Abstract
This paper examines the relationship between early marriage (before age 26), cohabitation, and health for African Americans and whites during the transition to adulthood using the National Longitudinal Study of Adolescent Health (Add Health). We examine three categories of health outcomes relevant to young adulthood: physical health, mental health, and health risk behaviors. Lagged dependent variable models are used to examine the health effects of early marriage and cohabitation accounting for potential health selection into unions. Our results indicate that early marriage by young adults does not have protective effects for African Americans, and finds more negative effects for African American men than women. There are mixed results for whites with some protective effects of marriage for binge drinking. Early marriage for both African Americans and whites is associated with increased Body Mass Index (BMI). Cohabitation is uniformly associated with negative health outcomes for all race and sex groups.
INTRODUCTION
The transition to adulthood is a period in the life course marked by important changes in living arrangements, union formation and health (Harris et al. 2006; Hogan and Astone 1986; Shanahan 2000). Although many now delay marriage until later in adulthood, early marriage is not uncommon. Recent data from the National Longitudinal Study of Adolescent Health (Add Health), a cohort of 18-26 year-olds in 2001-02, indicate that 16% of males and females had ever married. Others form cohabiting relationships that may serve as precursors to marriage; thirty-two percent of Add Health male and female respondents aged 18-26 had ever cohabited. The relationships between marriage and cohabitation with health during the transition to adulthood are not well understood, despite substantial research on marriage and health and increasing attention to health during the transition to adulthood.
Exploring new lifestyles and experimenting in risk behavior has always characterized the transition to adulthood (Schulenberg, Maggs and Hurrelmann 1997). However, the lengthening of this transition has extended the period of time during which young people engage in health risk behaviors (Settersten, Furstenberg and Rumbaut 2004), and patterns of health behaviors, including diet, physical inactivity, drinking, and smoking, may be set during this time period, with long-term consequences for health in later adulthood (Harris et al. 2006). In addition, multiple stressors accompany this transition, including moving out of the parental home, completing post-secondary education, finding work, and starting a family, and these multiple and often overlapping changes influence the mental health of young adults (Gore et al. 1997; Hagan and Foster 2003).
At the same time that involvement in risk behavior is prolonged as the transition from adolescence to adulthood lengthens, the onset and prevalence of a number of physical health conditions has begun to rise in this age group as well (Harris et al. 2006). For example, physical inactivity and lack of exercise has migrated into the adolescent and young adult ages (Andersen et al. 1998) and as a result of these trends, young adults are at increased risk of metabolic syndrome, high blood pressure, and premature coronary artery disease (Cook et al. 2003; Erikssen 2001; Muntner et al. 2004).
African Americans may face unique stressors in the transition to adulthood in part due to social contexts that include fewer resources, segregation and discrimination (Anderson 1999; Osypuk et al. 2008; Patillo 1999; Wilson 1987; Woldoff and Ovadia 2008). Despite the emergence of a significant African American middle class, African American youth continue to experience social and economic disparities in the social contexts in which they grow and develop (Patillo 2005). African Americans experience a higher rate of poverty, which puts them at higher risks of disease, disability and death (Williams and Collins 1995). Poverty is associated with poor health among African Americans to a greater degree than it is among whites because of the additional social disadvantages associated with poverty that African Americans experience (House and Williams 2000). For example, African Americans at all levels of socioeconomic status (SES) are more segregated from whites than any other racial or ethnic group (Iceland, Weinberg, and Steinmetz 2002). Segregated neighborhoods can be protective for African American youth, but are still more likely to be characterized by high poverty and crime, poor schools, and fewer economic opportunities and services (Williams and Collins 2001). These neighborhood disadvantages have serious implications for the health outcomes of young African Americans, including increased levels of obesity, HIV prevalence and violence (Aneshensel and Sucoff 1996; Kawachi and Berkman 2003). Finally, substantial research indicates that discrimination has direct negative health consequences for African Americans, impacting both mental and physical health (Williams, Neighbors and Jackson 2003). Discrimination has furthermore been linked to biological and self-reported measures of stress, suggesting an important mechanism of poor health (Mays, Cochran and Barnes 2007; Sellers et al. 2003). These multiple experiences shape the lives of African American young adults with implications, not only for their health, but their ability to make important life course transitions, including the decision to cohabit or marry. This paper addresses racial differences in marriage and subsequent changes in health during the transition to adulthood, with a particular focus on the African American population.
MARRIAGE AND HEALTH
Prior research on the links between marriage and health in the transition to adulthood has focused mostly on changes in health behaviors following entry into first marriage. For example, research using data from the Monitoring the Future (MTF) study show a negative association between marriage and substance abuse (drinking, cigarette smoking and drug), but no relationship between substance use and cohabitation, unless the cohabitation entailed engagement (for marriage) (Bachman et al. 1997; Bachman et al. 2002). Similarly, data from the National Longitudinal Survey of Youth (NLSY) show declines in binge drinking and drug use (but not smoking) after entry into first marriage (Duncan, Wilkerson and England 2006; Curran, Muthen, and Harford 1998; Miller-Tutzauer, Leonard and Windle 1991). Possible mechanisms or pathways that help to explain the relationship between marriage and health include change in time use, monitoring of behaviors by spouse, and norms that are associated with the idea that marriage entails “cleaning up one's act,” which include increased church attendance and reduced “partying” (Duncan et al. 2006). The effects of cohabitation on health behaviors are less consistent. It is argued that, although cohabitation has become a common living arrangement in recent decades, it is associated with a different set of social norms that do not lead to reductions in risk behaviors (Duncan et al. 2006).
Less evidence exists examining the relationship between marriage, especially early marriage, and health among young African Americans, despite well-documented differences in health profiles and marriage behaviors. Please see the first paper in this volume (Moiduddin, Koball, Henderson, Goesling, and Besculides 2009) for a general overview of the research literature on the relationship between marriage and health in the African American community. Data from Add Health on 18-26 year-olds in 2001-02 show that marriage rates are lower for African Americans (10%) compared to whites (19%) in the late teens and early twenties while cohabitation rates are slightly higher for African Americans (37%) compared to whites (31%). Clearly, early marriage is more prevalent among whites than African Americans, as has been found in previous research (Wood, Goesling and Avellar 2007). In addition, there are large racial differences among young adults in mental and physical health outcomes, as well as health risk behaviors (Fuligni and Hardway 2004; Harris et al. 2006). For example, a greater proportion of African American compared to white young adults are obese, physically inactive, and eat a poor diet. However, a larger proportion of white compared to African American young adults binge drink and smoke cigarettes (Harris et al. 2006).
In this paper we explore (1) the relationship between early marriage (defined as a marriage before the age of 26) and health for African Americans, (2) how this relationship differs by gender for African Americans and (3) how this relationship differs by race. We examine these questions using data provided by the National Longitudinal Study of Adolescent Health (Add Health), which began collection in 1994 and observes respondents in adolescence as well as early adulthood. We examine multiple measures of physical and mental health as well as risk behaviors across time, allowing us to comprehensively assess changes in multiple dimensions of health during the transition to adulthood. Furthermore, because of the selective nature of the population entering early marital unions, we control for the factors that are associated with early marriage, including prior health. Because of the unique stressors African Americans face in their social contexts, we control for socioeconomic status (SES) at multiple levels.
Studying the transition to adulthood adds to our knowledge of marriage and health for African-Americans because it provides crucial information about a stage in the life course that is relevant to later health and marital behavior. In addition, capturing the complex and dynamic nature of the social context is especially important when studying the transition to adulthood (Elder 1997; Shanahan 2000), as well as health development and precursors to chronic disease (Ben-Shlomo and Kuh 2000; Halfon and Hochstein 2002; Lynch and Smith 2005). As adolescents make decisions regarding union formation, health behaviors, schooling and employment, they are also influenced by multiple aspects of their environments, such as their family, peer, school and neighborhood context (Fuligni and Hardway 2004; Osgood et al. 2005). These contexts can serve as positive support systems facilitating optimal outcomes during life course transitions, or they can serve as sources of stress and negative role modeling that can lead to less optimal outcomes.
The life course (Elder et al. 1997) and ecological (Bronfrenbrenner 2005; Bronfrenbrenner and Morris 1998) perspectives both suggest that social disadvantage should be measured at multiple ecological levels, over time, and via different processes. This is particularly important in the study of African-Americans, as this population faces unique environmental challenges and stressors due to racial segregation, higher levels of single-parent households and a higher likelihood of living in disadvantaged neighborhoods all of which have important implications for current and future health and marriage behavior (Furstenberg et al. 1999; Wilson 1987; James 1985, 2006).
Understanding health and union formation at these young ages provides not only important information about the well-being of a vulnerable population but also baseline information that can be used to better understand the factors influencing the relationship between marriage and health as these young people move through the life course. Determining whether protective health effects of early marriage are relevant for the African-American population is important from both public health and public policy perspectives. Our research will also shed light on the role of health profiles within the African-American community in fostering marriage.
DATA
Add Health is a longitudinal, nationally representative, school-based study of ethnically diverse U.S. adolescents designed to explore the causes of health-related behaviors. The data also includes extensive information on socioeconomic status and race and has been linked to contextual data, including characteristics of the neighborhoods and communities in which Add Health sample members live. Wave I (WI) was collected in 1994 and 1995, when respondents were in grades 7 to 12 (aged 12 to 19 years), and consists of both an In-School Questionnaire, which was administered to every student in a nationally representative sample of schools [N= 90,118], and a more extensive In-Home Interview [N=20,745] administered to a sub sample of these individuals. In Wave III (WIII), all located WI In-Home respondents, now aged 18-26 years (2002) were re-interviewed [N=15,197]. A parent, generally the mother, was also interviewed in WI. In-home adolescent questionnaires were administered by computer-assisted personal-interview (CAPI), as well as computer-assisted self-interview (CASI) for more sensitive questions.
In the In-School Questionnaire students were asked to nominate up to 5 male and 5 female friends and to locate and record their student IDs from the school roster. Because the in-school sample was a saturated sample, with nearly all youth in the school interviewed, the identification numbers of nominated friends can be linked back to their own in-school questionnaire and characteristics of a respondent's peer group can be determined, such as its racial/ethnic makeup. In a similar fashion, school-level measures can be derived by aggregating the responses of the In-School Questionnaire for all students in their respective schools. In addition, contextual data containing information on the characteristics of the neighborhoods and communities in which Add Health sample members lived in Waves I, II and II have been linked to individual-level records.
This study uses data from the Wave I In –Home, School and Parent Questionnaires as well as the follow-up Wave III surveys, as well as contextual data from WI. Our final Add Health sample includes 9,158 respondents: WI and WIII In-Home respondents remaining after dropping non-blacks and non-whites (including Hispanics, Asians, and others), pregnant women in WIII, married individuals in WI, those with more than one marriage recorded by WIII, those who are disabled, and those missing on key indicators. Our final sample consists of 1,371African American females, 3,456 white females, 1,109 African-American males, and 3,222 white males. All analyses use STATA survey procedures with sampling weights to adjust for the clustered sample design and unequal probability of selection to ensure the results are nationally representative and that bias in standard errors are reduced.
Measuring Marriage and Cohabitation
Respondents were coded as married if they married between WI and WIII. We distinguish single respondents who cohabited between WI and WIII from those who did not marry or cohabit in this time period. Individuals who were married at WI, divorced between WI and WIII, or who married more than one time by WIII were excluded from the analysis. A sensitivity analysis on the coding of marriage was performed in which anyone who transitioned into marriage between WI and WIII was coded as married and anyone who married but then divorced were coded as not married, instead of excluding them from the sample. We found no substantial difference in our analyses.
RESEARCH DESIGN AND METHODS
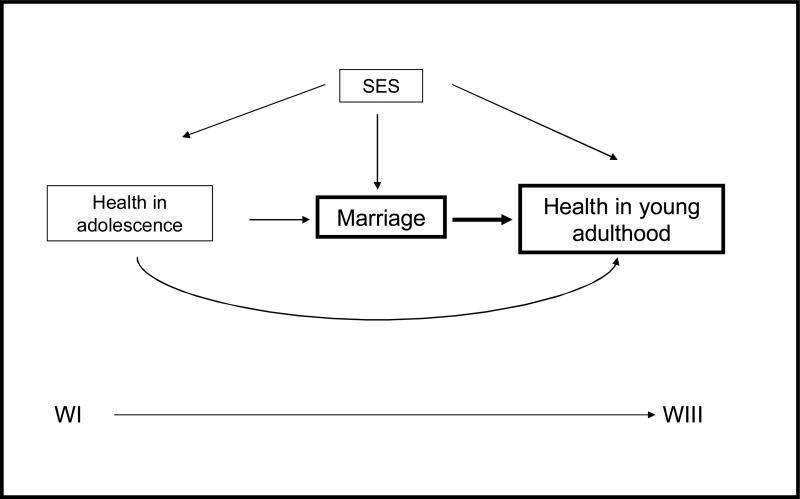
Figure 1 depicts the conceptual model for our analytic work and is based on a life course framework of health (Elder 1997; Halfon and Hochstein 2002). It also draws from previous social, demographic, and economic research linking health in childhood to health and social outcomes in later life (Elo and Preston 1992; Case, Fertig, and Paxson 2005). The relationship between marriage and health in young adulthood is influenced by baseline health in adolescence, which impacts both entry into marriage and later health directly (Halfon and Hochstein 2002). Socioeconomic status (SES) is relevant to marriage and health in both adolescence and young adulthood.
Figure 1.
Conceptual model
To examine the impact of early marriage on health, we use a change (or lagged dependent variable) model that sets health at WIII as a function of the initial level of adolescent health at WI, marriage between WI and WIII, and a set of time-invariant SES and control variables measured at WI (Allison 1990). Such models can be estimated correctly as long as exogenous predictors are well controlled (Johnson 2005). The simple model is depicted in Equation (1):
| (1) |
Here, Yi represents a vector of health indicators measured at WIII (Time 2) for person i and X1i represents a vector of identical health measures at WI (Time 1). X2i is an indicator for marriage between WI and WIII, and X3i is a vector of demographic controls. The vector X4i represents SES measures described below.
Potential health selection is accounted for in our lagged dependent variable regression analysis predicting health in young adulthood (WIII) by including baseline health (in WI) as a predictor. The resulting marriage coefficient, X2i from Equation (1), reflects the influence of marriage on health in young adulthood independent of these impacts. In a similar fashion, our models also include an indicator for cohabitation between WI and WIII, and its coefficient reflects the influence of cohabitation on health in young adulthood.
This research examines three categories of negative health outcomes at the individual level: physical health, mental health, and risk behaviors. Detailed descriptions of our measures are presented in the top panel of Table 1. Measures of physical health include body mass index (BMI) and poor self-reported health. Mental health (depression) is measured using questions from the Center for Epidemiologic Studies Depression (CES-D) scale1, and risk behavior is represented by reports of binge drinking, smoking, marijuana use, and lack of physical activity. We also create a composite measure of poor health by first categorizing the seven health indicators in Table 1 according to cut-offs for poor health and then summing to create a count of poor health indicators.
Table 1.
Measures used in lagged dependent variable analysis
| Variable | Description |
|---|---|
| MEASURES OF HEALTH USED IN LAGGED DEPENDENT VARIABLE ANALYSIS | |
| Physical Health | |
| BMI | Continuous measure of raw BMI measured as body weight in kilograms/height in meters squared. Height and weight measures were self-reported at WI and measured by trained interviewers at WIII (Range: 11.21-64.56). |
| Poor self-reported health | Ordinal measure of self reported health at WI where: 5 is poor, 4 is fair, 3 is good, 2 is very good and 1 is excellent. |
| Mental Health | |
| Depression index | Ordinal measure of sum of responses to 3 questions: How often was each of the following true during the past week: (1) You felt depressed, (2) You felt sad, (3) You felt like you could not shake off the blues, even with help from your family and friends (Range: 0-9). |
| Risk Behaviors | |
| Binge drinking episodes | Self-reported number of episodes of binge drinking (5 or more drink on one occasion) during the past year (range: 0-365). |
| Cigarettes smoked per day | Self reported number of cigarettes smoked per day in the past 30 days (Range: 0-95). |
| Marijuana Usage | Self reported number of times marijuana used in the past 30 days (Range: 0-999). |
| Lack of Physical Activity | Ordinal measure of bouts of physical activity, reverse coded so that higher numbers indicate lower levels of physical activity (Range: 0-18). |
| Composite Health Measure | Ordinal measure of sum of binary versions of health indicators above (Range: 0-7). Poor health binary measures are constructed in the following way: 1) obese defined by International Obesity Task Force (IOTF) definitions; 2) reported fair or poor health; 3) depression index score>3; 4) reported 5 or more drinks on one occasion in past year; 5) reported smoking at least 1 whole cigarette daily in last 30 days; 6) reported using marijuana at least one time in last 30 days; and 7) bouts of physical activity <5. |
| MEASURES OF SOCIOECONOMIC STATUS AND CONTROLS | |
| Individual Level Controls | |
| Low family SES at WI | Sum of responses to 3 binary items at WI: (1) 1 no 2 bio parents, (2) poverty/welfare and (3) parent education HS or less (Range:0-3) Categorical measure indicating religiosity index score is less than 1.5. Religiosity is measured as an index that represents the average response to three questions: 1) Church attendance (ranging from 4 for never attend to 1 for attend once a week or more) 2) The importance of religion (ranges from 4 for not important at all 1 for very important) 3) The frequency of prayer (ranges from 5 for never to 1 for at least once a day). |
| Low religiosity at WI | We rescale and reverse code responses to range from 0 to 3 rather than 1 to 4 to be more consistent with answer choices. Those who are missing on religion are given a value of -1 on each of these measures. |
| Non-marital birth | First birth reported prior to first marriage (females only measure) |
| Birth between WI and WIII | Birth reported between WI and WIII |
| Ever cohabited between WI and WIII | Report of living with a romantic partner in a nonmarital union between WI and WIII |
| Age at WI | Continuous measure of self-reported age in years at WI (Range: 11-21) |
| Peer Level SES | |
| High % parent HS or less: peer | Proportion of respondent's peers whose highest educated parent completed high school (or GED) or less is greater than 56% |
| High % single parent: peer | Proportion of respondent's peers living in a single parent household is greater than 20% |
| No friendship Information | Respondent either reported no school friends or information on reported friends was not available |
| School Level SES | |
| High % parent HS or less: school | Categorical measure indicating the proportion of students in a respondent's school whose highest educated parent completed high school (or GED) or less is greater than 53% |
| High % single parent: school | Categorical measure indicating the proportion of students in a respondent's school living in a single parent household is greater than 23.5% |
| Neighborhood Level SES | |
| High % parent less than HS: neighborhood | Categorical measure indicating the proportion of individuals 25 years or older in a respondent's neighborhood who completed less than a high school (or GED) is greater than 34% (Census tract level measure) |
| High % female headed household: neighborhood | Categorical measure indicating the proportion of female-headed households in a respondent's neighborhood is greater than 7.5% (Census tract level measure) |
| Low racial heterogeneity | Categorical measure indicating level of racial dispersion in a respondent's neighborhood is less than or equal to .05 (i.e., homogeneity of one racial group). The dispersion measures are based on the following formula: D~=~{k(N^2- E f SUB i^2)} OVER{ N SUP 2(k-1)} where k is the number of categories, N2 is the sum of all categories squared, and ‘fi2 is the sum of squared category frequencies over all i (=1, ..., k) groups. If D = 0, then only one category is nonzero; if D = 1, all category frequencies are equal. |
| Urban tract | Categorical measure to designate if respondent lives in an urbanized area |
It should be noted that BMI is self-reported at WI. Previous research examining the accuracy of adolescent self-report of height and weight in assessing obesity status has found that the prevalence of obesity is consistently underestimated by self-reported data. Females underestimate their weight more than males, and obese adolescents tend to underestimate their weight more than non-obese weight adolescents. There is less adequate information to determine differences by race. However, in nationally representative samples, correlation coefficients between self-reported and measured height and weight are still very high, ranging from 0.79 to 0.91 for height and 0.90 to 0.97 for weight (For a Review see Sherry, Jefferds and Grummer-Strawn 2007). More specifically, research using WII of Add Health to compare calculated BMI from self-reported height and weight versus measured height and weight found that when BMI cutoffs were used to determine obesity from self-reported measures, 96% of youth were correctly classified (3.8% were misclassified). Also, no difference in misclassification by sex or race was found (Goodman, Hinden and Khandelwal 2000). However, we preformed a check on the accuracy of our BMI measures by running models using WII BMI, which was calculated from measured height and weight (collected about 1 year after WI), in place of WI BMI (self-report). We found a similar pattern of results.
Our analysis employs measures of socioeconomic status at several levels (individual, peer, school and neighborhood) to examine the influence of multiple ecological levels of disadvantage in the marriage and health relationship. The bottom panel of Table 1 presents detailed descriptions of the SES and control measures used in our analysis. Our multi-level SES measures include family structure and parental education at the individual, peer, school, and neighborhood levels as well as controls for religiosity, childbearing, and age at the individual level. Unique to our analysis is the use of contextual family structure measures that tap role modeling effects in the social context of adolescents’ lives. We examine the percentage of single parent households at the peer, school and neighborhood levels during adolescence. These contextual family structure effects in adolescence have been shown to influence subsequent fertility behaviors (Harris and Cheng 2005). We focus on single parent households given that African Americans are more likely to be single parent families and to have friends, go to schools and live in neighborhoods with high levels of single parent households (Harris and Cheng 2005).
The descriptive sample statistics for these measures are shown in Table 2. Descriptive statistics indicate that, on average, respondents reported a health status of “very good” across race and sex subgroups and across waves. BMI was higher for African American females compared to all other groups at both waves. Males had higher levels of binge drinking and marijuana use compared to females at WI and WIII. Average levels of cigarette smoking were higher for whites, compared to African Americans across both waves. Females had higher levels of depression and lower levels of physical activity compared to males, with African American females experiencing the highest average levels of depression and lowest levels of physical activity across both waves. It is notable that changes in these measures between WI and WIII were in the same direction and relative rankings (i.e., whites vs. African American, males vs. females) remained the same with the exception of binge drinking and composite health. African Americans experienced lower levels of family and neighborhood SES compared to whites. They also had higher mean levels of peers, schoolmates and neighbors coming from single-parent households than whites.
Table 2.
Variable means and standard errors by sex and race
| Female | Male | Female | Male | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Af Amer | White | Af Amer | White | Af Amer | White | Af Amer | White | ||
| HEALTH MEASURES AT WI | INDIVIDUAL LEVEL SES AND CONTROLS | ||||||||
| Physical Health | Low family SES at WI | 1.864 | 1.171 | 1.830 | 1.158 | ||||
| BMI | 23.551 | 21.811 | 22.945 | 22.526 | 0.076 | 0.043 | 0.085 | 0.042 | |
| 0.182 | 0.141 | 0.226 | 0.162 | Low religiosity at WI | 0.133 | 0.277 | 0.218 | 0.324 | |
| Poor self-reported health | 2.198 | 2.134 | 1.982 | 2.010 | 0.018 | 0.015 | 0.027 | 0.015 | |
| 0.043 | 0.024 | 0.054 | 0.021 | Non-marital birth | 0.403 | 0.253 | ------- | ------- | |
| Mental Health | 0.021 | 0.015 | ------- | ------- | |||||
| Depression Index | 1.999 | 1.605 | 1.251 | 1.051 | Age | 15.469 | 15.274 | 15.702 | 15.463 |
| 0.099 | 0.052 | 0.077 | 0.037 | 0.200 | 0.133 | 0.228 | 0.132 | ||
| Risk Behaviors | PEER LEVEL SES | ||||||||
| Binge drinking episodes | 7.595 | 7.922 | 15.622 | 12.836 | High % parent HS or less: peer | 0.331 | 0.324 | 0.254 | 0.308 |
| 1.478 | 0.783 | 3.420 | 1.158 | 0.035 | 0.027 | 0.038 | 0.026 | ||
| Cigarettes smoked per day | 0.826 | 5.519 | 1.871 | 5.108 | High % single parent: peer | 0.514 | 0.284 | 0.326 | 0.243 |
| 0.199 | 0.369 | 0.311 | 0.353 | 0.029 | 0.020 | 0.023 | 0.016 | ||
| Lack of Physical Activity Scale | 12.788 | 11.764 | 10.580 | 10.273 | No friends | 0.276 | 0.305 | 0.467 | 0.363 |
| 0.229 | 0.139 | 0.185 | 0.158 | 0.027 | 0.035 | 0.028 | 0.031 | ||
| Marijuana use | 1.214 | 1.218 | 3.582 | 2.344 | SCHOOL LEVEL SES | ||||
| 0.369 | 0.177 | 1.164 | 0.455 | High % parent HS or less: school | 0.300 | 0.384 | 0.277 | 0.367 | |
| 0.065 | 0.048 | 0.062 | 0.046 | ||||||
| Composite Health Measure | 1.499 | 1.617 | 1.285 | 1.454 | High % single parent: school | 0.628 | 0.159 | 0.531 | 0.135 |
| 0.065 | 0.057 | 0.071 | 0.055 | 0.049 | 0.031 | 0.047 | 0.027 | ||
| HEALTH MEASURES AT WIII | NEIGHBORHOOD LEVEL SES | ||||||||
| Physical Health | High % parent less than HS: neighborhood | 0.529 | 0.169 | 0.515 | 0.180 | ||||
| BMI | 28.111 | 25.791 | 26.422 | 26.279 | 0.049 | 0.028 | 0.054 | 0.027 | |
| 0.327 | 0.195 | 0.256 | 0.183 | High % female headed household: neighborhood | 0.737 | 0.177 | 0.687 | 0.171 | |
| Self-reported health | 2.095 | 2.036 | 1.856 | 1.910 | 0.030 | 0.029 | 0.034 | 0.028 | |
| 0.040 | 0.022 | 0.036 | 0.021 | Low racial heterogeneity | 0.079 | 0.381 | 0.094 | 0.357 | |
| Mental Health | 0.035 | 0.050 | 0.038 | 0.047 | |||||
| Depression Index | 1.501 | 1.217 | 1.121 | 0.902 | Urban tract | 0.569 | 0.443 | 0.552 | 0.438 |
| 0.078 | 0.035 | 0.079 | 0.031 | 0.077 | 0.050 | 0.075 | 0.049 | ||
| Risk Behaviors | |||||||||
| Drinks per year | 4.946 | 13.598 | 15.834 | 32.548 | MARRIAGE AND COHABITATION | ||||
| 1.352 | 0.812 | 2.280 | 1.654 | ||||||
| Cigarettes smoked per day | 3.248 | 9.737 | 6.397 | 10.491 | Married between WI and WIII | 0.108 | 0.222 | 0.096 | 0.133 |
| 0.486 | 0.374 | 0.656 | 0.321 | 0.012 | 0.015 | 0.017 | 0.011 | ||
| Lack of Physical Activity Scale | 19.331 | 18.792 | 17.793 | 18.108 | Cohabited between WI and WIII | 0.355 | 0.323 | 0.383 | 0.303 |
| 0.076 | 0.063 | 0.124 | 0.070 | 0.022 | 0.014 | 0.025 | 0.013 | ||
| Marijuana use | 2.390 | 2.390 | 4.496 | 5.641 | Single between WI and WIII | 0.537 | 0.455 | 0.520 | 0.564 |
| 0.655 | 0.208 | 0.672 | 0.423 | 0.025 | 0.020 | 0.033 | 0.018 | ||
| Composite Health Measure | 2.126 | 2.569 | 2.173 | 2.688 | |||||
| 0.052 | 0.034 | 0.071 | 0.034 | ||||||
| N | 1371 | 3456 | 1109 | 3222 | 1371 | 3456 | 1109 | 3222 | |
PATTERNS OF EARLY MARRIAGE BY RACE
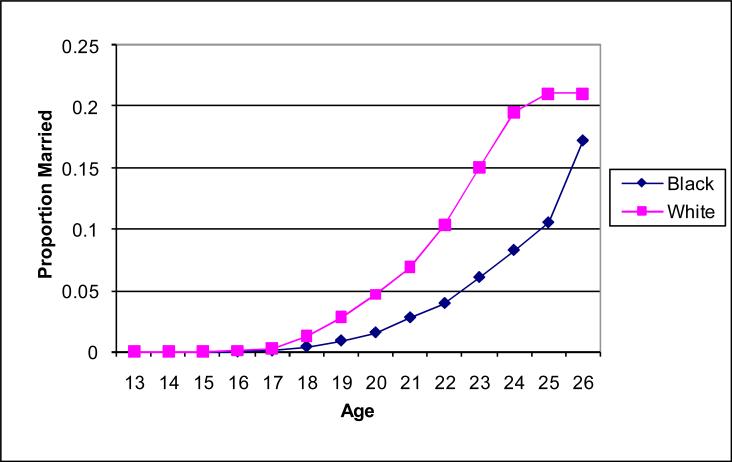
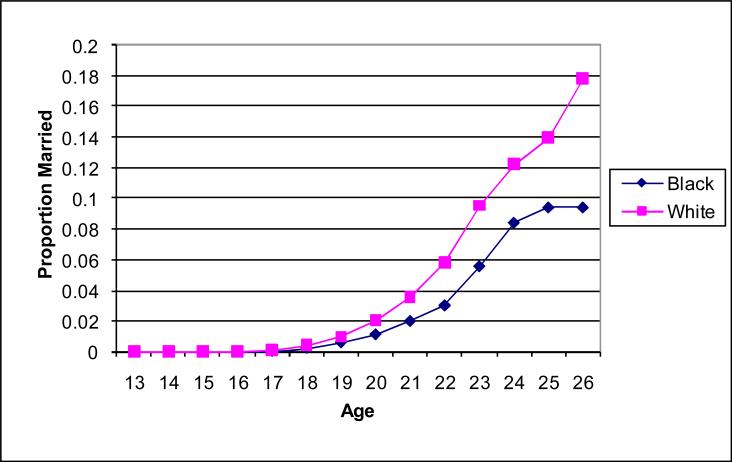
We first examine the patterns of early marriage by race and sex in Figures 2 and 3. These graphs show the cumulative probability of entry into marriage by age 26 by race and sex based on Kaplan-Meier survival estimates from our Add Health data. Clearly, early marriage is more prevalent among whites than African Americans, as has been found in previous research (Wood, Goesling and Avellar 2007). By age 25, over 20% of white females and 14% of white males have married, compared to approximately 10% of African American females and males.
Figure 2.
Cumulative proportion of females married by age 26 by race
Figure 3.
Cumulative proportion of males married by age 26 by race
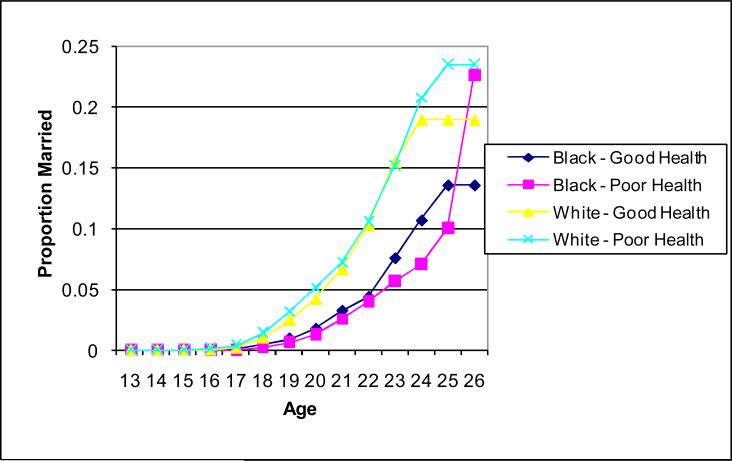
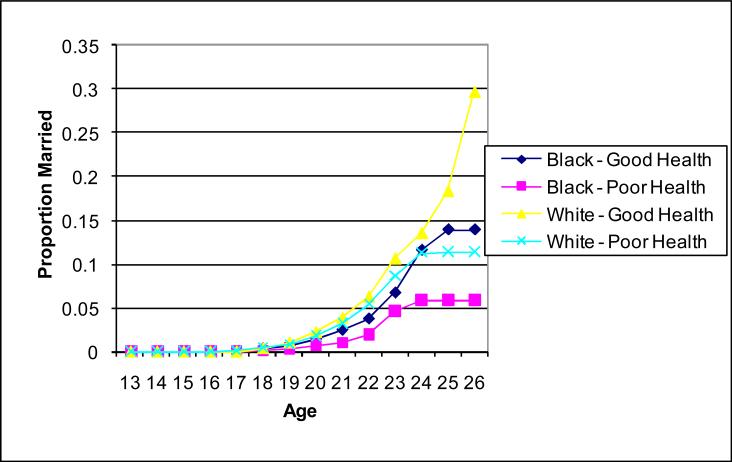
Because existing research indicates that those with better physical and mental health and desirable health-related habits (such as abstinence from drinking, smoking, and other risk behaviors) are more likely to marry than individuals with inferior health profiles (Goldman 1993, 1994), we examine patterns of early marriage between Waves I and III by our composite health measure at WI to explore potential health selection into marriage by race and sex. We categorize our composite health measure into two groups: poor health describes those with two or more of the seven negative health outcomes; and good health represents those with one or no negative health outcomes (see top panel of Table 1). Figures 4 and 5 present the cumulative probability distributions of marriage by race and poor/good health status for females and males, respectively. Health selection into marriage appears to operate differently by race for women. For white women, health status in adolescence does not significantly differentiate entry into marriage until the mid-20s, when those in poor health begin marrying at higher rates than those in good health. On the other hand, African American women in poor health are less likely to marry compared to their healthier peers across the entire age range. For men, a more consistent pattern emerges; those in good health are more likely to enter into marital unions than those with poor health.
Figure 4.
Cumulative proportion of females married by age 26 by race and health status
Figure 5.
Cumulative proportion of males married by age 26 by race and health status
MARRIAGE, COHABITATION AND HEALTH
Table 3 presents the bivariate relationships between marriage and cohabitation with each of our seven health outcomes at Wave III by race and sex. These results are primarily descriptive and represent both potential selection and protective effects of marriage (and cohabitation). We will control for potential health selection into marriage (and cohabitation) to isolate protective effects in the second stage of analysis below (following equation 1). We focus on the marriage effects first and limit our discussion to results that are statistically significant. Early marriage is associated with both potential health benefits and deficits for both whites and African Americans, though there are more effects for whites. Among white women and men, body weight is higher and physical activity lower at Wave III among those who marry between Wave I and Wave III compared to those who do not marry. However, married white women and men have lower levels of binge drinking and marijuana use and, among white women, cigarette smoking, indicating protective effects of marriage. Among African American men and women who marry by Wave III, there is no statistically significant association with BMI, although for African American women but not African American men, marriage is associated with lack of physical activity as it was for white men and women. African American women who marry, but not African American men, have lower levels of binge drinking and marijuana use. The overall beneficial effects of marriage that are more evident for whites but not African Americans is furthermore seen in the significant association between marriage and our composite health measure, indicating that marriage is associated with less health problems and health risk behavior.
Table 3.
Relationship between marriage (cohabitation) and health at WIII by sex and race
| Marriage | Cohabitation | |||||||
|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | |||||
| Black | White | Black | White | Black | White | Black | White | |
| Physical Health | ||||||||
| BMI | 0.641 | 2.098*** | 1.079 | 1.196*** | 1.492* | 0.489 | 0.312 | 0.246 |
| 0.768 | 0.367 | 1.079 | 0.359 | 0.582 | 0.325 | 0.460 | 0.260 | |
| Poor self-reported health | 0.065 | -0.019 | 0.094 | -0.022 | 0.141 | 0.228*** | 0.199** | 0.169*** |
| 0.116 | 0.047 | 0.199 | 0.046 | 0.076 | 0.042 | 0.069 | 0.036 | |
| Mental Health | ||||||||
| Depression index | 0.152 | -0.062 | 0.162 | -0.153 | 0.373* | 0.386*** | 0.392* | 0.160** |
| 0.254 | 0.085 | 0.286 | 0.098 | 0.158 | 0.068 | 0.156 | 0.058 | |
| Risk Behaviors | ||||||||
| Binge drinking episodes | -3.640* | -12.939*** | 5.242 | -17.764*** | 2.079 | -1.002 | 4.850 | -2.636 |
| 1.659 | 1.107 | 10.878 | 2.934 | 1.969 | 1.678 | 4.264 | 2.668 | |
| Cigarettes smoked per day | 0.664 | -1.429* | 0.428 | 0.104 | 3.956*** | 6.748*** | 3.891** | 5.320*** |
| 1.379 | 0.681 | 1.592 | 0.975 | 0.851 | 0.660 | 1.103 | 0.707 | |
| Marijuana Usage | -1.723* | -1.513*** | -2.105 | -4.670*** | 2.499 | 1.487*** | 3.181* | 2.007* |
| 0.695 | 0.370 | 1.568 | 0.640 | 1.431 | 0.363 | 1.346 | 0.907 | |
| Lack of Physical Activity | 0.443** | 0.464*** | 0.395 | 0.418** | 0.027 | 0.541*** | -0.076 | 0.240 |
| 0.166 | 0.094 | 0.377 | 0.150 | 0.142 | 0.083 | 0.243 | 0.130 | |
| Composite Health Measure | 0.091 | -0.291*** | 0.277 | -0.246* | 0.539*** | 0.596*** | 0.440** | 0.466*** |
| 0.136 | 0.074 | 0.260 | 0.104 | 0.087 | 0.056 | 0.146 | 0.060 | |
| N | 1371 | 3456 | 1109 | 3222 | 1371 | 3456 | 1109 | 3222 |
Data are weighted.
Standard errors listed below coefficients
significant at .05 level
significant at .01 level
significant at .001 level
Cohabitation does not seem to have positive health effects for either white or African American women and men. Among females, cohabitation between Waves I and III is associated with higher BMI, depression and cigarette smoking for African Americans and with poorer self-reported health, higher depression, cigarette smoking and marijuana use for whites, compared to females who did not cohabit. The higher BMI for African American females who cohabited is not small. An increase in 1.5 kg/m-squared for the average American adult female, with a height of 5’4” and a weight of 163 pounds (BMI = 28), is equivalent to a weight gain of 9 pounds (McDowell et al. 2005). Among men, cohabitation is associated with worse self-reported health, higher depression, cigarette smoking and marijuana usage for both African American and white men. Results on the composite health measure indicate that cohabitation between Waves I and III is associated with poorer health status at Wave III for both African American and white men and women.
We now move to an analysis of potential protective effects of marriage on the seven health outcomes for each race and sex group. Tables 4-7 present results from our lagged dependent variable regression predicting health in young adulthood (WIII) including baseline health (at WI) on the right-hand-side of the regression equation. We present these results by race and sex. There are some racial differences in the role of early marriage, but the effect of early marriage on health overall is weaker in the regression analysis than in the bivariate analysis, presumable because we control for health selection into marriage. Not surprisingly, baseline health is the strongest predictor of young adult health. For African American women (see Table 4) early marriage is predictive only of increasing BMI (by 1.2 points). For African American men, early marriage is associated with increases in BMI, depression, and as a result, an increase in the composite health measure, indicating marriage tends to increase the number of harmful health behaviors. (see Table 5). Cohabitation is associated with increased smoking for African American females and increased smoking, depression and marijuana use for African American males. In sum for African Americans, early marriage results in weight gain for both men and women and increases depression and poor composite health scores for men. For African Americans cohabitation protects health even less. While cohabitation does not impact BMI for either African American men or women, it does increase smoking for women and depression, smoking, and marijuana use for men. Early union formation overall seems to negatively impact health for African Americans reflected by the finding that the composite health score, capturing the number of poor health indicators, increases following marriage for an men and following cohabitation for African American men and women.
Table 4.
Regression results for black women (N=1371)
| Variable | BMI | Poor self-reported health | Depression | Binge drinking | Smoking | Lack of physical activity | Marijuana use | Composite health |
|---|---|---|---|---|---|---|---|---|
| HEALTH AT WI | 1.126*** | 0.326*** | 0.143*** | 0.043 | 0.603*** | 0.114*** | 0.921 | 0.264*** |
| 0.057 | 0.028 | 0.035 | 0.047 | 0.122 | 0.028 | 0.492 | 0.037 | |
| MARRIED BEWEEN WI AND WIII | 1.628* | 0.067 | 0.159 | -3.364 | 3.151 | 0.391 | 0.175 | 0.295 |
| 0.641 | 0.144 | 0.320 | 2.553 | 1.653 | 0.219 | 1.120 | 0.165 | |
| COHABITATION BETWEEN WI AND WIII | 0.636 | 0.047 | 0.195 | 2.686 | 4.082* | -0.070 | 2.472 | 0.398*** |
| 0.499 | 0.086 | 0.245 | 2.092 | 1.367 | 0.195 | 1.496 | 0.110 | |
| RELATIONSHIP DURATION | 0.004 | 0.006 | 0.006 | -0.074 | -0.021 | -0.005 | 0.026 | 0.002 |
| 0.017 | 0.003 | 0.007 | 0.123 | 0.039 | 0.008 | 0.041 | 0.003 | |
| INDIVIDUAL LEVEL CONTROLS | ||||||||
| Low family SES at WI | -0.025 | -0.019 | 0.116 | 0.591 | 0.207 | 0.115 | 0.137 | -0.003 |
| 0.252 | 0.036 | 0.082 | 1.284 | 0.230 | 0.092 | 0.356 | 0.050 | |
| Low religiosity at WI | 0.590 | 0.005 | -0.024 | -1.934 | 2.647** | -0.160 | -3.477 | 0.089 |
| 0.585 | 0.115 | 0.176 | 2.225 | 0.819 | 0.249 | 2.832 | 0.110 | |
| Birth between WI and WIII | 0.405 | -0.070 | 0.166 | -1.128 | -0.564 | 0.276 | -3.327 | 0.022 |
| 0.480 | 0.082 | 0.161 | 2.605 | 0.784 | 0.161 | 1.786 | 0.098 | |
| Age at WI | -0.462*** | -0.035 | -0.091* | 1.169 | -0.315 | -0.041 | 0.258 | -0.063* |
| 0.127 | 0.019 | 0.041 | 0.777 | 0.210 | 0.036 | 0.314 | 0.029 | |
| PEER LEVEL SES | ||||||||
| High % parent HS or less: peer | 0.212 | 0.131 | -0.044 | -2.984 | -0.183 | -0.023 | 1.660 | 0.035 |
| 0.600 | 0.076 | 0.172 | 3.915 | 0.753 | 0.177 | 1.110 | 0.107 | |
| High % single parent: peer | -0.120 | -0.047 | 0.155 | 0.078 | 1.338* | -0.242 | 0.279 | -0.028 |
| 0.498 | 0.083 | 0.138 | 2.793 | 0.619 | 0.153 | 1.013 | 0.103 | |
| No friends | 1.036 | 0.018 | 0.077 | -2.792 | 0.889 | -0.181 | -1.308 | -0.036 |
| 0.669 | 0.133 | 0.183 | 4.714 | 0.948 | 0.314 | 0.933 | 0.151 | |
| SCHOOL LEVEL SES | ||||||||
| High % parent HS or less: school | 0.098 | -0.007 | -0.046 | 7.556 | 1.029 | -0.158 | -1.230 | 0.093 |
| 0.445 | 0.100 | 0.180 | 4.386 | 0.838 | 0.204 | 0.965 | 0.091 | |
| High % single parent: school | 0.448 | -0.019 | -0.041 | -2.840 | -1.334 | 0.129 | -1.491 | -0.134 |
| 0.432 | 0.086 | 0.172 | 4.396 | 0.896 | 0.234 | 0.823 | 0.103 | |
| NEIGHBORHOOD LEVEL SES | ||||||||
| High % parent less than HS: neighborhood | -0.294 | -0.030 | 0.261 | 0.427 | -0.061 | -0.070 | 3.795** | 0.053 |
| 0.363 | 0.087 | 0.156 | 3.107 | 0.722 | 0.210 | 1.247 | 0.103 | |
| High % female headed household: neighborhood | 0.836* | 0.064 | -0.274 | 3.321 | 0.964 | -0.186 | -0.714 | 0.018 |
| 0.384 | 0.093 | 0.169 | 2.814 | 0.766 | 0.186 | 0.924 | 0.121 | |
| Low racial heterogeneity | 1.391* | -0.020 | -0.283 | -2.128 | 1.313 | 0.153 | -1.517 | 0.162 |
| 0.656 | 0.096 | 0.244 | 2.297 | 2.551 | 0.123 | 1.218 | 0.164 | |
| Urban tract | -1.240** | -0.029 | 0.294 | 1.473 | 0.922 | 0.037 | 3.069** | 0.136* |
| 0.371 | 0.071 | 0.136 | 2.558 | 0.583 | 0.177 | 1.112 | 0.068 |
Data are weighted.
Standard errors listed below coefficients
significant at .05 level
significant at .01 level
significant at .001 level
Table 7.
Regression results for white men (N=3222)
| Variable | BMI | Poor self-reported health | Depression | Binge drinking | Smoking | Lack of physical activity | Marijuana use | Composite health |
|---|---|---|---|---|---|---|---|---|
| HEALTH AT WI | 1.023*** | 0.302*** | 0.205*** | 0.173*** | 0.548*** | 0.129*** | 0.259 | 0.344*** |
| 0.029 | 0.024 | 0.027 | 0.040 | 0.031 | 0.013 | 0.201 | 0.020 | |
| MARRIED BEWEEN WI AND WIII | 0.491 | 0.007 | -0.056 | -10.984** | 2.258* | 0.348 | -1.555 | -0.007*** |
| 0.325 | 0.071 | 0.117 | 3.962 | 1.053 | 0.237 | 1.211 | 0.121 | |
| COHABITATION BETWEEN WI AND WIII | -0.089 | 0.108* | 0.072 | 0.983 | 3.426*** | 0.095 | 3.073** | 0.329 |
| 0.213 | 0.042 | 0.077 | 3.986 | 0.804 | 0.183 | 1.096 | 0.078 | |
| RELATIONSHIP DURATION | 0.004 | 0.000 | -0.003 | -0.134 | -0.021 | -0.003 | -0.064 | -0.003 |
| 0.008 | 0.002 | 0.002 | 0.118 | 0.022 | 0.006 | 0.041 | 0.002 | |
| INDIVIDUAL LEVEL CONTROLS | ||||||||
| Low family SES at WI | -0.083 | 0.023 | 0.058 | -4.089** | 0.314 | 0.107 | 0.454 | -0.034 |
| 0.099 | 0.019 | 0.035 | 1.421 | 0.356 | 0.066 | 0.486 | 0.032 | |
| Low religiosity at WI | -0.196 | 0.090** | -0.060 | 7.318* | 1.489* | 0.105 | 1.207 | 0.152** |
| 0.155 | 0.033 | 0.061 | 3.009 | 0.596 | 0.122 | 0.785 | 0.054 | |
| Age at WI | -0.228*** | 0.000 | -0.035 | -1.516* | -1.290*** | -0.007 | -0.501 | -0.100*** |
| 0.052 | 0.010 | 0.021 | 0.781 | 0.168 | 0.036 | 0.285 | 0.021 | |
| PEER LEVEL SES | ||||||||
| High % parent HS or less: peer | -0.165 | 0.054 | -0.017 | 3.102 | 1.168 | 0.147 | 1.288 | 0.030 |
| 0.197 | 0.047 | 0.111 | 3.917 | 0.947 | 0.191 | 1.067 | 0.078 | |
| High % single parent: peer | -0.231 | -0.002 | 0.176* | 5.416 | -0.078 | 0.062 | 0.770 | 0.053 |
| 0.195 | 0.042 | 0.090 | 3.744 | 0.726 | 0.157 | 1.110 | 0.078 | |
| No friends | 0.032 | 0.094* | 0.069 | -1.454 | -0.581 | 0.203 | 0.811 | -0.045 |
| 0.163 | 0.044 | 0.093 | 4.044 | 0.628 | 0.164 | 0.994 | 0.068 | |
| SCHOOL LEVEL SES | ||||||||
| High % parent HS or less: school | 0.078 | -0.001 | -0.002 | -8.796* | 0.392 | -0.171 | -0.211 | -0.057 |
| 0.183 | 0.052 | 0.093 | 4.026 | 0.703 | 0.193 | 1.017 | 0.068 | |
| High % single parent: school | 0.297 | 0.055 | -0.131 | -2.928 | -1.525 | 0.177 | -1.137 | -0.107 |
| 0.282 | 0.060 | 0.105 | 3.861 | 0.784 | 0.197 | 1.060 | 0.083 | |
| NEIGHBORHOOD LEVEL SES | ||||||||
| High % parent less than HS: neighborhood | 0.212 | 0.006 | -0.120 | -6.675 | 0.174 | -0.131 | -0.534 | -0.005 |
| 0.277 | 0.057 | 0.102 | 3.736 | 0.805 | 0.205 | 0.985 | 0.089 | |
| High % female headed household: neighborhood | 0.018 | 0.117* | 0.102 | -0.773 | -0.098 | -0.017 | -2.438* | 0.009 |
| 0.296 | 0.054 | 0.117 | 4.615 | 0.851 | 0.190 | 1.162 | 0.093 | |
| low racial heterogeneity | 0.345* | 0.003 | -0.011 | -0.937 | -0.526 | 0.268 | -1.853* | -0.017 |
| 0.171 | 0.036 | 0.067 | 2.813 | 0.635 | 0.141 | 0.756 | 0.060 | |
| Urban tract | 0.170 | -0.096* | 0.086 | -4.985 | -0.603 | -0.025 | 0.204 | 0.027 |
| 0.198 | 0.041 | 0.080 | 2.837 | 0.501 | 0.138 | 0.867 | 0.071 |
Data are weighted.
Standard errors listed below coefficients
significant at .05 level
significant at .01 level
significant at .001 level
Table 5.
Regression results for black men (N=1109)
| Variable | BMI | Poor self-reported health | Depression | Binge drinking | Smoking | Lack of physical activity | Marijuana use | Composite health |
|---|---|---|---|---|---|---|---|---|
| HEALTH AT WI | 1.008*** | 0.298*** | 0.244*** | 0.087 | 0.430*** | 0.148*** | 0.004 | 0.313*** |
| 0.065 | 0.047 | 0.055 | 0.055 | 0.070 | 0.029 | 0.007 | 0.041 | |
| MARRIED BEWEEN WI AND WIII | 1.982*** | 0.073 | 0.692* | 7.792 | 3.863 | 0.008 | 2.599 | 0.659* |
| 0.505 | 0.183 | 0.325 | 12.773 | 2.170 | 0.434 | 1.529 | 0.316 | |
| COHABITATION BETWEEN WI AND WIII | 0.233 | 0.055 | 0.611** | 6.401 | 4.369** | -0.348 | 5.523** | 0.473** |
| 0.344 | 0.097 | 0.183 | 4.746 | 1.339 | 0.314 | 1.726 | 0.141 | |
| RELATIONSHIP DURATION | -0.025* | 0.004 | -0.010 | -0.117 | -0.018 | 0.001 | -0.101** | -0.005 |
| 0.010 | 0.004 | 0.005 | 0.214 | 0.053 | 0.011 | 0.035 | 0.004 | |
| INDIVIDUAL LEVEL CONTROLS | ||||||||
| Low family SES at WI | -0.311* | -0.038 | 0.083 | 0.536 | 0.423 | 0.012 | 0.397 | -0.050 |
| 0.139 | 0.042 | 0.059 | 2.288 | 0.456 | 0.114 | 0.802 | 0.047 | |
| Low religiosity at WI | -0.297 | -0.065 | -0.082 | 2.055 | -1.268 | -0.087 | 1.575 | -0.177 |
| 0.337 | 0.105 | 0.149 | 6.960 | 1.143 | 0.407 | 1.905 | 0.111 | |
| Age at WI | -0.186 | 0.007 | -0.117** | 2.144 | -0.653* | 0.048 | -0.194 | -0.074* |
| 0.101 | 0.024 | 0.043 | 1.327 | 0.310 | 0.062 | 0.333 | 0.030 | |
| PEER LEVEL SES | ||||||||
| High % parent HS or less: peer | 0.294 | 0.142* | 0.133 | -2.749 | -1.048 | 0.697 | -1.901 | 0.113 |
| 0.376 | 0.097 | 0.172 | 6.616 | 1.496 | 0.314 | 1.303 | 0.132 | |
| High % single parent: peer | -0.068 | 0.000 | 0.102 | 3.719 | 0.862 | 0.262 | -1.218 | 0.261 |
| 0.380 | 0.085 | 0.137 | 6.235 | 1.131 | 0.373 | 1.994 | 0.147 | |
| No friends | 0.034 | 0.011 | 0.118 | -7.451 | -0.391 | -0.267 | -4.245 | -0.123 |
| 0.365 | 0.090 | 0.147 | 7.195 | 1.346 | 0.431 | 2.494 | 0.110 | |
| SCHOOL LEVEL SES | ||||||||
| High % parent HS or less: school | -0.483 | -0.004 | -0.095 | 1.972 | 1.146 | -0.363 | -0.309 | 0.004 |
| 0.466 | 0.083 | 0.146 | 7.456 | 1.288 | 0.383 | 1.643 | 0.157 | |
| High % single parent: school | 0.642 | -0.063 | -0.372*** | -6.284 | -1.211 | -0.649 | -1.500 | -0.267* |
| 0.380 | 0.075 | 0.096 | 5.145 | 1.396 | 0.367 | 1.459 | 0.129 | |
| NEIGHBORHOOD LEVEL SES | ||||||||
| High % parent less than HS: neighborhood | 0.315 | -0.068 | -0.079 | -8.753 | -0.093 | -0.059 | -0.945 | -0.027 |
| 0.321 | 0.060 | 0.155 | 5.791 | 1.071 | 0.223 | 1.099 | 0.111 | |
| High % female headed household: neighborhood | -0.098 | 0.031 | 0.072 | 7.112 | 2.096* | 0.347 | -0.055 | 0.091 |
| 0.354 | 0.085 | 0.171 | 5.033 | 0.999 | 0.285 | 1.216 | 0.131 | |
| Low racial heterogeneity | 0.255 | 0.205 | 0.498* | -11.342*** | 3.225* | 0.110 | -0.501 | 0.366* |
| 0.505 | 0.113 | 0.256 | 5.542 | 1.474 | 0.338 | 1.548 | 0.164 | |
| Urban tract | 0.480 | 0.039 | 0.006 | -8.227 | -1.026 | 0.430 | 1.622 | 0.120 |
| 0.375 | 0.077 | 0.130 | 5.098 | 1.065 | 0.272 | 0.826 | 0.123 |
Data are weighted.
Standard errors listed below coefficients
significant at .05 level
significant at .01 level
significant at .001 level
For white young adults, early marriage has mixed effects that are both beneficial and detrimental to their health. Early marriage is protective in that it significantly reduces binge drinking for both white women (Table 6) and white men (Table 7). However, early marriage also leads to increased BMI and decreased physical activity for white women (Table 6), and increased smoking among white men (Table 7). Perhaps because of the strong effects of marriage in reducing binge drinking, we also find a decrease in the composite harmful health score following marriage for both white men and women.
Table 6.
Regression results for white women (N=3456)
| Variable | BMI | Poor self-reported health | Depression | Binge drinking | Smoking | Lack of physical activity | Marijuana use | Composite health |
|---|---|---|---|---|---|---|---|---|
| HEALTH AT WI | 1.187*** | 0.338*** | 0.194*** | 0.056** | 0.508*** | 0.120*** | 0.174** | 0.305*** |
| 0.030 | 0.020 | 0.022 | 0.018 | 0.030 | 0.011 | 0.055 | 0.019 | |
| MARRIED BEWEEN WI AND WIII | 1.186** | -0.053 | 0.001 | -10.207*** | -0.398 | 0.295* | -0.592 | -0.247** |
| 0.334 | 0.060 | 0.116 | 1.635 | 0.990 | 0.134 | 0.531 | 0.089 | |
| COHABITATION BETWEEN WI AND WIII | -0.464 | 0.055 | 0.216* | 1.356 | 4.459*** | 0.266* | 1.258** | 0.318*** |
| 0.263 | 0.046 | 0.093 | 2.047 | 0.789 | 0.113 | 0.459 | 0.065 | |
| RELATIONSHIP DURATION | 0.025*** | 0.003* | 0.001 | 0.053 | 0.003 | 0.000 | 0.033 | 0.005* |
| 0.006 | 0.001 | 0.003 | 0.048 | 0.019 | 0.004 | 0.015* | 0.002 | |
| INDIVIDUAL LEVEL CONTROLS | ||||||||
| Low family SES at WI | 0.046 | 0.063** | 0.040 | -2.007** | 0.830* | 0.137** | -0.282 | 0.059** |
| 0.119 | 0.019 | 0.046 | 0.760 | 0.303 | 0.051 | 0.308 | 0.028 | |
| Low religiosity at WI | -0.184 | -0.010 | -0.067 | 0.298 | -0.467 | 0.082 | 1.098 | 0.038 |
| 0.196 | 0.039 | 0.077 | 1.888 | 0.500 | 0.087 | 0.569 | 0.060 | |
| Birth between WI and WIII | 0.492* | 0.026 | 0.244** | -2.739 | 0.681 | 0.340* | 0.068 | 0.016 |
| 0.228 | 0.045 | 0.091 | 1.888 | 0.697 | 0.132 | 0.638 | 0.065 | |
| Age at WI | -0.331*** | -0.051*** | -0.107*** | -1.072* | -0.925*** | -0.064 | -0.668*** | -0.135*** |
| 0.052 | 0.010 | 0.020 | 0.426 | 0.168 | 0.033 | 0.098 | 0.016 | |
| PEER LEVEL SES | ||||||||
| High % parent HS or less: peer | 0.491* | 0.127** | 0.021 | 0.315 | 1.092 | 0.079 | 0.309 | 0.189** |
| 0.212 | 0.039 | 0.088 | 1.868 | 0.560 | 0.114 | 0.462 | 0.066 | |
| High % single parent: peer | 0.154 | 0.079* | 0.012 | -0.161 | 0.569 | -0.151 | 0.786* | -0.019 |
| 0.237 | 0.036 | 0.080 | 1.858 | 0.582 | 0.117 | 0.360 | 0.054 | |
| No friends | 0.125 | 0.037 | 0.083 | -3.494 | 2.010** | 0.234 | 0.358 | 0.085 |
| 0.269 | 0.049 | 0.089 | 2.160 | 0.712 | 0.124 | 0.420 | 0.076 | |
| SCHOOL LEVEL SES | ||||||||
| High % parent HS or less: school | -0.061 | -0.045 | -0.116 | -3.651* | 0.571 | -0.031 | 0.413 | -0.013 |
| 0.241 | 0.040 | 0.082 | 1.885 | 0.711 | 0.133 | 0.486 | 0.058 | |
| High % single parent: school | -0.213 | 0.018 | 0.161 | -0.240 | 0.659 | 0.352** | 0.125 | 0.024 |
| 0.326 | 0.057 | 0.105 | 2.285 | 0.690 | 0.131 | 0.556 | 0.081 | |
| NEIGHBORHOOD LEVEL SES | ||||||||
| High % parent less than HS: neighborhood | 0.100 | 0.028 | -0.153 | -2.519 | 1.065 | 0.118 | -0.661 | 0.015 |
| 0.354 | 0.059 | 0.137 | 2.627 | 1.052 | 0.135 | 0.432 | 0.093 | |
| High % female headed household: neighborhood | -0.048 | -0.110 | 0.030 | 1.097 | -0.690 | -0.076 | 0.406 | -0.011 |
| 0.292 | 0.056 | 0.108 | 2.335 | 0.849 | 0.143 | 0.438 | 0.072 | |
| Low racial heterogeneity | -0.090 | 0.016 | 0.048 | 0.939 | 0.823 | -0.160 | -0.274 | 0.045 |
| 0.199 | 0.039 | 0.068 | 1.599 | 0.568 | 0.130 | 0.361 | 0.054 | |
| Urban tract | -0.029 | 0.121** | 0.123 | 0.811 | 0.682 | -0.083 | 0.256 | 0.101 |
| 0.180 | 0.040 | 0.070 | 1.681 | 0.571 | 0.107 | 0.319 | 0.058 |
Data are weighted.
Standard errors listed below coefficients
significant at .05 level
significant at .01 level
significant at .001 level
For both white men and women, cohabitation is associated with increases in multiple negative health outcomes. These include depression, smoking, reduced physical activity, marijuana use, and not surprisingly, an increase in the poor health composite score. Similar to the findings for African Americans, once prior health at WI is accounted for, protective effects of early marriage on health are minimal.
Our multi-level SES measures are only weakly predictive of health in young adulthood for African-Americans. Among African American women, significant predictors are found for neighborhood-level SES measures when examining BMI and marijuana use; analyses of other health outcomes reveal few significant results. More specifically, African American females living in neighborhoods with a high proportion of female-headed households and low racial heterogeneity have higher BMIs than those who do not live in such environments. However, African American females living in an urban tract have lower BMIs than those living in suburban or rural areas. For African American males, low racial heterogeneity is predictive of several negative health outcomes. Low racial heterogeneity is associated with increases in smoking and depression but decreases in binge drinking. Most individual, peer, and school level measures of SES are insignificant.
Several individual-level SES and control variables are relevant for health among white women. Low SES is associated with poor self-reported health and increased smoking and decreased physical activity. Oddly, low SES is also associated with decreased binge drinking in young adulthood. Several peer-level SES measures significantly predict negative health as well. Notably, for white women, having a high percentage of friends whose parents have a high school education or less is associated with poor a health composite measure and higher BMI in young adulthood. For white males, neighborhood SES influences BMI, poor self-reported health and marijuana usage. Peer SES influences depression and like white women, school SES influences binge drinking. In all analyses, but especially for whites, there is a consistent age effect such that an older age at Wave I is associated with less change in health outcomes between Wave I and Wave III. This finding suggests that health and health behavior stabilizes as adolescents enter their late teens.
DISCUSSION
The relationship between early marriage and health among African Americans in the transition to adulthood is a crucial and understudied stage in the life course with implications for future adult attainments and health (Call et al. 2002; Schulenberg et al. 1997). Early marriages have been linked to higher rates of dissolution (Teachman 1983) and lower subsequent earnings (Teachman, Polonko & Scanzoni 1986). Previous research examining the relationship between early first marriage and health has focused on risk behaviors given their saliency in young adulthood (Bachman et al. 1997; Curran Muthén and Harford 1998; Duncan, Wilkerson and England 2006).
This research focuses on the young adult stage of the life cycle, when health and marriage trajectories are first set and contributes new data on the relationship between marriage and physical health, marriage and mental health, and linkages between marriage and critical health behaviors (obesity, physical activity) that influence future health processes and cardiovascular disease risk. This paper adds to previous research that examines the relationship between early marriage and health by using a longitudinal dataset of a recent cohort of adolescents, examining dimensions of health beyond risk behaviors, controlling for factors known to account for selection into marriage, and controlling for multiple levels of SES known to influence both marriage and health.
Lagged dependent variable regression models indicate a strong link in the trajectory between adolescent health status and young adult health status that is only marginally affected by changes in union status through marriage or cohabitation. After controlling for prior health status, early marriage has no protective effect for African Americans and mixed effects for whites. Early marriage is protective for whites only with respect to binge drinking. There is no binge drinking protection for African Americans. For African American men and women and white women, early marriage is associated with increased BMI. There is an increase for white men as well, but it does not reach statistical significance. For white women, early marriage is also associated with decreased physical activity.
Early marriage also led to increased depression for African American men and increased smoking for white men. This increase in depression for African American men is interesting. Because we are examining the effects of early marriage on health, marriage may serve as an additional stressor for African American male young adults. Indeed, our finding of neighborhood heterogeneity on depression among African American men is consistent with other work indicating that neighborhood racial segregation is associated with poor mental health in adolescence (Aneshensel and Sucoff 1996). It is likely that young African American males remain in these neighborhoods when they marry, and lack the support of other married men in their local surroundings or access to good jobs with which to support their family. These ideas can be tested using the Add Health data in future research, because geo-coded census data are linked to WII and WIII surveys. Perhaps the most informative aspect of this study's findings is that while marriage did not have the expected protective effect on young adult health, for both African Americans and whites, cohabitation was associated with increases in multiple negative health outcomes.
Our analysis examined multiple dimensions of health including physical and mental health in addition to risk behavior. We found that the marriage and health relationship differed greatly depending on the health indicator examined, and that these associations also varied by race and sex. For example, although early marriage is related to levels of smoking and binge drinking for whites, these relationships were not found for African Americans. However, early marriage was associated with increases in BMI across race and sex. Our findings highlight the importance of using multiple health indicators when examining the marriage health relationship, especially if researchers are interested in studying racial differences. Although specific health indicators that were salient for whites were not for African Americans in our study, it will be important to continue to investigate race-relevant health outcomes to better understand the marriage-health relationship for African Americans. Research should examine other health indicators including stress measures, such as cortisol levels, preterm births, sleep patterns, and other dimensions of mental health.
Our findings that marriage decreased binge drinking for white young adults replicate previous research using longitudinal models to examine the relationship between marriage and health (Bachman et al. 1997; Curran, Muthén and Harford 1998; Duncan, Wilkerson and England 2006; Waldron, Hughes and Brooks 1996). There are several possible reasons why early marriage does not have the same effect on binge drinking for African Americans as it does for whites. The first is that binge drinking patterns in Wave I and Wave III are different for African American men and women than for white men and women. At Wave I African American adolescents report more binge drinking than do white adolescents. Between the waves binge drinking increases for white young adults but decreases or stays the same for African Americans. The different drinking patterns between African Americans and whites may partly explain the differential marriage effect on binge drinking.
In addition, the weaker effects of early marriage on health could be explained by the fact that early marriage patterns are also different for whites and African Americans, reflecting the diversity of African American life in general. Early marriage may not be a salient or viable option for African Americans. African Americans face multiple stressors in their social contexts that can deter successful transitions into adulthood. Marriage might be seen as a situation that will cause more stress rather than increase stability, especially given the higher unemployment and incarceration rates of African American young men (Anderson 1999, 1994, 1999; Edin and Kefalas 2000, 2005). Marriage may not provide avenue for increased economic security or family stability at these young ages.
Beyond marriage, African Americans have other important forms of social support in their community that can provide them with economic security and social stability. Previous research has detailed extensive kinship networks in the African American community that provide child care, residence and other forms of in-kind and emotional support (Burton and Sorensen 1993; Stack 1974). The availability of other forms of social support may make early marriage less salient among adolescents and young adults. In addition, African American women are socialized to be independent and to be able to take care of themselves (Browning and Miller 1999), which might also make early marriage a less viable option.
Our most robust finding is the strong relationship between early marriage and BMI for African American and white women and African American men. Although obesity deters entry into early marriage, once an individual is married, his/her BMI increases. These findings support previous longitudinal studies that find a relationship between marriage and increases in body weight (e.g., Jeffery and Rick 2002). One possible explanation is that marriage increases opportunities and cues for eating. Married people are more likely to share meals together and, therefore, encourage each other's increased food intake (Jeffery and Rick 2002). Research also indicates that marriage is associated with decreases in physical activity. Work and family roles leave less time for exercise for both married men and women (e.g. Nomaguchi and Bianchi). Obesity has become a particularly significant health issue for young Americans (Kumanyika and Grier 2006). Indeed, the transition period from adolescence to young adulthood has been shown to be a lifecycle period of particular risk for the development of obesity (Lee et al. 2009; McTigue, Garrett and Popkin, 2002). These results highlight that early marriage can have adverse as well as positive effects on health. While BMI in adolescence is more predictive of BMI in young adulthood than marriage, the positive impact of marriage on BMI should still be taken seriously. High BMIs at these young ages sets up a negative health trajectory leading to high BMI in young adulthood, increasing the likelihood of obesity in later adulthood. Trajectories of obesity coming out of adolescence are related to a number of diseases including type-2 diabetes and cardiovascular disease in adulthood, which are especially salient for African-American populations.
This study, which focuses on the transition to adulthood, informs our understanding of the marriage-health relationship for African Americans. First, it provides us with information on the unique health issues facing young adults during this critical stage in the life course. Second, our study highlights the effects of early marriage, before age 26, and provides insight into how marriage may affect health for young African American adults. Third, we are able to determine the influence of cohabitation on health as distinct from the influence of marriage. This is an important addition given the high frequency of cohabitation in this cohort of young people. Finally, our work sheds light on the array of social factors that influence young adult behaviors, setting the stage for union and health trajectories in the life course.
Acknowledgments
We gratefully acknowledge research support from the National Institute of Child Health and Human Development to Harris through grant 3 P01 HD31921 as part of the Add Health program project. This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (addhealth@unc.edu).
Footnotes
The standard CES-D is a 20-item self-report scale that measures depressive symptoms (Radloff 1977). We use three questions from an abbreviated, five-item version of the CES-D that can be used for cross-cultural comparisons among adolescents living in the U.S (Perreira et al. 2005).
Contributor Information
Kathleen Mullan Harris, Carolina Population Center and Department of Sociology University of North Carolina at Chapel Hill 505 University Square East 123 W. Franklin Street Chapel Hill, North Carolina 27516 kathie_harris@unc.edu Phone: 919-966-5560 or 919-962-1388 Fax: 919-966-6638.
Hedwig Lee, School of Public Health and Department of Epidemiology University of Michigan 1415 Washington Heights Ann Arbor, MI 48109 hedylee@umich.edu Phone: 734-615-9215 Fax: 734-763-5706.
Felicia Yang DeLeone, Carolina Population Center University of North Carolina at Chapel Hill 302-E University Square East 123 W. Franklin Street Chapel Hill, North Carolina 27516 felicia.deleone@unc.edu Phone: 919-843-5548 Fax: 919-962-7217.
REFERENCES
- Allison Paul D. Change scores as dependent variables in regression analysis. In: Clogg CC, editor. Sociological Methodology. Basil Blackwell; Oxford: 1990. pp. 93–114. [Google Scholar]
- Aneshensel Carol S., Sucoff Clea A. The Neighborhood Context of Adolescent Mental Health. Journal of Health and Social Behavior. 1996;37(4):293–310. [PubMed] [Google Scholar]
- Andersen RE, Crespo CH, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of Physical Activity and Television Watching with Body Weight and Level of Fatness among Children: Results from the third National Health and Nutrition Examination Survey. Journal of the American Medical Association. 1998;279(12):938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- Anderson Elijah. The Code of the Street: Decency, Violence, And The Moral Life Of The Inner City. W.W. Norton; New York: 1999. [Google Scholar]
- Anderson Elijah. Sex Codes and Family Life among Inner-City Youth. The Annals of the American Academy of Political and Social Science. 1989;501(1):59–78. [Google Scholar]
- Bachman JG, Wadsworth KN, O'Malley PM, Johnson LD, Schulenberg JE. Smoking, Drinking, and Drug Use in Young Adulthood. Lawrence Erlbaum Associates; Mahwah, NJ: 1997. [Google Scholar]
- Bachman JG, O'Malley PM, Schulenberg JE, Johnston LD, Bryant AL, Merline AC. The Decline of Substance Use in Young Adulthood: Changes in Social Activities, Roles, and Beliefs. Lawrence Erlbaum Associates; Mahwah, NJ: 2002. [Google Scholar]
- Ben-Shlomo Yoav, Kuh Diana. A Life Course Approach to Chronic Disease Epidemiology: Conceptual Models, Empirical Challenges and Interdisciplinary Perspectives. International Journal of Epidemiology. 2002;31:285–293. [PubMed] [Google Scholar]
- Bronfrenbrenner Urie. Making Human Beings Human: Bioecological Perspectives on Human Development. Sage; Thousand Oaks, CA: 2005. [Google Scholar]
- Bronfrenbrenner Urie, Morris Pamela. The Ecology of Developmental Processes. In: Damon W, Lerner R, editors. Handbook of Child Psychology: Vol. 1: Theoretical Models of Human Development. 5th ed. Wiley; New York: 1998. pp. 992–1028. [Google Scholar]
- Browning S, Miller R. Marital Messages: The Case of Black Women and Their Children. Journal of Family Issues. 1999;20(5):633–647. [Google Scholar]
- Burton Linda M., Sorensen S. Temporal Dimensions of Intergenerational Caregiving in African-American Multigeneration Families. In: Zarit SH, Pearlin LI, Schaie KW, editors. Caregiving Systems: Informal and Formal Helpers. Erlbaum Associates; 1993. pp. 47–66. [Google Scholar]
- Call KT, Riedel AA, Hein K, McLoyd V, Petersen A, Kipke M. Adolescent Health and Well-Being in the 21st Century: A Global Perspective. Journal of Research on Adolescence. 2002;12(1):69–98. [Google Scholar]
- Case Anne, Fertig Angela, Paxson Christina. The Lasting Impact of Childhood Health and Circumstance. Journal of Health Economics. 2005;24(2):365–389. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Clarkwest Andrew. Premarital Characteristics, Selection into Marriage, and African American Marital Disruption. Journal of Comparative Family Studies. 2006;37:361–380. [Google Scholar]
- Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a Metabolic Syndrome Phenotype in Adolescents. Archives of Pediatrics & Adolescent Medicine. 2003;157:821–827. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- Cox DR. Regression Models and Life Tables (with discussion). Journal of the Royal Statistical Society Series B (Methodological) 1972;34(2):187–220. [Google Scholar]
- Curran PJ, Muthen BO, Harford TC. The Influence of Changes in Marital Status on Developmental Trajectories of Alcohol Use in Young Adults. Journal of Studies on Alcohol. 1998;59:647–58. doi: 10.15288/jsa.1998.59.647. [DOI] [PubMed] [Google Scholar]
- Duncan Greg, Wilkerson Bessie, England Paula. Cleaning Up Their Act: The Effects of Marriage and Cohabitation on Licit and Illicit Drug Use. Demography. 2006;43(4):691–710. doi: 10.1353/dem.2006.0032. [DOI] [PubMed] [Google Scholar]
- Edin K. How low-income single mothers talk about marriage. Social Problems. 2000;47(1):112–133. [Google Scholar]
- Edin K, Kefalas M. Promises I Can Keep: Why Poor Women Put Motherhood before Marriage. University of California Press; Berkeley, CA: 2005. [Google Scholar]
- Elder Glen H., Jr. The Life Course and Human Development. In: Lerner RM, Damon W, editors. Handbook of Child Psychology, Volume 1: Theoretical Models of Human Development. Wiley; New York: 1997. pp. 939–991. [Google Scholar]
- Elo IT, Preston SH. Effects of Early-Life Conditions on Adult Mortality: A Review. Population Index. 1992;58:186–212. [PubMed] [Google Scholar]
- Erikssen G. Physical Fitness and Changes in Mortality: The Survival of the Fittest. Sports Medicine. 2001;31(8):571–576. doi: 10.2165/00007256-200131080-00001. [DOI] [PubMed] [Google Scholar]
- Fuligni Andrew J., Hardway Christina. Preparing Diverse Adolescents for the Transition to Adulthood. The Future of Children. 14(2):99–119. 20054. [Google Scholar]
- Furstenberg Frank, F., Jr., Cook Thomas D., Eccles Jacquelynne, Elder Glenn H., Jr., Sameroff Arnold. Managing to Make It: Urban Families and Adolescent Success. University of Chicago Press; Chicago: 1999. [Google Scholar]
- Goldman Noreen. Marriage Selection and Mortality Patterns: Inferences and Fallacies. Demography. 1993;30(2):189–208. [PubMed] [Google Scholar]
- Goldman Noreen. Social Factors and Health: the Causation-Selection Issue Revisited. Proceedings of the National Academy of Sciences of the United States of America. 1994;91(4):1251–5. doi: 10.1073/pnas.91.4.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman Elizabeth, Hinden Beth R., Khandelwal Seema. Accuracy of Teen and Parental Reports of Obesity and Body Mass Index. Pediatrics. 2000;106(1):52–28. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- Gore S, Aseltine R, Colton ME, Lin B. Life After High School: Development, Stress, and Well-Being. In: Gotlib I, Wheaton B, editors. Stress and Adversity Over the Life Course. Cambridge University Press; NY, NY: 1997. pp. 197–214. [Google Scholar]
- Hagan John, Foster Holly. S/He's a Rebel: Toward a Sequential Stress Theory of Delinquency and Gendered Pathways to Disadvantage in Emerging Adulthood. Social Forces. 2003;82(1):53–86. [Google Scholar]
- Halfon Neal, Hochstein Miles. Life Course Health Development: an Integrated Framework for Developing Health, Policy, and Research. Milbank Quarterly. 2002;80:433–79. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris Kathleen Mullan, Florey Francesca, Tabor Joyce W., Bearman Peter S., Jones Jo, Udry J. Richard. [September 21, 2004];The National Longitudinal Study of Adolescent Health: Research Design. 2003 ( http://www.cpc.unc.edu/projects/addhealth/design.html.)
- Harris Kathleen Mullan, Gordon-Larsen Penny, Chantala Kim, Udry J. Richard. Longitudinal Trends in Race and Ethnic Disparities in Leading Health Indicators from Adolescence to Young Adulthood. Archives of Pediatrics and Adolescent Medicine. 2006;160:74–81. doi: 10.1001/archpedi.160.1.74. [DOI] [PubMed] [Google Scholar]
- Harris Kathleen Mullan, Cheng Mariah. Family Structure Role Models and the Context of Nonmarital Childbearing.. Paper presented at the annual meeting of the American Sociological Association; Philadelphia. August 13-16, 2005.2005. [Google Scholar]
- Hogan Dennis P., Astone Nan Marie. The Transition to Adulthood. Annual Review of Sociology. 1986;12:109–130. [Google Scholar]
- House James S., Williams David R. Understanding and Reducing Socioeconomic and Racial/Ethnic Disparities in Health. In: Smedley Brian D., Syme S. Leonard., editors. Promoting Health: Intervention Strategies from Social and Behavioral Research. National Academies Press; 2000. pp. 81–124. [PubMed] [Google Scholar]
- Iceland John Daniel, Weinberg H, Steinmetz Erika. U.S. Census Bureau, Series CENSR-3, U.S. Government Printing Office; Washington, DC: 2002. [September 21, 2008]. Racial and Ethnic Residential Segregation in the United States:1980-2000. ( http://www.census.gov/hhes/www/housing/housing_patterns/pdf/censr-3.pdf) [Google Scholar]
- James Sherman A., Fowler-Brown Angela, Raghunathan Trevillore E., Van Hoewyk John. Life-course Socioeconomic Position and Obesity in African American Women: The Pitt County Study. American Journal of Public Health. 2006;96:554–560. doi: 10.2105/AJPH.2004.053447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James Sherman A. Psychosocial and Environmental Factors in Black Hypertension. In: Hall WD, Shulman NB, Saunders E, editors. Hypertension in Blacks: Epidemiology Pathophysiology and Treatment. Year book Medical Publishers; 1985. 1985. pp. 132–143. [Google Scholar]
- Jeffery Robert W., Rick Allison M. Cross-Sectional and Longitudinal Associations between Body Mass Index and Marriage-Related Factors. Obesity Research. 2002;10:809–815. doi: 10.1038/oby.2002.109. [DOI] [PubMed] [Google Scholar]
- Johnson David. Two-Wave Panel Analysis: Comparing Statistical Methods for Studying the Effects of Transitions. Journal of Marriage and the Family. 2005;67:1061–75. [Google Scholar]
- Kawachi Ichiro, Berkman Lisa F. Neighborhoods and Health. Oxford University Press; Urban Institute; New York: Washington, DC: 2003. [Google Scholar]
- Kumanyika Shiriki, Grier Sonya. Targeting Interventions for Ethnic Minority and Low-Income Populations. The Future of Children. 2006;16(1):187–20. doi: 10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- Lee H, Harris KM, Gordon-Larsen P. Life Course Perspectives on the Links Between Poverty and Obesity During the Transition to Young Adulthood. Population Research and Policy Review. 2009;28(4):505–532. doi: 10.1007/s11113-008-9115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch John, Smith George D. A Life Course Approach to Chronic Disease Epidemiology. Annual Review of Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- Mays Vickie M., Cochran Susan D., Barnes Namdi W. Race, Race-Based Discrimination, and Health Outcomes Among African Americans. Annual Review of Psychology. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell Margaret A., Fryar Cheryl D., Hirsch Rosemarie, Ogden Cynthia L. Anthropometric Reference Data for Children and Adults: U.S. Population, 1999–2002. [February 14, 2009];Advance Data from Vital and Health Statistics. 2005 ( http://www.cdc.gov/nchs/data/ad/ad361.pdf) [PubMed]
- McTigue Kathleen M, Garrett Joanne M., Popkin Barry M. The Natural History of Obesity: Weight Change in a Large US Longitudinal Survey. Annals of Internal Medicine. 2002;136:857–64. doi: 10.7326/0003-4819-136-12-200206180-00006. [DOI] [PubMed] [Google Scholar]
- Miller-Tutzauer C, Leonard KE, Windle M. Marriage and Alcohol Use: A Longitudinal Study of ‘Maturing Out.’. Journal of Studies on Alcohol. 1991;52:434–40. doi: 10.15288/jsa.1991.52.434. [DOI] [PubMed] [Google Scholar]
- Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in Blood Pressure Among Children and Adolescents. Journal of the American Medical Association. 2004;291(17):2107–2113. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- Nomaguchi Kei M., Bianchi Suzanne M. Exercise Time: Gender Differences in the Effects of Marriage, Parenthood, and Employment. Journal of Marriage and Family. 2004;66(2):413–430. [Google Scholar]
- Osgood Wayne D., Foster Michael E., Flanagan Constance, Ruth Gretchen R. On Your Own Without a Net: The Transition to Adulthood for Vulnerable Populations. University of Chicago Press; Chicago: 2005. [Google Scholar]
- Osypuk Theresa L., Galea Sandro, McArdle Nancy, Acevedo-Garcia Dolores. Quantifying Separate and Unequal Racial-Ethnic Distributions of Neighborhood Poverty in Metropolitan America. Urban Affairs Review OnlineFirst. 2009 doi: 10.1177/1078087408331119. published on February 4, 2009 as doi:10.1177/1078087408331119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patillo Mary. Black Picket Fences: Privilege and Peril among the Black Middle Class. University of Chicago Press; Chicago: 1999. [Google Scholar]
- Pattillo Mary. Black Middle-Class Neighborhoods. Annual Review of Sociology. 2005;31:305–29. [Google Scholar]
- Perreria Krista, Deeb-Sossa Natalia, Harris Kathleen Mullan, Bollen Kenneth. What Are We Measuring? An Evaluation of the CES-D Across Race, Ethnicity, and Immigrant Generation. Social Forces. 2005;83(4):1567–1601. [Google Scholar]
- Radloff Lenore. S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Schulenberg J, Maggs JL, Hurrelmann K. Negotiating Developmental Transitions During Adolescence and Young Adulthood: Health Risks and Opportunities. In: Schulenberg J, Maggs JL, Hurrelmann K, editors. Health Risks and Developmental Transitions During Adolescence. Cambridge University Press; Cambridge: 1997. pp. 1–19. [Google Scholar]
- Sellers Robert M., Caldwell Cleopatra H., Schmeelk-Cone Karen H., Zimmerman Marc A. Racial Identity, Racial Discrimination, Perceived Stress, and Psychological Distress among African American Young Adults. Journal of Health and Social Behavior. 2003;44(3):302–317. [PubMed] [Google Scholar]
- Settersten Richard A., Jr., Furstenberg Frank F., Jr., Rumbaut Rubén G. On the Frontier of Adulthood: Theory, Research, and Public Policy. University of Chicago Press; Chicago: 2004. [Google Scholar]
- Shanahan Michael J. Pathways to Adulthood in Changing Societies: Variability and Mechanisms in Life Course Perspective. Annual Review of Sociology. 2000;26:667–692. [Google Scholar]
- Sherry Bettylou, Jefferds Maria Elena, Grummer-Strawn Laurence M. Accuracy of Adolescent Self-report of Height and Weight in Assessing Overweight Status. Archives of Pediatrics and Adolescent Medicine. 2007;61(12):1154–1161. doi: 10.1001/archpedi.161.12.1154. [DOI] [PubMed] [Google Scholar]
- Teachman JD. Early Marriage, Premarital Fertility, and Marital Dissolution. Journal of Family Issues. 1983;4(1):105–126. doi: 10.1177/019251383004001006. [DOI] [PubMed] [Google Scholar]
- Teachman JD, Polonko KA, Scanzoni J. Family Demography: Recent Trends and Developments in the Field. In: Sussman MD, Steinmetx SK, editors. Handbook ofMarriage and the Family. Plenum Press; New York: 1986. pp. 3–36. [Google Scholar]
- Waldron I, Hughes ME, Brooks TL. Marriage Protection and Marriage Selection - Prospective Evidence for Reciprocal Effects of Marital Status and Health. Social Science and Medicine. 1996;43:113–123. doi: 10.1016/0277-9536(95)00347-9. [DOI] [PubMed] [Google Scholar]
- Williams David R., Collins Chiquita. U.S. Socioeconomic and Racial Differences in Health: Patterns and Explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams DR, Collins C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R., Neighbors Harold W., Jackson James S. Racial-ethnic Discrimination and Health: Findings from Community Studies. American Journal of Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson William J. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. University of Chicago Press; Chicago: 1987. [Google Scholar]
- Woldoff Rachael A., Ovadia Seth. Not Getting Their Money's Worth African-American Disadvantages in Converting Income, Wealth, and Education into Residential Quality. Urban Affairs Review OnlineFirst. 2009 published on December 17, 2008 as doi:10.1177/1078087408328947. [Google Scholar]
- Wood Robert, Goesling Brian, Avellar Sarah. The Effects of Marriage on Health: A Synthesis of Recent Research Evidence. Mathematica Policy Research, Inc.; Princeton, NJ: 2007. [January 6, 2009]. ( http://aspe.hhs.gov/hsp/07/marriageonhealth/index.htm) [Google Scholar]