Abstract
Objective
To compare the impact of three strategies for delivering a booster dose of adult-formulated tetanus–diphtheria–pertussis (Tdap) vaccine to adolescents in Australia. These comprise: (i) administering Tdap to: a one-year age cohort; (ii) administering Tdap to the entire high school and to subsequent entrant cohorts; and (iii) administering Tdap to the entire high school but without continuing to immunize entrant cohorts.
Methods
A series of ecologic analyses of pertussis notifications during epidemic periods in relevant age cohorts were conducted. The primary outcome measure was the incidence rate ratio (IRR), calculated by dividing pertussis incidence after the introduction of Tdap delivery programmes by pertussis incidence during the most recent pre-programme epidemic.
Findings
During the epidemic period of 2008–2009, the national-level IRR among age cohorts targeted for Tdap was 0.6 (95% confidence interval, CI: 0.6–0.7), but among other age cohorts it was 1.1 (95% CI: 1.1–1.2). Only the jurisdiction that implemented strategy 2 (Western Australia) experienced sustained decreases in pertussis notifications in both adolescents and infants under 6 months of age (IRR: 0.4; 95% CI: 0.3–0.6) until 2009.
Conclusion
If confirmed by longer experience in Australia and elsewhere, a broad school-based catch-up programme followed by immunization of school entrants may be the optimum strategy for the implementation of adolescent Tdap programmes.
ملخص
الغرض
المقارنة بين تأثير ثلاث استراتيجيات لإعطاء جرعة مُعزِّزة من اللقاح المُعدّ لليافعين ضد الكزاز-الخناق-السعال الديكي (Tdap) في أستراليا. وهذا يشمل: 1) إعطاء اللقاح لأتراب يبلغ عمرهم سنة واحدة؛ 2) إعطاء اللقاح لكل طلبة المدارس العليا ويلي ذلك تحصين المجموعات الأترابية الفرعية من الطلبة الجدد 3) إعطاء اللقاح لكل طلبة المدارس العليا ولكن بدون تمنيع الفئات الأترابية الفرعية من الطلبة الجدد.
الطريقة
أجريت سلسلة من التحليلات الإيكولوجية للتبليغ عن السعال الديكي أثناء فترات الوباء في فئة الأتراب العمرية ذات العلاقة. وكانت نتيجة القياس الأولى هي نسبة معدل الوقوع، والتي حسبت عن طريق قسمة معدل وقوع السعال الديكي بعد إدخال برامج إعطاء اللقاح على معدل وقوع السعال الديكي أثناء آخر وباء سابق للبرنامج.
النتائج
أثناء فترة الوباء في 2008-2009، كان المستوى الوطني لنسبة معدل الوقوع بين الأتراب في الفئة العمرية المستهدفة باللقاح 0.6 (فاصلة الثقة 95%: 0.6-0.7)، ولكن كانت بين الفئات الأترابية العمرية الأخرى 1.1 (فاصلة الثقة 95%: 1.1-1.2). وقد شهدت فقط منطقة تطبيق الاستراتيجية الثانية (في غرب أستراليا) انخفاضاً مستمراً في التبليغ عن السعال الديكي بين كل من اليافعين والرضع تحت عمر 6 أشهر (نسبة معدل الوقوع: 0.4؛ فاصلة الثقة 95%: 0.3-0.6) حتى عام 2009.
الاستنتاج
إذا تأكد حدوث ذلك بعد تجربة طويلة الأمد في أستراليا ومناطق أخرى، فإن البرنامج الواسع النطاق المرتكز على المدارس والذي يليه تحصين الطلبة الجدد في المدارس يمكن أن يكون هو أفضل استراتيجية لتنفيذ برامج تحصين اليافعين ضد الكزاز-الخناق-السعال الديكي.
Resumen
Objetivo
evaluar el desempeño de un estudio en centros de atención al paciente recientemente desarrollado para la detección de anticuerpos IgM específicos del sarampión en muestras en suero y secreciones orales y evaluar si el ácido nucleico del virus del sarampión puede recuperarse de las tiras usadas en los estudios en centros de atención al paciente.
Métodos
el estudio en centros de atención al paciente se utilizó para evaluar 170 muestras de suero recolectadas a través de programas de control o vacunación contra el sarampión en Etiopía, Malasia y la Federación de Rusia. Se obtuvieron 69 resultados positivos para anticuerpos de inmunoglobulina M (IgM) del sarampión, 74 resultados positivos para anticuerpos de IgM de rubéola y 7 resultados positivos para ambos. También se evaluaron 282 muestras de secreciones orales del programa de control del sarampión, paperas y rubéola del Reino Unido de Gran Bretaña e Irlanda del Norte. El inmunoensayo de enzimas IgM del sarampión microinmune fue el estándar de oro para la comparación. Se utilizó un panel de 24 secreciones orales para investigar si la hemaglutinina (H) del virus del sarampión y los genes nucleocápsides (N) podrían amplificarse por la reacción en cadena de polimerasa directamente de las tiras del estudio en centros de atención al paciente.
Resultados
Con el suero, el estudio en centros de atención al paciente mostró una sensibilidad y especificidad del 90,8% (69/76) y 93,6% (88/94), respectivamente; con las secreciones orales, la sensibilidad y especificidad fueron del 90,0% (63/70) y 96,2% (200/208), respectivamente. Tanto los genes H como N fueron confiablemente detectados en las tiras del estudio en centros de atención al paciente y los genes N se pudieron secuenciar por genotipo. Los genes del virus del sarampión se recuperaron de las tiras del estudio en centros de atención al paciente después de estar almacenados durante 5 semanas a 20-25 °C.
Conclusión
El estudio en centros de atención al paciente tiene la sensibilidad y especificidad requeridas para un estudio de campo para el diagnóstico del sarampión. No obstante, su papel en los programas de control de sarampión a nivel global requiere una mayor evaluación.
Résumé
Objectif
Comparer l’impact de trois stratégies d’injection de rappel du vaccin tétanos-diphtérie-coqueluche (Tdap) formulé pour adulte chez des adolescents en Australie. Elles comprennent: (1) l’administration du Tdap à: une cohorte âgée d’un an; (2) l’administration du Tdap à tout le lycée et aux cohortes des nouveaux venus; (3) l’administration du Tdap à toute l’école, mais sans continuer à vacciner les cohortes des nouveaux venus.
Méthodes
On a réalisé une série d’analyses écologiques des notifications de la coqueluche lors des périodes d’épidémie dans les cohortes d’âges applicables. La principale mesure des résultats a été le rapport du taux d’incidence (RTI), calculé en divisant l’incidence de la coqueluche après l’introduction des programmes de vaccination du Tdap par l’incidence de la coqueluche lors de l‘épidémie du préprogramme le plus récent.
Résultats
Lors de la période épidémique de 2008–2009, le RTI au niveau national chez les cohortes d’âges ciblées pour le Tdap était de 0,6 (intervalle de confiance de 95% IC: 0,6–0,7), mais chez les autres cohortes d’âges, il était de 1,1 (IC de 95%: 1,1–1,2). Seule la juridiction qui avait mis en place la stratégie 2 (Australie occidentale) a enregistré des baisses soutenues dans les notifications de la coqueluche chez les adolescents et les enfants de moins de 6 mois (RTI: 0,4; IC de 95%: 0,3–0,6) jusqu’en 2009.
Conclusion
S’il est confirmé par une plus longue expérience en Australie et partout dans le monde, un large programme de rattrapage au sein des écoles, suivi de la vaccination des nouveaux venus, pourrait être la stratégie optimale pour mettre en place les programmes de Tdap chez les adolescents.
Резюме
Цель
Сравнить воздействие трех стратегий назначения бустерной дозы взрослой коклюшно-дифтерийно-столбнячной вакцины (Tdap) австралийским подросткам. Эти стратегии включали в себя: (1) введение Tdap когорте детей в возрасте одного года; (2) введение Tdap всем учащимся средней школы и далее когортам вновь поступающих учеников; (3) введение Tdap всем учащимся средней школы без продолжения иммунизации когорт вновь поступающих учеников.
Методы
Была проведена серия аналитических экологических исследований уведомлений о случаях заболевания коклюшем в периоды эпидемий в соответствующих возрастных когортах. Показателем первичного исхода был коэффициент заболеваемости (КЗ), рассчитываемый путем деления показателя заболеваемости коклюшем после внедрения программы назначения вакцины Tdap на показатель заболеваемости коклюшем во время эпидемии, непосредственно предшествующей внедрению программы.
Результаты
В период эпидемии 2008–2009 года общенациональный КЗ в возрастных когортах, которым адресно вводилась вакцина Tdap, был равен 0,6 (95% доверительный интервал, ДИ: 0,6-0,7), а в других возрастных когортах составлял 1,1 (95% ДИ: 1,1–1,2). Устойчивое снижение числа уведомлений о случаях заболевания коклюшем, как среди подростков, так и среди детей в возрасте до шести месяцев, в период вплоть до 2009 года наблюдалось только в регионе, где внедрялась стратегия 2 (Западная Австралия) (КЗ: 0,4; 95% ДИ: 0,3–0,6).
Вывод
Если судить по долгосрочному опыту Австралии и других стран, то масштабная программа «наверстывающей» вакцинации на базе школы с последующей иммунизацией вновь поступающих учащихся может быть оптимальной стратегией внедрения программ иммунизации подростков вакциной Tdap.
摘要
目的
旨在比较运用三种策略为澳大利亚青少年接种成人配方破伤风白喉百日咳(Tdap)混合疫苗加强剂量的影响。此三种策略包括:(1)为一岁年龄组接种破伤风白喉百日咳混合疫苗;(2)为所有中学生以及随后的入学群体接种破伤风白喉百日咳混合疫苗;(3)为所有中学生接种破伤风白喉百日咳混合疫苗但是不继续为入学群体进行免疫接种。
方法
文章对相关年龄组流行阶段的百日咳呈报案例进行了系列生态学分析。主要结果测量指标是发病率比(IRR),用引入破伤风白喉百日咳混合疫苗接种计划之后的百日咳发病率除以接种计划前最近流行阶段的百日咳发病率计算得到。
结果
2008-2009年的流行阶段中,破伤风白喉百日咳混合疫苗的目标年龄组中国家级发病率比为0.6 (95%可信区间,CI:0.6-0.7),而其他年龄组的发病率比为1.1(95%可信区间,CI:1.1-1.2)。截至2009年,仅实施策略2(澳大利亚西部)的辖区经历了青少年和6个月以下婴儿百日咳呈报案例(发病率比:0.4; 95%可信区间,CI:0.3-0.6)的持续减少。
结论
如果可以肯定澳大利亚以及其他地方的长期经验,则新生入学免疫接种之后基于学校的大范围追赶计划可能是青少年破伤风白喉百日咳混合疫苗计划实施的最佳策略。
Introduction
Australia has seen large numbers of pertussis notifications in adolescents and adults over the past 10 to 15 years, as have some North American and European countries with long-standing high coverage for diphtheria–tetanus–pertussis (DTP) vaccines in childhood immunization programmes.1–3 DTP vaccines have been in general use in Australia since the 1950s,4–6 but because of concern about the possible adverse effects of the whole-cell pertussis component,7 during the 1970s and 1980s DTP vaccine was frequently substituted with diphtheria–tetanus (DT) vaccine, and this led to a partially immunized cohort.8 Members of this cohort, which was also the last to not be eligible to receive the pre-school DTP booster added to the immunization schedule in 1994,9 figured prominently in successive epidemics between 1993 and 2002. A similar cohort effect has been observed in Canada.3 School outbreaks were also frequent at this time.10 Acellular vaccines replaced the Australian-manufactured whole-cell vaccine for booster doses in 1997 and for all doses in 1999, and 95% coverage with three doses of this new vaccine (at 2, 4 and 6 months) by 2 years of age was attained within 4 years.11
The availability of a well formulated triple vaccine with an acellular pertussis component (Boostrix [Tdap], GlaxoSmithKline, Brentford, England) and the recognition that pertussis incidence in adolescents was increasing prompted the National Immunisation Programme to begin using Tdap on 1 January 2004 instead of the reduced antigen diphtheria–tetanus (Td) booster dose previously recommended at age 15 to 17 years.12 Delivery of Tdap vaccine was primarily school-based, with limited doses also available in primary care.
Although several countries, including Canada, France, Germany and the United States of America, have added an adolescent booster dose to their list of recommended immunizations, reports of the impact of adolescent pertussis vaccine programmes has been limited to early and/or regional data.13–17 The aim of this study was to compare the long-term impact of the approaches used in Australia – vaccinating a one-year age cohort versus the entire high school, with and without continued immunization of high school entrants – in the context of known historical differences in pertussis epidemic cycles by region.6 Our findings have implications for countries considering the introduction of Tdap boosters for children and adolescents 10 to 18 years of age.
Methods
We conducted a series of ecologic analyses of trends in pertussis notifications by age group, using relative incidence by time period, epidemic cycle and estimated vaccine coverage, to compare notification rates in relevant age cohorts. Data sources and methods of estimation for these analyses are described in the following sections.
Vaccine coverage
Immunization programme managers from each Australian state and territory provided coverage data from school-based delivery programmes for the period between January 2004 and December 2009. No data were available on vaccines administered outside the school setting, but these were thought to represent a small proportion of the doses administered.
Pertussis notification before and after Tdap
Notifications to the National Notifiable Diseases Surveillance System with an onset date between 1 January 1999 and 31 December 2009 were eligible for this analysis. Pertussis cases are notifiable in every Australian jurisdiction under public health legislation. The criteria for notification are nationally uniform and include a combination of clinical, epidemiological and laboratory evidence. Laboratory evidence rests on culture of Bordetella pertussis or on the detection of B. pertussis by nucleic acid testing or single point serology. Since 1993, all public and private laboratories have been required to notify all persons testing positive on diagnostic tests for pertussis to public health authorities. Cases can be notified on clinical grounds alone if they report having had a coughing illness lasting 2 or more weeks and paroxysms of coughing, inspiratory whoop or post-tussive vomiting.18 However, over the past decade cases without laboratory evidence have become increasingly rare. We calculated notification rates for each age group and time period using average annual Australian Bureau of Statistics population estimates.19 We used the ratio of notification rates between epidemiologically relevant time periods (incidence rate ratios, IRRs) as the measure for comparison of programme impact, and we calculated their 95% confidence intervals (CIs) using a Poisson distribution.
With respect to programme delivery comparisons, we calculated incidence rate ratios (IRRs) using regional groupings based on differing programme delivery characteristics (Table 1). Three regions (Australian Capital Territory, South Australia and Victoria) applied strategy 1 – delivery of the Tdap vaccine to a single school grade each year – and formed a single programme grouping. The states of New South Wales and Western Australia delivered the vaccine to grades 7 up to 12 (ages 12–19 years) in 2004, in the context of high pertussis notifications in adolescents in both regions. In New South Wales, this was followed by immunization of grade 7 students in 2005 and cessation of the programme for the following three years, before planned re-commencement of Tdap vaccine delivery to grade 10 students (strategy 2). In Western Australia, grade 7 students were immunized every year (strategy 3). In the state of Queensland there was little provision of free Tdap vaccine by private sector providers after 2003, but state-wide school-based immunization programmes targeting grade 10 students did not commence until 2007.
Table 1. Coverage with diphtheria, tetanus and acellular pertussis vaccine (Tdap) in students aged 12 to 19 years, by grade, year and jurisdiction, Australia, 2004–2009.
| Jurisdiction (2009 population 12–19 years old) | 2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gradea | Coverage (%) | Gradea | Coverage (%) | Gradea | Coverage (%) | Gradea | Coverage (%) | Gradea | Coverage (%) | Gradea | Coverage (%) | ||||||
| Australian Capital Territory (38 391) | 9 | 78 | 9 | 83 | 9 | 81 | 9 | 80 | 9 | 82 | 9 | 81 | |||||
| New South Walesb (753 430) | 7 | 64 | 7 | 72 | – | – | – | – | – | – | 10 | 68 | |||||
| 8 | 64 | ||||||||||||||||
| 9 | 62 | ||||||||||||||||
| 10 | 56 | ||||||||||||||||
| 11 | 41 | ||||||||||||||||
| 12 | 41 | ||||||||||||||||
| Av. 7–10 | 62 | ||||||||||||||||
| Av. 11–12 | 41 | ||||||||||||||||
| Queenslandc (489 248) | – | – | – | – | – | – | 10 | 62 | 10 | 63 | 10 | 62 | |||||
| South Australiad (164 705) | 8 | 80 | 8 | 85 | 8 | 81 | – | – | 9 | 74 | 9 | 78 | |||||
| Victoria (527 784) | 10 | 74 | 10 | 74 | 10 | 74 | 10 | 74 | 10 | 76 | 10 | 74 | |||||
| Western Australia (244 963) | 7 | 70 | 7 | 77 | 7 | 69 | 7 | 78 | 7 | 76 | 7 | 81 | |||||
| 8 | 50 | ||||||||||||||||
| 9 | 44 | ||||||||||||||||
| 10 | 37 | ||||||||||||||||
| 11 | 24 | ||||||||||||||||
| 12 | 4 | ||||||||||||||||
| Av. 7–10 | 50 | ||||||||||||||||
| Av. 11–12 | 14 | ||||||||||||||||
Av., average.
a Ages are as follows: grade 7, 12–13 years; grade 8, 13–14 years; grade 9, 14–15 years; grade 10, 15–16 years; grade 11, 16–17 years; grade 12, 17–19 years.
b No programme in 2006–2008.
c No programme until 2007.
d No programme in 2007.
To account for the variability of programme delivery and vaccine coverage by age cohort and time period, we defined immunized and unimmunized cohorts among students aged 12–19 years in each regional grouping above. As data on vaccination coverage were available by grade but not at the individual level, each grade was defined as vaccinated if the estimated Tdap vaccination coverage was 50% or higher. Grades not exposed to a school-based vaccination programme or where estimated vaccination coverage was less than 50% were considered unvaccinated. Data for Queensland for the years before commencement of a state-wide school-based programme were not included. As notification data were available by year of age, the single largest age group in each school grade (e.g. grade 7, 12 years; grade 8, 13 years; grade 9, 14 years, etc.) was used to generate an approximate incidence rate for each age group, defined as immunized or unimmunized as above, for calculation of the IRR (Table 2).
Table 2. Proportion of students considered immunized during two epidemic periods after diphtheria, tetanus and acellular pertussis vaccine programme roll-out, by age and jurisdictional grouping, Australia, 2005–2009.
| Jurisdictional groupinga | Percentage immunized |
||||
|---|---|---|---|---|---|
| 2005–2007 |
2008–2009 |
||||
| < 16 years | ≥ 16 years | < 16 years | ≥ 16 years | ||
| Australian Capital Territory/ South Australia/Victoria | 34 | 49 | 32 | 91 | |
| New South Wales | 75 | 51 | 25 | 100 | |
| Western Australia | 92 | 9 | 100 | 62 | |
| Queensland | 9 | 0 | 25 | 38 | |
a Jurisdictional groupings were based on programme delivery characteristics.
Results
Vaccination coverage
Overall, an estimated 1 066 000 of an estimated 1 650 000 eligible students aged 12 to 19 years (65%) received Tdap vaccine in school-based immunization programmes between January 2004 and December 2009. Annual coverage estimates were in the range of 55 to 76%, with coverage in subgroups of school grade and region varying from a low of 4% to a high of 85% (Table 1). However, estimated coverage within regions remained the same from year to year. In New South Wales and Western Australia, where the entire high school population was vaccinated within a single calendar year, higher coverage was obtained among younger students in the lower high school grades.
Pertussis notification before and after Tdap
By age group
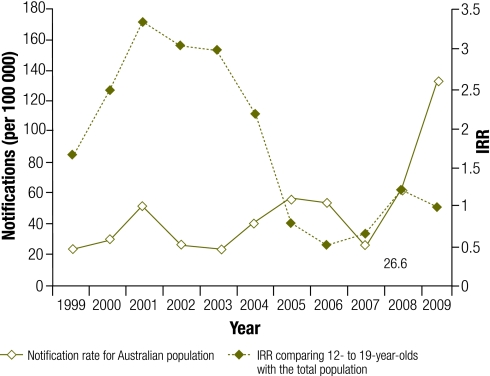
Between 1 January 1999 and 31 December 2009, 110 602 cases of pertussis were notified nationally. Averaged data shows that national epidemics occurred in 2001, 2005–2006 and 2008–2009, but the exact timing differed in each region.6 Fig. 1 shows pertussis notification rates per 100 000 population over the 10-year period from 1999 to 2009, as well as IRRs for the 12–19 age group in comparison to the remainder of the population. At the national level, 2001 was the year with the highest annual notification rate recorded for adolescents aged 12–19 years (127.7 cases per 100 000 population). This decreased significantly to 31.1 cases per 100 000 population in the period from 2005 to 2007. Notification rates in the 12–19 year age group remained significantly lower during the most recent epidemic (2008–2009) than during the 2001 epidemic, as shown by the 95% CIs for point estimates. This stood in contrast to the significant increases noted in all other age groups relative to 2001.
Fig. 1.
Australian pertussis notification rates and incidence rate ratios (IRRs) comparing the 12–19 year age group with the remainder of the population, Australia, 1999–2009
By period and programme delivery groupings
Table 3 shows the IRRs for regional groupings with varying programme delivery methods. In New South Wales, where the programme targeting the entire high school population achieved high coverage but was discontinued for three years, notification rates declined sharply at first but rose substantially in the 2008–2009 epidemic period. In Western Australia, where students entering high school continued to be vaccinated year after year after the entire high school population was vaccinated, notification rates also decreased rapidly but remained low to the end of 2009.
Table 3. Incidence rate ratios (IRRs)a for pertussis notifications in adolescents aged 12 to 19 years for each year after diphtheria, tetanus and acellular pertussis vaccine programme roll-out, by jurisdictional group, Australia, 2004–2009.
| Jurisdictional groupingb | Pre-programme epidemic ratec,d (95% CI) |
IRR (95% CI) |
|||||
|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | |||
| Australian Capital Territory/ South Australia/Victoria | 92.6 (87.4–98.0) | 0.41 (0.36–0.47) | 0.26 (0.23–0.31) | 0.20 (0.17–0.24) | 0.39 (0.34–0.35) | 1.03 (0.93–1.13) | |
| New South Wales | 156.8 (150.4–163.4) | 0.29 (0.25–0.32) | 0.20 (0.17–0.22) | 0.13 (0.11–0.15) | 1.22 (1.14–1.30) | 1.23 (1.15–1.31) | |
| Western Australia | 284.2 (263.2–306.9) | 0.08 (0.06–0.11) | 0.03 (0.02–0.05) | 0.01 (0.01–0.03) | 0.03 (0.02–0.05) | 0.05 (0.04–0.08) | |
| Queensland | 134.7 (127.1–142.8) | 0.57 (0.50–0.64) | 0.36 (0.31–0.42) | 0.18 (0.15–0.22) | 0.29 (0.25–0.34) | 0.95 (0.86–1.05 | |
CI, confidence interval.
a These represent the ratios given by dividing the notification rate during each of the two epidemic periods after diphtheria, tetanus and acellular pertussis vaccine programme roll-out by the notification rate during the most recent epidemic period before programme roll-out.
b Jurisdictional groupings were based on programme delivery characteristics.
c The recent epidemic periods used in the analysis were as follows: Australian Capital Territory, 2003; South Australia, 2001; Victoria, 2001/2002; New South Wales, 2000/2001; Queensland, 2001/2002; Western Australia, 2004; national, 2001.6
d Per 100 000 population.
By cohort immunization status
Given the wide variation in programme roll-out by age group and timing of epidemic peaks in notifications across regions, we used notification rates in immunized and unimmunized age groups, as defined in the methods section, to generate IRRs for each region. Table 4 shows IRRs for both immunized and unimmunized cohorts during the most recent epidemic period (2008–2009) and during the period immediately following programme implementation (2005–2007). In the period 2005–2007 immediately following programme implementation, notification rates were significantly lower in immunized cohorts than in unimmunized cohorts in most programme delivery jurisdictional groupings, and the rates in both cohorts were lower than the rates recorded in the most recent pre-programme epidemic year. The only exception was the state of Queensland, where the Tdap programme was not implemented until 2007.
Table 4. Incidence rate ratios (IRRs)a for pertussis notifications in adolescents aged 12 to 19 years categorized as immunized or unimmunized by birth cohort, by epidemic periodb and jurisdictional group, Australia, 2004–2009.
| Jurisdictional groupingc | Pre-programme epidemic rated (95% CI) | IRR (95% CI) |
||||
|---|---|---|---|---|---|---|
| 2005–2007e |
2008–2009f |
|||||
| Immunizedd | Unimmunized | Immunizedd | Unimmunized | |||
| Australian Capital Territory/ South Australia/Victoria | 92.6 (87.4–98.0) | 0.23 (0.19–0.27) | 0.33 (0.29–0.37) | 0.54 (0.48–0.60) | 1.00 (0.90–1.11) | |
| New South Wales | 156.8 (150.4–163.4) | 0.17 (0.15–0.19) | 0.26 (0.23–0.29) | 0.87 (0.81–0.93) | 1.85 (1.73–1.97) | |
| Western Australia | 284.2 (263.2–306.9) | 0.02 (0.02–0.04) | 0.06 (0.05–0.08) | 0.04 (0.03–0.06) | 0.04 (0.02–0.07) | |
| Queensland | 134.7 (127.1–142.8) | 0.25 (0.15–0.39) | 0.18 (0.14–0.22) | 0.59 (0.51–0.67) | 0.64 (0.58–0.71) | |
| National | 127.7 (123.0–132.6) | 0.17 (0.16–0.19) | 0.24 (0.22–0.26) | 0.62 (0.59–0.66) | 1.11 (1.06–1.17) | |
CI, confidence interval.
a These represent the ratios given by dividing the notification rate during each of the two epidemic periods after diphtheria, tetanus and acellular pertussis vaccine programme roll-out by the notification rate during the most recent epidemic period before programme roll-out.
b The recent epidemic periods used in the analysis were as follows: Australian Capital Territory, 2003; South Australia, 2001; Victoria, 2001/2002; New South Wales, 2000/2001; Queensland, 2001/2002; Western Australia, 2004; national, 2001.6
c Jurisdictional groupings were based on programme delivery characteristics.
d Per 100 000 population.
e For the period 2005–2007, data were limited to 2007 for Queensland.
f The single largest age group comprising each school grade was used to generate an approximate incidence among age groups, defined as immunized and unimmunized, with each grade defined as immunized if Tdap coverage was 50% or above.
Based on overall notification rates, pertussis epidemics commenced during 2008–2009 in all regions, except in Western Australia. In all programme delivery groups the IRR in immunized age cohorts was again lower than in unimmunized cohorts. In the jurisdictional grouping where the programme was implemented in a single grade, the IRR during the 2008–2009 epidemic period rose but was not significantly higher than during the comparator pre-programme epidemic period. By contrast, in New South Wales, where the entire high school population was vaccinated within a one-year period but high school entrants were not for the following three years, a significantly higher IRR was seen in the unimmunized cohort (Table 4). In the immunized cohort the overall IRR was 0.87, in grade 10 students immunized during the epidemic the IRR was 1.60 (95% CI: 1.4–1.8) as opposed to 0.69 (95% CI: 0.6–0.8) in students immunized in 2004 and 2005. In Western Australia, where vaccination of the entire high school population was followed by immunization of each successive entrant cohort, no epidemic occurred in any age group in 2008–2009. Notably, the IRRs in immunized and unimmunized cohorts were similar, as in 2005–2007, and both were substantially lower than in the comparator epidemic period. In Queensland, incidence did not differ among immunized and unimmunized cohorts but was significantly lower in both groups after the Tdap vaccination programme was implemented.
Notification trends in young infants
The same regional programme delivery groupings were used to compare trends over time in pertussis notification rates among infants less than 6 months of age (Table 5). In 2005–2007, rates dropped significantly (by 20–60%) in all groupings relative to the most recent pre-programme epidemic period. During the 2008–2009 epidemic, notification rates among infants less than 6 months of age returned to levels similar to those observed in the reference epidemic period with two exceptions. In New South Wales, notification rates in 2008–2009 were significantly higher, more than double what they were during the reference epidemic period, while in Western Australia notification rates were significantly lower, at around 40% of the rates reported in the most recent pre-programme epidemic.
Table 5. Incidence rate ratios (IRR)a for pertussis notifications in infants aged less than 6 months during epidemic periods,b by jurisdictional group, Australia, 2004–2009.
| Jurisdictional groupingc | Pre-programme epidemic rated (95% CI) | IRR (95% CI) |
|
|---|---|---|---|
| 2005–2007 | 2008–2009 | ||
| Australian Capital Territory/ South Australia/Victoria | 216.8 (185.1–253.9) | 0.20 (0.15–0.28) | 1.25 (1.02–1.53) |
| New South Wales | 268.4 (236.0–305.1) | 0.60 (0.50–0.73) | 2.82 (2.42–3.28) |
| Western Australia | 536.8 (421.8–683.3) | 0.18 (0.12–0.27) | 0.40 (0.28–0.57) |
| Queensland | 255.1 (214.1–304.0) | 0.37 (0.28–0.50) | 1.07 (0.85–1.36) |
| National | 251.4 (225.1–280.6) | 0.39 (0.33–0.45) | 1.62 (1.43–1.84) |
CI, confidence interval.
a These represent the ratios given by dividing the notification rate during each of the two epidemic periods after diphtheria, tetanus and acellular pertussis vaccine programme roll-out by the notification rate during the most recent epidemic period before programme roll-out.
b The recent epidemic periods used in the analysis were as follows: Australian Capital Territory, 2003; South Australia, 2001; Victoria, 2001/2002; New South Wales, 2000/2001; Queensland, 2001/2002; Western Australia, 2004; national, 2001.6
c Jurisdictional groupings were based on programme delivery characteristics.
d Per 100 000 population.
Discussion
In 2002, the Global Pertussis Initiative recommended that countries expand existing vaccination strategies to include a pertussis booster dose for adolescents.20 A recent meeting of the WHO Strategic Advisory Group of Experts on Immunization (SAGE) noted that supporting data on cost-effectiveness for programmes targeting adolescents were lacking and that data on impact on infant disease were particularly relevant.21 Countries that have added an adolescent booster dose to their schedules since the 2002 recommendation include Canada, France, Germany, New Zealand and the United States.22 Timing of programme commencement has varied widely and data on disease reduction in the targeted age group are lacking. In this national evaluation, we have taken account of variations in vaccine delivery, programme implementation and pertussis epidemic cycles by region6 to estimate the impact of the programme on pertussis in the targeted age group. This study is the first to specifically evaluate impact in young infants.
With respect to vaccine coverage, individual level data were not available, as the Australian Childhood Immunisation Register only records vaccinations given up to the age of 7 years. We therefore relied on estimates of coverage derived from the school-based programme and on data supplied by each state and territory in varying detail and format. Overall, approximately 65% of the targeted age group was vaccinated up to the end of 2009, but coverage varied from 4% to 85% by age group and region. These are minimum estimates of population coverage, as no data were available for doses administered in the private sector. However, confidence in our estimates of 50–80% is supported by their consistency with estimates from a similar Australian school-based meningococcal C conjugate vaccine catch-up programme in 2003,23 and with those from Canadian provinces immunizing school years 9 and 10 (14- to 16-year-olds).13,15 In the United States, Tdap was recommended for use in adolescents in 2006 but is not delivered through a school-based programme. Coverage estimates rose from 11% in 2006 to 30% in 2007, but, as in our data, they were significantly higher among adolescents aged 13–14 years than among those aged 15–17 years.24,25 Similarly, lower coverage in older high school students was observed in the Australian meningococcal C conjugate vaccine catch-up programme.23 This is probably because of more frequent absences from school among older students and lower school retention rates (81% for grades 10–12)26 and is likely to be applicable in comparable developed country settings.
The use of pertussis notification data to measure impact from an adolescent Tdap programme is confounded by interannual and epidemic variations in pertussis activity, which we took into account in our analysis, as well as by changes in diagnostic practice. The impact of testing practices is substantial, as laboratories in Australia are mandated to notify positive results on pertussis diagnostic tests, whereas clinicians are known to be much less reliable notifiers, whether or not there is laboratory confirmation. Between 2001 and 2009, the proportion of notifications recorded in the NNDSS as confirmed by any laboratory method increased from 55% to 90%. This increase was largely driven by positives detected with polymerase chain reaction (PCR), since PCR had become increasingly available through community laboratories since 2007. The increase in PCR use among adolescents was greater in New South Wales than in other jurisdictions. This may have led to amplified increases in notification rates in this age group in that jurisdiction during 2008–2009 but should have had minimal impact on notifications in infants among whom PCR has been predominantly used as a diagnostic test since 2001.
Despite the limitations of the available data, the range of analytic methods that we used – from aggregated age groups to smaller age subgroups and to regional groupings with differing vaccine coverage over time – showed consistent evidence of an impact. The relatively low notification rate in 12–19 year olds seen in 2004 was maintained until the 2008–2009 epidemic and the rate remained lower than during historical peaks. This was in marked contrast to what we observed in other age groups. When the data were further refined to consider immunized cohorts specifically, this trend is more clearly evident and is consistent with the early vaccine effectiveness estimates of 78–85% for Tdap obtained in New South Wales in 2004.16 We were unable to estimate vaccine effectiveness in the current study because individual level data on vaccination status is lacking.
In Western Australia, the notification rate in the unimmunized cohort was nearly identical to the rate in the immunized cohort in 2008–2009. While disease activity in all age groups in Western Australia was low in 2008, this finding is consistent with herd immunity among the unimmunized adolescent cohort. The increased IRR in the immunized and unimmunized cohorts in New South Wales may be the result of waning immunity, as most of the immunized cohort had not been vaccinated since 2004 or 2005. However, more detailed analysis showed that grade 10 students, who were being vaccinated during the epidemic, had a higher IRR than the rest of the immunized cohort.
A key question is whether adolescent pertussis immunization programmes have any impact on pertussis transmission among young, unimmunized infants. In our data, there was a decrease in the notification rate among infants younger than 6 months of age following the initiation of adolescent pertussis immunization in the National Immunization Programme in 2004, but this was also seen in other age groups during the inter-epidemic period and was sustained until 2008–2009 only in Western Australia. Although this finding could be explained by more dispersed epidemic cycles in Western Australia,6 pertussis notification rates in that state did increase in 2010 (data not shown) and were high in children aged 5–9 and 10–14 years; only 40% of the children aged 10–14 years were eligible for Tdap. In contrast, in 2010 notifications remained low in Western Australia among 15- to 19-year-olds (all eligible for Tdap) and the IRR for infants aged 0 to 6 months was not appreciably different in 2010 than in 2009 (0.46 [95% CI: 0.30–0.69] versus 0.40 [95% CI: 0.28–0.57], respectively, Table 5), maintaining the differential with other jurisdictions.27
Although limited by its ecologic design, our analysis provides some evidence that a pertussis vaccination catch-up component has an impact on herd immunity and on the incidence of disease among infants. Catch-up programmes can rapidly reduce pertussis incidence across a broad range of ages and ongoing immunization of children entering adolescence may be important for maintaining this in the long term. The consistently higher notification rates in younger adolescents also suggest that the programme should target younger age groups. Targeting a programme to younger people will have follow-up implications for countries considering cocooning recommendations for new parents, which must factor in the waning of antibody levels between adolescence and pregnancy. The most recent data suggest that antibody levels have dropped substantially by the tenth year after immunization.28
In conclusion, data from Australia demonstrate that school-based adolescent pertussis vaccination programmes can achieve high coverage relatively rapidly and have a demonstrable impact on the incidence of pertussis, as measured by case notifications. Our experience suggests that, in the context of school-based delivery, implementing a broadly based vaccination programme is more beneficial than introducing the vaccine in a single school year, but that it is necessary to immunize children entering high school on an ongoing basis. This is particularly important if it is shown that broad-based catch-up immunization of adolescents effectively decreases the incidence of severe disease in unimmunized infants.
Acknowledgements
We wish to acknowledge the contributions of the state and territory government immunization programme managers and staff. We also wish to acknowledge the contributions of the Communicable Diseases Network Australia.
Funding:
This work was supported by the Australian Government Department of Health and Ageing, the New South Wales Department of Health and The Children’s Hospital at Westmead.
Competing interests:
None declared.
References
- 1.America Academy of Pediatrics Commitee on Infectious Diseases Prevention of pertussis among adolescents: recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine. Pediatrics. 2006;117:965–78. doi: 10.1542/peds.2005-3038. [DOI] [PubMed] [Google Scholar]
- 2.Celentano LP, Massari M, Paramatti D, Salmaso S, Tozzi AE, EUVAC-NET Group Resurgence of pertussis in Europe. Pediatr Infect Dis J. 2005;24:761–5. doi: 10.1097/01.inf.0000177282.53500.77. [DOI] [PubMed] [Google Scholar]
- 3.Ntezayabo B, De Serres G, Duval B. Pertussis resurgence in Canada largely caused by a cohort effect. Pediatr Infect Dis J. 2003;22:22–7. doi: 10.1097/00006454-200301000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Gidding HF, Burgess MA, Kempe AE. A short history of vaccination in Australia. Med J Aust. 2001;174:37–40. doi: 10.5694/j.1326-5377.2001.tb143144.x. [DOI] [PubMed] [Google Scholar]
- 5.Hethcote HW, Horby P, McIntyre P. Using computer simulations to compare pertussis vaccination strategies in Australia. Vaccine. 2004;22:2181–91. doi: 10.1016/j.vaccine.2003.11.053. [DOI] [PubMed] [Google Scholar]
- 6.Quinn HE, McIntyre PB. Pertussis epidemiology in Australia over the decade 1995–2005 – trends by region and age group. Commun Dis Intell. 2007;31:205–15. [PubMed] [Google Scholar]
- 7.MacIntyre CR, Nolan T. Attitudes of Victorian vaccine providers to pertussis vaccine. Med J Aust. 1994;161:293–4. doi: 10.5694/j.1326-5377.1994.tb127448.x. [DOI] [PubMed] [Google Scholar]
- 8.Brotherton J, McAnulty J. A pertussis epidemic in NSW: how epidemiology reflects vaccination policy. N S W Public Health Bull. 2003;14:77–81. doi: 10.1071/NB03024. [DOI] [PubMed] [Google Scholar]
- 9.Torvaldsen S, McIntyre PB. Effect of the preschool pertussis booster on national notifications of disease in Australia. Pediatr Infect Dis J. 2003;22:956–9. doi: 10.1097/01.inf.0000095198.75170.b6. [DOI] [PubMed] [Google Scholar]
- 10.Horby P, Macintyre CR, McIntyre PB, Gilbert GL, Staff M, Hanlon M, et al. A boarding school outbreak of pertussis in adolescents: value of laboratory diagnostic methods. Epidemiol Infect. 2005;133:229–36. doi: 10.1017/S0950268804003401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hull BP, Mahajan D, Dey A, Menzies RI, McIntyre PB. Immunisation coverage annual report, 2008. Commun Dis Intell. 2010;34:241–58. [PubMed] [Google Scholar]
- 12.National Health and Medical Research Council. The Australian immunisation handbook Canberra: Australian Government Department of Health and Ageing; 2003. [Google Scholar]
- 13.David ST, Hemsley C, Pasquali PE, Larke B, Buxton JA, Lior LY. Enhanced surveillance for vaccine-associated adverse events: dTap catch-up of high school students in Yukon. Can Commun Dis Rep. 2005;31:117–26. [PubMed] [Google Scholar]
- 14.Disease Control and Epidemiology Newfoundland & Labrador Department of Health and Community Services Pertussis in Newfoundland and Labrador: 1991–2004. Can Commun Dis Rep. 2005;31:235–7. [PubMed] [Google Scholar]
- 15.Kandola K, Lea A, White W, Santos M. A comparison of pertussis rates in the Northwest Territories: Pre- and postacellular pertussis vaccine introduction in children and adolescents. Can J Infect Dis Med Microbiol. 2005;16:271–4. doi: 10.1155/2005/642315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rank C, Quinn HE, McIntyre PB. Pertussis vaccine effectiveness after mass immunization of high school students in Australia. Pediatr Infect Dis J. 2009;28:152–3. doi: 10.1097/INF.0b013e318185608e. [DOI] [PubMed] [Google Scholar]
- 17.Rendi-Wagner P, Kundi M, Mikolasek A, Vécsei A, Frühwirth M, Kollaritsch H. Hospital-based active surveillance of childhood pertussis in Austria from 1996 to 2003: estimates of incidence and vaccine effectiveness of whole-cell and acellular vaccine. Vaccine. 2006;24:5960–5. doi: 10.1016/j.vaccine.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Interim surveillance case definitions for the Australian National Notifiable Diseases Surveillance System, Version 1. 1 [Internet]. Canberra: Australian Government, Department of Health and Ageing; 2004. Available from: http://www.health.gov.au/internet/main/publishing.nsf/Content/cda-surveil-nndss-casedefs-distype.htm[accessed 17 June 2011].
- 19.Population by age and sex, Australian states and territories [Internet]. Canberra: Australian Bureau of Statistics; 2009. Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/second+level+view?ReadForm&prodno=3201.0&viewtitle=Population%20by%20Age%20and%20Sex [accessed 17 June 2011].
- 20.Forsyth KD, Wirsing von Konig CH, Tan T, Caro J, Plotkin S. Prevention of pertussis: recommendations derived from the second Global Pertussis Initiative roundtable meeting. Vaccine. 2007;25:2634–42. doi: 10.1016/j.vaccine.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization Meeting of the Strategic Advisory Group of Experts on immunization, April 2010 - conclusions and recommendations. Wkly Epidemiol Rec. 2010;85:197–212. [PubMed] [Google Scholar]
- 22.WHO Vaccine Preventable Diseases Monitoring System [Internet]. Geneva: World Health Organization; 2011. Available from: http://apps.who.int/immunization_monitoring/en/globalsummary/DiseaseSelect.cfm?U=years [accessed 17 June 2011].
- 23.Ward KF, Menzies RI, Quinn HE, Campbell-Lloyd S. School-based vaccination in NSW. N S W Public Health Bull. 2010;21:237–42. doi: 10.1071/NB10046. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC) Vaccination coverage among adolescents aged 13–17 years - United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57:1100–3. [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) National, state, and local area vaccination coverage among adolescents aged 13–17 years –United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:997–1001. [PubMed] [Google Scholar]
- 26.4221.0 – Schools, Australia [Internet]. Canberra: Australian Bureau of Statistics; 2010. Available from: http://www.ausstats.abs.gov.au/Ausstats/subscriber.nsf/0/0014934D84F64006CA2578550011905F/$File/nssc%20table%2064a%20apparent%20retention%20rates,%201996_2010.xls [accessed 17 June 2011].
- 27.National communicable diseases surveillance report: fortnight 25, 2010 summary notes for selected diseases, 4 to 17 December 2010 Canberra: Office of Health Protection, Surveillance Branch; 2010. Available from: http://www.health.gov.au/internet/main/publishing.nsf/Content/010561D59E66FCCACA2578020013CB45/$File/nndssreport-fn25-10.pdf [accessed 17 June 2011].
- 28.Mertsola J, Van Der Meeren O, He Q, Linko-Parvinen A, Ramakrishnan G, Mannermaa L, et al. Decennial administration of a reduced antigen content diphtheria and tetanus toxoids and acellular pertussis vaccine in young adults. Clin Infect Dis 201051656–62.[REMOVED HYPERLINK FIELD] 10.1086/655825 [DOI] [PubMed] [Google Scholar]