Abstract
Purpose
To understand racial/ethnic minority adolescent females’ experiences with the vaginal ring.
Methods
We conducted in-depth interviews with a clinic-based sample of 32 young women aged 15–24 years who had used the vaginal ring.
Results
Qualitative analysis using grounded theory revealed that adolescents undergo a multi-stage process when trying the ring and adopting ring use. These stages include hearing about the ring, initial reactions, first experiences with insertion and removal, and first sexual experiences. Adolescents subsequently enter an assessment and adjustment stage in which they decide whether to adopt or discontinue ring use. Ultimately they share their experiences with friends.
Conclusions
The model developed provides a context within which providers may advise adolescents as they begin use of the ring. Some specific recommendations are offered.
Keywords: Vaginal ring, adolescence, Adolescent, Contraception, Reproductive health, Qualitative
Unintended pregnancy—a major public health problem in the United States— disproportionately affects young, unmarried, low-income, and racial/ethnic minority women [1]. Oral contraceptive pills (OCPs) remain the most common method of hormonal contraception used by adolescents [2]. However the need for daily compliance and the occurrence of side effects can lead to method discontinuation [3].
The vaginal ring (NuvaRing®, Organon Pharmaceuticals USA), a hormonal contraceptive introduced in 2001, offers adolescents a novel contraceptive option. The ring is self-inserted into the vagina and is left in place for 21 days per cycle followed by a 7-day ring-free period. Effectiveness is not compromised if the ring is removed for less than 3 hours. The ring releases ethinyl estradiol and etonogestrel, a progestin similar to that found in OCPs. Like OCPs, the vaginal ring inhibits ovulation and has similar efficacy, with a 1-year failure rate of about 1% with perfect use [4 –7]. Although results from clinical trials have demonstrated efficacy, safety, and user acceptability [4,8 –11], research to date has not described adolescents’ or racial/ethnic minority women’s experiences with the ring. Knowledge regarding these experiences is important because young and racial/ethnic minority women are at highest risk for unintended pregnancy [1]. The availability of an additional contraceptive option may mean that more women will find a contraceptive method that fits their needs. Adolescents will be most likely to succeed in using the ring if they are counseled and supported by providers. Understanding adolescents’ attitudes toward the ring and appreciating the process through which they adopt ring use may improve our counseling about the vaginal ring.
Methods
Participants
A total of 32 in-depth interviews were conducted from December 2005 to April 2006 to describe adolescents’ experiences with the vaginal ring, using grounded theory as described by Glaser and Strauss [12]. Grounded theory is an approach to the collection and analysis of qualitative data that emphasizes the development of theory to explain a social or psychological phenomenon [12]. Adolescent females were recruited at four family planning clinics in the San Francisco Bay Area, each of which has a large volume of clients and a low-income, culturally diverse clinic population. Fliers were posted in clinic waiting rooms, and providers informed adolescents about the study. Clinic clients were eligible to participate if they were 15–24 years of age, able to speak English or Spanish, and had used the vaginal ring for at least one cycle. Participants were reimbursed $30 for participation in the 1-hour interview. The study was approved by the Committee on the Protection of Human Subjects at the University of California at Berkeley. Written informed consent was obtained from all participants.
Study procedures and analysis
Before the interview, participants completed a demographic survey, with items concerning age, race/ethnicity, and previous birth control use. All interviews were conducted by the first author using a standardized script that was piloted for clarity of questions with three vaginal ring users.
The specific dimensions explored in this study were informed by existing literature about adolescents’ attitudes toward both hormonal contraceptive methods and intravaginal contraceptive methods, and in particular by a prior study of adolescents’ attitudes toward the vaginal ring. The prior study was an analysis of opinions about the ring elicited from more than 100 adolescents participating in focus groups, most of whom had not used the ring [13]. The themes found to be important among adolescents in the focus groups included concerns about sexual partner perceptions, apprehensions about vaginal ring efficacy, worries about the ring getting stuck or lost inside the vagina, and discomfort with touching the vagina. After completing this study, it became clear that to understand adolescents’ attitudes toward the ring we needed to interview adolescents who had used the ring.
These preliminary findings from focus groups guided the theoretical sampling for the current study (i.e., interviewing ring users instead of adolescents in general). Likewise these findings informed development of the interview guide, which included themes from the first study [12,14]. As the data regarding the focus groups will be reported elsewhere, this article focuses on the interview findings. The interviews began with open-ended prompts or questions such as: “Tell me about why you started using the ring.” “What was your initial reaction to the ring?” “What do friends, sexual partners, parents think about the ring?” The interview guide then included relevant themes from the prior research in an open-ended flexible fashion. All interviews were audio taped and transcribed. Interviews were conducted in tandem with ongoing data analysis leading to iterative changes in the interview guide. This allowed us to incorporate emerging concepts and test hypotheses into the interview process [12,14]. The collection of data ceased when saturation of themes occurred, in which new data were not uncovered and additional data did not seem to make a substantial contribution to existing data or the findings [12,14]. Although it would have been interesting to recruit young ring users with particular characteristics, finding young ring users at all was a challenge because the ring is still little used.
Transcripts were analyzed using grounded theory, and the analysis began with open coding of all transcripts to generate a list of all themes addressed in interviews [12,14–16]. Next, a codebook was generated and memos were written to explore specific codes [12,14–16]. Data were then entered into N6 (NUD*IST) software, a qualitative data management program [17], and were reread and coded using the codebook.
Our initial focus was on perceptions of the ring. However in analyzing adolescents’ experiences, a process model for adopting or discontinuing ring use began to emerge. We then elaborated on the model by comparing adolescents’ descriptions of the different stages and by looking for exceptions. We made changes to the model based on ongoing hypotheses and new interview data until saturation of themes was reached. We developed our proposed process model from adolescents’ collective experiences, which is presented in Figure 1. We present our results in the context of this model.
Figure 1.
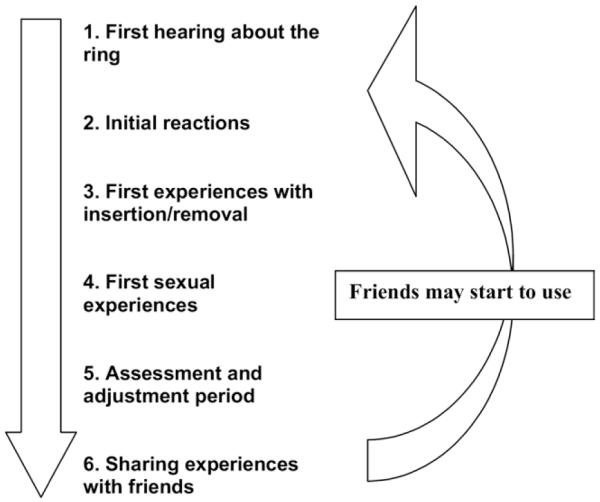
Process through which adolescents adopt or discontinue use of the vaginal ring.
Results
We interviewed 32 young women in total. Of these, 63% were 15–19 years of age and 37% were 20–24 years of age. The population was 28% Latina, 22% African-American, 25% Asian/Pacific Islander, and 25% mixed or other race/ethnicity. Of the participants, 69% had used the ring for more than 3 months. The average length of ring use was 9 months (range, 1–30 months). In all, 16% had discontinued the ring by the time of the interview after using it for 1 month or more; all other participants were current users. Contraceptive history was notable for the fact that 78% had used another continuous hormonal method before trying the ring.
The model developed through grounded theory analysis of interview data is presented in Figure 1 and is described in detail below.
First hearing about the ring
Most participants first heard about the vaginal ring from their providers at family planning clinics. Adolescents reported that their providers helped them in their decision to use the ring by personalizing the method to adolescents’ needs. “The counselor said, ‘If you’re very private and you don’t like to tell your parents everything,’ she recommended it. ‘If your mom sees [the patch] on your back or something, she’s going to have a fit, and if you’re not going to remember a pill, you should try the ring.’” (African-American, age 16 years)
Providers also helped adolescents by using ring samples and diagrams of the vagina to explain how the ring would be inserted and how it would sit in the vagina. Many explained that before seeing a diagram of the vagina and cervix, they would have worried that the ring would get lost inside the body. “[The provider] had a little model of a clear thing that was supposed to be a model of the vagina. And she just stuck the ring in there so you could see how it was and she was like, ‘This is how it is inside of the female’s body.’” (African-American, age 15)
Some providers even suggested that the client might feel more comfortable inserting the ring for the first time at the clinic, perhaps with the provider’s help. “She showed me how to put it in, and she did it for me. And then I tried to see if I was doing it the right way. I wouldn’t have tried it if she wouldn’t have shown me.” (Latina, age 21)
Each participant was asked where she had first heard about the ring. Four participants in our study (12%) reported first hearing about the ring from friends rather than from a clinic provider. They explained that it was comforting to know that their peers had already tried using the ring. Some commented that a friend’s recommendation might be more trustworthy than a provider’s. “[My friends would] be real with me; they would be like, ‘Oh no it sucks. [If a doctor told me first], I’d probably be a little hesitant, like if nobody uses it then there must be a reason why.’” (Asian/Pacific Islander, age 19)
Initial reactions
Even though all of the participants in this study ultimately decided to use the ring, many initially had concerns about it. Participants were worried about how the ring would be inserted, about cleanliness, about touching the vagina, about how the ring might “get stuck or lost in the vagina,” about how it would impact sex, and about its possible lack of effectiveness. “My concern was it was a pretty big ring. And it was kind of weird, like I didn’t know if it was flexible and if I would be able to put it in. And will it get stuck inside?” (Latina, age 17) Another participant said, “I’m like, ‘This lady’s trying to give me this thing in my vagina and leave it there for 3 weeks.’ I’m like, ‘No way. That’s probably going to make me stink.’” (African-American, age 15) According to another participant, “[I felt] uncomfortable. It was just the whole thing, putting my finger in there. I didn’t like that. You’re not supposed to touch yourself.” (Latina, age 20) One participant was skeptical: “What ring is going to prevent you from getting pregnant? It has a hole in it.” (Asian/Pacific-Islander, age 19)
Most expressed some reservations or concerns about using the ring because it is a relatively new method, because they hadn’t seen advertisements for it on television or in magazines, and because they didn’t know many women who had used it. “I was a little nervous [using a new method]. I felt like a test animal or something.” (African-American, age 17)
One participant explained that seeing a television commercial after she started using the ring made her feel more confident that it was effective and safe. “They got a commercial for it. It must not be too bad. It probably had to already been approved and stuff. If it wasn’t really cool, then people wouldn’t want to get too many people to use it because they don’t want to have no lawsuits or nothing.” (African-American, age 15)
In contrast to these initial concerns were positive and enthusiastic initial reactions by several participants. Typically, these were the participants who were happy to find a contraceptive method that fit their needs well. “I was very excited. I was like, ‘My God! Birth control that I can forget about and isn’t time consuming!’ Other birth control requires you to have a good memory. With the pill, I can’t remember it, so I’m not [getting] 100% effectiveness.” (Asian/Pacific-Islander, age 21)
First experiences with insertion/removal
Once participants decided to use the ring, their first experiences influenced how they ultimately felt about the ring and whether they continued to use it. Most participants explained that they went through an adjustment period during which they became more comfortable using the ring, as described below. When asked about their first experiences, many participants related using the ring to using tampons. “[It was] difficult ‘cause sometimes it unfolds when you put it in, and you have to squeeze it. It was just like a tampon after I got used to it.” (Asian/Pacific-Islander, age 21)
Some described initial insertion as difficult, and many who had initially been concerned about touching their vagina still were not comfortable touching their vagina for insertion. “[When I had to remove it] I was like, ‘No. Um-um.’ Then I finally [did it] and I was like, ‘That was unpleasant. Very unpleasant.’ [I didn’t like] the fact that I had to pull it out of my body like that with my own bare fingers!” (African-American, age 17)
Even though many participants equated using the ring to using tampons, it did not seem that prior use of tampons was necessary for successful ring use. Each participant was asked if she had used tampons and whether she liked or did not like using them. Four participants (12%) reported never having used tampons, and three participants (9%) reported having tried tampons but not liking to use them. These participants reported being pleased with the ring, and they continued to use it for multiple months; they were not the participants in this study who had discontinued using the ring.
First sexual experiences
Participants were asked about their sexual partners’ initial reactions to the ring. Some participants reported that their sexual partners were worried that the ring would not prevent pregnancy. In part, this reaction was related to the fact that partners had not previously heard about the ring and were not familiar with its mechanism of action. “My boyfriend was tripping. He was like, ‘That ain’t going to work. You should get up on the [contraceptive] patch. I would rather you be on the pill. How you know that works? I don’t know about this.’” (African-American, age 17)
Other adolescents reported that after explaining the ring to their sexual partners, partners were confident that the ring would be as efficacious as other hormonal methods. Participants said it was important to warn partners about the ring before sexual contact, because they wouldn’t want to “surprise” them if they felt the ring inside the vagina. For similar reasons, some participants thought that it would be awkward to use the ring in a casual relationship because it would necessitate explanation of the method, which might prove to be embarrassing with a casual partner. “I think in casual sex it’s kind of a surprise if they feel it or it’s like, ‘What’s that?’ They might think you are deformed inside or something. You might feel uncomfortable taking it out in front of somebody.” (African-American, age 18)
Most participants were initially concerned about what the ring would feel like for themselves and their partners during sex. However, most participants could not feel the ring during sex, and most partners could not either. All participants were asked how comfortable the ring was during sex. Four participants (12%) reported that the ring was uncomfortable during sex, leading them to take the ring out before intercourse and to reinsert it afterward. “I felt it poking me inside [my vagina]; it would just be something irritating you that you’re not used to and have to take it out.” (Asian/Pacific-Islander, age 18) Another participant reported, “It hurts the male during sex, or sometimes his penis hurts afterwards if we use the ring, so we have to take it out before sex.” (Asian/Pacific-Islander, age 21)
Assessment and adjustment period
Most participants described their first 1–2 months of using the ring as an adjustment period during which they decided whether to continue using the ring. Although initial insertion was difficult for many participants, most said that with practice, insertion became easier and more comfortable. “The more times you put the ring in, the more comfortable you get with it. Once you do it the first time, and then the second time you get comfortable.” (Latina, age 19)
Most participants described that after getting used to the ring, they did not often think about it because they could not feel it inside the vagina and they did not have to remember to use their birth control method on a daily basis. “You know that it’s there but you can’t feel it. And you don’t have to worry about it everyday!” (African-American/Asian/Pacific-Islander, age 18)
Participants adjusted to their initial concerns and developed practical strategies to feel more comfortable with the ring. The most common strategies discussed were taking the ring out during intercourse because it was uncomfortable, and taking the ring out to wash it during the month to achieve a sense of cleanliness. “I pull it out to wash it when I am in the shower, maybe like two to three times a week just to wash it, just to rinse it. Because I think it’s just cleaner. It’s more hygienic.” (Latina, age 20)
Five of the 32 participants (16%) were no longer using the ring, and discontinued ring use because they did not like the method. One participant discontinued because the ring could be felt in the vagina during intercourse, two because they could always feel the ring in the vagina, one because the ring caused nausea, and one because she disliked touching her vagina. “I liked the fact that I didn’t feel the ring when it was in there. And it was okay; I had sexual relationships, and I never got pregnant. But I just didn’t want to keep on putting my finger in there.” (Latina, age 20) Another participant commented, “I just didn’t like the feeling of it—it pushed against me when we had sex, so I stopped using it.” (African-American, age 17)
Sharing experiences with friends
Once participants decided to use the ring, they spoke to their friends about their experience and thus shared the new idea with other members of their peer group. Most described wanting to convince friends to use the ring because they liked it so much. “And I was like spokesperson for the ring really. ‘Cause I told all my girlfriends about it. I was like, ‘You guys have to get it. It’s really great.’ I feel like I’m some nurse that’s explaining everything. But I’m just telling them from personal experience, and it’s nice because I know them so well so they know that they can count on what I say.” (Asian/Pacific-Islander, age 23). Another participant commented “I said to my friends, ‘Just try it.’ With the ring, you get the best of all worlds. It’s 3 weeks, you don’t have to worry about putting it in every week or changing it. Time flies by so fast that you really don’t ever pay attention to it.” (Hispanic, age 21) After an adolescent or young woman shares her experiences with a friend, that friend may decide to use the ring. The friend may then go through the same process, as she is now a potential user of the ring.
Discussion
This exploratory, qualitative study of vaginal ring use yielded a proposed multi-stage model for the process by which adolescents adopt or discontinue use of the ring. Such knowledge of adolescents’ attitudes toward the ring and their experience using it may help providers to advise adolescents more successfully regarding this new contraceptive method.
The findings regarding the vaginal ring complement data from previous studies of intravaginal contraceptives such as the female condom and the diaphragm, which found that women had concerns about insertion and removal, about leaving the device inside the vagina, about interference with sex, and about the size of the device [18 –23]. The adolescents in our study had similar concerns. Although many participants had negative initial reactions, most were able to overcome their concerns through provider counseling and their own positive experiences with the ring and would recommend it to friends. Similarly clinical trials with women who had used the ring similarly found that acceptability was high, that women preferred the vaginal ring to other methods, and that women would recommend it to friends [4,8 –11]. This demonstrates that negative initial reactions do not necessarily predict future failure to adopt this method. Instead, when women have negative initial reactions, providers may present positive aspects of the ring, and can play a crucial role in counseling about the vaginal ring.
The proposed model provides a context within which providers may think about advising adolescents as they begin use of the ring. In describing their process of beginning to use the ring, adolescents discussed counseling techniques that seemed helpful in assisting them to move successfully through the stages outlined in the process model presented here. These techniques include: individualizing counseling, demonstrating vaginal ring effectiveness, addressing concerns, discussing strategies, and offering additional counseling once the client has chosen the ring. Table 1 summarizes recommendations for providers suggested by the results of this study. It is important to note that these recommendations were suggested by participants in the study or by the model derived from adolescents’ narratives. Specific recommendations would need to be formally tested to determine their impact on counseling.
Table 1.
Recommendations for healthcare providers’ counseling on contraceptive ring use, suggested by results of this study
Individualizing the counseling
|
Demonstrating vaginal ring mechanism of action
|
Addressing concerns
|
Discussing strategies
|
Counseling once client has chosen the ring
|
Many adolescents found that receiving education about their reproductive anatomy and addressing concerns regarding touching the vagina were helpful in increasing their acceptance and use of the vaginal ring. Many participants were concerned about the stigma of masturbation and the cleanliness of the vagina, and commented that these would be reasons not to use the ring. Although it is widely accepted in the adolescent development community that there is stigma around masturbation and the theme of touching the genitals, there are very few studies that directly address these stigmatized topics, particularly with adolescents. The concerns expressed by participants in our study have been described in some previous studies with adolescent females and adolescent males [24 –29]. Adolescents who successfully used the ring in this study reported that they had overcome concerns about touching their vagina. Thus, having an initial negative reaction toward touching the vagina did not seem to prevent adolescents from successfully using the ring. One study similarly showed that greater comfort with touching the genitals was not associated with greater satisfaction with the ring or greater likelihood of ring continuation [11], demonstrating that initial comfort with the vagina does not necessarily predict more successful ring use. Alternatively, adolescents may need to gain this comfort during the adjustment period.
Most participants described an adjustment period during which they became more comfortable using the ring. It may be helpful to explain to adolescents that they should anticipate an adjustment period. This time is necessary to become accustomed to all aspects of using the ring including touching the vagina to insert and remove the ring, having the ring inside the vagina on a daily basis, explaining the ring to sexual partners, and having the ring inside the vagina during intercourse.
This study has important limitations. First, because we studied a clinic-based sample, our sample may not represent the experiences of women who rarely seek provider attention for family planning. Second, because we sought adolescents or women who were ring users, our data likely overrepresent favorable views of the ring. Conclusions cannot be drawn about whether adolescents will or will not like the ring. We did not interview adolescents who had negative reactions and did not use the ring, so it is not clear when negative initial reactions impede adoption. Third, we also did not explore attitudes of those ring users who discontinued before completion of 1 month of use, so we have little information about early discontinuers. Fourth, the recommendations provided in Table 1 are based on the small sample of adolescents that we interviewed. Further research would be necessary to determine the recommendations’ utility and effectiveness.
The process model developed through these in-depth interviews about adolescents’ adoption of the vaginal ring may also be generalizable to other contraceptive methods, particularly new methods that have not yet been widely advertised or used. Further research should explore provider beliefs and practices regarding recommending the ring to adolescents; whether the process of adoption is the same in women of all ages, racial/ethnic backgrounds, and clinic settings; and whether the steps of adoption are the same for other new birth control methods. Subsequently, interventions should be developed to test which counseling approaches and techniques help adolescents move successfully through each stage of this process model.
Acknowledgment
This research was supported by the Joint Medical Program Graduate Block Grant Fellowship.
References
- [1].Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- [2].Mosher WD, Martinez GM, Chandra A, et al. Advance Data from Vital and Health Statistics. no 350. National Center for Health Statistics; Hyattsville, MD: 2004. Use of contraception and use of family planning services in the United States: 1982–2002. [PubMed] [Google Scholar]
- [3].Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: A prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179:577–82. doi: 10.1016/s0002-9378(98)70047-x. [DOI] [PubMed] [Google Scholar]
- [4].Dieben TOM, Roumen FJME, Apter D. Efficacy, cycle control, and user acceptability of a novel combined contraceptive vaginal ring. Obstet Gynecol. 2002;100:585–93. doi: 10.1016/s0029-7844(02)02124-5. [DOI] [PubMed] [Google Scholar]
- [5].Oddsson K, Leifels-Fischer B, de Melo NR, et al. Efficacy and safety of a contraceptive vaginal ring (NuvaRing®) compared with a combined oral contraceptive: A 1-year randomized trial. Contraception. 2005;71:176–82. doi: 10.1016/j.contraception.2004.09.001. [DOI] [PubMed] [Google Scholar]
- [6].Duijkers IJM, Klipping C, Verhoeven CHJ, et al. Ovarian function with the contraceptive vaginal ring or an oral contraceptive: A randomized study. Hum Reprod. 2004;19:2668–73. doi: 10.1093/humrep/deh493. [DOI] [PubMed] [Google Scholar]
- [7].Bjarnadottir RI, Tuppurainen M, Killick SR. Comparison of cycle control with a combined contraceptive vaginal ring and oral levonorgestrel/ethinyl estradiol. Am J Obstet Gynecol. 2002;186:389–95. doi: 10.1067/mob.2002.121103. [DOI] [PubMed] [Google Scholar]
- [8].Novak A, de la Loge C, Abetz L, et al. The combined contraceptive vaginal ring, NuvaRing ©: An international study of user acceptability. Contraception. 2003;67:187–94. doi: 10.1016/s0010-7824(02)00514-0. [DOI] [PubMed] [Google Scholar]
- [9].Weisberg E, Fraser IS, Mishell DR, et al. The acceptability of a combined oestrogen/progestogen contraceptive vaginal ring. Contraception. 1995;51:39–44. doi: 10.1016/0010-7824(94)00005-h. [DOI] [PubMed] [Google Scholar]
- [10].Szarewski A. High acceptability and satisfaction with NuvaRing ® use. Eur J Contracept Reprod Health Care. 2002;7(Suppl 2):31–9. [PubMed] [Google Scholar]
- [11].Schafer JE, Osborne LM, Davis AR, et al. Acceptability and satisfaction using Quick Start with the contraceptive vaginal ring versus an oral contraceptive. Contraception. 2006;73:488–92. doi: 10.1016/j.contraception.2005.11.003. [DOI] [PubMed] [Google Scholar]
- [12].Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Aldine Publishing Company; Chicago, IL: 1967. [Google Scholar]
- [13].Epstein LB. Adolescent attitudes toward and experiences with the vaginal ring [Master’s thesis] University of California at Berkeley; Berkeley, CA: 2007. [Google Scholar]
- [14].Strauss A, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2nd ed Sage Publications; Thousand Oaks, CA: 1998. [Google Scholar]
- [15].Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2nd ed Sage Publications; Thousand Oaks, CA: 1993. [Google Scholar]
- [16].Morse JM, editor. Critical issues in qualitative research methods. Sage Publications; Newbury Park, CA: 1994. [Google Scholar]
- [17].N6 (Non-numerical Unstructured Data Indexing Searching & Theorizing) qualitative data analysis program. Version 6 QSR International Pty Ltd.; Victoria, Australia: 2002. [Google Scholar]
- [18].El-bassel N, Krishnan SP, Schilling RF, et al. Acceptability of the female condom among STD clinic patients. AIDS Educ Prev. 1998;10:465–80. [PubMed] [Google Scholar]
- [19].Eldrige GD, St Lawrence JS, Little CE, et al. Barriers to condom use and barrier method preferences among low-income African-American women. Women Health. 1995;23:73–89. doi: 10.1300/J013v23n01_05. [DOI] [PubMed] [Google Scholar]
- [20].Choi KH, Roberts KJ, Gomez C, et al. Facilitators and barriers to use of the female condom: Qualitative interviews with women of diverse ethnicity. Women Health. 1999;30:53–70. doi: 10.1300/j013v30n01_04. [DOI] [PubMed] [Google Scholar]
- [21].Kulczycki A, Kim DJ, Duerr A, et al. The acceptability of the female and male condom: A randomized crossover trial. Perspect Sex Reprod Health. 2004;36:114–9. doi: 10.1363/psrh.36.114.04. [DOI] [PubMed] [Google Scholar]
- [22].Harvey SM, Bird ST, Maher JE, et al. Who continues using the diaphragm and who doesn’t: Implications for the acceptability of female-controlled HIV prevention methods. Womens Health Issues. 2003;13:185–93. doi: 10.1016/s1049-3867(03)00040-9. [DOI] [PubMed] [Google Scholar]
- [23].Maher JE, Harvey SM, Bird ST, et al. Acceptability of the vaginal diaphragm among current users. Perspect Sex Reprod Health. 2004;36:64–71. doi: 10.1363/psrh.36.64.04. [DOI] [PubMed] [Google Scholar]
- [24].Rodgers JL, Billy JOG, Udry JR. The rescission of behaviors: Inconsistent responses in adolescent sexuality data. Soc Sci Res. 1982;11:280–96. [Google Scholar]
- [25].Laumann EO, Gagnon JH, Michael RT, et al. The social organization of sexuality: Sexual practices in the United States. University of Chicago Press; Chicago, IL: 1994. [Google Scholar]
- [26].Halpern CT, Udry RJ, Campbell B, et al. Testosterone and pubertal development as predictors of sexual activity: A panel analysis of adolescent males. Psychosom Med. 1993;55:436–47. doi: 10.1097/00006842-199309000-00007. [DOI] [PubMed] [Google Scholar]
- [27].Halpern CT, Udry RJ, Suchindran C, et al. Adolescent males’ willingness to report masturbation. J Sex Res. 2000;37:327–32. [Google Scholar]
- [28].Frost L. Young women and the body: A feminist sociology. Palgrave; New York: 2001. [Google Scholar]
- [29].Oinas E. Medicalization by whom? Accounts of menstruation conveyed by young women and medical experts in medical advisory columns. Sociol Health Illn. 1998;20:52–70. [Google Scholar]


