Abstract
Objective
In the present study, authors retrospectively reviewed the clinical outcomes of halo-vest immobilization (HVI) versus surgical fixation in patients with odontoid fracture after either non-surgical treatment (HVI) or with surgical fixation.
Methods
From April 1997 to December 2008, we treated a total of 60 patients with upper cervical spine injuries. This study included 31 (51.7%) patients (22 men, 9 women; mean age, 39.3 years) with types II and III odontoid process fractures. The average follow-up was 25.1 months. We reviewed digital radiographs and analyzed images according to type of injury and treatment outcomes, following conservative treatment with HVI and surgical management with screw fixation.
Results
There were a total of 31 cases of types II and III odontoid process fractures (21 odontoid type II fractures, 10 type III fractures). Fifteen patients underwent HVI (10 type II fractures, 5 type III fractures). Nine (60%) out of 15 patients who underwent HVI experienced successful healing of odontoid fractures. The mean period for bone healing was 20.2 weeks. Sixteen patients underwent surgery including anterior screw fixation (6 cases), posterior C1-2 screw fixation (8), and transarticular screw fixation (2) for healing the odontoid fractures (11 type II fractures, 5 type III fractures). Fifteen (93.8%) out of 16 patients who underwent surgery achieved healing of cervical fractures. The average bone healing time was 17.6 weeks.
Conclusion
The overall healing rate was 60% after HVI and 93.8% with surgical management. Patients treated with surgery showed a higher fusion rate and shorter bony healing time than patients who received HVI. However, prospective studies are needed in the future to define better optimal treatment and cost-effective perspective for the treatment of odontoid fractures.
Keywords: Cervical fracture, Odontoid fracture, Operation, Halovest, Bony healing
INTRODUCTION
More than 60% of spinal injuries involve the cervical spine, and about 25% of all cervical spinal injuries affect the axis6,7). The most common axis injury is odontoid fracture, of which the majority are type II or type III dens fractures3,6). Treatment strategies for odontoid fractures are based on fracture type, the degree of initial dens displacement, the angulation of the dens with respect to the body of C2, and the age of the patient. The nonunion rate for odontoid fractures is between 4% and 64% depending on the fracture site and method of treatment16,21,26).
Therapeutic options range from conservative treatment, including soft neck collars, rigid cervical orthosis and halo-vest immobilization (HVI), to surgical treatments including anterior screw fixation, posterior C1-2 screw fixation, or transarticular screw fixation. Non-surgical treatment with cervical collar or HVI may provide adequate support in type II fracture or type III stable fractures. Posterior fixation of C1-2 achieves higher fusion rates compared to conservative treatment, but is a challenging surgical technique and results in limitations in the cervical range of motion after surgery5,17,18,22). Anterior fixation techniques such as direct anterior odontoid screw fixation preserve rotatory motion of the cervical spine, with immediate stabilization of the spine8,12,24,25).
In this study, we retrospectively analyzed preoperative and postoperative clinical and radiographic findings of patients with odontoid fractures who were treated with either nonsurgical management (HVI) or surgical fixation using the anterior or posterior approach. Efficacy and comparative treatment outcomes of these methods for odontoid type II and III fractures are also discussed.
MATERIALS AND METHODS
After we received approval from our Institutional Review Board, we retrospectively reviewed all patients with high cervical fractures treated between April 1997 and December 2008. We treated 60 patients with high cervical fractures. This study includes 31 (51.7%) patients (22 men, 9 women; mean age, 39.3 years) with types II and III odontoid process fractures using the Anderson and D'Alonzo1) classification. The follow-up period ranged from 12 to 84.3 months with an average of 25.1 months (mean follow-up 27.5 months in HVI and 22.5 months in operation group). Data including sex, age, neurological status, associated injuries, clinical outcome, and complications were collected. The causes of fracture included 7 falls, 21 motor vehicle accidents and 3 pedestrian accidents. We treated patients with either conservative management (HVI) or surgery (internal fixation by posterior fusion or anterior screw fixation) to achieve osseous healing.
Diagnoses were made according to radiographs, including standard anteroposterior, lateral, and open-mouth radiographs. In addition, presurgical computed tomography (CT) scans with 3-dimensional reconstruction were performed to more precisely assess fractures. Digital radiographs of the fracture site were reviewed before and after procedures, using a picture archiving and communication system. The location of the involved vertebrae, fracture type, and direction, displacement, and angulation of fracture were analyzed.
Decision for surgical or conservative treatment was at surgeon's discretion based on the surgeon's preference and patients' condition in this retrospective study. After the explanation of associated anesthesia risks, such as pulmonary problems and congestive heart failures, and the obtainment of proper informed consent, the decision for surgical or conservative treatment was made. Before February 2006, the surgeons in our institute preferred cervical immobilization treated with halo vest orthosis because it had less risks compared with surgical operations. After that period, various surgical technique and instrumentation have been introduced to treat the odontoid fractures with instabilities, and surgical operations were performed when there was no major reason not to perform the operations. In our study, surgical treatment groups except two case were mainly enrolled in our study after March 2006.
We excluded pathological fractures resulting from malignancy, infection, metabolic disease, or congenital cervical spine anomalies from the present study.
Based on treatment modalities, we divided odontoid type II and III fractures into two groups : 1) those managed with surgery, including internal fixation by anterior screw fixation or posterior fusion, and 2) those managed nonsurgically with HVI.
Anterior odontoid screw fixation (6 cases) was performed using 4.0 mm cannulated screws (USS, Medtronic, Memphis, TN, USA). Posterior C1-2 fixations were performed in the prone position. Posterior C1-2 fixation was performed using transarticular screws (2 cases) or C1 lateral mass-C2 transpedicular screw fixation (Harms' technique, 8 cases) using polyaxial screws and rods (Vertex, Medtronic, Memphis, TN, USA; Summit, Depuy Spine, Raynham, MA, USA). C1-2 sublaminar wire fixations were tightened over iliac bone grafts to achieve bony healing by means of a modified Gallie method.
HVI (Bremer Medical Incorp, Jacksonville, FL, USA) devices were applied in a standardized manner based on conventional clinical methods. Decisions regarding when to remove the halo-vest were made on the basis of radiographs with evidence of union, and lack of pain or minimal neck pain.
Bony healing was examined by radiological evaluation. All patients underwent immediate radiographic imaging consisting of open-mouth and lateral cervical spine views following HVI or surgical treatment. All patients underwent routine follow-up evaluations at 1 week after treatment and at scheduled follow-up visits. Patient progress was reviewed after 4 weeks, 8 weeks, and 12 weeks. After 12 weeks, cervical dynamic views (flexion and extension radiographs) were obtained to check the bony healing. If there was no movement of the odontoid process related to the body of the axis, we performed the cervical CT scans to confirm solid bony healing and then the fracture was regarded as stable fusion13). If there was dens movement, we repeatedly executed the radiographs in the patients, placing them in soft collars once every month for a year after the treatment. After one year, radiological follow-up assessments were performed with cervical dynamic radiographs or CT scans once every 6 months.
Direction, degree of displacement, and angulation were evaluated on initial radiographs or CT scans. The degree of displacement and angulation were measured to assess the degree of correction and fixation achieved (Fig. 1, 2). These measures were evaluated by comparing the fractured segment of the odontoid process and the remaining portion still attached to C2.
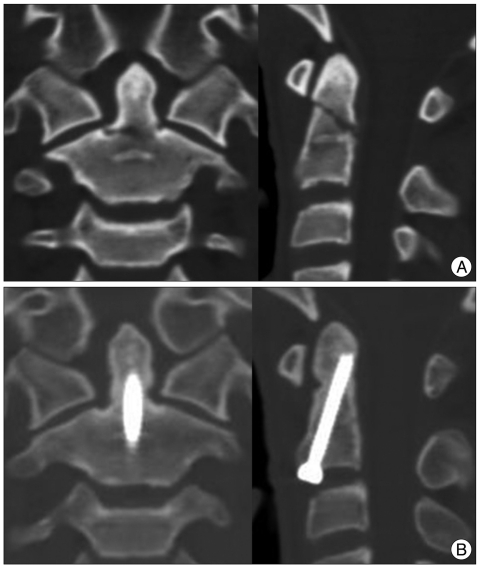
Fig. 1.
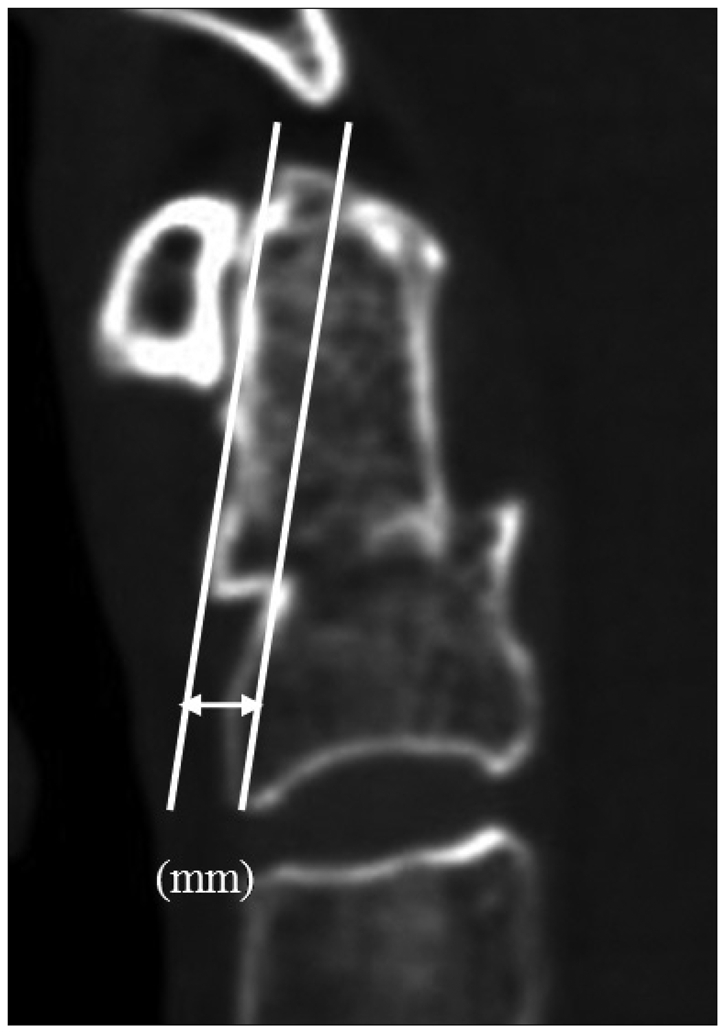
Odontoid fracture displacement. A tangent line is drawn along the anterior aspect of the odontoid fragment and the anterior aspect of the C2 body. A transverse line is drawn connecting these 2 lines. This distance is measured in millimeters and represents sagittal fracture displacement.
Fig. 2.
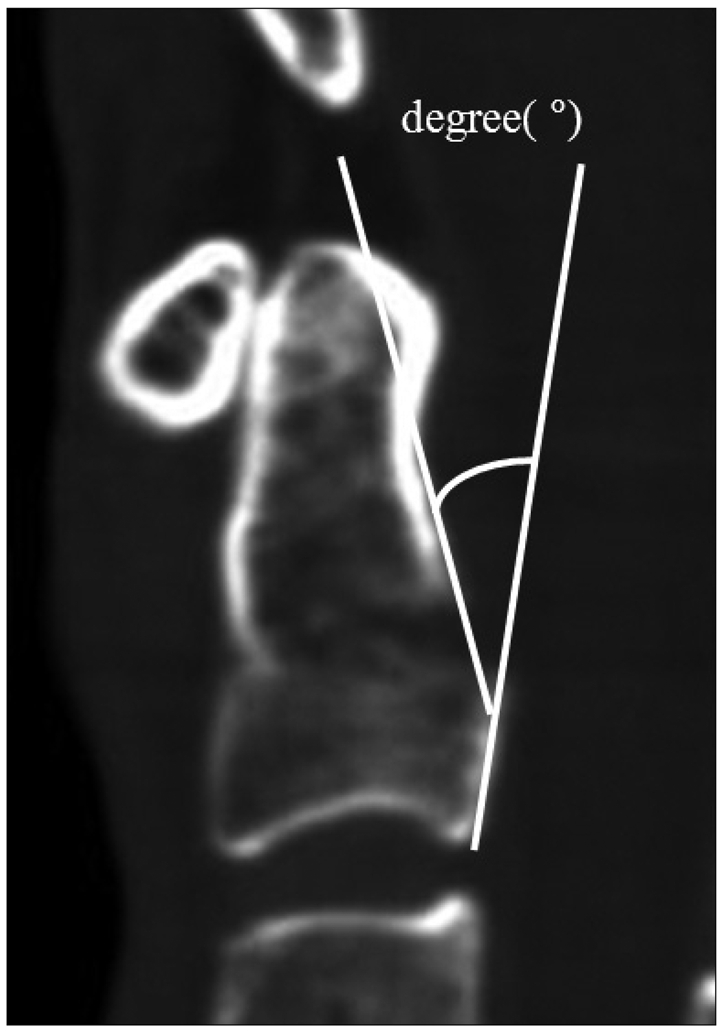
Odontoid fracture angulation. A tangent line is drawn along the posterior aspect of the odontoid fragment and the posterior aspect of the C2 body. The angle subtended by these lines is the degree of fracture angulation.
Our fusion criteria were evidence of trabeculation across the fracture, lack of visibility of the fracture line, and absence of movement on flexion-extension view. We defined failure as unsatisfactory healing, pseudoarthrosis, instability on dynamic films, significant postural pain, the development of neurologic symptoms, or any combination of these.
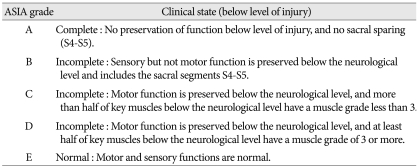
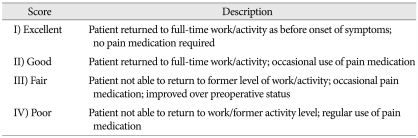
Clinical outcomes and complications were ascertained by reviewing hospital charts and by structured telephone interviews. We evaluated neurological outcomes according to American Spinal Injury Association (ASIA) grades to quantify the severity of neurological deficits (Table 1). After 12 months of conservative treatment or surgery, the patients were asked to grade their functional outcomes as excellent, good, fair, or poor, according to the Smiley-Webster Scale (Table 2).
Table 1.
American Spinal Injury Association (ASIA) Impairment Scale
Table 2.
Smiley-Webster scale used to assess clinical outcome
Normally distributed continuous data were analyzed by a Student's t test. For nonparametric analysis, the Mann-Whitney U-test was used to analyze the differences between two groups. All statistical analyses were conducted using MedCalc version 11.1 software (MedCalc, Mariakerke, Belgium). p-values less than 0.05 were considered statistically significant.
RESULTS
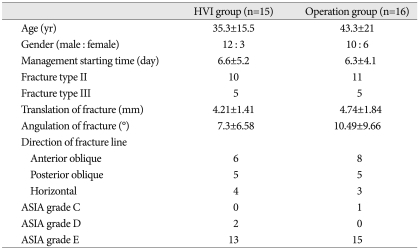
There were a total of 31 cases of odontoid fractures (21 odontoid type II fractures, 10 type III fractures). The fracture line was anterior oblique in 14 cases, posterior oblique in 10 cases, and horizontal in 7 cases. Of 31 patients, 15 underwent HVI for odontoid fracture healing (10 type II fractures, 5 type III fractures). Sixteen patients underwent surgical treatment including anterior screw fixation (6 cases), posterior C1-2 screw fixation (8), and transarticular screw fixation (2) for odontoid fractures (11 type II fractures, 5 type III fractures) (Table 3). The study groups did not differ significantly in patients' characteristics, including gender and initial fracture degree. Mean of the period from trauma to management starting time was 6.6±5.2 days in the HVI group and 6.3±4.1 days in the surgical group, there was no significant difference. Furthermore, the two groups did not differ in patients' age, BMD, smoking, and DM which could affect the bone fusion (Table 3).
Table 3.
Clinical characteristics in 31 patients with odontoid fractures
HVI : halo-vest immobilization, ASIA : American Spinal Injury Association Impairment Scale
Radiologic evaluation
Fusion rate
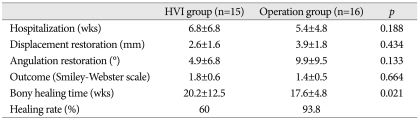
Overall, bony fusion was observed in 24 (77.4%) of 31 patients and achieved at an average of 19.5±15.2 weeks (minimum 6.4 weeks, maximum 28.1 weeks). Nine out of 15 patients who underwent HVI had healed odontoid fractures. The healing rate was 60%. The mean period for bone healing was 20.2 weeks (range, 13.1 to 28.1 weeks). In contrast, 15 (93.8%) out of 16 patients who underwent surgery had healed cervical fractures. The average bone healing time was 17.6 weeks (range, 6.4 to 25.0 weeks). There was a significant difference in bony healing time between the non-surgical and surgical groups (p<0.05) (Table 4). Surgical patients had a higher fusion rate and shorter bony healing time than patients who received conservative treatment (HVI).
Table 4.
Clinical outcomes according to group
HVI : halo-vest immobilization
Seven (22.6%) out of 31 patients experienced the failure. Six patients reported continued neck pain after conservative treatment (HVI) and 1 patient reported continued neck pain after surgical treatment. Of the 7 patients who experienced failure, 3 underwent additional operations (one anterior odontoid screw fixation, two posterior C1-2 screw fixations), but the other 4 patients refused further surgical intervention. These 4 patients received conservative therapy using neck braces.
Translation
The initial translation was 4.21±1.41 mm in the HVI group and 4.74±1.84 mm in the surgical group. After conservative management or surgical treatment, the translation was 1.66±1.35 mm in the HVI group and 0.81±1.55 mm in the surgical group. The reduction of odontoid fracture displacement was 2.56±1.62 mm in the HVI group and 3.93±1.84 mm in the surgical group. There were no statistically significant differences between the two groups (Table 4).
Angulation
The initial angulation was 7.3±6.58° in the HVI group and 10.49±9.66° in the surgical group. After conservative management or surgical treatment, the angulation was 2.33±2.42° in the HVI group and 0.54±1.26° in the surgical group. The reduction of odontoid angulation was 4.9±6.8° in the HVI group and 9.95±9.46° in the surgical group. There were no statistically significant differences between the two groups (Table 4).
Clinical outcomes
In patients treated with HVI for odontoid fracture, the initial ASIA spinal cord injury grades were distributed as follows : 2 ASIA D and 13 ASIA E. Among two patients with neurological deficits (two central cord syndrome), one patient was neurologically intact after HVI, and the other had residual deficits. Therefore, the grades were changed as follows : 1 ASIA D and 14 ASIA E. According to the Smiley-Webster Scale, patients achieved clinically excellent outcomes, 10 achieved good outcomes, and 1 achieved a fair outcome. 93.3% patients treated with HVI had good or excellent clinical outcomes.
In patients treated surgically with posterior fusion or anterior screw fixation for odontoid fractures, the presurgical ASIA spinal cord injury grades were distributed as follows : 1 ASIA C and 15 ASIA E. One patient with initial neurological deficits (one spinal cord contusion) improved markedly after posterior screw fixation. The grades improved to 1 ASIA D and 14 ASIA E. According to the Smiley-Webster Scale, 10 patients achieved clinically excellent outcomes and 6 patients achieved good outcomes. All patients (100%) experienced good or excellent clinical outcomes (Fig. 3).
Fig. 3.
A 24-year-old patient had severe neck pain following a traffic accident. A : Presurgical CT scan shows odontoid type II fracture. B : CT sagittal view shows odontoid union at 86 days after anterior odontoid screw fixation. The patient showed an excellent functional outcome and experienced no pain.
DISCUSSION
Type I and type III odontoid fracture based on the Anderson and D'Alonzo classification tend to heal well with external immobilization (healing rate of nearly 100% in type I and 84-88% in type III)15,20). Some reports cite nonunion rates ranging from 35% to 85% with nonsurgical management20,23,26). In particular, treatment options for type II fractures or type III fractures associated with atlanto-axial instability remain controversial15,20). Many authors advocate surgical intervention for fractures associated with atlanto-axial instability7,18).
We treated most of the odontoid fractures with nonsurgical management using HVI in our institute before February 2006. After that period, however, there was a significant increase in the rate of operative management that corresponded to the developments in internal fixation techniques and associated improvements in surgical outcomes. Since then, patients with type II or III odontoid fractures usually underwent primary surgical treatment by anterior or posterior screw fixation regardless of their age. In cases of ligament injuries, we usually performed posterior screw fixation for the treatment of odontoid fracture. Only in one patient who had significant comorbidities like severe pulmonary edema and congestive heart failure, we treated the odontoid fracture (type II) with HVI.
The goals of odontoid fracture treatment are radiographic bony fusion, relief of pain, and maximized quality of life. We observed favorable clinical outcomes for both surgical fixation and HVI. We found that 93.3% of patients treated with HVI had good or excellent clinical outcomes according to the Smiley-Webster Scale. All of the patients who underwent surgery accomplished good or excellent clinical outcomes. We achieved an overall bony fusion rate of 77.4% although there were relatively small number of patients. Average bony healing time was 19.5±15.2 weeks (minimum 6.4 weeks, maximum 28.1 weeks).
Many treatment options are acceptable for patients with odontoid fracture6,19). Bony fusion rates vary depending on treatment modality surgical options, including posterior fusion of the C1 and C2 vertebrae using wire/cable instrumentation, have demonstrated fusion rates of 87% and 100% for type II and III fractures respectively4,7). This procedure is associated with morbidity and mortality rates between 2% and 4%. Specific complications include vertebral artery injury and new onset neurological deficits. C1 to C2 fusion also causes the loss of atlantoaxial movement, rendering the patient unable to rotate his or her head. In our study, 100% bony fusion was achieved in patients who underwent posterior fusion of C1 and C2.
Other anterior surgical interventions such as anterior odontoid screw fixation also preserve atlantoaxial motion. Case series have demonstrated success rates of 90% to 95% for type II fractures, and 100% for type III10,14). In this study, the fusion rate was 83.3% in patients who underwent anterior screw fixation for type II and III odontoid fractures.
Conservative approaches include the application of a cervical collar or the use of an external immobilization device (the 'Halo' or 'Minerva' devices). Use of cervical collars alone has been shown to yield fusion rates approaching 100% in type I fractures, approximately 55% in type II, and 50% to 60% in type III injuries9). Unfortunately, external immobilization is poorly tolerated and is associated with an unacceptably high risk of inadequate bony fusion, as observed in our study23). In our experience, 60% patients who undergo HVI achieve healed odontoid fractures.
Several studies have reported that the healing rate after surgical treatment is superior to that after conservative treatment for odontoid fractures6,7). Clark and White6) documented a 68% healing rate after HVI and 96% after posterior surgery. To date, few studies have evaluated healing time with respect to treatment modalities in patients with odontoid fractures. In our study, we observed a higher fusion rate in the surgical group (93.8%) than in the nonsurgical group (60%). This finding is consistent with that of Clark and White6). The mean period for bone healing was 20.2 weeks (from 13.1 to 28.1 weeks) in patients who underwent HVI in our study. In contrast, the average bone healing time was 17.6 weeks in the surgical group. The related outcomes were therefore superior in the screw fixation group than in the HVI group.
We hypothesized that the inferior radiographic results of the HVI group may stem from differences in the limitation of neck motion. After external fixation by HVI, micromotion may occur following position changes. However, this effect may be reduced after internal fixation. Anderson and D'Alonzo1) originally reported the potential for significant fracture-site motion when moving between supine and upright positions despite HVI in a prospective study of 42 patients with cervical spine fractures. Five days after injury, Anderson and D'Alonzo1) observed an average of 7° angular motion and 1.7-mm translation when moving between the two positions. Kim et al.11) reported that when supine and upright X-rays were compared, an increased rate of fracture angulation was observed at all time points in a majority of patients who eventually developed nonunion.
Other radiological factors related to bony fusion are the degrees of angulation and translation. Apuzzo et al.2) found that odontoid fractures that were displaced more than 4 mm healed 12% lower than overall 64% union rate.1) They concluded that external immobilization was appropriate for the treatment of nondisplaced odontoid fractures, but that fractures displaced more than 4 mm were candidates for primary fusion. However, in our experience, we found that the nonunion rate in fractures that were displaced more than 4 mm was 20%, and in fractures that were displaced less than 4 mm was 23.8%. There were no statistically significant differences in fusion rate based on degree of displacement.
We evaluated whether surgical fixation can better restore displacement and angulation than nonsurgical management. The restoration of odontoid fracture displacement was 2.56±1.62 mm in the HVI group and 3.93±1.84 mm in the surgical group. After conservative management or surgical fixation, the restoration of odontoid angulation was 4.9±6.8° in the HVI group and 9.95±9.46° in the surgical group. We found that there were no statistically significant differences in degree of restoration according to treatment modalities.
In our study, as time went on, we observed a significant decline in the use of HVI, with a correlated increase in nonunion and complications of that non-surgical treatment for odontoid fractures. Based on these results and the results of a prior study23), at our institution, we have changed our therapeutic approach from non-surgical treatment to surgical treatment for odontoid type II fractures and type III unstable fractures. However, as with many degenerative and traumatic conditions of the spine, treatment decisions must be based on individual patient characteristics and fracture patterns to optimize outcomes. In addition, the patients' medical conditions and the surgeons' expertise must be considered to choose the best treatment option. As our present study with a retrospective design relying on written medical records, there are some limitation such as the lack of clinical data on cervical spine mobility, small sample size, and non-standardized method for treatment decision. We believe further rospective studies are necessary to define the better optimal treatment strategy and cost-effective perspectives for type II and III odontoid fractures.
CONCLUSION
We found that treatments of odontoid fracture type II and III are associated with favorable clinical outcomes regardless of the management strategy. The clinical outcomes were similar for patients managed with surgical fixation and those managed conservatively by HVI. However, surgical treatment by posterior fusion or anterior screw fixation yields a better fusion rate and shorter healing time than external immobilization. Further randomized, controlled trials are required to define optimal treatment strategies for this complex clinical problem.
References
- 1.Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 2.Apuzzo ML, Heiden JS, Weiss MH, Ackerson TT, Harvey JP, Kurze T. Acute fractures of the odontoid process. An analysis of 45 cases. J Neurosurg. 1978;48:85–91. doi: 10.3171/jns.1978.48.1.0085. [DOI] [PubMed] [Google Scholar]
- 3.Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979;61:1119–1142. [PubMed] [Google Scholar]
- 4.Campanelli M, Kattner KA, Stroink A, Gupta K, West S. Posterior C1-C2 transarticular screw fixation in the treatment of displaced type II odontoid fractures in the geriatric population--review of seven cases. Surg Neurol. 1999;51:596–600. doi: 10.1016/s0090-3019(98)00136-0. discussion 600-601. [DOI] [PubMed] [Google Scholar]
- 5.Choi JW, Yoon SH, Park HC, Park HS, Kim EY, Ha Y. The results and complications of the C1-C2 transarticular screw fixation methods. J Korean Neurosurg Soc. 2005;37:201–206. [Google Scholar]
- 6.Clark CR, White AA., 3rd Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67:1340–1348. [PubMed] [Google Scholar]
- 7.Frangen TM, Zilkens C, Muhr G, Schinkel C. Odontoid fractures in the elderly : dorsal C1/C2 fusion is superior to halo-vest immobilization. J Trauma. 2007;63:83–89. doi: 10.1097/TA.0b013e318060d2b9. [DOI] [PubMed] [Google Scholar]
- 8.Graziano G, Jaggers C, Lee M, Lynch W. A comparative study of fixation techniques for type II fractures of the odontoid process. Spine (Phila Pa 1976) 1993;18:2383–2387. doi: 10.1097/00007632-199312000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures : a review of 229 cases. J Neurosurg. 1989;71:642–647. doi: 10.3171/jns.1989.71.5.0642. [DOI] [PubMed] [Google Scholar]
- 10.Jenkins JD, Coric D, Branch CL., Jr A clinical comparison of one- and two-screw odontoid fixation. J Neurosurg. 1998;89:366–370. doi: 10.3171/jns.1998.89.3.0366. [DOI] [PubMed] [Google Scholar]
- 11.Kim DH, Vaccaro AR, Affonso J, Jenis L, Hilibrand AS, Albert TJ. Early predictive value of supine and upright X-ray films of odontoid fractures treated with halo-vest immobilization. Spine J. 2008;8:612–618. doi: 10.1016/j.spinee.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Kim MJ, Hwang JH, Sung JK, Hwang SK, Hamm IS, Park YM, et al. Anterior screw fixation of type II odontoid fracture. J Korean Neurosurg Soc. 2000;29:1461–1468. [Google Scholar]
- 13.Koller H, Kolb K, Zenner J, Reynolds J, Dvorak M, Acosta F, et al. Study on accuracy and interobserver reliability of the assessment of odontoid fracture union using plain radiographs or CT scans. Eur Spine J. 2009;18:1659–1668. doi: 10.1007/s00586-009-1134-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SH, Sung JK. Anterior odontoid fixation using a 4.5-mm Herbert screw : The first report of 20 consecutive cases with odontoid fracture. Surg Neurol. 2006;66:361–366. doi: 10.1016/j.surneu.2006.04.018. discussion 366. [DOI] [PubMed] [Google Scholar]
- 15.Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine (Phila Pa 1976) 2006;31:S53–S60. doi: 10.1097/01.brs.0000217941.55817.52. discussion S61. [DOI] [PubMed] [Google Scholar]
- 16.Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly : a death sentence? J Trauma. 2005;59:350–356. doi: 10.1097/01.ta.0000174671.07664.7c. discussion 356-358. [DOI] [PubMed] [Google Scholar]
- 17.Muller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8:360–365. doi: 10.1007/s005860050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ochoa G. Surgical management of odontoid fractures. Injury. 2005;36(Suppl 2):B54–B64. doi: 10.1016/j.injury.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 19.Polin RS, Szabo T, Bogaev CA, Replogle RE, Jane JA. Nonoperative management of Types II and III odontoid fractures : the Philadelphia collar versus the halo vest. Neurosurgery. 1996;38:450–456. doi: 10.1097/00006123-199603000-00006. discussion 456-457. [DOI] [PubMed] [Google Scholar]
- 20.Sasso RC. C2 dens fractures : treatment options. J Spinal Disord. 2001;14:455–463. doi: 10.1097/00002517-200110000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Schweigel JF. Management of the fractured odontoid with halo-thoracic bracing. Spine (Phila Pa 1976) 1987;12:838–839. doi: 10.1097/00007632-198711000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Seybold EA, Bayley JC. Functional outcome of surgically and conservatively managed dens fractures. Spine (Phila Pa 1976) 1998;23:1837–1845. doi: 10.1097/00007632-199809010-00006. discussion 1845-1846. [DOI] [PubMed] [Google Scholar]
- 23.Shin JJ, Kim SJ, Kim TH, Shin HS, Hwang YS, Park SK. Optimal use of the halo-vest orthosis for upper cervical spine injuries. Yonsei Med J. 2010;51:648–652. doi: 10.3349/ymj.2010.51.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song KJ, Lee KB, Kim KN. Treatment of odontoid fractures with single anterior screw fixation. J Clin Neurosci. 2007;14:824–830. doi: 10.1016/j.jocn.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 25.Sung JK. Anterior screw fixation using herbert screw for Type II odontoid process fractures. J Korean Neurosurg Soc. 2005;37:345–349. [Google Scholar]
- 26.Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60:199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]