Abstract
Cocaine is used to produce a euphoric effect by abusers, who may be unaware of the devastating systemic and ocular side effects of this drug. We describe the first known case of cilioretinal artery occlusion after intranasal cocaine abuse.
Keywords: Centrocecal visual field defect, cilioretinal artery occlusion, fluorescein angiogram, intranasal cocaine
Cocaine is an alkaloid derived from the leaves of the Erythroxylon coca plant, indigenous to the Andes mountains. The inhabitants of this region chew the leaves, which impart a sense of well-being, but it may also be absorbed by the mucous membranes and gastrointestinal mucosa, through intranasal insufflations, smoking the ‘crack’ form or by intravenous injection. There are many medical complications of abuse, particularly cardiovascular, which can endanger life.[1] We report a rare case of cilioretinal artery occlusion following intranasal cocaine abuse in a young female.
Case Report
A 23-year-old female presented with a complaint of a sudden central right-sided visual field defect. She was otherwise healthy, with no past history of thrombophillic disorders. The only medication prescribed to her was progesterone, only a contraceptive pill. She had no past ocular history and did not smoke. On direct questioning the patient admitted to intranasal cocaine use 72 hours previously, although she was not a chronic abuser.
On examination, the unaided visual acuities were 20/40 in the right eye and 20/20 in the left eye. Anterior segment examination was normal, intraocular pressures were 15 mmHg in both eyes, and there was no pupillary abnormality. Fundus examination showed an area of retinal edema along the course of the right cilioretinal artery, which spared the fovea along with few dot hemorrhages in the posterior pole [Fig. 1]. The retinal vasculature was otherwise normal. A fundus fluorescein angiogram was performed [Fig. 2], which demonstrated that there was a flow within the right cilioretinal artery. The automated visual field analysis demonstrated a central visual field defect and decreased foveal threshold sensitivity in the right eye [Fig. 3]. Extensive blood tests to rule out either a thrombophillic, vasculitic or embolic source for the occlusion were unhelpful; these included an echocardiogram, full blood count, erythrocyte sedimentation rate, electrolytes, and urea levels, as also a thrombophillia screening.
Figure 1.

Retinal edema along the course of the right cilioretinal artery sparing the fovea and few dot hemorrhages in the posterior pole
Figure 2.
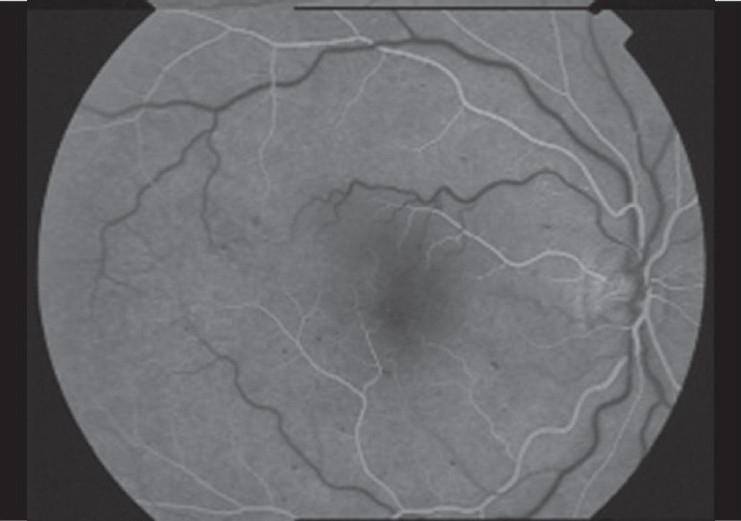
A fluorescein angiogram demonstrated that there was a flow within the right cilioretinal artery
Figure 3.
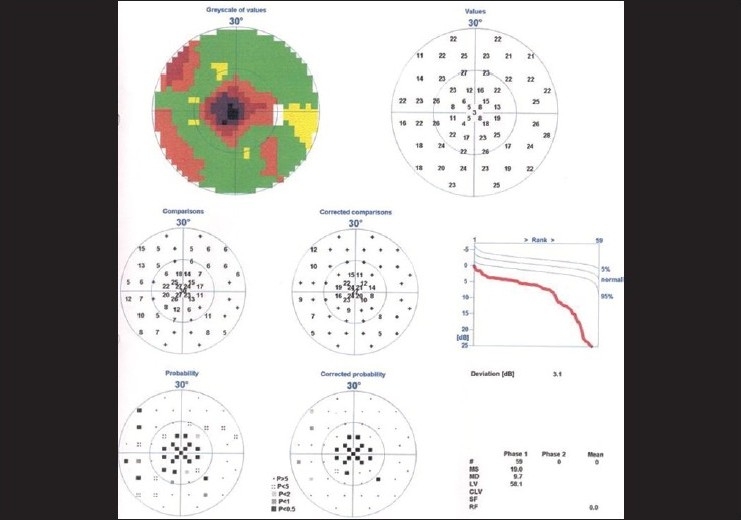
The octopus visual field demonstrated a central visual field defect and decreased foveal threshold sensitivity in the right eye
The patient was managed with vigorous manual massage of the eyeball, fast intravenous mannitol (250 ml in half an hour), followed by oral acetazolamide (500 mg) four times a day. Also, anterior chamber paracentesis was tried immediately. One day later, the patient felt a slight improvement in vision and was discharged against medical advice. She was lost to follow-up and presented after six months maintaining a visual acuity of 20/40 in the right eye and a normal appearing fundus.
Discussion
Apart from the medical complications, ocular complications of cocaine abuse include, keratopathy,[2] central retinal artery occlusion,[3] central retinal vein occlusion,[4] retinal hemorrhages,[5] papillitis,[6] and orbital infarction.[7] Cocaine has a complex pharmacological mode of action. It potentiates catecholamine action by inhibiting its reuptake at the adrenergic nerve endings. The voltage-dependent sodium ion channels are also blocked, which produces the local anesthetic properties of cocaine. The potentiating action with catecholamines produces an acute rise in blood pressure, which might be the underlying factor producing retinal hemorrhages and central retinal vein occlusion; the thrombogenic effect of cocaine could also be contributory. As cocaine has a plasma half-life of only 50 – 90 minutes, it would be difficult to explain the clinically observed incidences of vascular occlusions distant in time to this. A possible mechanism is the endothelin-1-mediated vasospasm. Cocaine is known to increase the production of endothelin-1, an effect observed as early as 12 hours after infusion and maximum at 48 hours.[7]
There are no proven treatments for the vasospasm produced by cocaine, but a stepped approach used in the treatment of cocaine-associated myocardial infarction may be helpful, including nitrates, calcium channel blockers, benzodiazepines, and anticoagulation / aspirin therapy.
References
- 1.Wallace RT, Brown GC, Benson W, Sivalingham A. Sudden retinal manifestations of intranasal cocaine and methamphetamine abuse. Am J Ophthalmol. 1992;114:158–60. doi: 10.1016/s0002-9394(14)73979-0. [DOI] [PubMed] [Google Scholar]
- 2.Zagelbaum B, Tannenbam M, Hersh P. Candida albicans corneal ulcer associated with crack cocaine. Am J Ophthalmol. 1991;111:248–9. doi: 10.1016/s0002-9394(14)72273-1. [DOI] [PubMed] [Google Scholar]
- 3.Devenyi P, Schneiderman JF, Devenyi RG, Lawby L. Cocaine induced central retinal artery occlusion. Can Med Assoc J. 1988;138:129–30. [PMC free article] [PubMed] [Google Scholar]
- 4.Sleiman I, Mangili R, Semeraro F, Mazzilli S, Spandria S, Balstreiri GP. Cocaine associated retinal vascular occlusion: Report of two cases. Am J Med. 1994;97:198–9. doi: 10.1016/0002-9343(94)90033-7. [DOI] [PubMed] [Google Scholar]
- 5.Newman NM, Dioreto DA, Ho JT, Klein JC, Birnbaum NS. Bilateral optic neuropathy and osteolytic sinusitis. Complications of cocaine abuse. JAMA. 1988;259:72–4. [PubMed] [Google Scholar]
- 6.Van Stavern GP, Gorman MG. Orbital infarction after cocaine use. Neurology. 2002;59:642–3. doi: 10.1212/wnl.59.4.642. [DOI] [PubMed] [Google Scholar]
- 7.Fandino J, Sherman JD, Zuccarello M, Rapports RM. Cocaine induced endothelin-1 dependent spasm in rabbit basilar artery in vivo. J Cardiovasc Pharmacol. 2003;41:158–61. doi: 10.1097/00005344-200302000-00002. [DOI] [PubMed] [Google Scholar]


