prior to obtaining the post-exercise weight used to estimate sweat weight.
Discussion
The major finding of the study was that calcium supplementation before intense exercise diminished the exercise-induced increase in PTH. Calcium during exercise may have a similar effect (p=0.07). However, neither calcium before or during exercise significantly attenuated the increase in CTX measured immediately after the exercise bout. To our knowledge, only one prior study investigated the effects of calcium supplementation temporally linked with exercise (4). The current study corroborated the finding in that study that calcium supplementation before and during exercise attenuated the exercise-induced increase in PTH and we extend the results of Guillemant et al. with the novel finding that calcium supplementation before exercise alone, as opposed to before and during exercise, is capable of minimizing the exercise-induced increase in PTH. However, our findings do not corroborate the attenuation of an exercised-induced increase in bone resorptive activity, as measured by CTX, that was previously observed. Thus, our findings would support the rationale for a prospective study of the effects of calcium supplementation before exercise training on exercise-induced changes in BMD.
There are limited data to support the conceptual model by which dermal calcium loss may lead to increased bone resorption in response to exercise. First, significant dermal calcium loss with exercise has previously been demonstrated. Two hours of moderate intensity cycling on a stationary ergometer lead to an estimated dermal calcium loss of 138 ± 72 mg (69 ± 36 mg/hr) (1). The same study also demonstrated an increase in PTH of 30.7 ± 28.5 pg/mL from baseline. In the current study, approximately 1 hour of more intense exercise was associated with an estimated dermal calcium loss of 126 ± 93 mg and an increase in PTH of 74.0 ± 63.3 pg/mL. These findings support the notion that vigorous and/or prolonged exercise can generate significant dermal calcium losses and suggest that the rate of dermal Ca loss may be a key factor underlying the PTH response to exercise.
There are limited data to support the second step in the conceptual model: a decline in serum calcium as the stimulus for an increase in PTH. Several studies measured ionized calcium, the form of calcium sensed by the parathyroid gland. The current study and others (9;10), found that intense exercise causes a decline in serum iCa levels (without adjustment for hemoconcentration). However, less intense exercise did not affect iCa concentrations (20). The decline in serum calcium observed in some studies suggests that exercise may lead to a decrease in intra-vascular calcium mass, perhaps as the result of dermal calcium loss in the form of sweat, and supports the notion that some forms of exercise trigger a decrease in serum calcium that requires activation of counter-regulatory mechanisms (i.e., PTH). Some of the discordance among studies may be due to the intensity or duration of the exercise studied, the timing of measurements during exercise, and/or the form of calcium assessed. The observation that serum iCa declined with exercise suggests that total calcium losses (either dermal, urinary, or gastrointestinal) exceeded intestinal calcium absorption during the study period.
Exercise has been associated with an increase in PTH in a number of studies (1;4;8;9;16;19). PTH is a calciotropic hormone that is secreted in response to a decrease in serum ionized calcium concentration. PTH defends serum calcium levels through multiple mechanisms, including the mobilization of calcium from bone, decreased urinary calcium excretion, and increased calcium absorption in the intestine. Although the mechanism underlying the increase in PTH in response to exercise is not known, we postulate that the trigger is a decrease in serum ionized calcium, perhaps secondary to calcium loss through sweating. To our knowledge, this hypothesis has not been tested in a definitive manner. PTH is secreted within seconds of even a small decrease in iCa (3). In response to the increase in PTH, calcium increases within minutes to normalize serum calcium (14). This dynamic process insures rapid regulation of serum calcium. Therefore, if dermal calcium loss causes a decline in serum calcium during exercise, the rapid increase in PTH would act as an acute counter-regulatory mechanism. Measuring PTH and iCa at a single time point after exercise does not reveal the dynamic nature of calcium regulation during exercise.
The findings of the present study and another investigation support the hypothesis that a decline in serum Ca during exercise triggers the increase in PTH. Guillemant et al. also found that calcium supplementation attenuated the increase in PTH with exercise (4). In their study, trained subjects exercised for 60 minutes at 80% of VO2max under two calcium supplementation conditions. On one occasion, low-calcium tap water was consumed on a scheduled basis before and during exercise. On another occasion, high-calcium mineral water was consumed on the same schedule. PTH increased under both calcium conditions, but to a lesser extent with the high-calcium mineral water. Presumably, supplemental calcium provides a non-skeletal source of calcium to help stabilize serum calcium, thereby minimizing the extent to which skeletal stores are released.
The fourth step of the conceptual model suggests that intense endurance exercise that generates an increase in PTH will trigger an increase in bone resorption. Two studies of intense exercise bouts lasting approximately one hour both revealed increases in PTH and CTX, a marker of bone resorption, immediately after exercise (4;8). The only study to measure these parameters during recovery after exercise found that CTX peaked 1 hour after exercise and was still elevated at 2 hours of recovery (4). Of particular note, high-calcium water ingested before and during exercise prevented the rise in CTX after exercise that occurred when low-calcium water was ingested; this was seemingly consequent to the attenuation of the exercise-induced PTH response in the high-calcium condition. The finding that calcium supplementation during exercise attenuates increases in PTH and bone resorptive activity (CTX) suggests that the disruption in calcium homeostasis can be minimized when calcium is available to be absorbed from the gut (Figure 1, panel B). In the current study, supplemental calcium before or during exercise did not significantly attenuate the CTX response when measured immediately after exercise. However, the smallest increase occurred when calcium was ingested before exercise. It is possible that differences in the change in CTX among conditions would have been more apparent 1 hour after exercise.
Timing of calcium supplementation relative to exercise may be a key determinant of its effects on both calcium homeostasis and bone metabolism. Competitive male road cyclists were recently found to lose BMD over a year of training and competition (2). Participants in that study were randomized to consume calcium at doses of either 1500 mg/day (500 mg with meals) or 250 mg/day (with one meal). There was no difference in the decrease in BMD between the high- and low-dose groups. In contrast, Klesges et al. found that calcium supplementation during exercise and with meals reversed the decrease in bone mineral content (BMC) observed in male collegiate basketball players the previous year (7) when no supplemental calcium was provided. In that study, the athletes had a ≥3% decrease in both leg and total body BMC during the first year of the investigation. The following year athletes consumed a calcium-fortified beverage during all practice sessions and a calcium supplement with meals (up to 1800 mg/day) BMC increased ≥2% at these sites. The disparate findings of these two studies suggest that the timing of supplemental calcium ingestion relative to exercise may be a critical determinant of its effects on bone.
The effects of repeated bouts of transient exercise-induced increases in PTH on bone have yet to be determined. If dermal calcium loss triggers the exercise-induced increases in PTH and CTX (i.e., bone resorptive activity), it is possible that any form of exercise that generates sweating disrupts calcium and bone homeostasis. Whether exercise training has beneficial effects on BMD may be determined by the balance of favorable factors (e.g, high magnitude skeletal strain) and potentially detrimental factors (e.g., skeletal demineralization to maintain eucalcemia).
This study had limitations that should be acknowledged. PTH is known to have a diurnal variation of approximately 13 pg/mL (6) and we did not standardize the time of testing between subjects. However, time of exercise within each subject was standardized and the magnitude of the changes in PTH was significantly greater than the reported diurnal variation. Diet was not standardized for calcium and vitamin D on the day of testing. O note, the absence of differences in pre-exercise PTH values suggests that dietary calcium intake preceding each TT was fairly constant as the ingestion of 180 mg of calcium decreases PTH for several hours in healthy younger men (17). Sweat rate and composition vary by body region, (13) and sweat rate varies greatly depending on exercise intensity, hydration status, acclimation, and ambient conditions. We are unaware of any studies comparing estimated dermal calcium losses from patch techniques to whole-body washdown. Recognizing these limitations, we were able to provide only a gross estimate of dermal calcium loss. Finally, much more work is needed to evaluate each step of the postulated mechanistic pathway (Figure 1).
In summary, calcium supplementation before exercise attenuated the increase in PTH, but had no affect on the changes in bone resorptive activity (i.e., CTX) or iCa. The ability of calcium to attenuate the increase in PTH is presumably due to an increased contribution of intestinal calcium absorption to normalize serum calcium during exercise. Further research is needed to determine if calcium supplementation timed relative to exercise can minimize detrimental effects or augment the beneficial effects of exercise training on BMD. This easily adoptable routine (calcium supplementation before exercise) could be used to prospectively study the effects of calcium supplementation on changes in BMD in response to exercise training.
Acknowledgements
The authors thank the staff of the University of Colorado Clinical and Translational Research Center for their technical assistance. This research was supported by Clinical and Translational Research Center award 1 UL1 RR 025780, the Clinical Nutrition Research Unit award P30 KD048520, GTC Nutrition (Golden, CO), and Marigot Ltd (Cork, Ireland).
Footnotes
The authors report no conflict of interest or endorsement by the ACSM.
Reference List
- 1.Barry DW, Kohrt WM. Acute effects of 2 hours of moderate-intensity cycling on serum parathyroid hormone and calcium. Calcif. Tissue Int. 2007;80:359–365. doi: 10.1007/s00223-007-9028-y. [DOI] [PubMed] [Google Scholar]
- 2.Barry DW, Kohrt WM. BMD decreases over the course of a year in competitive male cyclists. J.Bone Miner.Res. 2008;23:484–491. doi: 10.1359/jbmr.071203. [DOI] [PubMed] [Google Scholar]
- 3.Brown EM. Calcium receptor and regulation of parathyroid hormone secretion. Rev.Endocr.Metab Disord. 2000;1:307–315. doi: 10.1023/a:1026570518919. [DOI] [PubMed] [Google Scholar]
- 4.Guillemant J, Accarie C, Peres G, Guillemant S. Acute effects of an oral calcium load on markers of bone metabolism during endurance cycling exercise in male athletes. Calcif Tissue Int. 2004;74:407–414. doi: 10.1007/s00223-003-0070-0. [DOI] [PubMed] [Google Scholar]
- 5.Jeukendrup A, Saris WH, Brouns F, Kester AD. A new validated endurance performance test. Med.Sci.Sports Exerc. 1996;28:266–270. doi: 10.1097/00005768-199602000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Kitamura N, Shigeno C, Shiomi K, et al. Episodic fluctuation in serum intact parathyroid hormone concentration in men. J Clin.Endocrinol.Metab. 1990;70:252–263. doi: 10.1210/jcem-70-1-252. [DOI] [PubMed] [Google Scholar]
- 7.Klesges RC, Ward KD, Shelton ML, et al. Changes in bone mineral content in male athletes: mechanisms of action and intervention effects. JAMA. 1996;276:226–230. [PubMed] [Google Scholar]
- 8.Maimoun L, Manetta J, Couret I, Dupuy AM, Mariano-Goulart D, Rossi M. The intensity level of physical exercise and the bone metabolism response. Int J Sports Med. 2006;27:105–111. doi: 10.1055/s-2005-837621. [DOI] [PubMed] [Google Scholar]
- 9.Maimoun L, Simar D, Malatesta D, et al. Response of bone metabolism related hormones to a single session of strenuous exercise in active elderly subjects. Br J Sports Med. 2005;39:497–502. doi: 10.1136/bjsm.2004.013151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maimoun L, Simar D, Caillaud C, et al. Response of calciotropic hormones and bone turnover to brisk walking according to age and fitness level. J.Sci.Med.Sport. 2009;12:463–467. doi: 10.1016/j.jsams.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Nichols JF, Palmer JE, Levy SS. Low bone mineral density in highly trained male master cyclists. Osteoporosis Int. 2003;14:644–649. doi: 10.1007/s00198-003-1418-z. [DOI] [PubMed] [Google Scholar]
- 12.O'Toole ML, Johnson KC, Satterfield S, et al. Do sweat calcium losses affect bone mass during firefighter training? J Occup.Environ.Med. 2000;42:1054–1059. doi: 10.1097/00043764-200011000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Patterson MJ, Galloway SD, Nimmo MA. Variations in regional sweat composition in normal human males. Exp.Physiol. 2000;85:869–875. doi: 10.1111/j.1469-445x.2000.02058.x. [DOI] [PubMed] [Google Scholar]
- 14.Rasmussen H. Ionic and hormonal control of calcium homeostasis. Am J Med. 1971;50:567–588. doi: 10.1016/0002-9343(71)90113-6. [DOI] [PubMed] [Google Scholar]
- 15.Rector RS, Rogers R, Ruebel M, Hinton PS. Participation in road cycling vs running is associated with lower bone mineral density in men. Metabolism. 2008;57:226–232. doi: 10.1016/j.metabol.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Rong H, Berg U, Torring O, Sundberg CJ, Granberg B, Bucht E. Effect of acute endurance and strength exercise on circulating calcium-regulating hormones and bone markers in young healthy males. Scand J Med Sci Sports. 1997;7:152–159. doi: 10.1111/j.1600-0838.1997.tb00132.x. [DOI] [PubMed] [Google Scholar]
- 17.Sripanyakorn S, Jugdaohsingh R, Mander A, Davidson SL, Thompson RP, Powell JJ. Moderate ingestion of alcohol is associated with acute ethanol-induced suppression of circulating CTX in a PTH-independent fashion. J.Bone Miner.Res. 2009;24:1380–1308. doi: 10.1359/JBMR.090222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suominen H. Bone mineral density and long term exercise. An overview of cross-sectional athlete studies. Sports Med. 1993;16:316–330. doi: 10.2165/00007256-199316050-00003. [DOI] [PubMed] [Google Scholar]
- 19.Thorsen K, Kristoffersson A, Hultdin J, Lorentzon R. Effects of moderate endurance exercise on calcium, parathyroid hormone, and markers of bone metabolism in young women. Calcif Tissue Int. 1997;60:16–20. doi: 10.1007/s002239900179. [DOI] [PubMed] [Google Scholar]
- 20.Thorsen K, Kristoffersson A, Lorentzon R. The effects of brisk walking on markers of bone and calcium metabolism in postmenopausal women. Calcif.Tissue Int. 1996;58:221–225. doi: 10.1007/BF02508639. [DOI] [PubMed] [Google Scholar]
- 21.Van Beaumont W, Strand JC, Petrofsky JS, Hipskind SG, Greenleaf JE. Changes in total plasma content of electrolytes and proteins with maximal exercise. J.Appl.Physiol. 1973;34:102–106. doi: 10.1152/jappl.1973.34.1.102. [DOI] [PubMed] [Google Scholar]