Abstract
Numerous studies have examined the structure of the childhood externalizing disorder symptoms of Attention Deficit Hyperactivity Disorder (ADHD), Oppositional Defiant Disorder (ODD), and Conduct Disorder (CD), both separately as well as simultaneously. The present study expanded on previous findings by implementing a multi-level hierarchical approach to investigating the component structure of ADHD, ODD, and CD criteria in 487 14-year-old boys from the Minnesota Twin Family Study (MTFS). We found support for a hierarchical conceptualization of externalizing behavior criteria in early adolescent boys by specifying how one-, two-, three-, four-, five- and six-factor models of externalizing criteria can be integrated. These results suggest that it may be more beneficial to conceptualize different levels of this hierarchy as relevant to different issues in case conceptualization and research design, from the broad level of an overall externalizing spectrum, to the level of finer-grained subtypes within specific disorders.
Keywords: ADHD, ODD, CD, principle components, hierarchical modeling
1. Introduction
Findings from epidemiological studies consistently demonstrate high rates of co-occurrence among childhood and adolescent “externalizing” disorders, including attention-deficit hyperactivity disorder (ADHD; a continuing pattern of inattention and/or hyperactivity-impulsivity), oppositional defiant disorder (ODD; negativistic, defiant, disobedient, and hostile behavior directed at authority figures), and conduct disorder (CD; a continuing pattern of behavior resulting in the violation of the basic rights of others; Fergusson et al., 1993; Lahey and Loeber, 1997; and Ford et al., 2003). These externalizing disorders affect a substantial number of children, and account for more than half of the childhood referrals to mental health clinics (Robins, 1991; Fergusson and Horwood, 1995; Kazdin, 1995; Frick, 1998; Loeber et al., 2000; Costello et al., 2003; Frick and Kimonis, 2005; and Polanczyk et al., 2007). To better understand these distressing and socially-burdening disorders, numerous studies have examined the underlying structure of ADHD, ODD and CD through both exploratory and confirmatory factor analyses (Bauermeister et al., 1992a; Bauermeister, 1992b; Pelham et al., 1992; Frick et al., 1993; Lahey and Loeber, 1994; Molina et al., 2001; Hommerson et al., 2006; Lahey et al., 2008; and Farmer et al., 2009).
Previous studies that have examined externalizing disorders including ADHD, ODD, and CD symptoms and criteria have yielded valuable results (Lahey et al., 2008; and Farmer et al., 2009); however, these studies have not investigated the structure of the symptomatology of these childhood externalizing disorders simultaneously in the context of a hierarchical approach that allows for the integration of both broad and specific components of these disorders into a single model. The benefit of a hierarchical model of these externalizing disorders is that it would allow for multiple levels of generality and specificity along a continuum, ranging from broader factors to more fine-grained criterion clusters. This type of hierarchy has the potential to reconcile both “lumping” and “splitting”; the broader components would be what these disorders have in common, and the more refined components (at the lower levels of the hierarchy) would be comprised of more specific symptom or criterion clusters.
We next present a hierarchical approach to examining externalizing behaviors and how it may be useful in conceptualizing the structure of childhood externalizing problems, from the broad level of an overall externalizing spectrum to the level of finer-grained subtypes within specific disorders. To provide a context for the current research, we begin with a brief summary of the existing literature on the structure of these disorders, when considered both individually and jointly.
1.1 Attention Deficit Hyperactivity Disorder (ADHD)
Previous studies examining the structure of DSM-IV criteria of ADHD generally characterize it as consisting of two dimensions: ‘Inattention’ and ‘Hyperactivity/Impulsivity’. Several studies examining DSM-IV criteria of ADHD, as well as measures of more general disruptive behaviors, using multiple rater reports, have found support for a two-factor structure of ADHD symptoms in both community and clinic-referred samples of children (DuPaul, 1991; Pelham et al., 1992; Bauermeister et al., 1992a; Lahey and Loeber, 1994; Bauermeister et al., 1995; Burns et al., 1997a; 1997b; DuPaul et al., 1997, 1998; Pillow et al., 1998; Beiser et al., 2000; and Molina et al., 2001).
1.2 Conduct Disorder (CD) and Oppositional Defiant Disorder (ODD)
A number of studies in the literature simultaneously focus on CD and ODD. As a result, studies focusing on the structure of CD and ODD symptoms in children generally find evidence for a two-dimensional structure of these criteria, consisting of ‘aggressiveness’ and ‘delinquency/rule-breaking’ (Frick et al., 1993; Loeber et al., 1991; Burns et al., 1997a, 1997b; Burns and Patterson, 2000). Studies examining the structure of DSM-IV criteria of CD alone demonstrate that this same two-dimensional structure also characterizes CD symptoms best (Frick et al., 1993; Moffitt and Caspi, 2001; Tackett et al., 2003; Maughan et al., 2004). For example, Tackett and colleagues (2003) examined DSM-IV criteria of CD in a sample of 6- to 17-year-old Australian boys, and found that symptoms of CD loaded onto two sub-factors: a first factor encompassing overt aggressive behaviors such as, “initiating physical fights,” and a second factor made up of more covert rule-breaking or delinquent behaviors such as, “stealing without confrontation” (Tackett et al., 2003). (Empirical evidence for CD subtypes mirroring the DSM-IV defined symptom clusters of CD, i.e. aggression to people and animals, deceitfulness or theft, and serious violations of rules, is limited, e.g. Nock et al., 2006; Janson and Kjelsberg, 2006.) In contrast to the two-dimensional structure found for CD symptoms, studies examining criteria for ODD alone have generally found its symptoms to fall under a single factor of oppositional behavior (Hommerson et al., 2006).
Despite the consistent finding of a two-factor model of CD and ODD symptoms in school-aged children and adolescents, other studies primarily conducted with pre-school-aged children have yielded a single factor of aggressive and oppositional behavior when examining a combination of CD and ODD symptoms (McDermott, 1982; Doke and Flippo, 1983; Achenbach et al., 1987). As a result, some researchers have questioned the utility of conceptualizing aggressive and rule-breaking behaviors, such as those embodied in ODD and CD symptoms, as being multidimensional (Achenbach and Edelbrock, 1978; Dreger, 1981; Garber, 1984; Loeber et al., 1991; Frick and Kimonis, 2008). Thus, a closer examination of these symptoms during early adolescence is warranted.
1.3 Studies examining a combination of ADHD and ODD/CD criteria
Recent studies have also examined a combination of ADHD, CD and ODD criteria using confirmatory factor analyses (Lahey et al., 2008; Farmer et al., 2009) and have generally found factors that encompass inattention, impulsivity-hyperactivity, and oppositional problems. Oppositional problems were in turn comprised of two sub-factors including aggressive and rule-breaking symptoms (Achenbach and Edelbrock, 1978; Quay, 1986; Pelham et al., 1992; Burns et al., 1997a; 2001; Conners et al., 1998; Burns and Patterson, 2000; Molina et al., 2001; Zuddas et al., 2006). These studies not only demonstrated that a two-factor solution for ADHD symptoms was the most optimal, but they provided evidence for a potential distinction between ODD and CD constructs (Pelham et al., 1992; Burns et al., 1997a; Molina et al., 2001; Zuddas et al., 2006).
1.4 Synthesizing Models Using a Hierarchical Approach
While there has been extensive psychometric research conducted on the underlying factor structures of ADHD, ODD, and CD, previous research has focused predominantly on separate aspects of the factor structures of these disorders. The goal of the current work was to articulate a hierarchical model that ties together previous research, which focused either on specific disorders, or specific factors of specific disorders. With this goal in mind, we implemented a hierarchical approach articulated by Goldberg (2006). We used this approach to extract principal components connecting DSM-IV criteria of ADHD, ODD, and CD (going from the broadest single component to the most refined interpretable set of multiple components). The extracted components were varimax rotated such that each component was orthogonal to the preceding one, and the extracted components were saved as regression component scores (Goldberg, 2006). These scores were then correlated between different levels of the hierarchy, to illustrate how components are related to each other between adjacent levels (e.g., moving from level 2 to level 3).
Additionally, this model allows for varying degrees in breadth versus specificity of the components within the spectrum (at different levels of the hierarchy). For example, there may be specific factors that influence (and are shared among) all three disorders, which make up the broadest first component because, by definition, it accounts for the most variance among all criteria. Yet this model also allows for differences among specific disorders to be expressed through subsequently extracted components, at the lower levels of the hierarchy. In this way, at the higher levels of the hierarchy, components are more general and broad, while elements at the hierarchy’s lower levels are more specific and refined (such as specific disorder subtypes). This conceptualization may be helpful in identifying and targeting prevention and treatment methods specific to certain sets of symptoms within each component as well as more general behaviors.
The purpose of the current study was to contribute to the existing literature on early adolescent externalizing behaviors by examining the hierarchical structure of ADHD, ODD, and CD criteria in 14-year-old boys. The advantage of using this approach was two-fold. First, while previous studies have focused on different aspects of the structures of ADHD, ODD and CD, the current study combined the component structure of these disorders into a single model. Second, in a hierarchical-spectrum model, distinct clusters of criteria aggregate to form specific disorders, which in turn come together to form broader representations of a disorder. This allows for comparisons that can be described at different levels, on a continuum ranging from very narrow or specific to very general or broad. This may be beneficial because a hierarchical structure can be used to frame clinical and research conceptualization. For example, Weiss, Susser, and Catron (1998) suggested that features that are common across childhood psychopathology manifestations may be related to severity, while specific features may be related to differentiation of psychopathology. The current study is the first of which we are aware to examine the structure of these three DSM-IV childhood externalizing disorders simultaneously while implementing a hierarchical approach to investigating the dimensional structure of these symptoms.
2. Method
2.1 Participants
The present sample consisted of 487 individual 14-year-old boys participating in an ongoing longitudinal study, the Minnesota Twin Family Study (MTFS). These boys were part of an MTFS initiative known as the Enrichment Study (ES), which aimed to recruit twins at high risk for the development of childhood disruptive disorders and substance abuse. This sample was identified from the Minnesota birth records of same-sex twin pairs born between 1988 and 1994, and was ethnically representative of the Minnesota area (91% Caucasian). Of the twin pairs targeted for inclusion, 82% were successfully recruited to participate starting when the twins were 11 years of age. The present study included the boys of the ES sample, since boys are disproportionately affected by these externalizing symptoms and criteria (Crick, 2003; Maughan et al., 2004; Waschbusch and King, 2006). The mean age of the ES boys at intake was approximately 11 years of age, while children at follow-up were approximately 14-years-old.
The purpose of utilizing the ES sample for the current project was to ensure acceptable variance on disruptive behavior symptoms and criteria by over-sampling for problematic behaviors, but also to ensure the representativeness of the sample by appropriately weighting the sample. (Additionally, the ES sample was utilized for the current project in order to examine DSM-IV criteria; assessment of the original MTFS twin sample was begun prior to the release of DSM-IV criteria.) Since the ES sample was over-sampled for twins likely to have or develop ADHD and/or CD, a weighting scheme was utilized to account for non-random sampling in the analyses of these data. For further details regarding the ES recruitment, weighting scheme, and sample statistics, please see Keyes et al. (2009).
2.2 Measures and assessments
To obtain lifetime assessments of ADHD, ODD and CD criteria through age 14, we combined information obtained from assessments when the twins were 11- and 14-years-old. Assessments at age 11 (intake) inquired about symptoms and criteria that had ever been present, while assessments at 14 years of age (the first follow-up) inquired about criteria since the intake (age 11) assessment.
During day-long laboratory visits, each caregiver and twin was interviewed separately by trained interviewers. Child and caregiver reports of DSM-IV ADHD, ODD, and CD criteria for each child were obtained through a modified version of the Diagnostic Interview for Children and Adolescents – Revised (DICA-R; Reich and Welner, 1988). The presence or absence of each DSM-IV symptom/criterion was determined by consensus teams of at least two advanced clinical psychology doctoral students. Consensus teams were blind to participant identity, and different teams reviewed interviews of different family members to avoid contamination. Reliability (kappa) of the consensus diagnoses was high, exceeding 0.73 for all disorders. A best-estimate procedure was implemented where a symptom/criterion was considered to be present if either the caregiver or child ever reported it as present. That is, criteria were counted as being present if either the caregiver or child definitely endorsed them, either through age 11 or between the 11-year-old and 14-year-old assessments.
Weighted prevalence rates of all DSM-IV ADHD, ODD, and CD criteria for the current ES sample are provided in Table 1, and are comparable to those found in other community samples (e.g., Costello et al., 2003; Polanczyk et al., 2007). Two CD symptoms/criteria (‘ran away for a lengthy period’; and ‘stolen with confrontation’) were excluded from the present analyses due to prevalence rates below 0.5% (after combining caregiver and child self-reports). The CD criterion ‘forced sex’ was not assessed in this sample. Additionally, the number of total ADHD, CD, and ODD cases at age 11 (for boys in the ES sample) were N = 88, N = 130; and N = 92 for ADHD, CD, and ODD, respectively (see Keyes et al. 2009 for further details).
Table 1.
MTFS Enrichment Sample weighted prevalence rates for forty-three ADHD, ODD, and CD criteria in 14-year-old males (N = 478) based on combined caregiver and child self-reports.
| DSM-IV criteria | Prevalence |
|---|---|
| Attention Deficit Hyperactivity Disorder | |
| A 1. ADHD Inattention | |
| a. Makes careless mistakes | 42.4% |
| b. Difficulty sustaining attention | 32.8% |
| c. Often does not seem to listen | 21.3% |
| d. Difficulty following through on instructions | 25.1% |
| e. Difficulty organizing tasks | 34.9% |
| f. Avoids mental effort | 23.2% |
| g. Often loses necessary items | 26.8% |
| h. Often easily distracted | 48.0% |
| i. Often forgetful | 35.9% |
| 2. ADHD Hyperactivity/Impulsivity | |
| Hyperactivity | |
| a. Often fidgets or squirms | 37.2% |
| b. Difficulty remaining seated | 24.6% |
| c. Inappropriate running about | 12.3% |
| d. Difficulty playing quietly | 19.8% |
| e. Often “on the go” | 21.2% |
| f. Often talks excessively | 25.5% |
| Impulsivity | |
| g. Often blurts out answers | 16.2% |
| h. Difficulty awaiting turn | 9.3% |
| i. Often interrupts or intrudes | 20.0% |
| B. Onset before age 7 | 61.3% |
| Impairment: multiple settings | 50.7% |
| Oppositional Defiant Disorder | |
| 1. Often loses temper | 29.9% |
| 2. Often argues with adults | 21.7% |
| 3. Defies adults’ requests | 15.8% |
| 4. Deliberately annoys people | 31.5% |
| 5. Blames others for mistakes | 32.4% |
| 6. Touchy/easily annoyed by others | 16.3% |
| 7. Often angry and resentful | 12.6% |
| 8. Often spiteful and vindictive | 6.9% |
| Impairment: multiple settings | 37.1% |
| Duration of 6 months or more | 64.7% |
| Conduct Disorder | |
| 1. Often bullies, threatens, or intimidates | 3.6% |
| 2. Often initiates physical fights | 7.9% |
| 3. Used a weapon with potential for harm | 14.6% |
| 4. Cruel to people | 4.6% |
| 5. Cruel to animals | 10.8% |
| 6. Sets fires to cause damage | 4.6% |
| 7. Deliberately destroyed property | 7.9% |
| 8. Broken into house, car, building | 0.7% |
| 9. Lies to con others | 26.9% |
| 10. Stolen nontrivial items | 6.2% |
| 11. Stays out late before age 13 | 2.0% |
| 12. Truant before 13 | 0.8% |
| 13. Impairment – multiple settings | 22.7% |
Note: Prevalence rates are based on number of definite criteria.
2.3 Data Analysis
To examine the hierarchical structure of early adolescent externalizing behavior disorders, ADHD, ODD, and CD criteria (43 total) were subjected to criterion-level principal components analysis using varimax rotation in SPSS 15.0. The procedure implemented in the current study has been described in detail by Goldberg (2006) and Tackett, Krueger, Iacono, and McGue (2008). Briefly, we used a top-down approach to model successive levels of the component hierarchy characterizing criteria of adolescent externalizing behavior disorders. This approach began with extraction of the first unrotated principal component (FUPC, which is the largest possible component) from the DSM-IV ADHD, ODD, and CD criteria. That component was then represented as a regression-based component score. In the second step, two varimax-rotated principal components were extracted and those scores were saved as component scores. This procedure continued, extracting greater numbers of components and saving the resulting component scores, until a component emerged on which no criterion has its highest loading (Goldberg, 2006), which in this report occurred with the seven component solution. Thus, for each successive number of components the factor scores are computed and saved – one can then intercorrelate the total set of factor scores or components. Correlations between the factor or component scores at each level with those at the level below it can then be used to construct a hierarchical representation (with broader levels on top and more refined components on the bottom). The FUPC accounts for a significant portion of the disorder co-variation, while all subsequent factors account for smaller, but independent factors, which contribute to the total variance. The first principal component provides a measure of variance that is common to all variables (in this case, symptoms) that have been included in these analyses, and each subsequent component is again as large as possible after the influence of all preceding factors or components have been partialed out (Goldberg, 2006). This approach allowed for the development and integration of hierarchical representations of the structure of ADHD, ODD and CD criteria.
3. Results
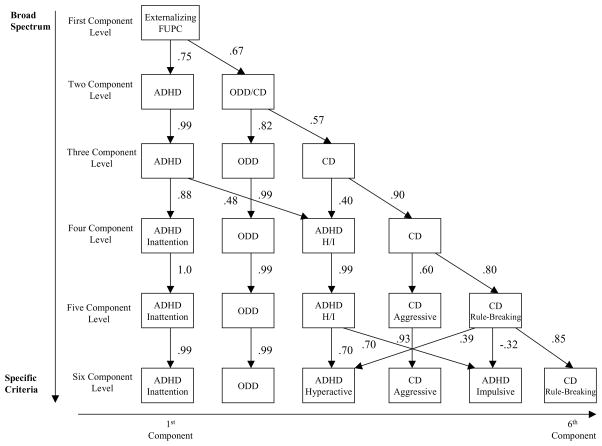
Criterion-level principal component analyses were conducted on a total of 43 ADHD, ODD, and CD criteria in 487 adolescent twin boys from the MTFS Enrichment Sample. We present and discuss specific results at each level of the component hierarchy below. Principal component loadings for each level of the hierarchy are presented in Tables 2 through 7 (that is, Table 2 presents the component loadings for the first component level, Table 3 for the two-component level, up to the final six-component level which is presented in Table 7). Component loadings greater than or equal to 0.30 are in bold. Each component (along with its primary loadings) in the tables is identified by a separate color. Each criterion was assigned to the component on which it had its greatest loading (if that met or exceeded 0.30), and was colored to match said component to illustrate this assignment. If a criterion had no loadings of at least 0.30 on any component, it was not assigned to any component. Figure 1 illustrates the hierarchical nature of all estimated component levels, and indicates with arrows the significant correlations between components across levels.
Table 2.
Principal Component Loadings for the One-Component Level
| Component 1 | |
|---|---|
| Attention Deficit Hyperactivity Disorder | |
| A 1. ADHD Inattention | |
| a. Makes careless mistakes | 0.53 |
| b. Difficulty sustaining attention | 0.56 |
| c. Often does not seem to listen | 0.51 |
| d. Difficulty following through on instructions | 0.48 |
| e. Difficulty organizing tasks | 0.57 |
| f. Avoids mental effort | 0.61 |
| g. Often loses necessary items | 0.47 |
| h. Often easily distracted | 0.56 |
| i. Often forgetful | 0.62 |
| 2. ADHD Hyperactivity/Impulsivity | |
| Hyperactivity | |
| a. Often fidgets or squirms | 0.49 |
| b. Difficulty remaining seated | 0.51 |
| c. Inappropriate running about | 0.51 |
| d. Difficulty playing quietly | 0.43 |
| e. Often “on the go” | 0.52 |
| f. Often talks excessively | 0.39 |
| Impulsivity | |
| g. Often blurts out answers | 0.48 |
| h. Difficulty awaiting turn | 0.54 |
| i. Often interrupts or intrudes | 0.51 |
| B. Onset before age 7 | 0.52 |
| Impairment: multiple settings | 0.70 |
| Oppositional Defiant Disorder | |
| 1. Often loses temper | 0.57 |
| 2. Often argues with adults | 0.59 |
| 3. Defies adults’ requests | 0.47 |
| 4. Deliberately annoys people | 0.45 |
| 5. Blames others for mistakes | 0.47 |
| 6. Touchy/easily annoyed by others | 0.54 |
| 7. Often angry and resentful | 0.51 |
| 8. Often spiteful and vindictive | 0.40 |
| Impairment: multiple settings | 0.69 |
| Duration of 6 months or more | 0.60 |
| Conduct Disorder | |
| 1. Often bullies, threatens, or intimidates | 0.37 |
| 2. Often initiates physical fights | 0.36 |
| 3. Used a weapon with potential for harm | 0.42 |
| 4. Cruel to people | 0.36 |
| 5. Cruel to animals | 0.26 |
| 6. Sets fires to cause damage | 0.39 |
| 7. Deliberately destroyed property | 0.41 |
| 8. Broken into house, car, building | 0.16 |
| 9. Lies to con others | 0.54 |
| 10. Stolen nontrivial items | 0.36 |
| 11. Stays out late before age 13 | 0.20 |
| 12. Truant before 13 | 0.18 |
| 13. Impairment – multiple settings | 0.64 |
Table 7.
Principal Component Loadings for the Six-Component Level
| Component 1 | Component 2 | Component 3 | Component 4 | Component 5 | Component 6 | |
|---|---|---|---|---|---|---|
| Attention Deficit Hyperactivity Disorder | ||||||
| A 1. ADHD Inattention | ||||||
| a. Makes careless mistakes | 0.41 | 0.14 | 0.53 | 0.09 | −0.09 | 0.08 |
| b. Difficulty sustaining attention | 0.64 | 0.19 | 0.11 | −0.05 | 0.15 | 0.14 |
| c. Often does not seem to listen | 0.60 | 0.04 | 0.11 | 0.07 | 0.27 | 0.04 |
| d. Difficulty following through on instructions | 0.47 | −0.01 | 0.13 | 0.22 | 0.32 | 0.01 |
| e. Difficulty organizing tasks | 0.71 | 0.15 | 0.14 | 0.11 | 0.03 | 0.02 |
| f. Avoids mental effort | 0.53 | 0.18 | 0.23 | 0.13 | 0.16 | 0.18 |
| g. Often loses necessary items | 0.69 | 0.11 | 0.04 | 0.15 | −0.01 | −0.14 |
| h. Often easily distracted | 0.60 | 0.18 | 0.26 | −0.05 | 0.04 | 0.14 |
| i. Often forgetful | 0.74 | 0.19 | 0.07 | 0.10 | 0.10 | 0.10 |
| 2. ADHD Hyperactivity/Impulsivity | ||||||
| Hyperactivity | ||||||
| a. Often fidgets or squirms | 0.27 | 0.08 | 0.61 | 0.04 | 0.06 | 0.10 |
| b. Difficulty remaining seated | 0.21 | 0.07 | 0.59 | −0.01 | 0.24 | 0.23 |
| c. Inappropriate running about | 0.15 | 0.18 | 0.55 | 0.31 | 0.08 | −0.06 |
| d. Difficulty playing quietly | 0.08 | 0.07 | 0.32 | 0.22 | 0.47 | −0.01 |
| e. Often “on the go” | 0.18 | 0.11 | 0.61 | 0.03 | 0.28 | 0.08 |
| f. Often talks excessively | 0.10 | 0.16 | 0.12 | 0.02 | 0.64 | −0.03 |
| Impulsivity | ||||||
| g. Often blurts out answers | 0.14 | 0.21 | 0.21 | 0.01 | 0.63 | 0.02 |
| h. Difficulty awaiting turn | 0.09 | 0.19 | 0.55 | 0.16 | 0.37 | −0.01 |
| i. Often interrupts or intrudes | 0.26 | 0.23 | 0.14 | 0.04 | 0.59 | −0.05 |
| B. Onset before age 7 | 0.47 | 0.01 | 0.43 | 0.08 | 0.21 | −0.06 |
| Impairment: multiple settings | 0.71 | 0.21 | 0.33 | 0.09 | 0.08 | 0.04 |
| Oppositional Defiant Disorder | ||||||
| 1. Often loses temper | 0.30 | 0.56 | 0.01 | 0.24 | 0.08 | −0.01 |
| 2. Often argues with adults | 0.15 | 0.68 | 0.03 | 0.15 | 0.22 | 0.10 |
| 3. Defies adults’ requests | 0.10 | 0.60 | 0.05 | 0.09 | 0.06 | 0.14 |
| 4. Deliberately annoys people | −0.01 | 0.66 | 0.17 | −0.03 | 0.03 | 0.15 |
| 5. Blames others for mistakes | 0.02 | 0.57 | 0.24 | 0.02 | 0.15 | 0.02 |
| 6. Touchy/easily annoyed by others | 0.32 | 0.51 | −0.10 | 0.16 | 0.12 | 0.17 |
| 7. Often angry and resentful | 0.15 | 0.48 | 0.07 | 0.29 | 0.07 | 0.15 |
| 8. Often spiteful and vindictive | 0.05 | 0.30 | 0.15 | 0.31 | 0.09 | 0.13 |
| Impairment: multiple settings | 0.21 | 0.84 | 0.07 | 0.18 | 0.13 | 0.01 |
| Duration of 6 months or more | 0.23 | 0.78 | 0.11 | −0.02 | 0.06 | −0.02 |
| Conduct Disorder | ||||||
| 1. Often bullies, threatens, or intimidates | 0.08 | 0.11 | 0.10 | 0.39 | 0.07 | 0.41 |
| 2. Often initiates physical fights | 0.09 | 0.09 | 0.02 | 0.64 | 0.12 | 0.02 |
| 3. Used a weapon with potential for harm | −0.02 | 0.32 | 0.13 | 0.47 | 0.07 | 0.14 |
| 4. Cruel to people | 0.16 | 0.03 | 0.03 | 0.69 | 0.03 | 0.06 |
| 5. Cruel to animals | 0.08 | −0.02 | −0.00 | 0.24 | 0.35 | 0.21 |
| 6. Sets fires to cause damage | 0.10 | 0.11 | 0.06 | 0.11 | 0.39 | 0.42 |
| 7. Deliberately destroyed property | 0.07 | 0.24 | 0.11 | 0.33 | 0.03 | 0.39 |
| 8. Broken into house, car, building | 0.03 | 0.01 | 0.05 | −0.00 | −0.07 | 0.66 |
| 9. Lies to con others | 0.16 | 0.36 | 0.31 | 0.32 | 0.06 | 0.06 |
| 10. Stolen nontrivial items | 0.09 | 0.10 | 0.27 | 0.22 | −0.05 | 0.46 |
| 11. Stays out late before age 13 | 0.05 | 0.12 | −0.08 | −0.00 | 0.20 | 0.38 |
| 12. Truant before 13 | −0.01 | 0.08 | 0.04 | 0.09 | −0.07 | 0.58 |
| 13. Impairment – multiple settings | 0.15 | 0.32 | 0.29 | 0.56 | 0.10 | 0.27 |
Table 3.
Principal Component Loadings for the Two-Component-Level
| Component 1 | Component 2 | |
|---|---|---|
| Attention Deficit Hyperactivity Disorder | ||
| A 1. ADHD Inattention | ||
| a. Fails to give close attention, makes careless mistakes | 0.57 | 0.17 |
| b. Difficulty sustaining attention | 0.62 | 0.15 |
| c. Often does not seem to listen | 0.63 | 0.07 |
| d. Difficulty following through on instructions | 0.55 | 0.10 |
| e. Difficulty organizing tasks | 0.65 | 0.13 |
| f. Avoids mental effort | 0.59 | 0.26 |
| g. Often loses necessary items | 0.58 | 0.05 |
| h. Often easily distracted | 0.62 | 0.15 |
| i. Often forgetful | 0.66 | 0.19 |
| 2. ADHD Hyperactivity/Impulsivity | ||
| Hyperactivity | ||
| a. Often fidgets or squirms | 0.54 | 0.14 |
| b. Difficulty remaining seated | 0.53 | 0.18 |
| c. Inappropriate running about | 0.43 | 0.29 |
| d. Difficulty playing quietly | 0.38 | 0.22 |
| e. Often “on the go” | 0.52 | 0.19 |
| f. Often talks excessively | 0.34 | 0.21 |
| Impulsivity | ||
| g. Often blurts out answers | 0.41 | 0.26 |
| h. Difficulty awaiting turn | 0.46 | 0.30 |
| i. Often interrupts or intrudes | 0.46 | 0.25 |
| B. Onset before age 7 | 0.66 | 0.04 |
| Impairment: multiple settings | 0.76 | 0.19 |
| Oppositional Defiant Disorder | ||
| 1. Often loses temper | 0.28 | 0.54 |
| 2. Often argues with adults | 0.20 | 0.67 |
| 2. Defies adults’ requests | 0.11 | 0.58 |
| 3. Deliberately annoys people | 0.07 | 0.60 |
| 4. Blames others for mistakes | 0.17 | 0.52 |
| 5. Touchy/easily annoyed by others | 0.25 | 0.53 |
| 6. Often angry and resentful | 0.18 | 0.57 |
| 7. Often spiteful and vindictive | 0.15 | 0.44 |
| Impairment: multiple settings | 0.23 | 0.78 |
| Duration of 6 months or more | 0.25 | 0.62 |
| Conduct Disorder | ||
| 1. Often bullies, threatens, or intimidates | 0.14 | 0.41 |
| 2. Often initiates physical fights | 0.15 | 0.37 |
| 3. Used a weapon with potential for harm | 0.09 | 0.53 |
| 4. Cruel to people | 0.18 | 0.33 |
| 5. Cruel to animals | 0.18 | 0.19 |
| 6. Sets fires to cause damage | 0.23 | 0.33 |
| 7. Deliberately destroyed property | 0.12 | 0.48 |
| 8. Broken into house, car, building | 0.01 | 0.22 |
| 8. Lies to con others | 0.31 | 0.47 |
| 9. Stolen nontrivial items | 0.19 | 0.34 |
| 10. Stays out late before age 13 | 0.05 | 0.24 |
| 11. Truant before 13 | −0.02 | 0.30 |
| 12. Impairment – multiple settings | 0.31 | 0.61 |
Figure 1.
Principal components of lifetime DSM-IV ADHD, ODD, and CD criteria in a sample of 14-year-old boys, organized in a single hierarchical model. All correlations between components are significant at p<.001, and only correlation coefficients greater than 0.30 are presented on the diagram. FUPC = First Unrotated Principal Component.
Briefly, the first component level illustrated in Figure 1 depicts the broadest component encompassing (and capturing 24% of the variance in) all ADHD, ODD, and CD symptom criteria. Subsequent levels provide more specificity in the separate clustering of ADHD, ODD, and CD symptoms, with the second through sixth component levels uniquely explaining approximately 7%, 5%, 4%, 3%, and 3% of the symptom variance, respectively. Notably, the third component level displays a near perfect correspondence in ADHD, ODD and CD symptoms, respectively, while the fourth component level captures the separate clustering of ADHD Inattentive and Hyperactive-Impulsive symptoms. The fifth and sixth component levels provide even greater specificity in the separation of CD and ADHD Impulsive and Hyperactive symptoms. We now turn to considering the interpretation of each component level in greater detail.
3.1 First Component Level
The first level of the hierarchy presented in Figure 1 was the first unrotated principal component (FUPC) obtained, and it explained 24.23% of the total variance among all criteria. At this component level, all criteria have positive but highly variable loadings ranging from 0.16 to 0.70 (see Table 2). This first component represents the broad externalizing propensity that ties together the DSM-IV ADHD, ODD, and CD criteria. Nevertheless, the variable magnitude of the loadings on this general propensity points to the likelihood of finer-grained distinctions that would be predicted to emerge at lower levels of an overall hierarchy.
3.2 Two-Component Level
At the two-component level, we see a break in the general cluster of externalizing criteria into two separate clusters of ADHD and ODD/CD criteria. The first cluster of criteria was comprised of all ADHD criteria, with loadings ranging from 0.34 to 0.76, as shown in red in Table 3. Within this second level of the hierarchy, ODD and CD criteria clustered together and loaded strongly onto a single component comprised of both ODD and CD criteria (with loadings ranging from 0.30 to 0.78, shown in blue, Table 3), with no CD or ODD criteria loading most strongly onto the ADHD component (Table 3). This illustrates a stronger empirical connection between the constructs and criteria of ODD and CD, by contrast with the connection between either of these constructs and ADHD. Additionally, three CD criteria “cruel to animals”, ‘broken into house, car, or building”, and “stays out late before age 13” did not strongly load onto either component of criteria (with loadings less than or equal to 0.24).
The ADHD component correlated r = 0.75, p<0.001 with the broader externalizing propensity (the FUPC), and the ODD/CD component correlated r = 0.67, p<0.001 with the FUPC. These correlations demonstrate the hierarchical nature of the first two levels presented in Figure 1. That is, each of the two components accounts for a proportion of the variance in the FUPC. The ADHD component accounts for 56% of the variance in the FUPC (0.75 squared) and the ODD/CD component accounts for the remaining 44% of the variance in the FUPC (0.67 squared). With regard to the total variance in all criteria, the two-component level captured an additional 6.59% of the total variance, beyond the 24.23% accounted for by the FUPC. Thus, the first and second components cumulatively captured 30.82% of the total variance.
3.3 Three-Component Level
At the three-component level, the three components roughly corresponded to the three disorders (ADHD, ODD, and CD), and uniquely captured 4.85% of the total variance (thus, the three preceding component levels cumulatively captured 35.67% of the total variance). The first component encompassed all ADHD criteria, with strong loadings ranging from 0.32 to 0.76 (shown in red, see Table 4) and showing a perfect correspondence of ADHD criteria from level two to level three, with a correlation of r = 0.99, p<0.001. The second component included ODD criteria (with loadings ranging from 0.49 to 0.85; shown in blue, see Table 4). The third component was comprised of CD criteria (with loadings ranging from 0.33 to 0.62; shown in green in Table 4). One DSM-IV ODD criterion, “often spiteful and vindictive,” loaded onto both the second (ODD) cluster (with a loading of 0.30) and third (CD) cluster (with a loading of 0.35). Similarly, one CD criterion, “lies to con others,” loaded most highly on the second (ODD) component with a loading of 0.35 (and a loading of 0.34 on the CD component). The CD criterion “stays out late before age 13” did not strongly load onto any of the components (with loadings of 0.03, 0.13, and 0.24 on the ADHD, ODD, and CD components, respectively). Both the ODD and the CD component clusters correlated highly with the broader ODD/CD factor found at the two-component level (r = 0.82, p<0.001; and r = 0.57, p<0.001, respectively), but were essentially uncorrelated with the broader ADHD component from the previous two-component level (r = 0.005, p = 0.915; r = 0.09, p = 0.05 for ODD and CD, respectively). At this level of the hierarchy, ODD and CD criteria were correlated but separable constructs, further illustrating hierarchy.
Table 4.
Principal Components Loadings for the Three Component Level
| Component 1 | Component 2 | Component 3 | |
|---|---|---|---|
| Attention Deficit Hyperactivity Disorder | |||
| A 1. ADHD Inattention | |||
| a. Makes careless mistakes | 0.55 | 0.10 | 0.20 |
| b. Difficulty sustaining attention | 0.62 | 0.23 | 0.00 |
| c. Often does not seem to listen | 0.63 | 0.10 | 0.04 |
| d. Difficulty following through on instructions | 0.54 | 0.05 | 0.16 |
| e. Difficulty organizing tasks | 0.66 | 0.21 | −0.01 |
| f. Avoids mental effort | 0.58 | 0.21 | 0.20 |
| g. Often loses necessary items | 0.60 | 0.19 | −0.12 |
| h. Often easily distracted | 0.62 | 0.20 | 0.04 |
| i. Often forgetful | 0.66 | 0.27 | 0.02 |
| 2. ADHD Hyperactivity/Impulsivity | |||
| Hyperactivity | |||
| a. Often fidgets or squirms | 0.51 | 0.01 | 0.28 |
| b. Difficulty remaining seated | 0.49 | −0.01 | 0.37 |
| c. Inappropriate running about | 0.40 | 0.13 | 0.36 |
| d. Difficulty playing quietly | 0.35 | 0.06 | 0.34 |
| e. Often “on the go” | 0.50 | 0.03 | 0.33 |
| f. Often talks excessively | 0.32 | 0.17 | 0.16 |
| Impulsivity | |||
| g. Often blurts out answers | 0.39 | 0.20 | 0.21 |
| h. Difficulty awaiting turn | 0.43 | 0.13 | 0.37 |
| i. Often interrupts or intrudes | 0.45 | 0.25 | 0.13 |
| B. Onset before age 7 | 0.65 | 0.00 | 0.12 |
| Impairment: multiple settings | 0.76 | 0.23 | 0.08 |
| Oppositional Defiant Disorder | |||
| 1. Often loses temper | 0.26 | 0.60 | 0.12 |
| 2. Often argues with adults | 0.18 | 0.69 | 0.20 |
| 3. Defies adults’ requests | 0.09 | 0.60 | 0.17 |
| 4. Deliberately annoys people | 0.05 | 0.61 | 0.17 |
| 5. Blames others for mistakes | 0.16 | 0.53 | 0.16 |
| 6. Touchy/easily annoyed by others | 0.24 | 0.56 | 0.14 |
| 7. Often angry and resentful | 0.15 | 0.49 | 0.30 |
| 8. Often spiteful and vindictive | 0.11 | 0.30 | 0.35 |
| Impairment: multiple settings | 0.22 | 0.85 | 0.16 |
| Duration of 6 months or more | 0.25 | 0.77 | 0.01 |
| Conduct Disorder | |||
| 1. Often bullies, threatens, or intimidates | 0.09 | 0.13 | 0.53 |
| 2. Often initiates physical fights | 0.11 | 0.15 | 0.43 |
| 3. Used a weapon with potential for harm | 0.04 | 0.33 | 0.46 |
| 4. Cruel to people | 0.14 | 0.10 | 0.44 |
| 5. Cruel to animals | 0.15 | 0.01 | 0.33 |
| 6. Sets fires to cause damage | 0.19 | 0.12 | 0.42 |
| 7. Deliberately destroyed property | 0.08 | 0.25 | 0.49 |
| 8. Broken into house, car, building | −0.02 | −0.01 | 0.40 |
| 1. Lies to con others | 0.28 | 0.35 | 0.34 |
| 2. Stolen nontrivial items | 0.14 | 0.07 | 0.49 |
| 3. Stays out late before age 13 | 0.03 | 0.13 | 0.24 |
| 4. Truant before 13 | −0.06 | 0.07 | 0.42 |
| 5. Impairment – multiple settings | 0.25 | 0.33 | 0.62 |
3.4 Four-Component Level
As with the three-component level, both ODD and CD criteria loaded onto separate clusters or components at the four-component level. CD criteria at the fourth component level correlated r = 0.90, p<0.001 with CD criteria from the previous level. Similarly, the ODD component correlated almost perfectly with the ODD component from the previous level (r = 0.99, p<0.001), demonstrating continuity throughout the hierarchy. Again at this level, we see the CD criterion “lies to con others” loaded onto the component of ODD criteria (with a loading of 0.35), while “spiteful and vindictive” (an ODD criterion) loaded onto the CD component (with a loading of 0.32, see Table 5).
Table 5.
Principal Component Loadings for the Four-Component Level
| Component 1 | Component 2 | Component 3 | Component 4 | |
|---|---|---|---|---|
| Attention Deficit Hyperactivity Disorder | ||||
| A 1. ADHD Inattention | ||||
| a. Makes careless mistakes | 0.49 | 0.08 | 0.26 | 0.20 |
| b. Difficulty sustaining attention | 0.64 | 0.19 | 0.14 | 0.06 |
| c. Often does not seem to listen | 0.59 | 0.07 | 0.24 | 0.05 |
| d. Difficulty following through on instructions | 0.46 | 0.03 | 0.31 | 0.13 |
| e. Difficulty organizing tasks | 0.72 | 0.16 | 0.08 | 0.09 |
| f. Avoids mental effort | 0.55 | 0.18 | 0.23 | 0.23 |
| g. Often loses necessary items | 0.68 | 0.14 | 0.00 | −0.01 |
| h. Often easily distracted | 0.63 | 0.16 | 0.15 | 0.10 |
| i. Often forgetful | 0.73 | 0.21 | 0.07 | 0.13 |
| 2. ADHD Hyperactivity/Impulsivity | ||||
| Hyperactivity | ||||
| a. Often fidgets or squirms | 0.36 | 0.01 | 0.43 | 0.18 |
| b. Difficulty remaining seated | 0.28 | 0.00 | 0.53 | 0.22 |
| c. Inappropriate running about | 0.23 | 0.14 | 0.44 | 0.24 |
| d. Difficulty playing quietly | 0.10 | 0.09 | 0.57 | 0.14 |
| e. Often “on the go” | 0.25 | 0.06 | 0.59 | 0.15 |
| f. Often talks excessively | 0.07 | 0.21 | 0.55 | −0.06 |
| Impulsivity | ||||
| g. Often blurts out answers | 0.13 | 0.24 | 0.59 | −0.01 |
| h. Difficulty awaiting turn | 0.15 | 0.17 | 0.65 | 0.15 |
| i. Often interrupts or intrudes | 0.23 | 0.28 | 0.52 | −0.04 |
| B. Onset before age 7 | 0.51 | −0.00 | 0.43 | 0.05 |
| Impairment: multiple settings | 0.74 | 0.19 | 0.25 | 0.12 |
| Oppositional Defiant Disorder | ||||
| 1. Often loses temper | 0.29 | 0.58 | 0.07 | 0.15 |
| 2. Often argues with adults | 0.13 | 0.69 | 0.18 | 0.17 |
| 3. Defies adults’ requests | 0.10 | 0.59 | 0.06 | 0.18 |
| 4. Deliberately annoys people | 0.01 | 0.62 | 0.13 | 0.13 |
| 5. Blames others for mistakes | 0.05 | 0.55 | 0.27 | 0.06 |
| 6. Touchy/easily annoyed by others | 0.29 | 0.54 | 0.00 | 0.21 |
| 7. Often angry and resentful | 0.15 | 0.48 | 0.09 | 0.32 |
| 8. Often spiteful and vindictive | 0.06 | 0.30 | 0.17 | 0.32 |
| Impairment: multiple settings | 0.20 | 0.85 | 0.15 | 0.14 |
| Duration of 6 months or more | 0.24 | 0.77 | 0.11 | −0.00 |
| Conduct Disorder | ||||
| 1. Often bullies, threatens, or intimidates | 0.08 | 0.11 | 0.10 | 0.56 |
| 2. Often initiates physical fights | 0.08 | 0.14 | 0.13 | 0.43 |
| 3. Used a weapon with potential for harm | −0.00 | 0.33 | 0.16 | 0.43 |
| 4. Cruel to people | 0.15 | 0.07 | 0.07 | 0.49 |
| 5. Cruel to animals | 0.05 | 0.01 | 0.24 | 0.27 |
| 6. Sets fires to cause damage | 0.08 | 0.13 | 0.29 | 0.35 |
| 7. Deliberately destroyed property | 0.08 | 0.23 | 0.07 | 0.52 |
| 8. Broken into house, car, building | 0.04 | −0.04 | −0.09 | 0.49 |
| 9. Lies to con others | 0.20 | 0.35 | 0.26 | 0.30 |
| 10. Stolen nontrivial items | 0.14 | 0.05 | 0.10 | 0.53 |
| 11. Stays out late before age 13 | 0.02 | 0.12 | 0.05 | 0.24 |
| 12. Truant before 13 | −0.00 | 0.04 | −0.07 | 0.50 |
| 13. Impairment – multiple settings | 0.18 | 0.31 | 0.26 | 0.61 |
At this level of the hierarchy, ADHD criteria became more refined and two separate components of ADHD criteria emerged: a cluster comprised of Inattentive criteria, and a cluster comprised of Hyperactive/Impulsive criteria. The ADHD ‘Inattentive’ component included criteria such as “difficulty sustaining attention,” with principal component loadings ranging from 0.46 to 0.74. The second cluster of ADHD criteria, the Hyperactivity/Impulsivity component, included criteria such as “difficulty remaining seated,” with loadings ranging from 0.43 to 0.65. Both of these two ADHD subtype components correlated substantially with the broader ADHD component found at the three-component level (r = 0.88, p<0.001 for ADHD Inattention, and r = 0.48, p<0.001 for ADHD Hyperactivity/Impulsivity) demonstrating that they were related but separable subtypes at this level. Although no CD criteria loaded strongly onto the ADHD Hyperactive/Impulsive cluster of criteria, these two constructs were moderately correlated between the third and fourth component levels (r = 0.40, p<0.001). Additionally, this four-component level uniquely captured an additional 4.17% of the total variance (cumulatively capturing approximately 40% of the total variance).
3.5 Five-Component Level
At the five-component level, both ADHD Inattentive and ADHD Hyperactive/Impulsive components moved from level four to level five perfectly, with correlations of r = 1.0, p<0.001, and r = 0.99, p<0.001, respectively, demonstrating the stable hierarchical nature of these ADHD sub-types. Similarly, the ODD component at the five-component level correlated almost perfectly with ODD at the four-component level (r = 0.99, p<0.001).
Additionally, at the five-component level two separate clusters of CD criteria emerged. ‘Aggressive’ criteria comprised the primary CD component, while ‘rule-breaking’ criteria comprised the secondary CD component. The ‘aggressive’ component, including criteria such as “often initiates physical fights,” had loadings ranging from 0.34 to 0.65 (shown in plum, see Table 6); and the ‘rule-breaking’ component, including criteria such as “truancy” and “staying out,” had loadings ranging from 0.41 to 0.60 (shown in pink, see Table 6). These two newly-emerging clusters of CD criteria correlated strongly with the broader cluster of CD criteria found at the previous four-component level (‘aggressive’ component: r = 0.60, p<0.001; ‘rule-breaking’ component: r = 0.80, p<0.001), indicating that they were separable but correlated subtypes of CD. CD criteria “sets fires to cause damage” and “stays out late before age 13” did not load strongly onto any of the components at the five-component level (with loadings ranging from 0.07 to 0.29 and 0.02 to 0.23, respectively). Additionally, “lies to con others” still loaded (at 0.35) onto the ODD cluster of criteria. This level uniquely captured 3.13% of the total variance and approximately 43% of the total variance cumulatively.
Table 6.
Principal Component Loadings for the Five-Component Level
| Component 1 | Component 2 | Component 3 | Component 4 | Component 5 | |
|---|---|---|---|---|---|
| Attention Deficit Hyperactivity Disorder | |||||
| A 1. ADHD Inattention | |||||
| a. Makes careless mistakes | 0.49 | 0.11 | 0.28 | −0.05 | 0.29 |
| b. Difficulty sustaining attention | 0.64 | 0.20 | 0.14 | 0.00 | 0.07 |
| c. Often does not seem to listen | 0.59 | 0.06 | 0.23 | 0.14 | −0.03 |
| d. Difficulty following through on instructions | 0.46 | 0.01 | 0.29 | 0.29 | −0.05 |
| e. Difficulty organizing tasks | 0.72 | 0.15 | 0.07 | 0.11 | 0.04 |
| f. Avoids mental effort | 0.55 | 0.19 | 0.23 | 0.14 | 0.18 |
| g. Often loses necessary items | 0.69 | 0.12 | −0.01 | 0.15 | −0.12 |
| h. Often easily distracted | 0.63 | 0.18 | 0.17 | −0.06 | 0.17 |
| i. Often forgetful | 0.73 | 0.21 | 0.07 | 0.14 | 0.06 |
| 2. ADHD Hyperactivity/Impulsivity | |||||
| Hyperactivity | |||||
| a. Often fidgets or squirms | 0.35 | 0.05 | 0.45 | −0.07 | 0.29 |
| b. Difficulty remaining seated | 0.27 | 0.04 | 0.56 | −0.07 | 0.34 |
| c. Inappropriate running about | 0.23 | 0.15 | 0.44 | 0.18 | 0.17 |
| d. Difficulty playing quietly | 0.10 | 0.08 | 0.55 | 0.25 | −0.01 |
| e. Often “on the go” | 0.25 | 0.08 | 0.61 | −0.03 | 0.22 |
| f. Often talks excessively | 0.08 | 0.19 | 0.53 | 0.15 | −0.18 |
| Impulsivity | |||||
| g. Often blurts out answers | 0.13 | 0.23 | 0.58 | 0.13 | −0.11 |
| h. Difficulty awaiting turn | 0.15 | 0.18 | 0.65 | 0.11 | 0.11 |
| i. Often interrupts or intrudes | 0.24 | 0.26 | 0.51 | 0.16 | −0.18 |
| B. Onset before age 7 | 0.51 | −0.00 | 0.43 | 0.05 | 0.03 |
| Impairment: multiple settings | 0.74 | 0.20 | 0.25 | 0.05 | 0.11 |
| Oppositional Defiant Disorder | |||||
| 1. Often loses temper | 0.29 | 0.57 | 0.05 | 0.23 | −0.00 |
| 2. Often argues with adults | 0.13 | 0.69 | 0.17 | 0.17 | 0.05 |
| 3. Defies adults’ requests | 0.10 | 0.61 | 0.07 | 0.07 | 0.14 |
| 4. Deliberately annoys people | 0.01 | 0.65 | 0.15 | −0.08 | 0.20 |
| 5. Blames others for mistakes | 0.05 | 0.56 | 0.28 | −0.03 | 0.08 |
| 6. Touchy/easily annoyed by others | 0.29 | 0.53 | −0.01 | 0.21 | 0.09 |
| 7. Often angry and resentful | 0.15 | 0.48 | 0.08 | 0.27 | 0.18 |
| 8. Often spiteful and vindictive | 0.06 | 0.30 | 0.16 | 0.27 | 0.18 |
| Impairment: multiple settings | 0.20 | 0.85 | 0.14 | 0.15 | 0.03 |
| Duration of 6 months or more | 0.24 | 0.77 | 0.12 | −0.07 | 0.01 |
| Conduct Disorder | |||||
| 1. Often bullies, threatens, or intimidates | 0.08 | 0.12 | 0.09 | 0.39 | 0.41 |
| 2. Often initiates physical fights | 0.08 | 0.11 | 0.09 | 0.63 | 0.07 |
| 3. Used a weapon with potential for harm | −0.00 | 0.33 | 0.14 | 0.42 | 0.22 |
| 4.Cruel to people | 0.16 | 0.05 | 0.02 | 0.65 | 0.13 |
| 5.Cruel to animals | 0.05 | 0.01 | 0.22 | 0.34 | 0.09 |
| 6.Sets fires to cause damage | 0.07 | 0.14 | 0.29 | 0.22 | 0.27 |
| 7.Deliberately destroyed property | 0.07 | 0.25 | 0.07 | 0.31 | 0.41 |
| 8.Broken into house, car, building | 0.03 | 0.01 | −0.06 | 0.02 | 0.60 |
| 9. Lies to con others | 0.20 | 0.35 | 0.25 | 0.23 | 0.20 |
| 10. Stolen nontrivial items | 0.13 | 0.09 | 0.12 | 0.16 | 0.54 |
| 11. Stays out late before age 13 | 0.02 | 0.14 | 0.06 | 0.09 | 0.23 |
| 12. Truant before 13 | −0.01 | 0.09 | −0.05 | 0.10 | 0.55 |
| 13. Impairment – multiple settings | 0.18 | 0.32 | 0.25 | 0.49 | 0.38 |
3.6 Six-Component Level
To lend further support to the hierarchical nature of these constructs, ADHD Inattention and ODD criteria move almost in unity from the five- to the six-component level (with correlations of r = 0.99, p<0.001 for both ADHD Inattention and ODD). Both CD ‘aggressive’ and ‘rule-breaking’ criteria also correlated highly between the five- and six-component levels (with correlations of r = 0.93, p<0.001 and r = 0.85, p<0.001, respectively), which further illustrates hierarchy within this model.
At this level of the hierarchy, we see an additional refinement in ADHD Hyperactive/Impulsive criteria, with two separate components emerging. One component was comprised of predominantly ‘hyperactive’ criteria, including “often fidgets, squirms, restless,” with a pattern of strong component loadings ranging from 0.53 to 0.61 (shown in green under ‘component 3’). A second component encompassed predominantly ‘impulsive’ criteria, including “often interrupts or intrudes,” with loadings ranging from 0.35 to 0.64 (shown in pink, Table 7). These two newly-formed components of ‘Hyperactivity’ and ‘Impulsivity’ correlated highly with the combined Hyperactive/Impulsive component found at the previous five-component level; both the hyperactivity and the impulsivity components correlated r = 0.70, p<0.001 with the single Hyperactive/Impulsive cluster from the previous level of the hierarchy. This illustrates that these two new clusters of ADHD Hyperactive and Impulsive criteria were strongly related but also separable at this level of the hierarchy.
Additionally at this level (which captured 2.91% of the total variance and approximately 46% of the total variance cumulatively), we observed several instances of cross-disorder criterion loadings. The CD criterion “lies to con others” loaded strongly onto the ODD cluster, as well as onto the ADHD ‘hyperactive’ cluster and the CD ‘aggressive’ cluster of criteria (with loadings of 0.36, 0.31, and 0.32, respectively). The ODD criterion “often spiteful and vindictive” loaded onto the CD ‘aggressive’ cluster of criteria with a loading of 0.31, and the CD criterion “cruel to animals” loaded strongly onto the ADHD ‘impulsive’ cluster of criteria with a loading of 0.35. The previously ‘aggressive’ CD criterion, “sets fires to cause damage,” loaded strongly onto the ‘rule-breaking’ cluster of CD criteria at this level; however, the cluster of CD ‘aggressive’ criteria was not strongly associated with the more ‘rule-breaking’ cluster of CD criteria found at the five-component level (see Figure 1). Additionally, CD ‘rule-breaking’ criteria from the previous five-component level were negatively correlated with the six-component level ADHD ‘impulsive’ criteria (r = -0.32, p<0.001), but positively correlated with the six-component level ‘hyperactive’ criteria of ADHD (r = 0.39, p<0.001). No criterion loaded most strongly onto a seventh component; thus, the model reached a stopping-point prior to the addition of a seventh level to this hierarchy (Goldberg, 2006).
4. Discussion
The goal of the present study was to examine the hierarchical factor structure of ADHD, ODD and CD criteria in early adolescent boys in an attempt to further understand how to conceptualize relationships among criteria or subtypes of these externalizing disorders within a hierarchical spectrum. Current results integrated the existing structural literature on ADHD, ODD, and CD into a single model. Our findings showcase both the similarities among ADHD, ODD, and CD with regard to a broader propensity for externalizing behaviors, as well as the distinctions among these disorders at more refined levels. At the higher levels of the hierarchy, we saw collective clusters of criteria that represent general aspects of childhood or adolescent externalizing psychopathology. At the more refined lower levels of the hierarchy, we saw evidence for more specific features that enabled us to distinguish the individual disorders (and in some cases, subtypes) from one another. We turn now to considering the strengths and limitations of the current study and, keeping these in mind, continue to examine the integration of the present hierarchical model into the existing literature on the structure of externalizing disorders in early adolescence, as well as the benefits of conceptualizing psychopathology in a hierarchical fashion.
4.1 Strengths and Limitations
Several factors must be considered when interpreting the current results. First, the sample was over-sampled for externalizing behavior, but an examination of the prevalence rates of ADHD, CD, and ODD criteria indicated that the weighted prevalence rates found in the current sample were comparable to those found in other community samples. Similarly, Keyes et al. (2009) found that weighted rates of these disorders were virtually identical to those from the original population-based MTFS sample of twins, underlining the utility of the sampling weights used here. Additionally, the twins were treated as independent observations in the current analyses, which should not affect parameter estimates (i.e. factor loadings). Twins may differ from non-twins and exhibit slower language development and somewhat more ADHD symptoms (Lahey et al., 2008), but do not tend to differ in other symptoms (Ehringer et al., 2006). The use of both caregiver reports as well as child self-reports of ADHD, CD, and ODD behaviors may be considered a strength, by increasing validity through multiple rater reports. Also, the current study examined these externalizing behaviors in a community sample of boys in early adolescence, while most previous studies have focused their attention on examining these traits in younger school-aged children. Additionally, the specific age range employed in the current study (with lifetime assessments through age 14) may limit the generalizability of our results. A final limitation, which is common within the early externalizing behavior literature, was that we found it necessary to limit our model (and findings) to boys, since boys are generally disproportionately affected by externalizing behavior criteria (Crick, 2003; Maughan et al., 2004). Furthermore, recent evidence has also suggested structural differences in disruptive behaviors when comparing girls with boys (Ford et al., 2003; Loeber et al., 2009). Future studies from this sample will explore these externalizing behaviors and criteria in adolescent girls, to extend the findings for boys presented here.
4.2 Integrating the Current Model into the Existing Externalizing Structural Literature
Previous studies that have examined the structural nature of ADHD, ODD, and CD report (symptom/criterion) clustering patterns that are consistent with different levels of the single hierarchical model presented here. For instance, studies examining the structure of DSM-IV ADHD criteria have generally found it to yield two factors: one factor comprised mainly of ‘Inattentive’ criteria and another a factor comprised of ‘Hyperactive/Impulsive’ criteria (Burns et al., 1997a, 1997b; Waschbusch and King, 2006). The results from these previous studies on ADHD were well-integrated into the current hierarchical model, which also demonstrated the clustering of ADHD criteria into these same inattentive and hyperactive/impulsive subtypes. For example, both Toplak et al. (2009) and Martel et al., (2010) demonstrated that ADHD symptoms not only have a unitary component, but also discreet and distinct separable factors or components for inattention and hyperactivity/impulsivity symptoms similar to the hierarchical component structures found in the current study. Results from the present study complement previous work conducted by Toplak et al., (2009) who used a clinical sample to investigate the component structure of ADHD symptoms. Thus, studies using both community and clinical samples find similar support for a multidimensional structure for ADHD symptoms.
The factor structure of CD has also been extensively explored (Moffitt and Caspi, 2001; Tackett et al., 2003; Maughan et al., 2004). The literature often characterizes CD as consisting of predominantly aggressive traits; however, several lines of research including the current study indicate that purely aggressive criteria cluster into a separate subtype that does not seem to be pervasive (Nock et al., 2006). Consistent with this, in our model we observed that the more common ‘rule-breaking’ criteria of CD clustered into a separate component or subtype from the less common ‘aggressive’ criteria. The identification of reliable subtypes of CD criteria may help bring order to the variety of symptom profiles that can be obtained from the current DSM-IV criteria for CD (Nock et al., 2006).
Although not as extensive, researchers have also investigated the underlying structure of ODD symptoms/criteria and have generally found evidence that a single-factor adequately captures the disorder (Burns et al., 1997a, 1997b; Hommerson et al., 2006). Similarly, the model presented in the current study also demonstrates the consistently one-dimensional nature of ODD.
4.3 Advantages of the Current Hierarchical Model
Findings from the current study demonstrated the advantages in examining criteria from multiple disorders within a single hierarchical model. This hierarchical approach reconciled both “lumping” and “splitting”; the broader components (at the higher levels of the hierarchy) captured the elements common across disorders, and the more refined components (at the lower levels of the hierarchy) represent elements unique to each disorder. Thus, the general externalizing component (the FUPC) accounts for a significant portion of the variation (24% of the variance explained), while all subsequent factors account for smaller, but independent, portions of variance, which in total explain substantial variance above and beyond that captured by the general externalizing component. Each subsequent component is again as large as possible after the influence of all preceding factors or components have been partialed out (Goldberg, 2006). The second through sixth component levels as a whole explained nearly 21% of the total variance; while, the first principal component explains the larger part of the variance, the lower subsequent component levels capture unique, important information for specificity in these behaviors. Thus, these analyses not only provide satisfactory evidence for ‘lumping’ but also for ‘splitting’ components such as those observed for CD and ADHD. One advantage of examining criteria from multiple disorders hierarchically is that certain common features may exist across multiple forms of externalizing psychopathology, as evidenced by the broader components at the top levels of the hierarchy. However, there may also be specific features that distinguish certain disorders or subtypes from one another, such as CD ‘aggressive’ versus ‘rule-breaking’ criteria (Weiss et al., 1998). Recognizing hierarchy in this domain may, in turn, be beneficial in devising treatment options targeting either specific or common features, perhaps depending on presenting comorbidity, as well as useful in devising assessments that evaluate both the common and specific features captured by these childhood externalizing disorders (Weiss et al., 1998).
In addition to identifying common or specific disorder features expressed at different levels of the hierarchy, another significant advantage to this approach is the illustration of the co-morbidity among these components as demonstrated by the presence of moderate to high cross-disorder correlations between component levels (Figure 1). In the current model, we identified specific boundaries between various disorders, but we also identified substantial overlap among disorders. Recognizing associations or covariation among disorders and subtypes may be crucial in identifying both common and specific risk factors for these behaviors, as well as explaining the pervasive pattern of comorbidity often observed among externalizing disorders. For instance, by focusing on the broader levels of the hierarchy, researchers may identify common risk factors for the development of any externalizing disorder, while focusing on risk factors for the criteria found at the more refined levels of the hierarchy (after accounting for common variance shared among disorders, as has been done in our model by the inclusion of the broader components) may help identify risk factors involved in the development of a specific externalizing disorder or subtype.
Additionally, the current findings may aid in identifying and targeting specific sets of symptoms within each component as well as more general behaviors for both prevention and treatment applications. Our findings suggest that both common and unique factors may be important for understanding not only the etiology of certain disorders, but also for treatment methods. For example, this conceptualization suggests that general and specific risks for inattention, hyperactivity, impulsivity, conduct disorders and other externalizing behaviors may need to be assessed separately to provide maximal information about the symptom profiles for ADHD for each individual in order to accurately predict risk and outcome. In turn, treatment may be tailored accordingly to specific constellations of general and or specific symptoms (and risk) that characterize the individual. For example, general ADHD risk may be best treated with a combination of medication and behavioral therapy, whereas specific inattentive symptoms may be treated with medication alone (Martel et al., 2010). Thus, researchers and clinicians should consider both specific and unique factors for assessment, prediction, prevention and treatment methods.
4.4 Conclusions
In sum, the current study’s findings effectively integrated different aspects of the existing literature on the structure of ADHD, ODD, and CD criteria into a single hierarchical model. The current results suggest that focusing on one particular aspect or level of the hierarchy may be limiting in terms of conceptualizing the underlying structure of childhood externalizing problems. Thus, it may be beneficial to examine behavioral differences at different levels of the hierarchy ranging from very broad to very narrow (e.g., examining aspects common across externalizing disorders, as well as those specific to certain disorders or subtypes). Future studies could expand on the hierarchical conceptualization presented here by identifying risk factors that may be more related to externalizing in general, and others that may be associated with externalizing at the level of more refined and specific disorders or subtypes.
Acknowledgments
Data collection was supported by NIH grant R01-DA013240-09. Serena Bezdjian was supported by NIDA training grant T32-DA07313. Steve Malone was supported in part by NIH grant K01-AA01561.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Edelbrock CS. The classification of child psychology: A review and analysis of empirical efforts. Psychological Bulletin. 1978;85:1275–1301. [PubMed] [Google Scholar]
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. [PubMed] [Google Scholar]
- Bauermeister JJ, Bird HR, Canino G, Rubio-Stipec M, Bravo M, Alegria M. Dimensions of attention deficit hyperactivity disorder: Findings from teacher and parent reports in a community sample. Journal of Clinical Child Psychology. 1995;24:264–271. [Google Scholar]
- Bauermeister JJ, Alegría M, Bird HR, Rubio-Stipec M, Canino G. Are attentional-hyperactivity deficits unidimensional or multidimensional syndromes? Empirical findings from a community survey. Journal of the American Academy of Child & Adolescent Psychiatry. 1992a;31:423–431. doi: 10.1097/00004583-199205000-00007. [DOI] [PubMed] [Google Scholar]
- Bauermeister JJ. Factor analyses of teacher rating of attention-deficit hyperactivity and oppositional defiant symptoms in children aged four through thirteen years. Journal of Clinical Child Psychology. 1992b;21:27–34. [Google Scholar]
- Beiser M, Dion R, Gotowiec A. The structure of Attention-Deficit and Hyperactivity symptoms among native and non-native elementary school children. Journal of Abnormal Child Psychology. 2000;28:425–437. doi: 10.1023/a:1005179521820. [DOI] [PubMed] [Google Scholar]
- Burns GL, Alves de Moura M, Walsh JA, Desmul C, Silpakit C, Sommers-Flanagan J. Invariance and convergent and discriminant validity between mothers’ and fathers’ rating of Oppositional Defiant Disorder toward adults, ADHD-HI, ADHD-IN, and academic competence factors within Brazalian, Thai, and American children. Psychological Assessment. 2008;20:121–130. doi: 10.1037/1040-3590.20.2.121. [DOI] [PubMed] [Google Scholar]
- Burns GL, Walsh JA, Boe B, Sommers-Flanagan R, Teegarden LA. A confirmatory factor analysis on the DSM-IVADHD and ODD symptoms: What is the best model for the organization of these symptoms? Journal of Abnormal Child Psychology. 2001;29:339–349. doi: 10.1023/a:1010314030025. [DOI] [PubMed] [Google Scholar]
- Burns GL, Patterson DR. Factor Structure of the Eyberg Child Behavior Inventory: A Parent Rating Scale of Oppositional Defiant Behavior Toward Adults, Inattentive Behavior, and Conduct Problem Behavior. Journal of Clinical Child Psychology. 2000;29:569–577. doi: 10.1207/S15374424JCCP2904_9. [DOI] [PubMed] [Google Scholar]
- Burns GL, Walsh JA, Owen SM, Snell J. Internal validity of attention deficit hyperactivity disorder, oppositional defiant disorder, and overt conduct disorder symptoms in young children: Implications from teachers’ ratings for a dimensional approach to symptom validity. Journal of Clinical Child Psychology. 1997a;26:266–275. doi: 10.1207/s15374424jccp2603_5. [DOI] [PubMed] [Google Scholar]
- Burns GL, Walsh JA, Patterson DR, Holte CS, Sommers-Flanagan R, Paerker CM. Internal validity of disruptive behavior disorder symptoms: Implications from parent ratings for a dimensional approach to symptom validity. Journal of Abnormal Child Psychology. 1997b;25:307–319. doi: 10.1023/a:1025764403506. [DOI] [PubMed] [Google Scholar]
- Conners CK, Sitarenios G, Parker JDA, Epstein JN. Revision and restandardization of the Conners Teacher Rating Scale (CTRS-R): Factor structure, reliability, and criterion validity. Journal of Abnormal Child Psychology: An official publication of the International Society for Research in Child and Adolescent Psychopathology. 1998;26:279–291. doi: 10.1023/a:1022606501530. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Crick NR, Zahn-Waxler C. The development of psychopathology in females and males: Current progress and future challenges. Developmental Psychopathology. 2003;15:719–742. [PubMed] [Google Scholar]
- Doke LA, Flippo JR. Aggressive and oppositional behavior. In: Ollendick TH, Hersen M, editors. Handbook of child psychopathology. New York: Plenum Press; 1983. pp. 323–356. [Google Scholar]
- Dreger RM. First-, second-, and third-order factors from the Children’s Behavioral Classification Project instrument and an attempt at rapprochement. Journal of Abnormal Psychology. 1981;90:242–260. doi: 10.1037/0021-843X.90.3.242. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ. Parent and teacher ratings of ADHD symptoms: Psychometric properties in a community-based sample. Journal of Clinical Child Psychology. Special Issue: Child psychopharmacology. 1991;20:245–253. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, Reid R, McGoey KE, Ikeda MJ. Teacher ratings of attention deficit hyperactivity disorder symptoms: Factor structure and normative data. Psychological Assessment. 1997;9:436–444. doi: 10.1037/pas0000166. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, Anastopoulos AD, Power TJ, Reid R, McGoey KE, Ikeda MJ. Parent ratings of ADHD symptoms: Factor structure, normative data, and psychometric properties. Journal of Psychopathology and Behavioral Assessment. 1998;20:83–102. [Google Scholar]
- Ehringer MA, Rhee SH, Young S, Corley R, Hewitt JK. Genetic and environmental contributions to common psychopathologies of childhood and adolescence: A study of twins and their siblings. Journal of Abnormal Child Psychology. 2006;34:1– 17. doi: 10.1007/s10802-005-9000-0. [DOI] [PubMed] [Google Scholar]
- Farmer RF, Seeley JR, Kosty DB, Lewinsohn PM. Refinements in the hierarchical structure of externalizing psychiatric disorders: Patterns of lifetime liability from mid-adolescence through early adulthood. Journal of Abnormal Psychology. 2009;118:699–710. doi: 10.1037/a0017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ. Early disruptive behavior, IQ, and later school achievement and delinquent behavior. Journal of Abnormal Child Psychology. 1995;23:183–199. doi: 10.1007/BF01447088. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT. The effects of conduct disorder and attention deficit in middle childhood on offending and scholastic ability at age 13. Journal of Child Psychology and Psychiatry. 1993;34:899–916. doi: 10.1111/j.1469-7610.1993.tb01097.x. [DOI] [PubMed] [Google Scholar]
- Ford T, Goodman R, Meltzer H. The British Child and Mental Health Survey 1999: The prevalence of DSM-IV disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Van Horn Y, Lahey BB, Christ MAG, Loeber R, Hart EA, … Hanson K. Oppositional Defiant Disorder and Conduct Disorder: A meta-analytic review of factor analyses and cross-validation in a clinic sample. Clinical Psychology Review. 1993;13:319–340. [Google Scholar]
- Frick PJ. Conduct disorders and severe antisocial behavior. New York: Plenum Press; 1998. [Google Scholar]
- Frick PJ, Kimonis ER. Externalizing disorders of childhood and adolescence. In: Maddux JE, Winstead BA, editors. Psychopathology: Foundations for contemporary understanding. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2005. pp. 325–51. [Google Scholar]
- Frick PJ, Kimonis ER. Externalizing disorders in childhood. In: Maddux E, Winstead BA, editors. Psychopathology: Foundations for contemporary understanding. 2. New York, New York: Routledge/Taylor & Francis Group; 2008. pp. 349–374. [Google Scholar]
- Garber J. Classification of childhood psychopathology: A developmental perspective. Child Development. 1984;55:30–48. [PubMed] [Google Scholar]
- Goldberg LR. Doing it all bass-ackwards: The development of hierarchical factor structures from the top down. Journal of Research in Personality. 2006;40:347–358. [Google Scholar]
- Hommerson P, Murray C, Ohan JL, Johnston C. Oppositional Defiant Disorder Rating Scale: Preliminary evidence of reliability and validity. Journal of Emotional and Behavioral Disorders. 2006;14:118–125. [Google Scholar]
- Janson H, Kjelsberg E. Factor structure and individual patterns of DSM-IV conduct disorder criteria in adolescent psychiatric inpatients. Nordic Journal of Psychiatry. 2006;60:168–175. doi: 10.1080/08039480600610101. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Conduct Disorder. In: Verhulst FC, Koot HM, editors. The epidemiology of child and adolescent psychopathology. New York: Oxford University Press; 1995. pp. 258–290. [Google Scholar]
- Keyes MA, Malone SA, Elkins IJ, Legrand LN, McGue M, Iacono WG. The Enrichment Study of the Minnesota Twin Family Study: Increasing the yield of twin families at high risk for externalizing psychopathology. Twin Research and Human Genetics. 2009;12:489–501. doi: 10.1375/twin.12.5.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Van Hulle C, Urbano RC, Krueger RF, Appelgate B, Garriock HA, Chapman DA, Waldman ID. Testing structural models of DSM-IV symptoms of common forma of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R. Attention-deficit/hyperactivity disorder, oppositional defiant disorder, conduct disorder, and adult antisocial behavior: A life span perspective. In: Stoff DM, Breiling J, Maser JD, editors. Handbook of antisocial behavior. Hoboken, NJ: John Wiley & Sons Inc; 1997. pp. 51–59. [Google Scholar]
- Lahey BB, Loeber R. Framework for a developmental model of oppositional defiant disorder and conduct disorder. In: Routh DK, editor. Disruptive Behavior Disorders in Childhood. New York: Plenum Press; 1994. pp. 139–180. [Google Scholar]
- Loeber R, Pardini DA, Hipwell A, Stouthamer-Loeber M, Keenan K, Sembower MA. Are there stable factors in preadolescent girls’ externalizing behaviors? Journal of Abnormal Child Psychology. 2009;37:777–791. doi: 10.1007/s10802-009-9320-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Burke JD, Lahey BB, Winters A, Zera M. Oppositional defiant and conduct disorder: a review of the past 10 years, part I. Journal of the American Academy Child and Adolescent Psychiatry. 2000;39:1468–1484. doi: 10.1097/00004583-200012000-00007. [DOI] [PubMed] [Google Scholar]
- Loeber R, Lahey BB, Thomas C. Diagnostic conundrum of oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology. 1991;100:379–390. doi: 10.1037//0021-843x.100.3.379. [DOI] [PubMed] [Google Scholar]
- Martel MM, von Eye A, Nigg JT. Revisiting the latent structure of ADHD: Is there a ‘g’ factor? Journal of Child Psychology and Psychiatry. 51:905–914. doi: 10.1111/j.1469-7610.2010.02232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct disorder and oppositional defiant disorder in a national sample: Developmental epidemiology. Journal of Child Psychology and Psychiatry. 2004;45:609–621. doi: 10.1111/j.1469-7610.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- McDermott PA. Generality of disordered behavior across populations of normal and deviant school children: Factorial relations analyses. Multivariate Behavioral Research. 1982;17:69–85. [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Developmental Psychopathology. 2001;13:355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Smith BH, Pelham WE. Factor structure and criterion validity of secondary school teacher ratings of ADHD and ODD. Journal of Abnormal Child Psychology: An official publication of the International Society for Research in Child and Adolescent Psychopathology. 2001;29:71–82. doi: 10.1023/a:1005203629968. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE, Hiripi E, Kessler RC. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychological Medicine. 2006;36:699–710. doi: 10.1017/S0033291706007082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE, Evans S, Gnagy E, Greenslade KE. Teacher ratings of DSM-III-R symptoms for the disruptive disorders: Prevalence, factor analyses, and conditional probabilities in a special education sample. School Psychology Review. 1992;21:285–299. [Google Scholar]
- Pillow DR, Pelham WE, Hoza B, Molina BSG, Stultz CH. Confirmatory factor analyses examining attention deficit hyperactivity disorder symptoms and other childhood disruptive behaviors. Journal of Abnormal Child Psychology. 1998;26:293–309. doi: 10.1023/a:1022658618368. [DOI] [PubMed] [Google Scholar]
- Polanczyk G, Silva de Lima M, Lessa Horta B, Biederman J, Rohde LU. The Worldwide Prevalence of ADHD: A Systematic Review and Metaregression Analysis. American Journal of Psychiatry. 2007;164:856–858. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- Quay HC. Classification. In: Quay HC, Werry JS, editors. Psychopathological disorders of childhood. 3. New York: Wiley; 1986. pp. 1–34. [Google Scholar]
- Reich W, Welner Z. Diagnostic Interview for Children and Adolescents – Revised: DSM-III-R version (DICA-R) St. Louis, MO: Washington University; 1988. [Google Scholar]
- Robins LN. Conduct disorder. Journal of Child Psychology and Psychiatry. 1991;32:193– 212. doi: 10.1111/j.1469-7610.1991.tb00008.x. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Krueger RF, Iacono WG, McGue M. Personality in middle childhood: A hierarchical structure and longitudinal connections with personality in late adolescence. Journal of Research in Personality. 2008;42:1456–1462. doi: 10.1016/j.jrp.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tackett JL, Krueger RF, Sawyer MG, Graetz BW. Subfactors of DSM-IV Conduct Disorder: Evidence and connections with syndromes from the Child Behavior Checklist. Journal of Abnormal Child Psychology. 2003;31:647–654. doi: 10.1023/a:1026214324287. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Pitch A, Flora DB, Iwenofu L, Ghelani K, Jain U, Tannock R. The unity and diversity of inattention and hyperactivity/impulsivity in ADHD: Evidence for a general factor with separable dimensions. Journal of Abnormal Child Psychology. 2009;37:1137–1150. doi: 10.1007/s10802-009-9336-y. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA, King S. Should sex-specific norms be used to assess attention-deficit/hyperactivity disorder or oppositional defiant disorder? Journal of Consulting and Clinical Psychology. 2006;74:179–185. doi: 10.1037/0022-006X.74.1.179. [DOI] [PubMed] [Google Scholar]
- Weiss B, Susser K, Catron T. Common and specific features of childhood psychopathology. Journal of Abnormal Psychology. 1998;107:118–127. doi: 10.1037//0021-843x.107.1.118. [DOI] [PubMed] [Google Scholar]
- Zuddas A, Marzocchi GM, Oosterlaan J, Cavolina P, Ancilletta B, Sergeant J. Factor structure and cultural factors of disruptive behaviour disorders symptoms in Italian children. European Psychiatry. 2006;21:410–418. doi: 10.1016/j.eurpsy.2005.08.001. [DOI] [PubMed] [Google Scholar]