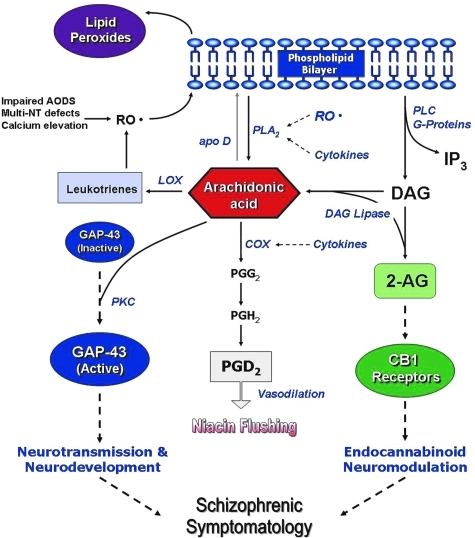
FIG. 9.
A putative model integrating lipid peroxidation, phospholipids turnover, AA signaling, and SZ symptomatology. As shown, several possible mechanisms can lead to increased phospholipid breakdown and AA release, including decreased AA incorporation and increased phospholipase activities (PLA2 and PLC), possibly resulting from increased oxidative stress and cytokine release. The resulting changes in AA level could then affect more downstream processes, including neurodevelopment via growth-associated protein (GAP)-43, neurotransmitter homeostasis, phosphatidylinositol signaling, and neuromodulatory actions of endocannabinoids. It is proposed that the specific behavioral symptomatology of SZ is related mostly to the effect of AA changes on the neurochemistry of deaminase, glutamate release, and circulating levels of the endocannabinoids anandamide and 2-arachidonoylglycerol (2-AG). In addition, alterations in AA may also affect the inflammatory response, which can then affect PLA2 release via cytokines, further exacerbating phospholipid turnover and AA release. Hence, in the current conceptualization, AA is at a nexus point in the cascade leading to the syndrome of SZ, and represents a common biochemical pathway leading to the highly heterogeneous symptomatology of psychosis. Reprinted with permission from Skosnik and Yao (236). (To see this illustration in color the reader is referred to the web version of this article at www.liebertonline.com/ars).