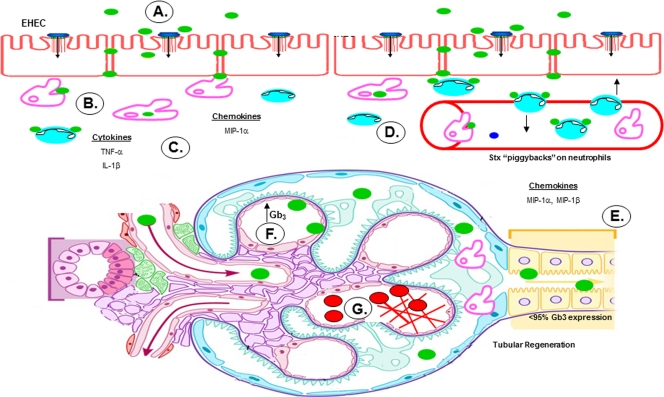
Fig. 9.
Potential role of human proximal tubule epithelial cells in the pathogenesis of hemolytic uremic syndrome. (A) STEC adheres to the colonic epithelium. (B) The bacteria produce and release Stxs (green), which may gain access to the submucosa via transcytotic or paracellular mechanisms. (C) Stxs are internalized by resident tissue macrophages, inducing the production and secretion of proinflammatory cytokines and chemokines. Simultaneously, Stxs bind to and “piggyback” on neutrophils through circulation. (D) TNF-α and IL-1β upregulate expression of the Stx receptor on endothelial cells, resulting in increased vascular damage and systemic transport of Stxs in the blood. (E) Once in circulation, Stxs target the renal epithelium, which is rich in membrane-bound Gb3. Renal proximal tubular epithelial cells are damaged, but a subpopulation of cells survive and, in response to Stx2, secrete both MIP-1α and MIP-1β, which in turn recruit inflammatory cells, such as macrophages and neutrophils, to sites of damage. (F) Activated macrophages secrete TNF-α and IL-1β, further sensitizing the microvascular endothelial cells. (G) Fibrin deposits build up in the microvasculature of the kidney, trapping circulating red blood cells and platelets. (Figure adapted from Medical Illustrations, Michal Komorniczak, with permission.)