Abstract
We present a case of Neuro-Behçet's disease with an unpredictable clinical course. A 47-year-old man was admitted to the neurosurgery department of our hospital with a mild headache. Three days after admission, his consciousness suddenly decreased and respiratory distress progressed rapidly. A brain MRI revealed that the previously observed abnormal signal had extended markedly to both the thalamic areas and the entire brain stem, and the surrounding brain parenchyma were compressed by cerebral edema. Based on the patient's symptoms of recurrent oral and genital ulcers, skin lesions, and uveitis, a rheumatologist made a diagnosis of Behçet's disease with CNS involvement. The patient was treated with high-dose methylprednisolone with respiratory assistance in the intensive care unit for 9 days and his neurologic symptoms improved remarkably. Neuro-Behçet's disease must be considered in the differential diagnosis in rapidly deteriorated young neurological patients along with a stroke, low-grade glioma, multiple sclerosis, and occlusive venous disease.
Keywords: Behçet's disease, Neuro-Behçet's disease, Central Nerve System manifestation, Neurological deterioration
INTRODUCTION
Behçet's disease is a chronic relapsing inflammatory disorder of unknown etiology that involves many organ systems including the central nervous system (CNS). Neurologic deficits occur in 10% to 30% of patients and may be the presenting feature in up to 5% of patients10). Behçet's disease is characterized by recurrent oral and genital ulcers, relapsing uveitis, mucocutaneous, articular, neurologic, urogenital, vascular, intestinal, and pulmonary manifestations. In this article, we present our experience of a Behçet's disease that showed unpredictably rapid respiratory distress and neurologic deterioration. We also discuss the clinical presentations, diagnostic tools, treatment options, and prognosis of Behçet's disease.
CASE REPORT
A 47-year-old man with a mild headache visited the neurosurgery department of our hospital as recommended by a local radiologist. His family history was unremarkable, and he recalled only a mild head trauma, due to a traffic accident, two weeks before. Brain MRI performed at the local hospital revealed abnormal signal intensity at the left tegmentum of the midbrain in Axial Fluid-Attenuated Inversion-Recovery (FLAIR) images (Fig. 1). In small portions of the brainstem, minimal peri-lesional swellings were noted; however sulci around the lesions were well recognized. Abnormal signal regions showed ill-defined margins. Neurologic and radiologic findings by the referring radiologist suggested lacuna brainstem infarction.
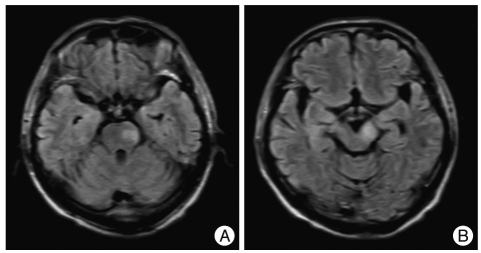
Fig. 1.
Abnormal high signal intensity in both T1 weighted image (A) and T2 weighted image (B) in the left pons and left mid brain (cerebral peduncle). At this time, abnormal signals were noted only in small limited portion of the brainstem.
The chief complaint of the patient was mild headache. His vital signs were stable and his complete blood count, routine biochemistry tests, urinalysis, liver function tests, thyroid function tests, lipid profiles, and creatine kinase level were normal, as were his erythrocyte sedimentation rate and C-reactive protein level. Furthermore, a neurologic examination failed to reveal any deficit. At that time, we suspected demyelinating disease with subclinical manifestation, or possibly low-grade glioma, and thus we requested diffusion MRI and MR angiography. Diffusion MRI failed to produce any definite abnormal finding indicating ischemic stroke, other than confirmation of the previous abnormal brainstem findings, and MR angiography showed neither tumor stains nor any other vascular abnormality including occlusion.
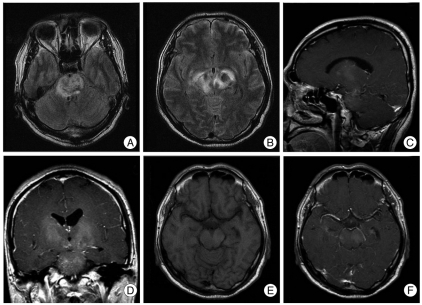
Accordingly, his symptoms were conservatively treated. On hospital day 3, the patient's consciousness suddenly deteriorated and respiratory distress progressed rapidly, and within only hours his mental status deteriorated to a stuporous level and his respiratory difficulty to near respiratory arrest. He was transferred immediately to the ICU for emergency intubation and mechanical ventilatory support. Simple chest radiography provided no information regarding the cause of respiratory arrest. However, an emergency brain MRI revealed that the abnormal signal at the brain stem had extend-ed to both the thalami and the whole brainstem, and that cerebral edema was compressing surrounding tissues. The lesion showed high intensity on T2-weighted MR images (Fig. 2A-D), and exhibited a mild gadolinium contrast enhancement (Fig. 2E, F).
Fig. 2.
This brain MRI scan taken at hospital at 3 days post-presentation revealing abnormal signal intensity initially observed in the brainstem that were not enhanced strongly (pre-enhanced T1 weighted image (E) and post-enhanced T1 weighted image (F). It had extended to the whole brain stem and the both thalami, both basal ganglia, periventricular white matter, both mid brain cerebral peduncles, and involved the whole stem, whole ventral and dorsal aspects, and that edema associated with the lesion was compressing surrounding tissue (A and B : Axial fluid-attenuated inversion-recovery (FLAIR) images, C : Sagittal FLAIR image, D : Coronal FLAIR image).
When we intubated the patient, we found that the oral ulceration had occurred and there were some additional swelling and redness in the peri-orbital area. A reevaluation then revealed multiple aphthous ulcers in the patient's gums and tongue mucosa. A genital examination revealed several ulcers on the scrotal surface. These findings led us to suspect Behçet's disease. Accordingly, a rheumatologist's consultation result has confirmed a diagnosis of Behçet's disease with Central Nerve System (CNS) involvement, based on the symptoms of recurrent oral ulcers, genital ulcers, skin lesions, and uveitis. The patient was administered with high-dose methylprednisolone with respiratory assistance. A remarkable improvement of his neurologic symptoms ensued within one day of administrating the steroid, and on hospital day 12, he was able to return to the general ward without a definite neurological deficit. However, the recurrent oral aphthous ulcer, an ulcerating genital lesion, uveitis, and multiple arthralgias remained. After return to the general ward, he was managed by the rheumatologist. One month later, a follow-up brain MRI showed that the previous abnormal signal was substantially decreased and the brain swelling had disappeared (Fig. 3).
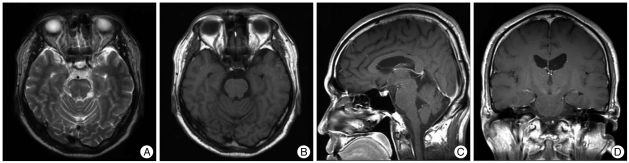
Fig. 3.
Brains MR scan taken one month later showing a marked reduction in the abnormal signal as compared with the scan taken at 10 days without brain swelling. Minimal abnormal signals were noted in the mid brain bilaterally. (A and B : Axial T1 and T2 weighted image, C : Sagittal FLAIR image, D : coronal FLAIR image).
DISCUSSION
Clinical features of Neuro-Behçet's disease
Some studies suggest that the most common presentation of Neuro-Behçet's disease are symptoms related to the brainstem1,8). Depends on where in the brain the lesion is located, neurologic symptoms can be presented accordingly. Brainstem involvement may present as long-tract signs, cranial nerve palsies, and cerebella signs7). Optic neuritis and ischemic optic neuropathy are not rare symptoms in Neuro-Behçet's disease11). Neurotologic manifestations have also been reported and cochlear and neural hearing loss are known to be not uncommon. Audio-vestibular disturbance5) and vestibulo-ocular reflex abnormality have also been reported16).
In Neuro-Behcet's disease, involvements of intracranial or extracranial arteries or veins have been reported. Afshin et al.2) reported non-parenchymal CNS involvement (neurovasculo-Behçet's disease) which includes dural sinus thrombosis, arterial occlusion, and arterial aneurysms. Venous involvement of Neuro-Behçet's disease usually produces intracranial hypertension, so it can manifest as an acute or more commonly subacute evolution of headache, papilledema, focal neurologic deficits, seizures, sixth-nerve palsy, and altered consciousness. Intracranial hypertension, with or without cerebral vein thrombosis, appears in 11-35% of all patients with Neuro-Behçet's disease14).
Arterial involvement is a rare cause of neurovascular-Behçet's disease in comparison to venous involvement2). Arterial involvement of brain, heart, and other vital organs can be a cause of a cause of mortality and major morbidities.
In our case, the patient had not noted seizure-like behavior or focal neurologic deficit. Cerebral vein thrombosis was not noted in radiologic examinations and there was no abnormal finding in cerebral angiography. However, the patient showed altered mental state and severe brain swelling was noted on MRI. Based on this evidence, we believed that this patient showed clinical and radiologic manifestations of venous type of Neuro-Behcet's disease.
Clinical diagnostic tools of Neuro-Behcet's disease
Radiologic investigations are critically important for the diagnosis of Neuro-Behçet's disease. Computerized tomography has been used for radiologic diagnosis of Neuro-Behçet's disease6), but recently, many other radiologic tools have been used, such as MRI, MR venography, and MR spectroscopy.
Chae et al.4) classified radiologic findings of involving brain parenchyma as typical and atypical involvement. Typical radiologic finding of Neuro-Behçet's disease is involvement of the brainstem, especially around the cerebral peduncles and the pons. The thalamus and basal ganglia are the next most common sites of involvement, and similar foci can be noted in the cerebral hemispheres2). MRI findings in Neuro-Behcet's disease are small foci of high signal intensity on T2-weighted images; these foci are iso- or hypointense relative to brain parenchyma on T1-weighted images. Lesions may be circular, linear, crescent-shaped, or irregular. Atypical Neuro-Behçet's disease is seen as a space-occupying lesion or masquerading as a unilateral brain tumor. Differential diagnoses include lymphoma, malignant tumors, or metastatic tumor and abscess or meningitis. These atypical manifestations of Neuro-Behcet's disease may make diagnosis more difficult. In particular, diagnosis is difficult in cases, in which the neurologic manifestation does not occur simultaneously with a flare-up of Behçet's disease.
Accordingly, to avoid misdiagnosis of Neuro-Behcet's disease as a brain tumor, some authors have recommended a stereotactic biopsy to obtain a precise differential diagnosis. However, these findings may not be specific as it reveales the perivascular infiltration of leukocytes and microglia, oligodendroglial degeneration, diapedetic bleeding, and perivascular softening or necrosis. Thus, it may be difficult to diagnose Neuro-Behçet's disease using pathologic findings alone. Nevertheless, stereotactic biopsy can be used to definitively rule out the possibility of a brain tumor12).
Treatment and prognosis of Neuro-Behçet's disease
Based on literature, medical therapy with methylprednisolone is regarded as the treatment of choice for Neuro-Behçet's disease. Methylprednisolone 1 g is usually given intravenously daily for up to 7 days, followed by prednisone 0.5 to 1 mg/kg/day. Prednisone is a favored option for acute attacks, but to prevent early relapses, it must be gradually tapered over 2 to 3 months15).
During the last few years, many publications have suggested that the inhibition of Tumor Necrosis Factor (TNF) offers a promising therapeutic approach. Furthermore, treatments based on Granulocyte colony-stimulating factor (G-CSF), zinc sulfate, and selective granulocytopheresis have also been tried to improve treatment results9).
In 2010, Borhani and safari3) proposed an algorithm for treatment of differential manifestations of Neuro-Behçet's disease. They divided anti-Neuro Behçet's disease (NBD) armamentarium to first-line, second-line, and experimental drugs. First-line drugs are more extensively studied, less hazardous, and more affordable. They included corticosteroids, azathioprine, methotrexate, and cyclophosphamide. Second-line drugs are the therapeutic options with higher prices, potentially dangerous effects, or more limited data on efficacy, safety, and tolerability. They include anti-tumor necrosis factor (TNF) drugs, interferon-α, chlorambucil, and mycophenolate mofenil. Experimental drugs have been used in single cases or small series or only hypothetically can be used for NBD.
Neurologic manifestations of Behçet's disease have been known to be a bad prognosis factors, However, based on a review of literature, the most common and important risk factor is Behçet's disease with arterial involvement. Saadoun et al.13) reported mortality in Behçet's disease. They analyzed clinical record of 817 patients with Behçet's disease and found 26.9% had Neuro-Behcet's disease. These patients had an overall mortality of 5% after a median follow-up time of 7.7 years. The main causes of death included major vessel disease (i.e. arterial aneurysm and Budd-Chiari syndrome). Mortality rate of pulmonary arteritis in Behçet's disease patients has been reported as about 50%.
Based on the literature, our case is regarded as radiologically typical and "venous involved" type of Neuro-Behçet's disease The most common symptom of typical venous involved type of Neuro-Behçet's disease is headache and focal neurologic deficit. Sometimes the lesions are recognized after the acute stage. However, as in our case, the patient can experience extremely rapid progress of neurologic deterioration, going from free of neurological symptoms to a stuporous mental state within a few hours.
Saadoun et al. reported other factors associated with mortality are genital ulceration, a high frequency of Behçet's disease flare and being male. In our case, the patient met most of the criteria for high mortality risk being a male with genital ulceration, Behçet's disease flares and neurologic manifestation.
CONCLUSION
Behçet's disease usually presents as atypical symptoms, such as, an oral ulcer, arthritis, or uveitis. Similarly, Neuro-Behçet's disease can present as various neurologic statuses, ranging between headaches, hemiparesis, and life-threatening neurologic deficits. In our case, no neurologic abnormality was evident initially, but the patient deteriorated to a stuporous mental state and respiratory arrest only a few days later. We caution that Behçet's disease should be included in the differential diagnosis of multiple sclerosis, systemic lupus erythematosus, primary CNS lymphoma or primary glial tumors, space-occupying lesions of the brain, such as, tumors or abscesses, or stroke in young adults.
References
- 1.Akman-Demir G, Serdaroglu P, Tasçi B The Neuro-Behçet Study Group. Clinical patterns of neurological involvement in Behçet's disease: evaluation of 200 patients. Brain. 1999;122:2171–2182. doi: 10.1093/brain/122.11.2171. [DOI] [PubMed] [Google Scholar]
- 2.Borhani Haghighi A, Pourmand R, Nikseresht AR. Neuro-Behçet disease. A review. Neurologist. 2005;11:80–89. doi: 10.1097/01.nrl.0000156343.16797.c4. [DOI] [PubMed] [Google Scholar]
- 3.Borhani Haghighi A, Safari A. Proposing an algorithm for treatment of different manifestations of neuro-Behcet's disease. Clin Rheumatol. 2010;29:683–686. doi: 10.1007/s10067-010-1414-6. [DOI] [PubMed] [Google Scholar]
- 4.Chae EJ, Do KH, Seo JB, Park SH, Kang JW, Jang YM, et al. Radiologic and clinical findings of Behçet disease: comprehensive review of multisystemic involvement. Radiographics. 2008;28:e31. doi: 10.1148/rg.e31. [DOI] [PubMed] [Google Scholar]
- 5.Choung YH, Cho MJ, Park K, Choi SJ, Shin YR, Lee ES. Audio-vestibular disturbance in patients with Behçet's disease. Laryngoscope. 2006;116:1987–1990. doi: 10.1097/01.mlg.0000237442.80711.65. [DOI] [PubMed] [Google Scholar]
- 6.Dobkin BH. Computerized tomographic findings in neuro-Behcet's disease. Arch Neurol. 1980;37:58–59. doi: 10.1001/archneur.1980.00500500088017. [DOI] [PubMed] [Google Scholar]
- 7.Kermode AG, Plant GT, MacManus DG, Kendall BE, Kingsley DP, Moseley IF. Behçet's disease with slowly enlarging midbrain mass on MRI : resolution following steroid therapy. Neurology. 1989;39:1251–1252. doi: 10.1212/wnl.39.9.1251. [DOI] [PubMed] [Google Scholar]
- 8.Kidd D, Steuer A, Denman AM, Rudge P. Neurological complications in Behçet's syndrome. Brain. 1999;122:2183–2194. doi: 10.1093/brain/122.11.2183. [DOI] [PubMed] [Google Scholar]
- 9.Krause I, Weinberger A. Behçet's disease. Curr Opin Rheumatol. 2008;20:82–87. doi: 10.1097/BOR.0b013e3282f154d1. [DOI] [PubMed] [Google Scholar]
- 10.Mirsattari SM, McGinn GJ, Halliday WC. Neuro-Behcet disease with predominant involvement of the brainstem. Neurology. 2004;63:382–384. doi: 10.1212/01.wnl.0000130192.12100.8d. [DOI] [PubMed] [Google Scholar]
- 11.Mitra S, Koul RL. Paediatric neuro-Behçet's disease presenting with optic nerve head swelling. Br J Ophthalmol. 1999;83:1096. doi: 10.1136/bjo.83.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park JH, Jung MK, Bang CO, Park HK, Sung KB, Ahn MY, et al. Neuro-Behçet's disease mimicking a cerebral tumor: a case report. J Korean Med Sci. 2002;17:718–722. doi: 10.3346/jkms.2002.17.5.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saadoun D, Wechsler B, Desseaux K, Le Thi Huong D, Amoura Z, Resche-Rigon M, et al. Mortality in Behçet's disease. Arthritis Rheum. 2010;62:2806–2812. doi: 10.1002/art.27568. [DOI] [PubMed] [Google Scholar]
- 14.Serdaroğlu P. Behçet's disease and the nervous system. J Neurol. 1998;245:197–205. doi: 10.1007/s004150050205. [DOI] [PubMed] [Google Scholar]
- 15.Siva A, Fresko II. Behçet's Disease. Curr Treat Options Neurol. 2000;2:435–448. doi: 10.1007/s11940-000-0042-x. [DOI] [PubMed] [Google Scholar]
- 16.Sugasawa J, Ishikawa S. Vestibulo-ocular reflex abnormality in Behçet's disease. Jpn J Ophthalmol. 1986;30:91–99. [PubMed] [Google Scholar]