Abstract
Working memory impairment is considered a core deficit in schizophrenia, but the precise nature of this deficit has not been determined. Multiple lines of evidence implicate deficits at the encoding stage. During encoding, information is held in a precategorical sensory store termed iconic memory, a literal image of the stimulus with high capacity but rapid decay. Pathologically increased iconic decay could reduce the number of items that can be transferred into working memory before the information is lost and could thus contribute to the working memory deficit seen in the illness. The current study used a partial report procedure to test the hypothesis that patients with schizophrenia (n = 37) display faster iconic memory decay than matched healthy control participants (n = 28). Six letters, arranged in a circle, were presented for 50 ms. Following a variable delay of 0–1000 ms, a central arrow cue indicated the item to be reported. In both patients and control subjects, recall accuracy decreased with increasing cue delay, reflecting decay of the iconic representation of the stimulus array. Patients displayed impaired memory performance across all cue delays, consistent with an impairment in working memory, but the rate of iconic memory decay did not differ between patients and controls. This provides clear evidence against faster loss of iconic memory representations in schizophrenia, ruling out iconic decay as an underlying source of the working memory impairment in this population. Thus, iconic decay rate can be added to a growing list of unimpaired cognitive building blocks in schizophrenia.
Keywords: schizophrenic, working memory, encoding, capacity, sensory store
Introduction
Among the neurocognitive impairments identified in schizophrenia, working memory impairment is considered a core deficit.1–3 Working memory refers to the short-term storage of information in the service of ongoing cognitive tasks4; information represented in working memory is available for further processing and decision making. Thus, the ability to encode, maintain, and retrieve information from working memory is crucial for a broad range of cognitive operations and everyday functioning.
To date, there is little consensus on what aspect or core component of working memory performance may be the central underlying deficit in schizophrenia. A primary deficit in the maintenance of information stored in working memory would cause impairments to worsen with longer delays between encoding and retrieval. Although some studies have found evidence in favor of this hypothesis,5–7 differences in delay period do not explain between-study variations in working memory performance, and patients show deficits even at very short delays.8 Thus, although maintenance deficits may exist, they do not appear to lie at the heart of the working memory impairment. Deficits at the retrieval stage, although they may exist, also appear an unlikely candidate for a primary underlying deficit because patients exhibit impaired performance in delayed match-to-sample paradigms that are designed to minimize retrieval demands.9–12 There is more robust evidence to suggest a primary impairment in the encoding stage. Patients with schizophrenia need more uninterrupted processing time to build a stable working memory representation,10,11,13,14 and encoding deficits can sometimes be reduced by longer stimulus exposure.9,11,12 These findings point toward impairments in the initial perceptual and/or encoding processes that transform a fleeting perceptual representation into a more durable working memory representation.
Encoding information into visual working memory involves a sequence of steps in which sensory information is increasingly categorized and interpreted. Visual stimuli are initially held in iconic memory, a low-level precategorical memory system that contains a literal image of the just extinguished stimulus, with high capacity but rapid decay.15 Iconic memory provides the inputs that may be transformed into working memory representations. The transfer of each item from iconic into working memory takes time16; thus, slow iconic decay enables more items to be transferred and consolidated before the information is lost. Conversely, fast iconic decay would reduce the information that is available for working memory encoding.
The current study tested the hypothesis that patients with schizophrenia display an accelerated loss of information from iconic memory storage, which could explain reduced working memory capacity as well as performance benefits from longer stimulus exposure (enabling stimulus encoding from physical rather than iconic representations). Thus, working memory deficits in schizophrenic patients may reflect an encoding deficit based on an inability to work from a low-level “snapshot” of the sensory stimulus held in iconic memory.
Previous research in the 1970s has provided suggestive but inconclusive evidence of faster iconic decay in schizophrenia. This possibility was first raised in the context of experiments on the “span of apprehension,” the number of items that can be attended at once. These tasks tap into several functions, including rate of iconic decay, rate of conversion from iconic into working memory, and serial scanning. Findings that schizophrenic patients performed worse on these tasks17 prompted further exploration of iconic decay rates. Another approach was to employ a picture integration task in which 2 slides of random lines were tachistoscopically flashed in alternation and complemented each other to yield a picture. Increasing the stimulus onset asynchrony (SOA) between the picture pairs progressively decreases recognition accuracy, reflecting the decay of the icon. Schizophrenia patients displayed decay rates equal to that of normal controls.18 However, using stimuli of lower salience in the same procedure, another study19 found trends toward faster decay in patients.
The most common procedure for isolating iconic memory in the basic science literature is the partial report technique.20 An array of items is presented briefly. Shortly after its offset, a small subset of the array is cued, indicating the items to be reported. Because the participant does not know which items will be sampled prior to the cue, the percentage of correctly recalled sample items reflects the percentage of the entire array available for report at the time of cueing. If the delay between array offset and cue onset is short, healthy subjects are able to report most or all of the cued items, indicating that all or most of the items in the whole array were present in iconic memory at the time of the cue. As the cue delay increases, performance decreases, until, at long delays, only items that made the transfer into short-term memory without the benefit of cueing are recalled. Thus, the rate at which performance falls off between short and long delays reflects the rate of decay of the iconic memory. For example, patients with Mild Cognitive Impairment (MCI) displayed faster iconic memory decay in this paradigm, and individual decay rates were associated with dementia ratings and may account for a range of mnemonic deficits.21 The Sperling partial report technique has been used in only 1 previous experiment on schizophrenia.22 Some patient subgroups exhibited impaired performance, but the impairment did not consist of a faster rate of decay. Instead, these patient subgroups failed to use the cue information at all, with poor performance observed at all delay intervals. This impairment may have resulted from an inability to select the relevant items, rather than a deficit in iconic storage. However, more recent research has directly tested the ability of schizophrenia patients to use spatial cues to select parts of a stimulus array for memory encoding and found no deficit.23 Thus, factors specific to their experimental procedures may have prevented the older partial report study22 from measuring the rate of iconic decay in some of the patients. In summary, the literature to date, some of which predates modern diagnostic criteria, does not provide a clear answer to the question of whether the rate of iconic decay is increased in schizophrenia.
The present study was designed to provide a definitive answer to this question by using a well-validated version of the partial report technique, based on the MCI study,21 to measure the rate of iconic decay. A large number of SOAs between target array and cue onset were used to ensure coverage of each part of the decay curve. We contrasted 2 competing hypotheses. One hypothesis states that iconic memory is dysfunctional in schizophrenia, leading to a faster rate of decay but normal or near-normal performance at short cue delays (ie, before significant iconic decay has occurred). The alternative hypothesis states that iconic memory is not the source of working memory impairment in schizophrenia; a normal iconic memory decay rate coupled with delay-independent impairment of overall task performance would support this latter hypothesis.
Methods
Participants
Thirty-seven patients meeting Diagnostic and Statistical Manual of Mental Disorders (Fourth Revision, American Psychiatric Association, 1994) criteria for schizophrenia (N = 15 paranoid, 18 undifferentiated, 1 disorganized, 2 residual) or schizoaffective disorder (N = 1) and 28 matched healthy control subjects participated in this study. Diagnosis was established using a best estimate approach in which information from a Structured Clinical Interview for DSM-IV (SCID) was combined with a review of patient medical records at a consensus diagnosis meeting chaired by 1 of the authors (J.G.). Demographic information is summarized in table 1. Groups did not differ in age (t63 = 1.41, P > .16), parental education (t60 = 0.30, P > .7), sex, or ethnicity (χ2 P > 0.8 in both cases). However, patients had significantly fewer years of education than controls (t63 = 3.60, P < .001).
Table 1.
Group Demographics
| Patients | Controls | |
| Age | 42.7 ± 9.5 (range 18–56) | 46.1 ± 9.7 (range 21–58) |
| Male:female | 27:10 | 21:7 |
| AA:A:C:O | 14:0:23:0 | 10:0:18:0 |
| Education (years) | 12.5 ± 2.2* | 14.7 ± 2.6 |
| Parental educationa | 12.9 ± 2.8b | 12.7 ± 2.7 |
| WAIS-III IQc | 90.9 ± 16.8d* | 108.0 ± 16.3 |
| WRAT-3 standard score | 97.2 ± 14.0b | 103.0 ± 11.6d |
| WTAR standard score | 96.3 ± 17.5e* | 107.9 ± 15.6d |
| RBANS total scale score | 82.4 ± 12.6e* | 104.5 ± 14.7 |
| WMS-III Spatial Span | 8.8 ± 3.4c* | 11.0 ± 2.6 |
Note: AA, African American; A, Asian; C, Caucasian; O, Other; WAIS-III, Wechsler Adult Intelligence Scale version 3; IQ, intelligence quotient; WRAT-3, Wide Range Achievement Test version 3; WTAR, Wechsler Test for Adult Reading; RBANS, Repeatable Battery for the Assessment of Neuropsychological Status; WMS-III, Wechsler Memory Scale version 3.
Average over mother’s and father’s years of education.
Data unavailable for 3 subjects.
IQ estimate based on 4 WAIS subscales: information, block design, arithmetic and symbol search.
Data unavailable for 2 subjects.
Data unavailable for 1 subject.
Significant (P < .01) difference between patients and controls in independent-samples t test.
The patients were clinically stable outpatients. At the time of testing, patients obtained a total score of 36.5 ± 9.6 (mean ± SD) on the Brief Psychiatric Rating Scale (range 21–70) and 35.2 ± 18.5 on the Scale for the Assessment of Negative Symptoms (range 8–88). All patients were receiving antipsychotic medication at the time of testing; 4 were treated with first-generation antipsychotics, 30 with second-generation antipsychotics, and 3 with both. Thirteen patients additionally received mood-stabilizing medication, 8 anxiolytic, and 4 antiparkinsonian medication. One patient was also treated with a cholinesterase inhibitor. Only patients whose medication had not changed in the preceding 4 weeks were enrolled. Control participants were recruited from the community and had no Axis I or II diagnoses as established by a SCID, had no family history of psychosis, and were not taking any psychotropic medication. All participants provided informed consent for a protocol approved by the University of Maryland School of Medicine Institutional Review Board.
Neuropsychological Testing
All participants completed 6 subscales of the Wechsler Adult Intelligence Scale version 3 (WAIS-III): the information subscale, block design, arithmetic, symbol search, digit symbol, and letter number sequencing. Intelligence quotient (IQ) was estimated based on the first 4 subtests. (While the information, block design, arithmetic, and digit symbol subtests had been suggested as the combination that most fully accounted for the variance in full-scale IQ in schizophrenic patients,24 we included symbol search instead of the digit symbol subtest for IQ estimation to reduce the role of motor speed in the estimation of processing speed.) Subjects furthermore completed the Wide Range Achievement Test version 3 (WRAT-3), the Wechsler Test for Adult Reading (WTAR), the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), and the Wechsler Memory Scale version 3 (WMS-III) Spatial Span subtest. These tests were usually performed on a separate day to avoid fatiguing subjects. Total scores are summarized in table 1. Patients scored lower than controls on WAIS-III, WTAR, RBANS, and WMS-III Spatial Span (P < .01 in each case, independent-samples t tests).
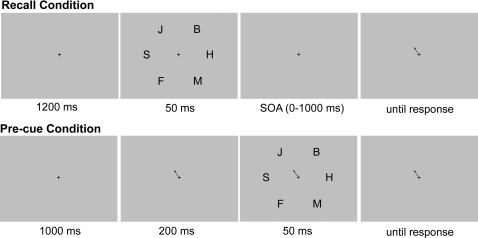
Stimuli
The stimuli, which were presented on a cathode ray tube video display at a viewing distance of 70 cm, are illustrated in figure 1. On each trial, 6 letters were presented in black on a gray (11.09 cd/m2) background for 50 ms. Each letter was chosen at random, without replacement from the set B, C, D, F, H, J, K, L, M, Q, S, T, V, X, Y. The letters subtended 0.6–1.5° horizontally and 1.4–1.7° vertically, with a 0.3°-wide stroke. The 6 letters were equally spaced around a notional circle with a 3.51° radius around the central fixation point. Cues were 0.87° × 0.34° arrows drawn in black, originating at 0.76° from the center of the screen.
Fig. 1.
Sequence of Events in the Partial Report Procedure Employed to Estimate Iconic Decay Rates. Participants verbally reported the letter that was cued by the central arrow. SOA = stimulus onset asynchrony.
Procedure
Each trial started with a black fixation cross presented at the center of the display for 1200 ms. The array of 6 letters was then presented for 50 ms. A cue pointing to 1 letter was presented at 1 of 12 SOAs: 0, 33, 67, 100, 150, 200, 250, 350, 500, 750, and 1000 ms (from letter array onset to cue onset). Subjects were instructed to verbally report the letter that had been presented in the cued location, and the experimenter entered the response using the keyboard. Responses were not restricted to the set of letters from which the stimuli were chosen. In precue trials, the cue was presented 200 ms before the onset of the letter array. In all conditions, the cue stayed on until a response was made.
The experiment consisted of 648 trials (54 at each cue SOA and 54 precue trials), administered over 3 blocks. Short breaks were provided every 20 trials, with longer breaks between blocks. Prior to the experiment, instructions were provided, including a PowerPoint presentation, followed by 1 practice block of 20 trials. Additional practice blocks were administered if needed.
Data Analysis
The percentage of correct responses was determined for each SOA. These percentages were then transformed into the sensitivity index d′ to minimize skewing and maximize normality.25
Schizophrenia patients often exhibit lower overall levels of accuracy in cognitive tasks, and these differences make it more difficult to assess decay rates. That is, the shape of the decay curve will depend on whether overall accuracy is high or low even if the rate of decay is the same (eg, the curve will appear to be shallow if performance is already low at short delays). Thus, conventional linear analyses on the accuracy or d′ values would be inappropriate. Instead, we used the approach employed in the MCI study,21 in which the rate of memory decay was estimated with a curve-fitting procedure. Specifically, each participant's d′ scores at the different SOAs were fit with a simple exponential decay function: d′(SOA) = a + Δe−SOA/τ, where a is the asymptotic d′ value, Δ is the difference between the d′ value at an SOA of 0 ms and the asymptotic d′ value, and τ is the time constant for the decay process. A simplex gradient descent algorithm was used to find the set of parameters that produced the best fit (lowest root mean squared error) between the model and the observed d′ values. Neither group reached asymptote within the tested range of SOAs, and this led to considerable variance in both the asymptote and the Δ parameter estimates. Thus, these parameters were not used in the group comparisons.
The time constant is the parameter of interest and describes the amount of time required for the memory to decay to 1/e (37%) of its current value. A larger time constant reflects a slower decay rate. Importantly, the time constant assesses decay rate independently of the overall performance level. The time constant parameter was compared between patients and healthy controls with an independent-sample t test. Overall performance was quantified as the average d′ across all cue delays and was also tested with an independent-sample t test. Levene’s tests determined whether t tests assumed equal or unequal variances (equal unless otherwise specified). The time constant parameter and average d′ scores underwent Pearson correlation with the WAIS-III subtests and IQ estimate, the WRAT-3 and WTAR, and with WMS-III Spatial Span.
Results
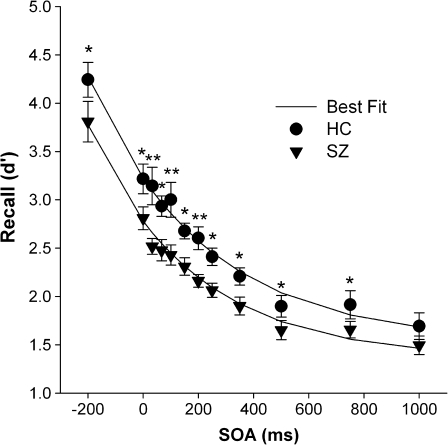
Figure 2 shows d′ scores as a function of the SOA between the letter array and the cue. Online supplementary figure 1 shows the raw percent correct data before transformation into d′. For both patients and control subjects, d′ was highest in the precue condition and declined in a negatively accelerated manner as the SOA increased. The d′ scores were lower in patients than in control subjects by an approximately equivalent amount across all SOAs, such that decay curves almost paralleled each other.
Fig. 2.
Mean Memory Performance, Reflected by Discrimination Index d′, in Patients With Schizophrenia (SZ, n = 37) and Matched Healthy Control Subjects (HC, n = 28) Across a Range of Delay Periods Between Target Array Onset and Cue Onset (Stimulus Onset Asynchrony, SOA). Error bars reflect 95% confidence intervals, adjusted to remove within-group between-subject variability in average d′ scores across SOAs.36
When the curve-fitting procedure was applied, the goodness of fit between the observed and predicted d′ values was quite high for both the patient group (average Pearson r = 0.94) and the healthy control group (r = 0.94). There was no difference between groups in the mean goodness of fit (Fisher’s z transformation test for difference in correlation: z = 0.19, P > .8) or in the mean total estimate error (independent-samples t test, unequal variances: t44 = 1.33, P > .19). Thus, the curve-fitting procedure modeled the data in the 2 groups equally well.
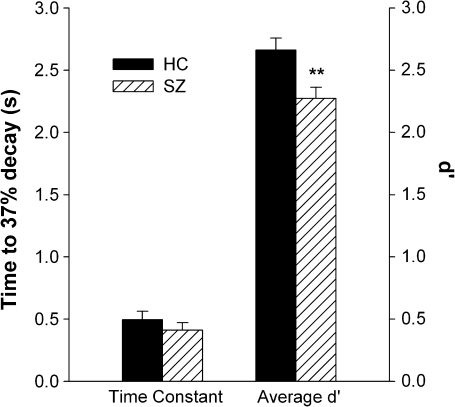
The mean time constant estimates and overall d′ scores for the patients and control subjects are shown in figure 3. The key finding was that the time constant did not differ between groups (t63 = 0.93, P > .35). That is, consistent with the parallel decay curves, the rate of iconic decay was similar for patients with schizophrenia and healthy control subjects. However, overall performance was impaired in patients, leading to a significant group difference in the average d′ scores across SOA (t63 = 2.94, P = 0.005, Cohen’s d = 0.75).
Fig. 3.
Mean Time Constant Estimates (± SEM) and Overall d′ Scores, Averaged Across Delay Intervals, for Patients With Schizophrenia (SZ) and Healthy Control Subjects (HC).
Iconic decay rate, as indexed by the time constant parameter, was not significantly correlated with any measure of neuropsychological performance, neither in patients nor in controls, nor with psychiatric symptom ratings. However, in patients, average d′ scores correlated robustly with WRAT (R = 0.52, P = .002) and WTAR (R = 0.51, P = .002) scores. These tests are based on single-word reading performance and are thought to reflect premorbid crystallized intelligence. The information subscale of the WAIS-III is also thought to assess crystallized intelligence but did not correlate with average d′ (R = 0.15, P = .4). Thus, it is more likely that the correlations with WTAR and WRAT reflect poorer reading performance in patients with low average d′. To explore this further, we excluded subjects with standardized WTAR/WRAT scores below 85 (n = 8, all patients) and repeated group comparisons of the time constant and average d′. The average d′ increased from 2.27 (n = 37) to 2.4 (n = 29) in the patients and thus moved closer to the healthy control average of 2.66, although the group difference was still marginally significant (t55 = 1.96, P = .06). Thus, differences in reading ability appear to at least partially explain the difference in overall performance. There was still no group difference in the time constant (P > .3) when the patients with low WTAR/WRAT scores were removed from the analysis.
Marginally significant correlations were also identified in the patient group between the average d′ value and several WAIS-III subscales (block design: r = 0.34; digit symbol: r = 0.41; letter number sequencing: r = 0.41; P < .05 in each case), WAIS-III estimated full-scale IQ (r = 0.34, P < .05), and the WMS-III Spatial Span subtest (r = 0.35, P < .05). In healthy controls, the only significant correlation of average d′ was with WAIS-III Symbol Search (r = 0.38, P < 0.05).
Discussion
The current experiment was designed to test the hypothesis that iconic memory representations decay more rapidly in schizophrenia patients. Such a finding would pinpoint a circumscribed processing deficit that could explain frequently reported reductions in working memory capacity and their alleviation by longer stimulus displays. The current findings rule out this explanation.
Although overall accuracy was reduced in the patients, similar reductions were seen at each SOA. The key finding is that performance in patients and healthy control participants deteriorated at the same rate with increasing cue delay. The longer the delay between target array and cue, the longer an iconic representation of the entire array has to survive to facilitate recall performance. The decay in recall with cue delay thus reflects the decay rate of iconic memory representations. Decay curves of patients and control participants were almost parallel and were characterized by similar time constants, indicating that patients with schizophrenia display normal temporal dynamics of these early sensory representations. The present results thus speak against faster iconic decay as an explanation for working memory impairment in schizophrenia.
Faster iconic decay has also been suggested to underlie deficits in span of apprehension tasks, where patients with schizophrenia tend to reproduce fewer items or detect fewer target items from briefly presented item arrays.17 Performance of these tasks is thought to require scanning the array in iconic memory. The present results do not support faster iconic decay as the underlying problem and suggest that deficits in other domains are responsible. For example, schizophrenia patients exhibit slower scanning in visual search tasks that do not require memory storage,26–29 and a slowed scanning rate could at least partially explain the reduced span of apprehension performance.
Although it is difficult to interpret the absence of a significant group difference as indication of equal group performance, the data from this experiment were quite clean: The pattern of changes in d′ across SOAs was very orderly in both groups, with tight 95% confidence intervals at each SOA (see figure 2), and the data were fit extremely well with a simple exponential function. These factors indicate that measurement error was relatively low, as would be expected given the large number of trials tested at each SOA (54 per subject). Moreover, we tested a relatively large sample of patients (n = 37) and control subjects (n = 28), minimizing sampling error. Despite this, the group difference in iconic decay rates did not even approach significance. Thus, although we cannot conclude that the decay rate is completely unaffected in schizophrenia, it is unlikely that the disease produces a meaningful change in iconic decay.
We obtained a significant group difference in the average d′ score, which reflects overall task performance independent of when the cue was presented. There are many possible explanations for this delay-independent impairment in patients. It may reflect impaired icon formation (rather than maintenance), such that slowed or impaired sensory processing may have reduced the number of items entering iconic storage in the first place or led to low-quality representations. Indeed, greater backward masking effects on the identification of briefly presented stimuli have been suggested to reflect greater disruption of icon formation in schizophrenia.30 Furthermore, previous studies suggest that adjusting perceptual difficulty by increasing stimulus presentation time or facilitating sensory discrimination can reduce deficits of schizophrenia patients in working memory tasks.9,12,31
The finding that even precue performance was impaired in patients supports that visual processing may have been a limiting factor across cue delays. Previous studies suggest abnormalities in magnocellular pathway functioning that are associated with impaired object recognition and reading ability.32,33 The observed correlations of the overall d′ value with WRAT and WTAR scores suggest that reading proficiency may indeed be a performance-limiting factor for some patients, and excluding patients with WRAT/WTAR scores more than 1 SD below population average reduced the group difference. Thus, impaired processing of the letter identities, possibly based on visual processing abnormalities, could explain the lower overall d′ in patients. However, the curve-fitting procedure used to quantify decay rates is independent of the overall accuracy level, so any differences in perceptibility would not have confounded the measurement of iconic decay.
Further explanations for the delay-independent impairment include deficits in sustained attention and alertness that may have caused problems allocating sufficient information processing resources to the task or patients may on random trials not have paid attention to the target array at all. Alternatively or additionally, the reduced recall accuracy across cue delays may reflect the working memory deficit typically seen in schizophrenia. Working memory encoding, maintenance, and decision processes are equally necessary at all cue delays in this paradigm, and deficits in one or more of these processes would explain the observed pattern of delay-independent performance reduction. Significant correlations of overall d′ scores with WAIS subtests of processing speed, attention, and working memory confirm that patient performance was partially determined by such general ability functions.
The present results contradict previous partial report findings in schizophrenia patients,22 where impairments consisted of certain patient subgroups (“underinclusives” and “middle inclusives”) not taking any advantage of the cue information at any delay. In the present study, each participant's recall performance was SOA dependent, indicating that all patients used the cue information to select and process the relevant target item. That is consistent with other recent results indicating that the ability to selectively encode portions of a stimulus array is not impaired in schizophrenia.23 We can only speculate about possible reasons underlying the failure of some patients’ to use the cue in the previous study.22 One difference to the present procedure was that 3 out of 9 items were cued in the previous study, but only a single item was cued in the present study. This subselection may have exceeded some patients’ working memory capacity to a degree that cueing still provided little benefit over whole report. In addition, given that this previous study was performed in an era marked by different diagnostic and clinical practices than modern-day psychiatry, it is likely that the different patterns of results were at least partially a result of differences in the patient populations being sampled.
In addition to demonstrating that patients were able to use the cue to direct attention to an item for further processing, the present results also demonstrate that the speed of cue processing and attention shifting was unimpaired in patients. That is, if patients had been slowed to shift attention to the cued location, this would have been equivalent to lengthening the delay between the letter array and the cue, which would have produced a rightward shift in the function relating cue delay to d′. Instead, we observed a downward shift. This is consistent with a prior study that used both psychophysical and electrophysiological measures to assess the speed with which attention shifts in schizophrenia patients and control subjects.34 This prior study found that, with the exception of a small number of outlier patients, schizophrenia does not lead to slowed shifting of visual-spatial attention. Moreover, many studies using variants of the Posner orienting paradigm have shown that patients are able to use central arrow cues to facilitate shifts of spatial attention. The present study extends these results by showing that patients are able to use cues to direct attention within iconic memory representations. This provides converging evidence that patients with schizophrenia are able to use selective attention to facilitate performance across a range of perceptual and working memory encoding tasks.
The present study settles an old controversy18,19,22 by demonstrating that iconic memory representations decay at the same rate in patients with schizophrenia as in healthy control subjects. On the basis of this finding, faster iconic decay can be excluded as a mechanism underlying working memory deficits in schizophrenia. The present results add to the recently reviewed evidence35 that a range of cognitive mechanisms is remarkably unimpaired in schizophrenia.
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Funding
National Institute of Mental Health (MH065034 to J.M.G. and S.J.L.).
Supplementary Material
Acknowledgments
We thank Rebecca C. Wilbur for her assistance in the conduct of this study. We extend thanks to all volunteers participating in this study.
References
- 1.Goldman-Rakic PS. Working memory dysfunction in schizophrenia. J Neuropsychiatry Clin Neurosci. 1994;6:348–357. doi: 10.1176/jnp.6.4.348. [DOI] [PubMed] [Google Scholar]
- 2.Gold JM, Carpenter C, Randolph C, Goldberg TE, Weinberger DR. Auditory working memory and Wisconsin Card Sorting Test performance in schizophrenia. Arch Gen Psychiatry. 1997;54:159–165. doi: 10.1001/archpsyc.1997.01830140071013. [DOI] [PubMed] [Google Scholar]
- 3.Barch DM. The cognitive neuroscience of schizophrenia. Annu Rev Clin Psychol. 2005;1:321–353. doi: 10.1146/annurev.clinpsy.1.102803.143959. [DOI] [PubMed] [Google Scholar]
- 4.Baddeley AD. Working Memory. Oxford, England: Clarendon; 1986. [Google Scholar]
- 5.Park S, Holzman PS. Schizophrenics show spatial working memory deficits. Arch Gen Psychiatry. 1992;49:975–982. doi: 10.1001/archpsyc.1992.01820120063009. [DOI] [PubMed] [Google Scholar]
- 6.Barch DM, Carter CS, MacDonald AW, III, Braver TS, Cohen JD. Context-processing deficits in schizophrenia: diagnostic specificity, 4-week course, and relationships to clinical symptoms. J Abnorm Psychol. 2003;112:132–143. [PubMed] [Google Scholar]
- 7.Stephane M, Pellizzer G. The dynamic architecture of working memory in schizophrenia. Schizophr Res. 2007;92:160–167. doi: 10.1016/j.schres.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 8.Lee J, Park S. Working memory impairments in schizophrenia: a meta-analysis. J Abnorm Psychol. 2005;114:599–611. doi: 10.1037/0021-843X.114.4.599. [DOI] [PubMed] [Google Scholar]
- 9.Lencz T, Bilder RM, Turkel E, et al. Impairments in perceptual competency and maintenance on a visual delayed match-to-sample test in first-episode schizophrenia. Arch Gen Psychiatry. 2003;60:238–243. doi: 10.1001/archpsyc.60.3.238. [DOI] [PubMed] [Google Scholar]
- 10.Fuller RL, Luck SJ, McMahon RP, Gold JM. Working memory consolidation is abnormally slow in schizophrenia. J Abnorm Psychol. 2005;114:279–290. doi: 10.1037/0021-843X.114.2.279. [DOI] [PubMed] [Google Scholar]
- 11.Fuller RL, Luck SJ, Braun EL, Robinson BM, McMahon RP, Gold JM. Impaired visual working memory consolidation in schizophrenia. Neuropsychology. 2009;23:71–80. doi: 10.1037/a0013854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tek C, Gold J, Blaxton T, Wilk C, McMahon RP, Buchanan RW. Visual perceptual and working memory impairments in schizophrenia. Arch Gen Psychiatry. 2002;59:146–153. doi: 10.1001/archpsyc.59.2.146. [DOI] [PubMed] [Google Scholar]
- 13.Saccuzzo DP, Hirt M, Spencer TJ. Backward masking as a measure of attention in schizophrenia. J Abnorm Psychol. 1974;83:512–522. doi: 10.1037/h0037072. [DOI] [PubMed] [Google Scholar]
- 14.Hartman M, Steketee MC, Silva S, Lanning K, McCann H. Working memory and schizophrenia: evidence for slowed encoding. Schizophr Res. 2002;59:99–113. doi: 10.1016/s0920-9964(01)00366-8. [DOI] [PubMed] [Google Scholar]
- 15.Irwin DE, Thomas LE. Visual sensory memory. In: Luck SJ, Hollingsworth A, editors. Visual Memory. New York, NY: Oxford University Press; 2008. pp. 9–33. [Google Scholar]
- 16.Vogel EK, Woodman GF, Luck SJ. The time course of consolidation in visual working memory. J Exp Psychol Hum Percept Perform. 2006;32:1436–1451. doi: 10.1037/0096-1523.32.6.1436. [DOI] [PubMed] [Google Scholar]
- 17.Asarnow RF, Granholm E, Sherman T. Span of apprehension in schizophrenia. In: Steinhauer SR, Gruzelier JH, Zubin J, editors. Handbook of Schizophrenia, Vol. 5: Neuropsychology, Psychophysiology and Information Processing. New York, NY: Elsevier Science Publishers B.V.; 1991. pp. 335–370. [Google Scholar]
- 18.Knight R, Sherer M, Putchat C, Carter G. A picture integration task for measuring iconic memory in schizophrenics. J Abnorm Psychol. 1978;87:314–321. [PubMed] [Google Scholar]
- 19.Spaulding W, Rosenzweig L, Huntzinger R, Cromwell RL, Briggs D, Hayes T. Visual pattern integration in psychiatric patients. J Abnorm Psychol. 1980;89:635–643. doi: 10.1037//0021-843x.89.5.635. [DOI] [PubMed] [Google Scholar]
- 20.Sperling G. The information available in brief visual presentations. Psychol Monogr. 1960;74:1–29. [Google Scholar]
- 21.Lu ZL, Neuse J, Madigan S, Dosher BA. Fast decay of iconic memory in observers with mild cognitive impairments. Proc Natl Acad Sci USA. 2005;102:1797–1802. doi: 10.1073/pnas.0408402102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knight R, Sherer M, Shapiro J. Iconic imagery in overinclusive and nonoverinclusive schizophrenics. J Abnorm Psychol. 1977;86:242–255. doi: 10.1037//0021-843x.86.3.242. [DOI] [PubMed] [Google Scholar]
- 23.Gold JM, Fuller RL, Robinson BM, McMahon RP, Braun EL, Luck SJ. Intact attentional control of working memory encoding in schizophrenia. J Abnorm Psychol. 2006;115:658–673. doi: 10.1037/0021-843X.115.4.658. [DOI] [PubMed] [Google Scholar]
- 24.Blyler CR, Gold JM, Iannone VN, Buchanan RW. Short form of the WAIS-III for use with patients with schizophrenia. Schizophr Res. 2000;46:209–215. doi: 10.1016/s0920-9964(00)00017-7. [DOI] [PubMed] [Google Scholar]
- 25.Macmillan NA, Creelman CD. Detection Theory: A User's Guide. New York, NY: Cambridge University Press; 1991. [Google Scholar]
- 26.Mori S, Tanaka G, Ayaka Y, et al. Preattentive and focal attentional processes in schizophrenia: a visual search study. Schizophr Res. 1996;22:69–76. doi: 10.1016/0920-9964(96)00049-7. [DOI] [PubMed] [Google Scholar]
- 27.Carr VJ, Dewis SA, Lewin TJ. Preattentive visual search and perceptual grouping in schizophrenia. Psychiatry Res. 1998;79:151–162. doi: 10.1016/s0165-1781(98)00035-3. [DOI] [PubMed] [Google Scholar]
- 28.Fuller RL, Luck SJ, Braun EL, Robinson BM, McMahon RP, Gold JM. Impaired control of visual attention in schizophrenia. J Abnorm Psychol. 2006;115:266–275. doi: 10.1037/0021-843X.115.2.266. [DOI] [PubMed] [Google Scholar]
- 29.Gold JM, Fuller RL, Robinson BM, Braun EL, Luck SJ. Impaired top-down control of visual search in schizophrenia. Schizophr Res. 2007;94:148–155. doi: 10.1016/j.schres.2007.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Green MF, Nuechterlein KH, Mintz J. Backward masking in schizophrenia and mania. II. Specifying the visual channels. Arch Gen Psychiatry. 1994;51:945–951. doi: 10.1001/archpsyc.1994.03950120017004. [DOI] [PubMed] [Google Scholar]
- 31.Javitt DC, Liederman E, Cienfuegos A, Shelley AM. Panmodal processing imprecision as a basis for dysfunction of transient memory storage systems in schizophrenia. Schizophr Bull. 1999;25:763–775. doi: 10.1093/oxfordjournals.schbul.a033417. [DOI] [PubMed] [Google Scholar]
- 32.Revheim N, Butler PD, Schechter I, Jalbrzikowski M, Silipo G, Javitt DC. Reading impairment and visual processing deficits in schizophrenia. Schizophr Res. 2006;87:238–245. doi: 10.1016/j.schres.2006.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Javitt DC. When doors of perception close: bottom-up models of disrupted cognition in schizophrenia. Annu Rev Clin Psychol. 2009;5:249–275. doi: 10.1146/annurev.clinpsy.032408.153502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luck SJ, Fuller RL, Braun EL, Robinson B, Summerfelt A, Gold JM. The speed of visual attention in schizophrenia: electrophysiological and behavioral evidence. Schizophr Res. 2006;85:174–195. doi: 10.1016/j.schres.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 35.Gold J, Hahn B, Strauss GP, Waltz JA. Turning it upside down: areas of preserved cognitive function in schizophrenia. Neuropsychol Rev. 2009;19:294–311. doi: 10.1007/s11065-009-9098-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cousineau D. Confidence intervals in within-subject designs: a simpler solution to Loftus and Masson's method. Tutorials Quant Methods Psychol. 2007;1:42–45. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.