Abstract
Introduction:
Transversus abdominis plane (TAP) block is a new regional analgesic technique for postoperative pain in abdominal surgery. Its efficacy is not clear, and thus it needs to be explored for its regular utilisation on prolonged period. The objective was to study the continuous local anaesthetic infusion effect on postoperative analgesia. Continuous use of TAP block as an analgesic technique has not been evaluated prospectively in clinical trials. This study evaluates the efficacy of ultrasound-guided TAP block in comparison with PCA fentanyl in major abdominal surgery.
Materials and Methods:
There were 20 patients in the study, allocated to TAP and control groups. The parameters measured were pain scores on a numerical rating scale (NRS) of 0-10 at various time intervals and the amount of fentanyl used as rescue analgesia. Patient satisfaction scores were recorded in the TAP block group and along with any complications related to the block.
Results:
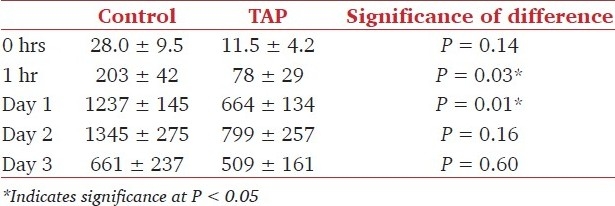
The postoperative median pain scores on coughing on day one were 6.0 for control group and 2.0 for the TAP group (P = 0.02); on day two, the equivalent scores were 7.0 and 2.0 (P = 0.01). The fentanyl requirement at one hour was 203 μ for the control group and 78 μg for the TAP group (P = 0.03); at day one, the control and TAP requirements were 1237 μg and 664 μg respectively (P = 0.01). Three TAP patients rated their satisfaction as ‘excellent’, four as ‘satisfied, and two as ‘poor’.
Conclusion:
TAP block is a promising technique for postoperative analgesia in major abdominal surgeries. Our study demonstrated lower pain scores in the TAP group with reduced fentanyl requirement. Further, a large scale study is needed to establish the efficacy of TAP block in this setting.
Keywords: PCA, postoperative pain, transversus abdominis plane, ultrasound
Introduction
In recent times, tremendous interest has evolved over the utility of Transversus Abdominis plane (TAP) blocks. TAP block has been used as a single-shot technique both by traditional landmark approach and ultrasound guidance over the four years.[1–9] These single-shot studies demonstrated decreased opioid use and pain scores, but the analgesic effect wore off in 24-48 hours. There has not been any clinical trial reporting continuous use of TAP block for a prolonged period. This study evaluates the ultrasound guided bilateral TAP block as a continuous analgesic technique after major abdominal surgery. The primary outcome was postoperative pain scores and amount of opioids used.
Materials and Methods
Twenty patients were prospectively included in this clinical trial, after permission at our institute. Patients having elective abdominal surgery with supra/infra-umbilical incisions were included. Patients opting for regional anesthesia or who were on long-term opioids were excluded. Informed written consent was obtained in the holding bay of the operating room suite. Randomisation of 20 patients was performed by alternating patients to either the TAP or control group.
General anesthesia (GA) was standardised in both groups using propofol 1-2 mg/kg (Propofol, Sandoz, Sydney NSW, Australia), rocuronium 0.5 mg/kg (Esmeron, Shering-Plough, Sydney, NSW, Australia), and fentanyl 100 μg (Fentanyl, Astra Zeneca, Sydney, NSW, Australia), used at preinduction and intubation and then up to 500 μg during maintenance. Maintenance of anesthesia was with 50:50 O2 and air with Sevoflurane. In the TAP group, the catheter was placed at the end of surgery, prior to extubation by the primary investigator under ultrasound guidance (Sonosite Inc Micromax, Bothell, WA, USA, PO 6468-10). In the control group, the mode of postoperative analgesia included regular Paracetamol (Perfalgan, Bristol-Myers Squibb, Victoria, Australia), 1 g 6 hourly and fentanyl patient controlled analgesia (PCA). In the TAP group, analgesia included continuous TAP block infusion, paracetamol 1 g 6 hourly and fentanyl PCA.
The technique used was posterior approach.[5] The investigator was scrubbed and gowned and the ultrasound probe was covered by a sterile plastic cover and placed in the midaxillary line just superior to the iliac crest [Figure 1]. After identifying the abdominal layers, the transversus abdominal plane was reached by using an 18-G Touhy's needle (Portex Epidural Minipack, Smiths Medical Australasia Pty, Brisbane, QLD, Australia). Correct placement of the needle tip was confirmed by injecting 5-10 ml of saline bilaterally. A bolus dose of 15 ml of 0.5% ropivacaine (Naropin, Astra Zeneca, Sydney, NSW, Australia) was administered [Figure 2]. The epidural catheter (Portex Epidural Minipack, Smiths Medical Australasia Pty, Brisbane, QLD, Australia) was then advanced cephalad up to the 10-15 cm skin mark. The needle was removed and catheter connected to a bacterial filter. A 0.2% ropivacaine infusion at 8-10 ml/ hr was continued for 72 hours on each side. Our technique involved placement of the bevel of the needle superiorly, and then inserting the catheter and to advance it as superiorly as possible. The catheter needs to be advanced normally up to the 10 cm mark but may require to be advanced up to 15 cm mark in obese patients.
Figure 1.

Tuohy needle (18-G) inserted anterior to Ultrasound transducer, which is held transversely in plane to perform the TAP block
Figure 2.
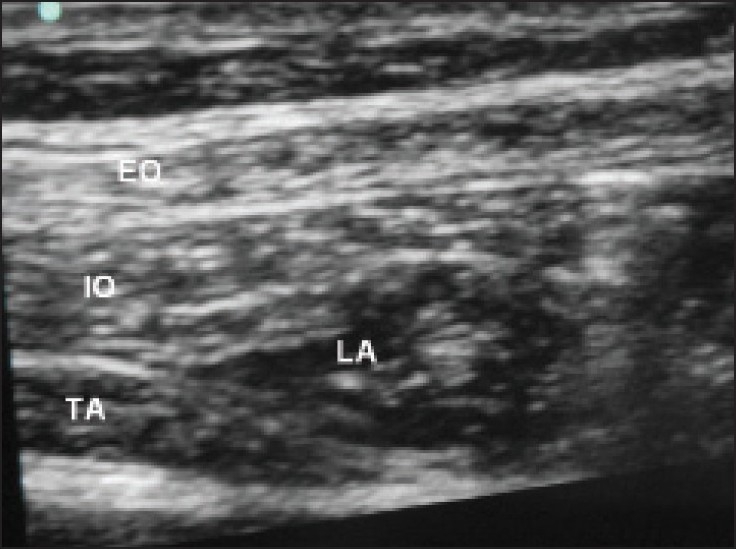
Sonographic image of the abdominal muscles layers with local anesthetic spread in TAP. EO = External oblique, IO = internal oblique, LA = local anaesthetic in TAP, TA = transversus abdominis muscle
Pain scores were recorded on a numerical rating scale (NRS) from 0-10 both at rest and on coughing. The recovery staff in the post-anesthesia care unit (PACU) recorded pain score on arrival and at 1 hour postoperatively. Generally, patients are discharged from PACU with adequate pain relief after 1 hour. The Acute Pain Service team recorded the pain scores in the ward from day one to day three. Other observations recorded included the amount of fentanyl used at various pain assessment times, number of episodes of nausea and vomiting, and complications related to the procedure or catheter placement. Additionally, in order to assess satisfaction in the TAP analgesia group, patients were asked to rate their pain relief as poor, satisfactory, or excellent.
The sample size was adequate to detect a difference of three units in pain score between its group at anytime point with a significance level of P = 0.05 and a power of 0.8. Pain scores are presented as median and interquartile range (IQR). Fentanyl use is presented as mean and standard error. Differences in pain scores were tested with a Mann–Whitney U test and differences in fentanyl use with a t test. All calculations were carried out using the R statistical language (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org
Results
There were no differences in age, sex, or the American Society of Anesthesiologists (ASA) classification between the groups. The pain scores and rescue analgesia are shown in Tables 1 and 2. Median pain scores were consistently lower in the TAP group, but only significantly so on days one and two on coughing and that on day two at rest. Rescue analgesia was required in PACU in both groups, but it was significantly less in the TAP group. This difference remained significant the next day.
Table 1.
Pain scores (median (IQR)) for control and TAP patients
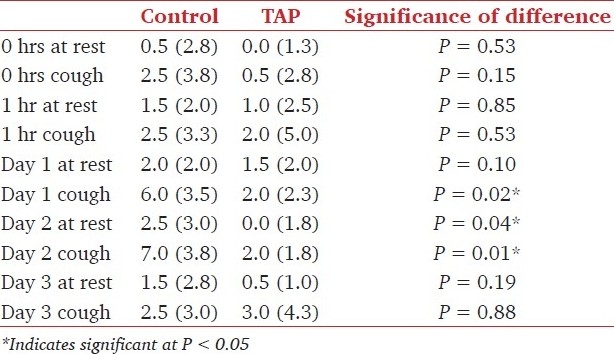
Table 2.
Fentanyl use in mg (mean ± SE) at each time point
Average recovery time was 81 ± 9 min for the TAP group (range, 60-120 min) and 91 ± 9 min for the control group (range, 50-135 min). The difference was not statistically significant (P = 0.44). The complications related to the TAP block were recorded in three patients: Disconnection from filter and catheter fell out (n = 1); leaking (n = 1); and increasing pain (n = 1). Control group patients experienced one episode of nausea and vomiting but none in the TAP group. Since this is a new technique, the satisfaction ratings were done in the TAP group only to compare to the previous experience of PCA. Out of 10 patients, two rated it as poor, four were satisfied, three had excellent scores, and one had no block.
Discussion
TAP analgesia is gaining place as a new regional analgesic technique for postoperative pain. Its role in major abdominal surgery is not fully defined. Our study demonstrates its probable efficacy in major abdominal surgery, in terms of reduced pain scores and opioid use in PACU on days one and two. Hebbard recommends a subcostal approach to achieve the block,[10] but it is technically difficult for upper abdominal surgery. We found that the posterior ultrasound-guided approach described by him was easier to perform in this setting.[5] To date, eight clinical trials reported single-shot use, of which one was a case series and the others were randomised trials. There were two audits and a case report on its continuous use[11–13] mostly in Intensive Care Unit as rescue analgesia and by surgeons inserting the catheter close to the wound.
McDonnell et al. conducted the first study and reported that a single-shot TAP block was effective even in supra-umbilical incision surgery.[2] To support this in their initial study, they performed TAP block through the Petit's triangle using local anaesthetic and dye and demonstrated, using magnetic resonance imaging, definite spread of dye in the transverse plane from superior margin of iliac crest to the level of costal margin.[14] In addition, their study on volunteers achieved sensory block to T7 dermatome level. To support this, we placed a catheter at the same depth as the subcostal approach with the skin mark at 10 cm or more. This eliminates the need for a subcostal TAP block for supra-umbilical incisions. We achieved low pain scores and reduced fentanyl requirement in the TAP group.
Shibita reported TAP block use in gynecological procedures with sensory block up to T10 and recommended its use only in lower abdominal surgery.[15] Laffey reported that that the upper level of the TAP block prior to full spread could be misleading. Measurement of the full block height was achieved gradually over several hours after the performance of block.[16] Our study also showed its maximal benefit on day 1, with lower pain scores in the TAP block group.
The limitation to our study is that the level of block was not assessed in all cases. A randomised trial on a larger scale might confirm this. We are planning to conduct such a trial in the future.
Technical problems encountered during the procedure included the need of an assistant to hold the transducer probe, to use large saline flush to confirm the space, and leakage around the catheter. The latter problem was solved by subcutaneous tunnelling of the catheter, with benefit to some patients. There are certain disadvantages in inserting the catheter before surgery. TAP dressing may be soiled with preparatory solutions and there is potential for dislodgement and removal of the catheter if the incision is extended. One of the postoperative issues was encroachment of the surgical dressing onto the catheter dressing. Based on the results of our study, we suggest that TAP block with multimodal analgesia plays an important role in postoperative analgesia but a large-scale study will be necessary.
Conclusions
TAP is a regional technique, which can be potentially used when the use of an epidural is contraindicated. There is however a need for fentanyl supplementation to cover visceral pain. Our study showed that combining TAP block with multimodal analgesia and fentanyl PCA gave satisfactory pain scores in major abdominal surgery.
Acknowledgments
We appreciate Dr Elizabeth Chye and Dr Venkat for the time spent on proof reading.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.O’Donnell BD, McDonnell JG, McShane AJ. The transversus abdominis plane block in open retropubic prostatectomy. Reg Anesth Pain Med. 2006;31:91. doi: 10.1016/j.rapm.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 2.McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg. 2007;104:193–7. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 3.McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after caesarean delivery: A randomized controlled trial. Anesth Analg. 2008;106:186–91. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 4.El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, et al. Ultrasound-guided transversus abdominis plane block: Description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102:763–7. doi: 10.1093/bja/aep067. [DOI] [PubMed] [Google Scholar]
- 5.Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35:616–7. [PubMed] [Google Scholar]
- 6.Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. Transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107:2056–60. doi: 10.1213/ane.0b013e3181871313. [DOI] [PubMed] [Google Scholar]
- 7.Niraj G, Searle A, Mathews M, Misra V, Baban M, Kiani S, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth. 2009;103:601–5. doi: 10.1093/bja/aep175. [DOI] [PubMed] [Google Scholar]
- 8.Belavy D, Cowalishaw PJ, Howes M, Phillips F. Ultrasound guided transversus abdominis plane block for analgesia after Caesarean delivery. Br J Anaesth. 2009;103:726–30. doi: 10.1093/bja/aep235. [DOI] [PubMed] [Google Scholar]
- 9.Costello JF, Moore AR, Wieczorek PM, Macarthur AJ, Balki M, Carvalho JC. The transversus abdominis plane block when used as part of multimodal regimen inclusive of intrathecal morphine, does not improve analgesia after caesarean delivery. Reg Anesth Pain Med. 2009;34:586–9. doi: 10.1097/aap.0b013e3181b4c922. [DOI] [PubMed] [Google Scholar]
- 10.Hebbard P. Subcostal transversus abdominis plane block under ultrasound guidance. Anesth Analg. 2008;106:674–5. doi: 10.1213/ane.0b013e318161a88f. [DOI] [PubMed] [Google Scholar]
- 11.Hebbard P. Audit of ‘rescue’ analgesia using TAP block. Anaesth Intensive Care. 2007;35:617–8. [PubMed] [Google Scholar]
- 12.Niraj G, Kelkar A, Fox AJ. Oblique sub-costal transversus abdominis plane (TAP) catheters: An alternative to epidural analgesia after upper abdominal surgery. Anaesthesia. 2009;64:1137–40. doi: 10.1111/j.1365-2044.2009.06006.x. [DOI] [PubMed] [Google Scholar]
- 13.Jankovic ZB, Pollard G, Nachiappan MM. Continuous transversus abdominis plane block for renal transplant recipients. Anesth Analg. 2009;109:1710–1. doi: 10.1213/ANE.0b013e3181ba75d1. [DOI] [PubMed] [Google Scholar]
- 14.McDonnell JG, O’Donnell BD, Farrell T, Gough N, Tuite D, Power C, et al. Transversus abdominis plane block: A cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32:399–404. doi: 10.1016/j.rapm.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Shibata Y, Sato Y, Fujiwara Y, Komatsu T. Transversus abdominis plane block. Anesth Analg. 2007;105:883. doi: 10.1213/01.ane.0000268541.83265.7d. [DOI] [PubMed] [Google Scholar]
- 16.McDonnell JG, Laffey JG. Transversus abdominis plane block. Anesth Analg. 2007;105:883. doi: 10.1213/01.ane.0000268542.45107.79. [DOI] [PubMed] [Google Scholar]


