Abstract
Background
Co-occurring alcohol use disorder and major depression (C-ALDP) is a major public health problem. Yet, the available evidence is mixed regarding the implications of C-ALDP for alcohol involvement. The purpose of this research was to examine the associations between past 12-month co-occurring AUDs (abuse and dependence) and major depressive episode (MDE) and alcohol involvement in a representative community sample.
Design
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) is a national household survey of 43,083 adults ages 18 and older. For the NESARC, the target population is the civilian noninstitutionalized population, 18 years of age and older, living in the United States and the District of Columbia.
Methods
All NESARC interviews were conducted with the Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM IV Version (AUDADIS-IV; Grant et al., 2003).
Results
Prevalence of past 12-month co-occurring AUD (abuse or dependence) and MDE was 1.2%, corresponding to about 2.4 million adults ages 18 and older. Among males with alcohol dependence, comorbid MDE was associated with a greater number of days drinking at home alone. Among females and males with alcohol abuse and dependence, comorbid MDE was associated with higher prevalence of drinking to enhance depressed mood. Comorbid MDE was also associated with lower levels of some drinking behaviors among those with alcohol abuse.
Conclusions
Co-occurring AUDs and MDE are associated with specific dimensions of alcohol involvement, and this association is more consistent for alcohol dependence than abuse.
Keywords: Comorbidity, Alcohol Use Disorders, Major Depressive Episode, Solitary Drinking, Affect Regulation
1. INTRODUCTION
Do individuals with co-occurring alcohol use disorders (AUDs) and major depression have greater alcohol involvement than those with AUD alone? Some studies using clinical samples showed that the co-occurrence of alcoholism and depression (C-ALDP) is associated with worse alcohol-related outcomes, and this relationship appears to be stronger in males than females (Pettinati et al., 1997). However, “less is known…about patterns and correlates of dual diagnosis in the general population” (Kessler, 2004, p. 730). The purpose of the present study was to examine the prevalence and alcohol-related correlates of a particular form of comorbidity, i.e., the co-occurrence of abuse and dependence (AUD) and major depressive episode (MDE).
Results from several epidemiologic studies indicated substantial co-occurrence of psychiatric and substance use disorders (SUD) (Epstein et al., 2004; Grant et al., 2004; Kandel et al., 2001; Kessler et al., 1997; Merikangas et al., 1998; Regier et al., 1990). For example, results from the 1990–1992 National Comorbidity Study (NCS) showed that 50.9% of participants with a lifetime DSM-III-R diagnosis of at least one psychiatric disorder also had a lifetime diagnosis of at least one SUD; similarly, 51.4% of participants with a lifetime SUD also had a lifetime diagnosis of at least one psychiatric disorder (Kessler et al., 1996). Among the numerous forms of comorbid mental health and substance use disorders, the co-occurrence of alcohol use disorders and depression has received considerable attention (Li et al., 2004). Below we review previous research on the prevalence of AUD and MDE, along with evidence suggesting that the co-occurrence of AUD and MDE may be more pernicious than either disorder alone.
1. AUDs and depression are among the most prevalent psychiatric disorders (Grant et al., 2004)
Recent epidemiologic studies indicated that the past 12-month prevalence rate of any AUD (including alcohol abuse and dependence) is about 8.5% of adults ages 18 and over (Grant et al., 2004), and the past 12-month prevalence rate of MDE is about 7.2% of adults ages 18 and over (Grant et al., 2004). Epidemiologic studies consistently show that AUDs are more prevalent among males than females (Zucker, 2006), although this gender difference appears to be decreasing (Grant et al., 2004; Nolen-Hoeksema, 2004). By contrast, depressive disorders are about two times more prevalent among females than males (Nolen-Hoeksema, 2001). Although gender differences in C-ALDP are not as well documented, evidence suggests that rates may be higher among females than males (Blazer et al., 1994; Davis et al., 2005).
2. AUDs and depression have relatively high rates of co-occurrence
AUDs and depression co-occur at levels greater than expected by chance in clinical and epidemiological samples (Sullivan et al., 2005; Swendsen and Merikangas, 2000). Evidence from the 2001–02 NESARC showed that 13.7% of those with a past year AUD also had a past year MDE, compared to a 7.2% base rate of past year MDE (Grant et al., 2004). In addition, 16.4% of those with a past year MDE had a past year AUD, compared to an 8.5% base rate of past year AUD (Grant and Harford, 1995). Using the same data set but assessing MDD instead of MDE, Hasin et al. (2005), found that 40.3% of those with a lifetime MDD also had a lifetime AUD.
3. AUDs, depression, and their co-occurrence impose a tremendous burden on individuals, families, and communities
As separate disorders, AUDs and depression exact a tremendous toll world-wide. The Global Burden of Disease 2000 Study conducted by the World Health Organization (WHO, 2001) found that AUDs and depression are among the leading causes of disability in the world, as measured by disability-adjusted life years (DALYs) and years of life lived with disability (YLDs) (Room et al., 2005; Ustun et al., 2004). Among those with an AUD, comorbid depression is associated with an earlier onset of alcohol dependence, higher rates of lifetime drug dependence (Schuckit et al., 1997); worse outcomes among those entering treatment for alcohol and drug problems (Hasin et al., 2002); higher relapse following AUD treatment among adolescents (Cornelius et al., 2004) and adults (Greenfield et al., 1998); greater severity of suicidality in adult psychiatric patients (Cornelius et al., 1995); and higher likelihood of suicide attempts (Conner et al., 2007; Preuss et al., 2002) and completed suicides (Conner and Duberstein, 2004).
The purpose of this research was to examine the associations between past 12-month co-occurring AUDs and major depressive episode (MDE) and alcohol involvement in a representative community sample. Conner et al. (2009, p. 128), observed that, despite good evidence linking C-ALDP with numerous adverse outcomes, data on the implications of C-ALDP for drinking outcomes are not as definitive. Affect regulation models highlight the reduction of negative affect as a motivation for alcohol and other drug use (Baker et al., 2004; Kassel et al., 2003). Accordingly, we hypothesized that C-ALDP would be associated with higher levels of alcohol involvement and drinking to enhance mood compared to AUDs and MDE alone. In addition, previous research showed that C-ALDP may have a greater impact on males than females (Kranzler et al., 1996). Based on this work, we also hypothesized that the effects of C-ALDP on alcohol involvement would be stronger among males than females.
2. Methods
We conducted secondary data analyses of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Grant et al., 2003), a national household survey sponsored, designed and conducted by the National Institute on Alcohol Abuse and Alcoholism (NIAAA). The NESARC is the largest and most comprehensive study of alcohol use disorders and co-occurring psychiatric disorders that has ever been conducted in the United States.
Sample Design
For the NESARC, the target population is the civilian noninstitutionalized population, 18 years of age and older, living in the United States and the District of Columbia. The target population included persons living in households and in certain noninstitutionalized group quarters (i.e., boarding and rooming houses, nontransient hotels and motels, shelters, facilities for housing workers, college quarters, and group homes). After the sample was weighted, the NESARC data were adjusted based on the 2000 Decennial Census so that they were representative of the civilian noninstitutionalized U.S. population for region, sex, age race, and ethnicity (Grant et al., 2003; Grant et al., 2004).
Response Rates and Sample Characteristics
For Wave 1 (W1) of the NESARC, face-to-face interviews were conducted with 43,093 participants using computer assisted personal interviewing (CAPI). At W1, the NESARC achieved a sampling frame response rate of 99%, a household response rate of 89%, and a person response rate of 93%, for an overall response rate of 81% (Grant et al., 2004). Based on weighted data, the final sample was 52.1% female; with respect to age, 21.8% of the participants were 18–20 years old, 30.9% were 30–44 years old, 31.1% were 45–64 years old, and 16.2% were 65 years or older; with respect to race/ethnicity, 70.9% of the participants were White, 11.1% were Black, 11.6% were Hispanic, 4.4% were Asian or Pacific Islander; and 2.1% were Native American (Grant et al., 2004).
2.1. Measures
Demographic and background variables assessed in the NESARC included sex, age, race/ethnicity, marital status, highest year of school completed, and total household income in the past 1 year.
AUDADIS-IV
All NESARC interviews were conducted with the National Institute on Alcohol Abuse and Alcoholism Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM IV Version (AUDADIS-IV) (Grant et al., 2003). The AUDADIS-IV is a structured diagnostic interview with modules that assess DSM-IV alcohol use disorders, mood and anxiety disorders, drug and nicotine use disorders, personality and conduct disorders, pathological gambling, and family history of alcoholism, and major depression. Numerous psychometric studies have documented the reliability and validity of the AUDADIS-IV (Grant et al., 2003).
Past 12 Month DSM-IV Alcohol Use Disorder (AUD)
Consistent with DSM-IV criteria (American Psychiatric Association, 1994), a diagnosis of past 12 month DSM-IV alcohol abuse required participants to meet at least one of four criteria for alcohol abuse in the year preceding the interview, without meeting criteria for alcohol dependence. The past year prevalence of DSM-IV alcohol abuse in W1 of the NESARC was 4.6% (Grant et al., 2004). A diagnosis of past 12 month DSM-IV alcohol dependence required participants to meet at least three of seven alcohol dependence criteria in the year preceding the interview. The past year prevalence of DSM-IV alcohol dependence in W1 of the NESARC was 3.8% (Grant et al., 2004).
Past 12 Month DSM-IV Major Depressive Episode (MDE)
Consistent with DSM-IV criteria (American Psychiatric Association, 1994), a diagnosis of past 12 month major depressive episode (MDE) required participants to meet at least five of nine criteria for at least 2 weeks (at least one of which must be depressed mood or anhedonia). Following Grant et al. (2004), we used DSM-IV diagnosis of primary MDE, which excludes substance-induced MDE and MDE due to medical conditions or bereavement. The past 12-month prevalence of MDE was 7.2% (Grant et al., 2004).
Past 12 Month Co-Occurrence of AUD and MDE (C-ALDP) was constructed from the past year AUD and MDE variables. This categorical variable was coded 1=No past year AUD/No past year MDE; 2=Yes past year MDE/No past year AUD; 3=No past year MDE/Yes past year alcohol abuse (AB); 4=Yes past year MDE/Yes past year AB; 5=No past year MDE/Yes past year alcohol dependence (AD); and 6=Yes past year MDE/Yes past year AD.
Past 12-Month Alcohol Involvement
Eight items assessed the frequency of various forms of alcohol involvement in the past 12 months, including 1) number of drinking days, 2) number of days drank enough to feel intoxicated or drunk, 3) number of days drank at home alone, 4) number of days drank before 3pm on any day of the week, 5) number of days drank at two or more separate times during the same day, 6) number of days drove a car or other motor vehicle after having 3 or more drinks, 7) number of days drank after midnight on any day of the week, and 8) number of days drank in public places. Two items assessed quantity of alcohol consumption in the past 12 months: 1) usual number of drinks per drinking day, and 2) largest number of drinks in a single day. One variable assessed average daily volume of ethanol intake, and one item assessed the use of alcohol to enhance mood.
3. Results
3.1. Analysis Plan
In order to examine the main and interactive effects of past 12-month C-ALDP and sex on alcohol involvement, we used the framework outlined in Jaccard (1998; Jaccard and Guilamo-Ramos, 2002). Past 12-month C-ALDP was designated as the focal independent variable and sex was designated as the first-order moderator variable. We conducted a series of weighted design-based multiple linear and multiple logistic regression analyses to assess the effects of past 12-month C-ALDP and sex on continuous and binary alcohol-related outcomes, respectively. For alcohol-related response variables that took the form of counts, we estimated a series of weighted design-based generalized linear models with a log link and a Poisson sampling model (Long, 1997). The REGRESS, LOGISTIC, and LOGLINK procedures in SUDAAN were used to estimate conditional marginal means for C-ALDP and sex (controlling for covariates). Main effects, simple main effects, and interaction contrasts were tested with single degree-of-freedom contrasts (Jaccard, 1998). As described by Jaccard and Turrisi (2003), simple main effects analyses examine the association between a focal independent variable and a dependent variable at a given level of a moderator variable. Interaction contrasts compare the effects of a focal independent variable on the dependent variable at different levels of the moderator variable. All analyses statistically controlled for age, race/ethnicity, past 12-months personal income, level of education, marital status, urbanicity, geographic region, past 12-months anxiety disorder (Schuckit et al., 1997); past 12-months tobacco dependence (Daeppen et al., 2000); past 12-months drug use disorder (Regier et al., 1990); and any lifetime personality disorder (Hasin et al., 2007).
Because the NESARC used a complex sample design, estimation procedures that assume simple random sampling cannot be used (West, 2008). Accordingly, all parameters, 95% confidence intervals (CIs) and standard errors were estimated using SUDAAN v. 10.0 (Research Triangle Institute, 2008), a statistical software program that uses Taylor series linearization to adjust for complex survey sample design effects. A modified Bonferrroni correction (Holland and Copenhaven, 1987) to maintain the alpha at .05 was applied to the following families: 1) main effects, 2) simple main effects, and 3) interaction contrasts (Jaccard, 1998).
3.2. Prevalence and Demographic Correlates of Past 12-Month C-ALDP
The prevalence of past 12-month comorbid alcohol abuse and MDE was 0.4%, and the prevalence of past 12-month comorbid alcohol dependence and MDE was 0.8%. The overall prevalence of past 12-month C-ALDP was 1.2%, representing approximately 2.4 million adults ages 18 and over. Bivariate associations between demographic variables and C-ALDP showed that the prevalence of C-ALDP was virtually identical for females and males. C-ALDP was more prevalent among the 18–29 age group and decreased with age. Race/ethnicity was also significantly associated with C-ALDP, with a pattern of results indicating that prevalence of C-ALDP, and AUD with no MDE, were highest among American Indians and b) lowest among Asians.
3.3. Past 12-Month Alcohol Involvement as a Function of AUD-MDE
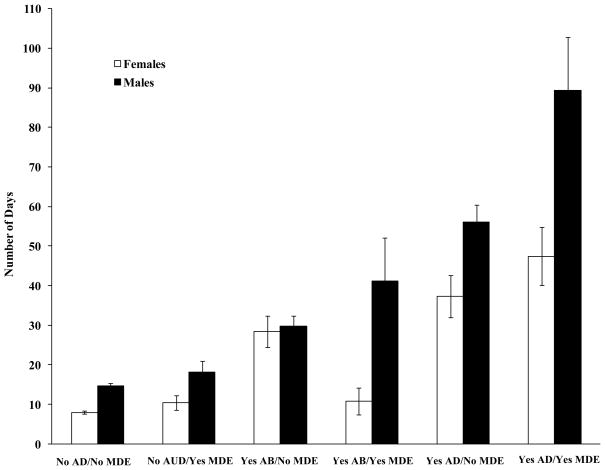
Estimated marginal means for each dependent variable by C-ALDP and sex are presented in Table 1. Results for the eight measures of drinking frequency indicated main effects of sex and C-ALDP. Males showed significantly higher frequency of all forms of alcohol involvement compared to females. Simple main effects contrasts showed that, among males with alcohol dependence, MDE was associated with higher frequency of drinking across all eight measures. However, this contrast was statistically significant for only one measure: males in the Yes MDE/Yes AD group reporting significantly more days drinking at home alone in the past 12 months than males in the No MDE/Yes AD group, c = 33.2, p < .01 (see Figure 1). In line with these results, simple main effects analyses showed that the odds of drinking to enhance mood (DEM) were higher for a) the Yes MDE/Yes AB group compared to the No MDE/Yes AB group, and b) the Yes MDE/Yes AD group compared to the No MDE/Yes AD group. As seen in Table 1, the effects of C-ALDP did not differ by sex. None of the interaction contrasts were statistically significant.
Table 1.
Alcohol Involvement as a Function of Co-Occurring Past Year Alcohol Use Disorder and Major Depressive Episode and Sex
| 1. No. of drinking days in past year | 2. No. of days intoxicated/past year | 3. No. of days drank home alone/past year | 4. No. of days drank 2+ times in same day | |||||
|---|---|---|---|---|---|---|---|---|
| Females | Males | Females | Males | Females | Males | Females | Males | |
| No AUD/No MDE | 54.4 | 81.8 | 4.1 | 6.8 | 7.9 | 14.7 | 1.7 | 4.1 |
| No AUD/Yes MDE | 46.7 | 72.1 | 4.0 | 6.3 | 10.4 | 18.2 | 1.9 | 3.1 |
| Yes Abuse/No MDE | 121.4 | 147.9 | 11.0 | 15.2 | 28.4 | 29.7 | 5.9 | 9.7 |
| Yes Abuse/Yes MDE | 101.0 | 123.5 | 7.1 | 21.4 | 10.7 | 41.1 | 3.6 | 13.7 |
| Yes Dependence/No MDE | 169.6 | 207.3 | 28.6 | 44.6 | 37.3 | 56.1 | 12.7 | 23.5 |
| Yes Dependence/Yes MDE | 159.9 | 215.7 | 24.0 | 51.5 | 47.4 | 89.3 | 15.8 | 41.8 |
|
| ||||||||
| 5. No. of days drank before 3pm | 6. No. of days drank after midnight | 7. No. of days drink driving | 8. No. of days drank in public places | |||||
|
| ||||||||
| Females | Males | Females | Males | Females | Males | Females | Males | |
|
| ||||||||
| No AUD/No MDE | 3.1 | 7.1 | 4.2 | 6.5 | 1.7 | 3.1 | 11.0 | 14.3 |
| No AUD/Yes MDE | 3.6 | 8.1 | 6.3 | 4.5 | 1.9 | 2.7 | 11.7 | 13.1 |
| Yes Abuse/No MDE | 9.9 | 20.7 | 10.8 | 19.8 | 10.2 | 21.3 | 30.9 | 38.4 |
| Yes Abuse/Yes MDE | 8.1 | 15.3 | 11.1 | 15.7 | 4.5 | 13.9 | 24.0 | 32.9 |
| Yes Dependence/No MDE | 20.0 | 37.3 | 24.3 | 31.2 | 19.8 | 29.4 | 43.1 | 50.1 |
| Yes Dependence/Yes MDE | 20.0 | 48.2 | 20.7 | 32.2 | 12.8 | 42.5 | 31.4 | 50.5 |
|
| ||||||||
| 9. Avg. drinks per day/past year | 10. Max drinks in 1 day/past year | 11. Avg. daily volume consumed | 12. Drank to enhance mood | |||||
|
| ||||||||
| Females | Males | Females | Males | Females | Males | Females | Males | |
|
| ||||||||
| No AUD/No MDE | 1.8 | 2.5 | 2.7 | 4.4 | 0.2 | 0.5 | 0.01 | 0.02 |
| No AUD/Yes MDE | 1.8 | 2.4 | 2.7 | 4.1 | 0.2 | 0.4 | 0.04 | 0.07 |
| Yes Abuse/No MDE | 3.0 | 4.1 | 5.2 | 8.4 | 0.7 | 1.1 | 0.07 | 0.06 |
| Yes Abuse/Yes MDE | 2.7 | 3.3 | 4.8 | 8.0 | 0.6 | 0.8 | 0.17 | 0.26 |
| Yes Dependence/No MDE | 3.9 | 5.2 | 7.3 | 11.4 | 1.3 | 2.0 | 0.31 | 0.33 |
| Yes Dependence/Yes MDE | 3.5 | 5.0 | 6.5 | 11.6 | 1.2 | 2.0 | 0.55 | 0.52 |
Note. For all count variables, cell means are conditional marginal means estimated from weighted design-based multiple Poisson regression analysis. For “avg. daily volume consumed,” cell means are conditional marginal means estimated from weighted design-based multiple linear regression analysis. For “drank to enhance mood,” cell means are conditional prevalence estimates from weighted design-based multiple logistic regression analysis. Adjacent cells within the same column that are shaded with bold text indicate that the means for “No MDE” and “Yes MDE” groups were statistically significantly different based on simple main effects contrasts. All analyses controlled for current age, race/ethnicity, education level, personal income, marital status, urbanicity, geographic region, and other psychiatric disorders (any drug use disorder, any nicotine dependence, any anxiety disorder, and any personality disorder). AUD=Past 12 months DSM-IV Alcohol Use Disorder (abuse and/or dependence). MDE=Past 12 months DSM-IV Major Depressive Episode.
Figure 1.
Number of Days Drank At Home Alone by Past 12 Month Alcohol Use Disorders, Major Depressive Episode, and their Co-Occurrence
Contrary to predictions, results from simple main effects analyses of the contrast between the Yes MDE/Yes AB group and the Yes MDE/Yes AB group showed that, among females with alcohol abuse, MDE was associated with significantly lower frequency of drinking at home alone. In addition, results from simple main effects analyses also showed that, among males with alcohol abuse, MDE was associated with significantly lower quantity of drinking (i.e., average drinks per drinking day and average daily volume of ethanol intake). None of the interaction contrasts were statistically significant.
4. Discussion
The purpose of this research was to examine levels of past 12-month alcohol involvement as a function of C-ALDP in a representative community sample. Compared to each individual disorder, past 12-month C-ALDP had a relatively low prevalence. However, at the national level the prevalence of co-occurring AUDs and MDE (1.1%) translates into approximately 2.4 million adults ages 18 and older. Results from the NSDUH showed a similar but slightly higher prevalence rate of past year major depressive episode (MDE) and AUD (1.2%, approximately 2.7 million adults ages 18 and over) (OAS, 2007). The slightly higher rate obtained by the NSDUH is likely due to the fact that, unlike NESARC, the NSDUH did not exclude participants with MDE caused by medical illness, bereavement, or substance use disorder.
4.1. Alcohol Dependence and MDE
We originally hypothesized that C-ALDP would be associated with higher levels of alcohol involvement compared to AUD and MDE alone, and that these associations would be stronger among males than females. This hypothesis received only partial support. Specifically, we found that 1) among males with past 12-month alcohol dependence, MDE was associated with a greater number of drinking days at home alone; and 2) among females and males with past 12-month alcohol abuse and dependence, MDE was associated with higher odds of drinking to enhance mood. Some previous research has documented higher levels of alcohol involvement among those with C-ALDP compared to those with AUD alone (Hanna and Grant, 1997), and some evidence showed that the effects of C-ALDP are stronger for males than females (Pettinati et al., 1997). However, to our knowledge this is the first study to show more frequent solitary drinking days and higher odds of drinking to enhance mood among those with comorbid AUDs and MDE.
Other studies found no differences in alcohol involvement between those with AUDs alone and those with C-ALDP (Davidson and Blackburn, 1998; Schuckit, 1985). Also, previous research found that C-ALDP is associated with some but not other drinking measures. For example, Rounsaville et al. (1987) followed a sample of 266 hospitalized participants with AUDs one year after discharge and found no significant differences between males with and without MDD on number of drinking days. Our findings concur with those from other studies showing that C-ALDP is differentially associated with drinking outcomes. Results also suggest that if in fact those with C-ALDP consume alcohol to reduce or regulate negative affect, this may translate into a pattern of solitary, sustained heavy drinking.
Results are also consistent with previous research on solitary drinking. For example, Christiansen et al. (2002), found that college students who reported at least one heavy-drinking episode in the past 3 months and at least one lifetime episode of drinking alone had higher levels of depressive symptoms compared to heavy drinkers who never drank alone and non-heavy drinkers. Participants who reported drinking alone also showed higher levels of alcohol involvement, more alcohol-related problems, higher levels of alcohol expectancies, and lower levels of readiness to change their drinking. Gonzalez et al. (2009), studied a sample of college students with a history of at least passive suicidal ideation. They also found that solitary heavy drinkers reported higher levels of alcohol involvement and alcohol-related problems. Further, suicidal ideation (but not depressive symptoms) predicted a higher number of solitary drinking episodes. In an interesting longitudinal study, Tucker et al. (2006), found that solitary drinking in Grade 8 was concurrently associated with several negative academic and social outcomes. Also, solitary drinking in Grade 8 was associated with a) higher odds of alcohol and drug problems and b) lower odds of graduating college 9 years later at age 23 (Bourgault and Demers, 1997). To our knowledge, ours is the first study to show higher levels of solitary drinking as a function of comorbid alcohol dependence and MDE among males. Although this pattern also fits with a negative affect regulation model of alcohol involvement, results from previous work suggest a more complex model. For example, Mohr et al. (2001), used a daily process design and found that participants consumed more alcohol alone on days with more negative social interactions. Using the same sample, Armeli et al. (2003), examined the within-day associations between morning mood, daily negative events, daily alcohol use, and evening mood. They found that, consistent with a stress-response dampening hypothesis, the negative effects of daily stress on some evening moods became weaker as a function of daily drinking. However, the buffering effects of daily drinking were largely limited to drinking with others. For nervous mood, Armeli et al. found that the effect of daily stress on evening nervousness actually increased in magnitude as a function of daily drinking, but only in the case of drinking alone. Drawing on the Attention-Allocation Model (AAM) (Steele and Josephs, 1988; Steele et al., 1986), Armeli et al., suggested that drinking alone (i.e., without the distraction of social interaction) worsens the effects of daily stress. Paradoxically, although solitary drinking is associated with drinking to regulate negative affect (Cooper, 1994), it may intensify the effects of external stressors. One reason may be that solitary drinking allows for rumination about external stressors, and rumination has been shown to exacerbate both depression and alcohol use (Nolen-Hoeksema et al., 2007).
4.2. Alcohol Abuse and MDE
Contrary to predictions, we did not observe greater alcohol involvement among those with alcohol abuse and MDE. In fact, among females with alcohol abuse, MDE was associated with lower frequency of drinking at home alone; among males with alcohol abuse, MDE was associated with lower quantity of daily consumption. Some previous work has documented inverse associations between depressive symptoms and alcohol involvement (Schutte et al., 1995; Windle and Miller, 1990). Males may be more likely to withdraw socially when depressed, which might result in lower consumption (Schutte et al., 1995). However, it is not clear why this pattern was not observed for alcohol dependence. Other results from the NESARC (Grant et al., 2007) and from the NLAES (Hasin and Paykin, 1999) have raised questions about the construct validity of the DSM-IV diagnosis of alcohol abuse. Thus, the current results showing reduced alcohol involvement among those with abuse and MDE should be viewed with caution.
4.3. Limitations
This study had several limitations. DSM-IV diagnoses were based on information from structured interviews conducted by lay interviewers, rather than clinical assessment (Schuckit, 2006). Also, the current study was based on cross-sectional data, and we are not able to discern the temporal order of the associations between C-ALDP and alcohol involvement. Thus, we cannot, for example, rule out the possibility that drinking alone predicted comorbid alcohol dependence and MDE (Helzer et al., 2006). However, as noted earlier, the NESARC included DSM-IV diagnosis of primary MDE excluding substance-induced MDE and MDE due to medical conditions or bereavement, making it less likely that MDE was induced by the more frequent solitary drinking that we observed (Hasin and Grant, 2002; Schuckit, 2006).
Another limitation is that even using a past 12-month time frame, we cannot state that AUD and MDE were occurring at the same time. It is possible, for example, that some percentage of cases may have experienced past 12-month AUD and MDE that were separated by several months (e.g., an episode of AUD lasting 2 months, followed by an 8 month period of no AUD or MDE, followed by an episode of MDE lasting 2 months). Use of a shorter time frame (e.g., past 30 days) would better address this question (Blazer et al., 1994; Regier et al., 1988).
Hasin et al. (2007), showed that the association between past 12-month alcohol dependence and MDD became nonsignificant when sociodemographic and other psychiatric disorders were controlled. We found this same pattern when examining the associations between past 12-month alcohol dependence and MDE, supporting Hasin et al.’s assertion that the relationship between alcohol dependence and depression is due to factors common to both disorders. Although we have focused on C-ALDP, it is clear that other psychiatric disorders have a strong influence on the associations between AUDs and depression.
On a related note, we reported on associations between C-ALDP and alcohol involvement after statistically controlling for several demographic and clinical variables. The inclusion of additional predictors can potentially reduce statistical power (Cohen et al., 2003). Accordingly, we tested all models with and without the inclusion of the demographic and clinical covariates. There were no substantive differences between the two sets of results. Finally, some of the nonsigificant effects we observed deserve comment. Among males with alcohol dependence, MDE was associated with more days of drink driving and drinking twice in the same day. Although nonsignificant, these findings highlight the public health implications of comorbid alcohol dependence and MDE.
4.4. Summary and Conclusions
Using a nationally representative sample, we found that 1) among females and males with past 12-month alcohol abuse and dependence, MDE was associated with higher odds of drinking to enhance mood; and 2) among males with past 12-month alcohol dependence, MDE was associated with a greater number of drinking days at home alone. These results may help us understand why previous research on C-ALDP and alcohol involvement has yielded mixed findings, i.e., C-ALDP appears to be related to a specific pattern of alcohol involvement that differs by sex. Findings also indicated that C-ALDP is associated with solitary drinking, identified in previous research as a correlate of several adverse outcomes. Results suggest that therapeutic efforts aimed at C-ALDP might benefit by focusing on reasons for drinking and reductions in solitary drinking.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
James A. Cranford, Addiction Research Center, Department of Psychiatry, Rachel Upjohn Building, The University of Michigan, 4250 Plymouth Road, Ann Arbor, MI 48109-2700, jcranfor@med.umich.edu, Phone: (734) 232-0215
Susan Nolen-Hoeksema, Yale University.
Robert A. Zucker, The University of Michigan
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Armeli S, Tennen H, Todd M, Carney MA, Mohr CD, Affleck G. A daily process examination of the stress-response dampening effects of alcohol consumption. Psychol Addict Behav. 2003;17:266–276. doi: 10.1037/0893-164X.17.4.266. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151:979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- Bourgault C, Demers A. Solitary drinking: a risk factor for alcohol-related problems? Addiction. 1997;92:303–312. [PubMed] [Google Scholar]
- Cadoret R, Winokur G. Depression in alcoholism. Ann NY Acad Sci. 1974;233:34–39. doi: 10.1111/j.1749-6632.1974.tb40279.x. [DOI] [PubMed] [Google Scholar]
- Christiansen M, Vik PW, Jarchow A. College student heavy drinking in social contexts versus alone. Addict Behav. 2002;27:393–404. doi: 10.1016/s0306-4603(01)00180-0. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Erlbaum; Mahwah, N.J: 2003. [Google Scholar]
- Conner KR, Duberstein PR. Predisposing and precipitiating factors for suicide among alcoholics: empirical review and conceptual integration. Alcohol Clin Exp Res. 2004;28:6S–17S. doi: 10.1097/01.alc.0000127410.84505.2a. [DOI] [PubMed] [Google Scholar]
- Conner KR, Hesselbrock VM, Meldrum SC, Schuckit MA, Bucholz KK, Gamble SA. Transitions to, and correlates of, suicidal ideation, plans, and unplanned and planned suicide attempts among 3,729 men and women with alcohol dependence. J Stud Alcohol Drugs. 2007;68:654–662. doi: 10.15288/jsad.2007.68.654. [DOI] [PubMed] [Google Scholar]
- Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abuse Treat. 2009;37:127–137. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: development and validation of a four-factor model. Psychol Assess. 1994;6:117–128. [Google Scholar]
- Cornelius JR, Maisto SA, Martin CS, Bukstein OG, Salloum IM, Daley DC. Major depression associated with earlier alcohol relapse in treated teens with AUD. Addict Behav. 2004;29:1035–1038. doi: 10.1016/j.addbeh.2004.02.056. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Salloum IM, Mezzich J, Cornelius MD, Fabrega H, Ehler JG. Disproportionate suicidality in patients with comorbid major depression and alcoholism. Am J Psychiatry. 1995;152:358–364. doi: 10.1176/ajp.152.3.358. [DOI] [PubMed] [Google Scholar]
- Daeppen JB, Smith TL, Danko GP, Gordon L, Landi NA, Nurnberger JI. Clinical correlates of cigarette smoking and nicotine dependence in alcohol-dependent men and women. Alcohol Alcohol. 2000;35:171–175. doi: 10.1093/alcalc/35.2.171. [DOI] [PubMed] [Google Scholar]
- Davidson KM, Blackburn IM. Co-morbid depression and drinking outcome in those with alcohol dependence. Alcohol Alcohol. 1998;33:482–487. doi: 10.1093/alcalc/33.5.482. [DOI] [PubMed] [Google Scholar]
- Davis LL, Rush JA, Wisniewski SR, Rice K, Cassano P, Jewell ME, Biggs MM, Shores-Wilson K, Balasabrumani GK, Husain MM, Quitkin FM, McGrath PJ. Substance use disorder comorbidity in major depressive disorder: an exploratory analysis of the Sequenced Treatment Alternatives to Relieve Depression cohort. Compr Psychiatry. 2005;46:81–89. doi: 10.1016/j.comppsych.2004.07.025. [DOI] [PubMed] [Google Scholar]
- Epstein J, Barker P, Vorburger M, Murtha C. DHHS Publication No. SMA 04–3905, Analytic Series A-24. Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, M.D: 2004. Serious Mental Illness and its Co-Occurrence with Substance Use Disorders, 2002. [Google Scholar]
- Gonzales JJ, Insel TR. The conundrum of co-occurring mental and substance use disorders: Opportunities for research. Biol Psychiatry. 2004;56:723–725. doi: 10.1016/j.biopsych.2004.09.007. [DOI] [PubMed] [Google Scholar]
- Gonzalez VM, Collins RL, Bradizza CM. Solitary and social heavy drinking, suicidal ideation, and drinking motives in underage college drinkers. Addict Behav. 2009;34:993–999. doi: 10.1016/j.addbeh.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: results of a national survey. Drug Alcohol Depend. 1995;39:197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Muthen BO, Yi HY, Hasin DS, Stinson FS. DSM-IV alcohol dependence and abuse: further evidence of validity in the general population. Drug Alcohol Depend. 2007;86:154–166. doi: 10.1016/j.drugalcdep.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: 2003. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR. The effect of depression on return to drinking: a prospective study. Arch Gen Psychiatry. 1998;55:259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Hanna EZ, Grant BF. Gender differences in DSM-IV alcohol use disorders and major depression as distributed in the general population: clinical implications. Compr Psychiatry. 1997;38:202–212. doi: 10.1016/s0010-440x(97)90028-6. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Grant BF. Major depression in 6050 former drinkers: association with past alcohol dependence. Arch Gen Psychiatry. 2002;59:794–800. doi: 10.1001/archpsyc.59.9.794. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002;59:375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- Hasin D, Paykin A. Alcohol dependence and abuse diagnoses: concurrent validity in a nationally representative sample. Alcohol Clin Exp Res. 1999;23:144–150. [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Badger GJ, Searles JS, Rose GL, Mongeon JA. Stress and alcohol consumption in heavily drinking men: 2 years of daily data using interactive voice response. Alcohol Clin Exp Res. 2006;30:802–811. doi: 10.1111/j.1530-0277.2006.00093.x. [DOI] [PubMed] [Google Scholar]
- Holland BS, Copenhaver MD. An improved sequentially rejective Bonferroni test procedure. Biometrics. 1987;43:417–423. [Google Scholar]
- Jaccard J. Interaction Effects in Factorial Analysis of Variance. Sage; Thousand Oaks, C.A: 1998. [Google Scholar]
- Jaccard J, Guilamo-Ramos V. Analysis of variance frameworks in clinical child and adolescent psychology: issues and recommendations. J Clin Child Adolesc Psychol. 2002;31:130–146. doi: 10.1207/S15374424JCCP3101_15. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Huang FY, Davies M. Comorbidity between patterns of substance use dependence and psychiatric symptoms. Drug Alcohol Depend. 2001;64:233–241. doi: 10.1016/s0376-8716(01)00126-0. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The epidemiology of dual diagnosis. Biol Psychiatry. 2004;56:730–737. doi: 10.1016/j.biopsych.2004.06.034. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Liu J. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry. 1996;168(Suppl 30):17–30. [PubMed] [Google Scholar]
- Kranzler HR, Del Boca FK, Rounsaville BJ. Comorbid psychiatric diagnosis predicts three-year outcomes in alcoholics: a posttreatment natural history study. J Stud Alcohol. 1996;57:619–626. doi: 10.15288/jsa.1996.57.619. [DOI] [PubMed] [Google Scholar]
- Leonard KE, Eiden RD. Marital and family processes in the context of alcohol use and alcohol disorders. Ann Rev Clin Psychol. 2007;3:285–310. doi: 10.1146/annurev.clinpsy.3.022806.091424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li TK, Hewitt BG, Grant BF. Alcohol use disorders and mood disorders: a National Institute on Alcohol Abuse and Alcoholism Perspective. Biol Psychiatry. 2004;56:718–720. doi: 10.1016/j.biopsych.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Long JS. Regression Models for Categorical and Limited Dependent Variables. Sage; Thousand Oaks, C.A: 1997. [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Auilar-Gaziola S. Comorbidity of substance use disorders with mood and anxiety disorders: results of the international consortium in psychiatric epidemiology. Addict Behav. 1998;23:893–908. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Mohr CD, Armeli S, Tennen H, Carney MA, Affleck G, Hromi A. Daily interpersonal experiences, context, and alcohol consumption: crying in your beer and toasting good times? J Pers Soc Psychol. 2001;80:489–500. doi: 10.1037/0022-3514.80.3.489. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Curr Dir Psychol Sci. 2001;10:173–176. [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clin Psychol Rev. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychol Bull. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. J Abnorm Psychol. 2007;116:198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- O’Brien CP, Charney DS, Lewis L, Cornish JW, Post RM, Woody GE. Priority actions to improve the care of persons with co-occurring substance abuse and other mental disorders: a call to action. Biol Psychiatry. 2004;56:703–713. doi: 10.1016/j.biopsych.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Office of Applied Studies. The NSDUH Report: Co-occurring Major Depressive Episode (MDE) and Alcohol Use Disorder Among Adults. Substance Abuse and Mental Health Services Administration; Rockville, M.D: 2007. Feb 16, [Google Scholar]
- Pettinati HM, Pierce JD, Jr, Wolf AL, Rukstalis MR, O’Brien CP. Gender differences in comorbidly depressed alcohol-dependent outpatients. Alcohol Clin Exp Res. 1997;21:1742–1746. [PubMed] [Google Scholar]
- Preuss UW, Schuckit MA, Smith LT, Danko GP, Buckman K, Bierut L. Comparison of 3190 alcohol-dependent individuals with and without suicide attempts. Alcohol Clin Exp Res. 2002;26:471–477. [PubMed] [Google Scholar]
- Regier DA, Boyd JH, Burke JD, Rae DS. One-month prevalence of mental disorders in the United States: based on five epidemiologic catchment area sites. Arch Gen Psychiatry. 1988;45:977–986. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Research Triangle Institute. Software for Survey Data Analysis (SUDAAN), Version 9.0.0. 2005. [Google Scholar]
- Room R, Babor T, Rehm J. Alcohol and public health. Lancet. 2005;365(9458):519–530. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Arch Gen Psychiatry. 1987;44:505–513. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- Schuckit M, Rimmer J, Reich T, Winokur G. The bender alcoholic. Br J Psychiatry. 1971;119:183–184. doi: 10.1192/bjp.119.549.183. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. The clinical implications of primary diagnostic groups among alcoholics. Arch Gen Psychiatry. 1985;42:1043–1049. doi: 10.1001/archpsyc.1985.01790340021003. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006;101:76–88. doi: 10.1111/j.1360-0443.2006.01592.x. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Danko GP, Bucholz KK, Reich T. Five-year clinical course associated with DSM-IV alcohol abuse or dependence in a large group of men and women. Am J Psychiatry. 2001;158:1084–1090. doi: 10.1176/appi.ajp.158.7.1084. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Tipp JE, Bergman M, Reich W. Comparison of induced and independent major depressive disorders in 2,945 alcoholics. Am J Psychiatry. 1997;154:948–957. doi: 10.1176/ajp.154.7.948. [DOI] [PubMed] [Google Scholar]
- Schutte KK, Moos RH, Brennan PL. Depression and drinking behavior among women and men: a three-wave longitudinal study of older adults. J Consult Clin Psychol. 1995;63:810–822. doi: 10.1037//0022-006x.63.5.810. [DOI] [PubMed] [Google Scholar]
- Steele CM, Josephs RA. Drinking your troubles away II: an attention-allocation model of alcohol’s effect on psychological stress. J Abnorm Psychol. 1988;97:196–205. doi: 10.1037//0021-843x.97.2.196. [DOI] [PubMed] [Google Scholar]
- Steele CM, Southwick L, Pagano R. Drinking your troubles away: the role of activity in mediating alcohol’s reduction of psychological stress. J Abnorm Psychol. 1986;95:173–180. doi: 10.1037//0021-843x.95.2.173. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Report to Congress on the Prevention and Treatment of Co-Occurring Substance Use Disorders and Mental Disorders. U.S. Department of Health and Human Services; Rockville, M.D: 2002. [Google Scholar]
- Sullivan LE, Fiellin DA, O’Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. 2005;118:330–341. doi: 10.1016/j.amjmed.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20:173–189. doi: 10.1016/s0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, Collins RL, Klein DJ. Does solitary substance use increase adolescents’ risk for poor psychosocial and behavioral outcomes? A 9-year longitudinal study comparing solitary and social users. Psychol Addict Behav. 2006;20:363–372. doi: 10.1037/0893-164X.20.4.363. [DOI] [PubMed] [Google Scholar]
- Ustun TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJL. Global burden of depressive disorders in the year 2000. Br J Psychiatry. 2004;184:386–392. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]
- West BT. Statistical and methodological issues in the analysis of complex sample survey data: practical guidance for trauma researchers. J Trauma Stress. 2008;21:440–447. doi: 10.1002/jts.20356. [DOI] [PubMed] [Google Scholar]
- WHO. Mental Health: New Understanding, New Hope. World Health Organization, Geneva; Switzerland: 2001. The World Health Report: 2001. [Google Scholar]
- Windle M, Miller BA. Problem drinking and depression among DWI offenders: a three-wave longitudinal study. J Consult Clin Psychol. 1990;58:166–174. doi: 10.1037//0022-006x.58.2.166. [DOI] [PubMed] [Google Scholar]
- Zucker RA. Alcohol Use and the Alcohol Use Disorders: A Developmental-Biopsychosocial Systems Formulation Covering the Life Course. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology, Vol 3: Risk, Disorder, and Adaptation. 2. John Wiley & Sons, Inc; Hoboken, N.J: 2006. pp. 620–656. [Google Scholar]