Abstract
Object
Delayed (24 hours post injury) treatment with erythropoietin (EPO) improves functional recovery following experimental traumatic brain injury (TBI). In this study, we tested whether therapeutic effects of delayed EPO treatment for TBI are dose-dependent in an attempt to establish an optimal dose paradigm for the delayed EPO treatment.
Methods
Experimental TBI was performed in anesthetized young adult male Wistar rats using a controlled cortical impact device. Sham animals underwent the same surgical procedure without injury. The animals (8 rats/group) received 3 intraperitoneal injections of EPO (0, 1000, 3000, 5000 or 7000 U/kg body weight, at 24, 48 and 72 hours) after TBI. Sensorimotor and cognitive functions were assessed using a modified neurological severity score and foot fault test, and Morris water maze tests, respectively. Animals were sacrificed 35 days after injury and brain sections stained for immunohistochemical analyses.
Results
Compared to the saline treatment, EPO treatment at doses from1000 to 7000 U/kg did not alter lesion volume but significantly reduced hippocampal neuron loss, enhanced angiogenesis and neurogenesis in the injured cortex and hippocampus, and significantly improved sensorimotor function and spatial learning. The medium dose at 5000 U/kg exhibited a significant improvement in histological and functional outcomes compared with the lower or higher EPO dose groups.
Conclusions
These data demonstrate that delayed (24 hours post injury) treatment with EPO provides dose-dependent neurorestoration which may contribute to improved functional recovery after TBI, implying that application of an optimal dose of EPO is likely to increase successful preclinical and clinical trials for treatment of TBI.
Keywords: angiogenesis, cell proliferation, erythropoietin, neurogenesis, rat, sensorimotor, spatial learning, traumatic brain injury
Introduction
Traumatic brain injury (TBI) is a leading cause of mortality and morbidity worldwide, particularly among the young. The most prevalent and debilitating features in survivors of TBI are cognitive deficits and motor dysfunctions.14 To date, despite very encouraging preclinical results, almost all phase II/III clinical neuroprotection trials in TBI have failed to improve the outcome of TBI patients.40,44 The disappointing clinical trials may be due to heterogeneity of the population of TBI patients and variability in treatment approaches. Another important aspect is that most strategies to date have used drugs in clinical trials targeting a single pathophysiological mechanism that contributes to early necrotic cell death.48 Targeting multiple injury mechanisms that contribute to the secondary injury cascade may reduce brain injury, facilitate repair and improve functional recovery.
Erythropoietin (EPO) and the EPO receptor (EPOR), essential for erythropoiesis, are also expressed in the neurons, astrocytes, and cerebral endothelial cells.42 EPO is a multifunctional agent with tissue protection exerting antiapoptotic, anti-inflammatory, antioxidative, angiogenic and neurotrophic properties.13,55 EPO shows neuroprotection in animal models of stroke,20,58 spinal cord injury,5,22,24 concussive brain injury,3 kainate-induced seizure activity,3 and autoimmune encephalomyelitis.6,45 EPO has been demonstrated to be safe and beneficial in an earlier small clinical trial of stroke 17 but did not show benefits (but had a higher mortality compared to placebo controls) in a recent large clinical trial of stroke.18 Combination of tissue plasminogen activator (tPA) with EPO may be one of the important factors for this failed clinical trial because a very large number of EPO-treated stroke patients received tPA treatment in this stroke clinical trial and combination of EPO with tPA has been demonstrated to cause detrimental effects in animal models of stroke.28 Low doses of EPO used for clinical trials may also contribute to this failure because much higher EPO doses are required to provide neuroprotection and functional benefits in animal stroke models.23,37,58 In a recent small EPO clinical trial, a single dose of EPO administered within 6 hours after TBI did not show efficacy. 41 In addition, several EPO TBI clinical trials are ongoing (www.clinicaltrials.gov: NCT00987454; NCT00313716; NCT00375869). However, the optimal EPO dose, dosing interval, and number of doses required for reducing brain injury, promoting neurorestoration and improving functional recovery have not been fully investigated in preclinical trials after TBI. Therefore, it is imperative to investigate dose-response effect of EPO treatment on functional and histological outcomes after TBI. Our recent work demonstrates that delayed treatment (24 hours post injury) with EPO provides long-term benefits in rats after TBI 33,36 and after stroke.58 In an attempt to establish an optimal therapeutic dose, using a controlled cortical impact (CCI) TBI rat model, we investigated the effects of the delayed administration of different doses of EPO on lesion volume, cell proliferation, neurogenesis, angiogenesis, and long-term sensorimotor function and spatial learning recovery after TBI in rats.
Materials and Methods
All experimental procedures were approved by the Institutional Animal Care and Use Committee of Henry Ford Health System.
TBI Model
A CCI model of TBI in the rat was utilized for the present study.16,35 Young adult male Wistar rats (313.4 ± 8.9 g) were anesthetized intraperitoneally with chloral hydrate (350 mg/kg body weight). Rectal temperature was maintained at 37°C using a feedback-regulated water-heating pad. A CCI device was used to induce injury. Rats were placed in a stereotactic frame. Two 10-mm-diameter craniotomies were performed adjacent to the central suture, midway between lambda and bregma. The second craniotomy allowed for lateral movement of cortical tissue. The dura mater was kept intact over the cortex. Injury was delivered by impacting the left cortex (ipsilateral cortex) with a pneumatic piston containing a 6-mm-diameter tip at a rate of 4 m/second and 2.5 mm of compression. Velocity was measured with a linear velocity displacement transducer.
Experimental Groups and Treatment
Young adult male Wistar rats were randomly divided into 6 groups (n = 8/group): 1) Sham; 2) TBI/saline group; 3) TBI + EPO1K; 4) TBI + EPO3K; 5) TBI + EPO5K; and 6) TBI + EPO7K. TBI was induced by CCI over the left parietal cortex. Sham rats underwent surgery without injury. EPO at doses of 0 (saline), 1000 (EPO1K), 3000 (EPO3K), 5000 (EPO5K) and 7000 (EPO7K) U/kg body weight (Epoetin alpha, AMGEN, Thousand Oaks, CA) was administered intraperitoneally at 24, 48 and 72 hours after TBI. Animals in the saline-treated group received an equal volume of saline at 24, 48 and 72 hours after TBI. For labeling proliferating cells, 5-bromo-2′-deoxyuridine (BrdU, 100 mg/kg; Sigma) was injected intraperitoneally into rats daily for 10 days, starting 1 day after TBI. Allrats were sacrificed at 35 days after TBI or surgery.
Hematocrit Level
To determine the effects of EPO on HCT, a blood sample (50 μl) was collected via tail vein before injury, on Day 4, and weekly after TBI or sham treatment up to 5 weeks. Hematocrit was measured in micro-HCT capillary tubes (Fisher Scientific) using standard procedures (Readacrit Centrifuge).62
Evaluation of Neurological Outcome
All functional tests were performed by investigators blinded to the treatment status.
Morris Water Maze Test
To detect spatial learning impairments, a recent version of the MWM test was used.11 The procedure was modified from previous versions15,38,39,51 and has been found to be useful for chronic spatial memory assessment in rats and mice with brain injury.11,33 All animals were tested during the last five days (that is, 31–35 days after TBI or surgery) before sacrifice. Data collection was automated by the HVS Image 2020 Plus Tracking System (US HVS Image). If the animal reached the platform within 90 seconds, the percentage of time traveled within the NE (correct) quadrant was calculated relative to the total amount of time spent swimming before reaching the platform and employed for statistical analysis. The advantage of this version of the water maze is that each trial takes on the key characteristics of a probe trial because the platform is not in a fixed location within the target quadrant.46
Footfault Test
To evaluate sensorimotor function, the footfault test was carried out before TBI and at 1, 4, 7, 14, 21, 28 and 35 days after TBI or surgery. The rats were allowed to walk on a grid.64 With each weight-bearing step, a paw might fall or slip between the wires and, if this occurred, it was recorded as a footfault.1,2 A total of 50 steps were recorded for each right forelimb and hindlimb.63
Modified Neurological Severity Score (mNSS) Test
Neurological functional measurement was performed using the mNSS score.8 The test was carried out on all rats preinjury and on Days 1, 4, 7, 14, 21, 28, and 35 after TBI. The mNSS score is a composite of the motor (muscle status, abnormal movement), sensory (visual, tactile and proprioceptive) and reflex tests and has been employed in previous studies.34 This test is suitable for evaluating long-term neurological function after unilateral brain injury.63
Tissue Preparation and Measurement of Lesion Volume
On Day 35 after TBI, rats were anesthetized intraperitoneally with chloral hydrate and were perfused transcardially first with saline solution, followed by 4% paraformaldehyde in 0.1 M PBS (pH 7.4). Their brains were removed and post-fixed in 4% paraformaldehyde for 2 days at room temperature. The brain tissue was cut into 7 equally spaced 2-mm coronal blocks and processed for paraffin sectioning. A series of adjacent 6-μm-thick sections were cut from each block in the coronal plane and stained with hematoxylin and eosin (H & E). For lesion volume measurement, the 7 brain sections were traced by a microcomputer imaging device (MCID) (Imaging Research, St. Catharine’s, Ontario, Canada), as previously described.9,52 The lesion volume was presented as a volume percentage of the lesion compared with the contralateral hemisphere.
Immunohistochemistry
To examine the effect of EPO on cell proliferation and angiogenesis, coronal sections were immunohistochemically stained with mouse anti-BrdU (1:200; Dako, Carpinteria, CA) and rabbit anti-human von Willebrand factor (vWF, 1:200; DakoCytomation), respectively. The detailed procedures were described in our previous study.33
Immunofluorescent Staining
Newly generated neurons were identified by double labeling for BrdU and NeuN. After dehydration, coronal sections were boiled in 10 mM citric acid buffer (pH 6) for 10 minutes. Sections were incubated in 2.4 N HCl at 37°C for 20 minutes. Sections were incubated with 1% BSA containing 0.3% Triton-X-100 in PBS, and then incubated with mouse anti-NeuN antibody (1:200; Chemicon) at 4°C overnight. After incubation with FITC-conjugated anti-mouse antibody (1:400; Jackson ImmunoResearch) at room temperature for 2 hours, sections were incubated with rat anti-BrdU antibody (1:200; Dako) at 4°C overnight. Sections were then incubated with Cy3-conjugated anti-rat antibody (1:400; Jackson ImmunoResearch) at room temperature for 2 hours. Coronal sections were mounted with Vectashield mounting medium (Vector Laboratories).
Cell Counting and Quantitation
Five sections with 100-μm intervals from the dorsal dentate gyrus were analyzed with a microscope (Nikon i80) at a magnification of 400 via the MCID system.33 All counting was performed on a computer monitor to improve visualization and in one focal plane to avoid oversampling.65 To evaluate whether intraperitoneally administered EPO reduces neuronal damage after TBI, the number of cells was counted in the hippocampus. Although H&E staining is not neuron-specific, the morphological characteristics of neuronal cells in the dentate gyrus, CA1, and CA3 region aid in counting them. Counts were averaged and normalized by measuring the linear distance (in mm) of the dentate gyrus, CA1 and CA3 for each section. Although it is just an estimate of the cell number, this method permits a meaningful comparison of differences between groups. For cell proliferation, the total number of BrdU-positive cells was counted in the lesion boundary zone and the dentate gyrus. The cells with BrdU (brown stained) that clearly localized to the nucleus (hematoxylin stained) were counted as BrdU-positive cells. The number of BrdU-positive cells was expressed in cells/mm2. To evaluate neurogenesis, BrdU/NeuN-colabeled cells were counted in the dentate gyrus and the cortex.43
Statistical Analyses
All data are presented as means with standard deviations (SD). Data on mNSS were first evaluated for normality. The rank data were used for the analysis since data were not normal. Analysis of variance (ANCOVA), PROC MIXED with CONTRAST statement in SAS, was employed to test the group difference on mNSS. The analysis began testing the overall group effect, followed by pair-wise group comparisons if the overall group effect was detected at the 0.05 level; otherwise the pair-wise group comparisons would be considered as exploratory analysis. Data on HCT, body weight, footfault, and spatial learning function were analyzed by ANOVA for repeated measurements. For lesion volume, cell counting, and vWF-stained vascular density, a one-way ANOVA followed by post hoc Student-Newman-Keuls test was used to compare the difference between the EPO-treated, EPO-hemodilution-treated, saline-treated and sham groups. Statistical significance was set at p < 0.05.
Results
Body Weight and Hematocrit
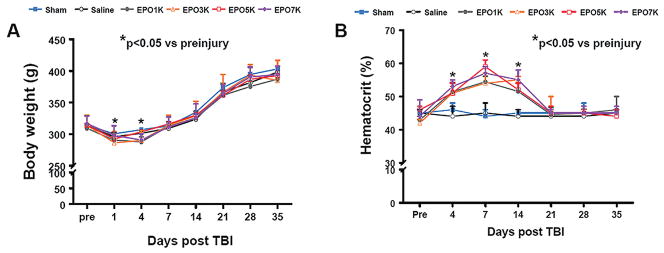
There was no significant difference in the body weight among groups before TBI (Fig.1A). Compared to preinjury level, the body weight significantly decreased at Day 1 (p < 0.001) and Day 4 (p < 0.001), returned to preinjury level one week after TBI and then gained steadily until sacrifice. EPO treatment at different doses did not significantly change the body weight. The baseline of HCT was similar for all animals before injury (Fig.1B). As compared to saline treatment, EPO treatment significantly increased HCT up to 2 weeks (p < 0.001), which returned to normal thereafter. There was no significant difference in HCT among EPO-treated groups.
Fig. 1.
Body weight and hematocrit. “Pre” represents preinjury level. Data represent mean ± SD. *p < 0.05 vs. corresponding Pre. N (rats/group) = 8.
Lesion Volume
Lesion volume measurements were performed at 35 days post TBI. Delayed (24 hours post injury) EPO treatment did not affect the lesion volume after TBI (p > 0.05) compared to saline controls. The lesion volume was 17.5 ± 0.8%, 17.1 ± 0.3%, 16.3 ± 0.3%, 16.4 ± 0.6% and 17.0 ± 0.4% for TBI rats treated with saline, EPO1K, EPO3K, EPO5K, and EPO7K, respectively.
Spatial Learning Test
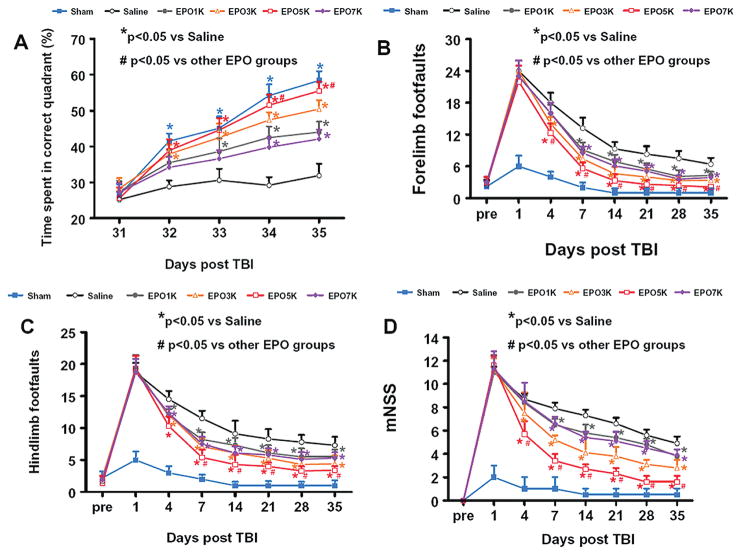
To analyze day-by-day differences in the MWM, a repeated-measures ANOVA was performed and followed by Student-Newman-Keuls tests for multiple comparisons. As shown in Fig. 2A, the time spent in the correct quadrant (northeast) by sham rats gradually increased from Days 31 to 35 after surgery. The saline-treated rats with TBI were significantly impaired compared to sham-operated rats at Days 32–35 (that is, for Days 32, 33, 34 and 35, p = 0.001, < 0.001, < 0.001, and < 0.001, respectively) after injury. As compared to saline treatment, EPO-treated rats with TBI showed significant improvement at Day 32 (p = 0.010 and = 0.013 for EPO3K and EPO5K, respectively), Day 33 (p = 0.020, = 0.002, < 0.001 for EPO1K, EPO3K and EPO5K, respectively), Day 34 (p = 0.022, < 0.001, < 0.001, and = 0.040 for EPO1K, EPO3K, EPO5K and EPO7K, respectively) and Day 35 (p = 0.013, < 0.001, < 0.001, and < 0.001 for EPO1K, EPO3K, EPO5K and EPO7K, respectively). However, as compared to other EPO groups, the EPO5K group showed a significant improvement in spatial learning (that is, a larger percentage of time spent in the correct quadrant) at Day 34 (p < 0.05) and Day 35 (p < 0.05).
Fig. 2.
Effect of EPO treatment on functional outcomes. (A) Spatial learning measured by a recent version of the Morris water maze test at Days 31–35 after TBI. TBI significantly impaired spatial learning at Days 32–35 compared to sham controls (p < 0.05). Delayed treatment with EPO improves spatial learning performance at Days 33–35 compared with the saline group (p < 0.05). However, the spatial learning performance at Days 34 and 35 in the EPO5K group is better than that in other EPO groups (p < 0.05). (B) Effect of EPO on sensorimotor function (forelimb footfault) before and after TBI. Delayed EPO treatment significantly reduces forelimb foot faults at Days 7–35 while EPO3K and 5K treatment significantly reduces them at Day 4 compared with the saline group (p < 0.05). EPO5K shows better effects on reducing forelimb footfaults compared to other EPO groups at Days 4–35 (p < 0.05). (C) Effect of EPO on sensorimotor function (hindlimb footfault) before and after TBI. Delayed EPO treatment significantly reduces hindlimb foot faults at days 4–35 while EPO5K treatment significantly reduces them at Days 7 –35 compared with the other EPO groups (p < 0.05). (D) The plot shows the functional improvement detected on the modified neurological severity scores (mNSS). EPO treatment significantly lowers mNSS scores at Days 7–35 compared to saline group (p < 0.05). EPO3K and 5K significantly reduces mNSS scores at Day 4 (p < 0.05). However, the functional recovery (lowered mNSS score) at Days 4–35 in the EPO5K group is better than that in the EPO3K group (p < 0.05). Data represent mean ± SD. *p < 0.05 vs. Saline group. #p < 0.05 vs. other EPO groups. N (rats/group) =8.
Footfault Test
The incidence of forelimb footfaults during baseline (preoperatively) among all groups was comparable (Fig.2B). Sham surgery alone mildly but significantly increased the incidence of footfaults at post-operative Day 1 (p = 0.015) and Day 4 (p = 0.003). TBI significantly increased the incidence of right forelimb footfaults contralateral to the TBI at 1 to 35 days post injury as compared with the pre-injury baseline (p < 0.001 for Days 1 to 35). EPO treatment at all doses (1000–7000 U/kg) significantly reduced the number of contralateral forelimb footfaults at 7 to 35 days after TBI compared to treatment with saline (p < 0.05), while the medium dosage (EPO3K and EPO5K) showed significantly better benefits at Day 4 (p < 0.001 vs saline). Moreover, EPO5K provides optimal efficacy in reducing forelimb footfaults from Days 4 to 35 (p < 0.05) compared to other EPO groups.
Similar results were found for the contralateral hindlimb (Fig. 2C). As compared to preinjury baseline, TBI significantly increased the incidence of contralateral hindlimb footfaults at 1 to 35 days post-injury (p < 0.05). EPO treatment with all doses tested significantly reduced the number of contralateral hindlimb footfaults at 4 to 35 days after TBI compared to treatment with saline (p < 0.05) while EPO5K showed better benefits at Days 7 to 35 (p < 0.05) compared to other EPO groups.
Neurological Severity Score
Figure 2D shows that there is no significant difference in the mNSS score among the saline and EPO-treated groups at Day 1 post TBI. TBI significantly increased the mNSS scores (the higher the mNSS scores, the worse the sensorimotor function) at 1 to 35 days post injury compared to the sham groups (p < 0.001 for days 1 to 35). However, significantly improved scores (i.e., reduced scores) were measured at Days 7 to 35 after TBI in the EPO-treated groups compared to the saline-treated groups (p < 0.05). The medium dosage (EPO3K and EPO5K) showed significantly better benefits at Day 4 compared to saline treatment (for EPO3K and EPO5K, p = 0.014 and < 0.001 respectively). Moreover, EPO5K provides optimal efficacy in reducing mNSS scores at Days 7 to 35 (p < 0.05 vs other EPO groups).
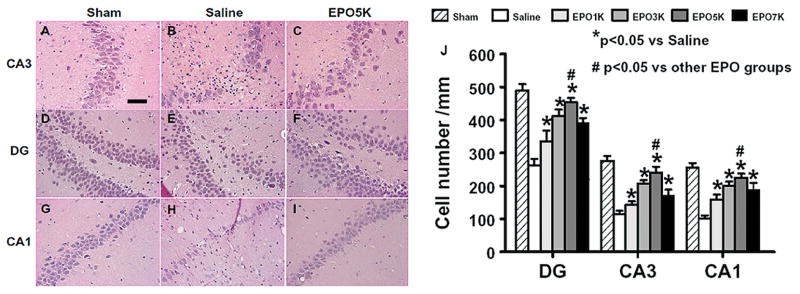
Cell Loss in the Hippocampus
When examined at 35 days post TBI (Fig.3), the neuron counts in the CA3, dentate gyrus, and CA1 of the ipsilateral hippocampus significantly decreased after TBI (Fig. 3B, E and H, p < 0.001) compared to sham controls (Fig.3A, D and G). As compared to saline controls, EPO treatment significantly increased the neuron counts in these regions (Fig.3C, F and I, p<0.05). EPO5K had significantly higher neuron counts in these regions as compared to other EPO dose groups (Fig. 3J, p < 0.001).
Fig. 3.
Effect of EPO on cell loss in the ipsilateral hippocampus at 35 days after TBI. H&E staining: A–I. TBI caused significant cell loss in the CA3, DG and CA1 regions (B, E, and H, p < 0.05) of the ipsilateral hippocampus compared to sham controls (A, D, and G). Delayed treatment with EPO (C, F, and I) significantly reduced cell loss as compared with the saline group (p < 0.05). The cell number in the DG, CA3 and CA1 region is shown in (J). As compared to other EPO groups, the cell number in the EPO5K group was significantly higher (J, p < 0.05). Data represent mean ± SD. Scale bar = 25μm (a–h). *p < 0.05 vs. Saline. #p < 0.05 vs. other EPO groups. N (rats/group) = 8.
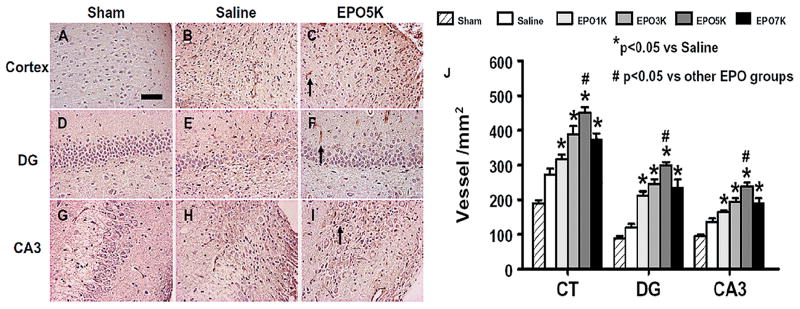
Angiogenesis
TBI alone significantly increased the density of vessels in the cortex, dentate gyrus, and CA3 of the ipsilateral hemisphere (Fig. 4B, E and H, p < 0.001) compared to sham controls (Fig.4A, D and G). EPO treatment significantly increased the vascular density in the cortex, DG and CA3 (Fig. 4C, F and I, p < 0.05) compared to saline treatment. A significantly higher vascular density was observed in the EPO5K group compared to the other EPO groups (Fig. 4J, p < 0.001).
Fig. 4.
Effect of EPO on vWF-staining vascular structure in the injured cortex, ipsilateral DG and CA3 region 35 days after TBI. TBI alone (B, E and H, p < 0.05) significantly increased the vascular density in these regions compared to sham controls (A, D and G, p < 0.05). EPO treatment further enhanced angiogenesis after TBI compared to saline groups (C, F and I, p < 0.05). The density of vWF-stained vasculature is shown in (J). As compared to other EPO groups, the EPO5K group had a significantly higher vascular density in these regions (J, p < 0.05). Data represent mean ± SD. Scale bar = 50μm (a); 25 μm (e). *p < 0.05 vs. Saline. #p < 0.05 vs. other EPO groups. N (rats/group) = 8.
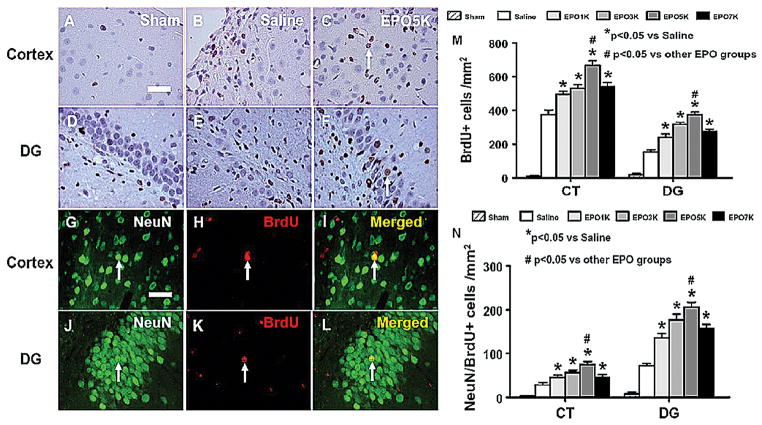
Cell Proliferation
BrdU labeling and staining is commonly used to detect cell proliferation.33 The number of BrdU-positive cells found in the ipsilateral cortex and dentate gyrus (Fig. 5B and E, p < 0.001) was significantly increased at 35 days after TBI, compared with sham controls (Fig. 5A and D). However, EPO treatment further increased the number of BrdU-positive cells in the cortex and dentate gyrus (Fig. 5C and F, p < 0.001) after TBI compared to saline controls. A significantly higher density of BrdU-positive cells in these regions was observed in the EPO5K group compared to other EPO-treated groups (Fig. 5M, p ≤ 0.001).
Fig.5.
Effect of EPO on BrdU-positive cells and NeuN/BrdU-positive cells in the injured cortex and ipsilateral DG 35 days after TBI. The cells with BrdU (brown stained) that clearly localized to the nucleus (hematoxylin stained) were counted as BrdU-positive cells (arrows in C and F). TBI alone (B and E) significantly increased the number of BrdU-positive cells in the ipsilateral cortex and DG compared to sham controls (A and D, p < 0.05). The number of BrdU-positive cells is shown in M). EPO treatment significantly increased the number of BrdU-positive cells in these regions (p < 0.05) compared to saline groups. As compared to other EPO groups, the EPO5K group had a significantly larger number of BrdU-positive cells in these regions (M, p < 0.05). Double fluorescent staining for BrdU (red, H and K) and NeuN (green, G and J) to identify newborn neurons (yellow after merge, I and L) in the injured cortex (G–I) and the ipsilateral DG (J–L) at 35 days after TBI and EPO treatment. The newborn neuron number in the injured cortex and DG is shown in (N). EPO treatment significantly increased the number of NeuN/BrdU-positive cells in these regions (p < 0.05) compared to saline groups. As compared to other EPO groups, the EPO5K group had a significantly larger number of NeuN/BrdU-positive cells in these regions (N, p < 0.05). Data represent mean ± SD. Scale bar = 25μm. *p < 0.05 vs. Saline. #p < 0.05 vs. other EPO groups. N (rats/group) = 8.
Neurogenesis
Newly generated neurons were identified by double labeling for BrdU (proliferating marker, Fig. 5H and K) and NeuN (mature neuronal marker, Fig. 5G and J). The number of NeuN/BrdU-colabeled cells (newborn neurons) was significantly higher in the injured cortex and dentate gyrus (Fig. 5N, p < 0.001) after TBI compared to sham controls. EPO treatment significantly increased the number of newborn neurons in the injured cortex and dentate gyrus (Fig. 5N, p < 0.001) compared to saline controls. In addition, the number of newborn neurons in the injured cortex and dentate gyrus was significantly higher in the EPO5K group than in the other EPO groups (Fig. 5N, p < 0.001).
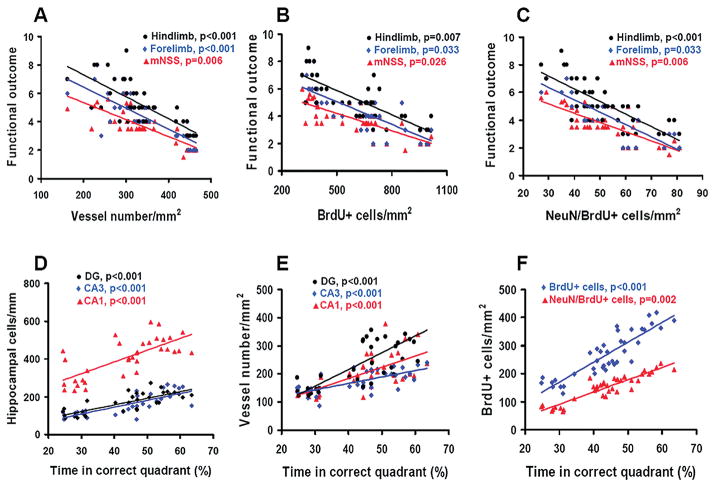
Correlation of Histological Changes with Functional Recovery
Although delayed EPO therapy did not reduce cortical lesion volume caused by TBI, EPO treatment significantly improved sensorimotor and spatial learning recovery assessed by footfault and mNSS as well as MWM tests. Correlation analyses indicate that sensorimotor functional deficits (as measured by forelimb, hindlimb footfault and mNSS) are highly and inversely correlated to increased vascular density (Fig. 6A), cell proliferation (Fig. 6B) and neurogenesis (Fig. 6C) in the injured cortex examined at Day 35 after TBI (p < 0.05). Similarly, spatial learning (percentage of time spent in correct quadrant) is highly and positively correlated to increased neuron number (Fig. 6D) and vascular density in the injured dentate gyrus, CA3, and CA1 (Fig. 6E) as well as to increased cell proliferation and newborn neurons in the dentate gyrus (Fig. 6F) assessed at Day 35 after TBI (p < 0.05). Theses data indicate that EPO may improve neurological recovery by reducing neuronal loss and promoting angiogenesis and neurogenesis.
Fig. 6.
Correlation of functional outcomes with cell loss, angiogenesis, cell proliferation and neurogenesis. The top panel line graphs show that the functional outcomes (hindlimb, forelimb footfault and mNSS scores) are significantly and inversely correlated with the number of vessels (A), BrdU-positive cells (B) and NeuN/BrdU-positive cells (C) in the injured cortex measured at Day 35 after TBI and EPO treatment (p < 0.05). The bottom panel line graphs show that spatial learning performance is significantly and positively correlated with the number of neuron cells (D), vessels (E), BrdU-positive and NeuN/BrdU-positive cells (F) in the ipsilateral hippocampus measured at Day 35 in rats after TBI and EPO treatment (p < 0.05). Data represent mean ± SD. N (rats/group) = 8.
Discussion
Our present study demonstrates a significant dose-dependent long-lasting improvement in sensorimotor and spatial learning after TBI in rats treated with EPO. The main findings are: 1) delayed (24 hours post injury) EPO treatment after TBI provides long-term behavioral benefits with a wide range of effective EPO doses (from 1000 to 7000 U/kg ip); 2) although all EPO doses tested shows substantial benefits after TBI, the repeated 5000 U/kg paradigm provides an optimal functional outcome; and 3) the improvements in spatial learning and sensorimotor function are highly and significantly correlated to the effect of EPO on reducing hippocampal cell loss and promoting angiogenesis and neurogenesis in the injured cortex and hippocampus.
EPO given within 6 hours after TBI reduces brain damage and improves functional recovery in rats.10,61 Our recent findings demonstrated that delayed (24 hours post injury) EPO therapy does not reduce cortical lesion volume but improves functional outcomes after TBI,33,63 indicating that the therapeutic time window may not be limited to the early hours after TBI. However, the optimal EPO dose, dosing interval, and number of doses for reducing brain injury and promoting neurorestoration after TBI have not been fully investigated. In the present study, EPO doses used for treating TBI were much higher than those used for correcting anemia and therefore significantly increased HCT. Although no significant difference in the HCT level was observed among the EPO-treated groups, there was a significant functional improvement in different EPO dose groups. This suggests that EPO-induced therapeutic effects are independent of increased HCT, which is consistent with our previous finding that normalization of the HCT by normovolemic hemodilution does not affect the histological and functional outcome of EPO therapy for TBI.69 The present study demonstrated that delayed EPO treatment improved functional recovery, reduced hippocampal neuron loss, and increased angiogenesis and neurogenesis in a dose-dependent manner. The medium dose (5000 U/kg given intraperitoneally at 24, 48, and 72 hours post TBI) provided the maximal functional recovery. In addition, EPO treatment significantly increased the total number of newborn neurons found in the injured cortex, suggesting the EPO treatment induces SVZ-derived neurogenesis (that is, migration of neuroblasts from the SVZ into the injured cortex where some of the SVZ-derived neuroblasts differentiate into mature neurons, which has been demonstrated after stroke and TBI).19,50,66,67 EPO therapy also significantly increased the total number of newborn neurons in the dentate gyrus in the present study, which agrees with findings from our previous studies. 33,63 Newborn granule neurons in the dentate gyrus are capable of establishing anatomical integration into the CA3 region after TBI.49 Our present data suggest that EPO-promoted newborn neurons may participate in brain repair and functional recovery after TBI.
The adult brain vascular system is stable under normal conditions, but is activated in response to certain pathological conditions including injuries.25 Adult vascular remodeling includes angiogenesis by either mature endothelial cells (that is, the formation of new capillaries from pre-existing vessels) and vasculogenesis by endothelial progenitor cells (EPCs). EPCs are present in the bone marrow and peripheral blood, and are mobilized to the peripheral blood following TBI.26 Our present study shows that EPO promotes TBI-induced angiogenesis in a dose-dependent manner. Angiogenesis may provide the critical neurovascular microenvironments for neuronal remodeling. The coupling of angiogenesis and neurogenesis has been demonstrated in rodents after brain injuries.7,12,58,60 Treatment with EPO contributes to neurovascular remodeling, leading to improved neurobehavioral outcomes following ischemic brain injury.27,58 EPO stimulates vascular repair by facilitating EPC migration into the brain and neovascularization, and promotes neurogenesis.55 EPO treatment upregulates the EPOR level in vascular endothelial cells, confers neurovascular protection, and enhances angiogenesis after permanent focal cerebral ischemia in adult mice.30 Our recent study demonstrates that tumor necrosis factor alpha primes cerebral endothelial cells for erythropoietin-induced angiogenesis.57 In addition, our in vitro study shows that EPO enhances VEGF secretion in neural progenitor cells through activation of the phosphatidylinositol-3 kinase/protein kinase B (PI3K/Akt) and extracellular signal-regulated kinases 1 and 2 (ERK1/2) signal-transduction pathways and that neural progenitor cells treated with EPO upregulate VEGFR2 expression in cerebral endothelial cells, which along with VEGF secreted by neural progenitor cells promotes angiogenesis.56 In addition to its robust angiogenic effects, VEGF is capable of promoting hippocampal neurogenesis in the SVZ and SGZ in response to TBI.29,53
EPO and EPOR are weakly expressed in normal adult brains.21 EPO expression is transiently upregulated the first 3 days after TBI while upregulated expression of EPOR lasts for at least one week.31 These findings suggest that the transient increase in endogenous EPO expression may not match prolonged increased expression of EPOR, and therefore may not provide sufficient neuroprotection after TBI. Prolonged EPOR upregulation provides a platform for exogenous EPO treatment and suggests multiple doses may be required. In the present study, low (1000 U/kg) or high (7000 U/kg) doses of delayed EPO therapy show substantial benefits; while the medium dose of EPO (5000 U/kg) provides optimal outcomes. EPO has a limited capacity to cross the blood-brain barrier.3,59 The low dose of EPO would lead to a low brain EPO level, which may limit the benefits as demonstrated in animal stroke and TBI.32,59 However, the higher dose of EPO did not show better benefits compared to the medium dose in the present study. Some studies have shown that high doses of EPO are associated with a lack of or reduced efficacy compared to lower doses.4,18 Systemic administration of higher dose EPO will fully activate its hematopoietic (for example, increased HCT) and other vascular activities, including strong pro-coagulant and hemodynamic effects. Recent clinical EPO studies confirmed these concerns, with a significantly increased incidence of thrombosis4,18 or risk of serious complications (intracerebral hemorrhage, brain edema) and death especially when combined with tPA after stroke.18
Several EPO clinical trials in patients with TBI or aneurysmal subarachnoid hemorrhage (aSAH) are ongoing or have been completed. In a small pilot randomized trial, TBI patients either received a single dose of EPO (40,000 U iv, n = 11) or saline placebo (n = 5) within 6 hours after injury and the primary outcome measure was serum S-100B and neuron-specific enolase (NSE) levels.41 The EPO treatment did not impact NSE or S100B levels compared to placebo. Outcome failure in this small clinical study does not necessarily indicate a lack of therapeutic potential of EPO, but suggests that EPO is safe to use and that a higher dose or different dosing regimen may be required to demonstrate efficacy. In addition, several EPO TBI clinical trials are ongoing (www.clinicaltrials.gov: NCT00987454; NCT00313716; NCT00375869) with doses based on the EPO stroke clinical trials.17,18 In a double-blind randomized clinical trial, the beneficial effects of EPO (500 U/kg/day for three days) in patients with aSAH could not be concluded.47 However, in a recent Phase II randomized, double-blind, placebo-controlled trial, within 72 hours of aSAH, 80 patients were randomized to receive intravenous EPO (30,000 U) or placebo every 48 hours for a total of 90,000 U.54 This preliminary study showed that EPO reduced delayed cerebral ischemia following aSAH via decreasing severity of vasospasm and shortening impaired autoregulation. Among the 71 survivors, the EPO group had fewer deficits measured using the National Institutes of Health Stroke Scale. These inconclusive results encourage further investigation of the potential of EPO as a candidate drug for the treatment of brain injury by improving preclinical experimental design and performing associated clinical trials.
There are several limitations in the present study. First, the brain EPO level was not measured although previous studies show that a dose-dependent increase was observed in the brain EPO level in rats treated with EPO after stroke59 and TBI.32 Second, although we found that EPO treatment at doses from 1000 to 7000 U/kg similarly increases HCT, the effects of these doses on pro-coagulant activities and hemodynamics as well as PO2, PCO2 and blood pH were not examined, the potential side effects of which may affect the outcome. Third, the optimal dose (5000 U/kg intraperitoneally at 24, 48 and 72 hours post injury) cannot be simply extended to other therapeutic time windows or paradigms such as intravenous injection, a single-dose treatment, and other therapeutic times of multiple-dose chronic treatment. Fourth, although our data show that the EPO-induced effects on hippocampal cells, cell proliferation, and angiogenesis and neurogenesis may contribute to functional recovery; other beneficial effects of EPO cannot be excluded. For example, our recent study demonstrates that EPO-induced corticospinal axonal sprouting from contralateral cortex is highly correlated to sensorimotor functional recovery after TBI.68 Further investigation of these aspects is warranted.
In conclusion, delayed (24 hour) repeated EPO therapy for TBI significantly reduces hippocampal cell loss, enhances angiogenesis and neurogenesis, and improves sensorimotor function and spatial learning recovery in a dose-dependent manner. These findings suggest that selecting the optimal EPO dose for treatment of TBI is crucial and should be emphasized in designing preclinical and clinical trials.
Acknowledgments
Sources of financial support: NINDS grants RO1 NS62002 (Ye Xiong) and PO1 NS42345 (Asim Mahmood, Michael Chopp).
Footnotes
Disclosure
This work was supported by NIH Grant Nos. RO1 NS62002 (to Dr. Xiong) and PO1 NS42345 (to Drs. Mahmood and Chopp). Special thanks to Ms. Susan MacPhee-Gray for editorial assistance.
Author contributions to the study and manuscript preparation include the following: Conception and design - Xiong, Mahmood, Chopp; Acquisition of data -Meng, Zhang, Xiong, Qu; Analysis and interpretation of data - Meng, Xiong, Chopp; Drafting of the manuscript - Meng, Xiong, Chopp; Critical review of the manuscript -Xiong, Chopp; and Review of final version of the manuscript and approval for submission - all authors.
References
- 1.Barth TM, Jones TA, Schallert T. Functional subdivisions of the rat somatic sensorimotor cortex. Behav Brain Res. 1990;39:73–95. doi: 10.1016/0166-4328(90)90122-u. [DOI] [PubMed] [Google Scholar]
- 2.Baskin YK, Dietrich WD, Green EJ. Two effective behavioral tasks for evaluating sensorimotor dysfunction following traumatic brain injury in mice. J Neurosci Methods. 2003;129:87–93. doi: 10.1016/s0165-0270(03)00212-7. [DOI] [PubMed] [Google Scholar]
- 3.Brines ML, Ghezzi P, Keenan S, Agnello D, de Lanerolle NC, Cerami C, et al. Erythropoietin crosses the blood-brain barrier to protect against experimental brain injury. Proc Natl Acad Sci U S A. 2000;97:10526–10531. doi: 10.1073/pnas.97.19.10526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cariou A, Claessens YE, Pene F, Marx JS, Spaulding C, Hababou C, et al. Early high-dose erythropoietin therapy and hypothermia after out-of-hospital cardiac arrest: a matched control study. Resuscitation. 2008;76:397–404. doi: 10.1016/j.resuscitation.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Celik M, Gokmen N, Erbayraktar S, Akhisaroglu M, Konakc S, Ulukus C, et al. Erythropoietin prevents motor neuron apoptosis and neurologic disability in experimental spinal cord ischemic injury. Proc Natl Acad Sci U S A. 2002;99:2258–2263. doi: 10.1073/pnas.042693799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cerami A. Beyond erythropoiesis: novel applications for recombinant human erythropoietin. Semin Hematol. 2001;38:33–39. doi: 10.1016/s0037-1963(01)90128-3. [DOI] [PubMed] [Google Scholar]
- 7.Chen J, Chopp M. Neurorestorative treatment of stroke: cell and pharmacological approaches. NeuroRx. 2006;3:466–473. doi: 10.1016/j.nurx.2006.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen J, Sanberg PR, Li Y, Wang L, Lu M, Willing AE, et al. Intravenous administration of human umbilical cord blood reduces behavioral deficits after stroke in rats. Stroke. 2001;32:2682–2688. doi: 10.1161/hs1101.098367. [DOI] [PubMed] [Google Scholar]
- 9.Chen J, Zhang C, Jiang H, Li Y, Zhang L, Robin A, et al. Atorvastatin induction of VEGF and BDNF promotes brain plasticity after stroke in mice. J Cereb Blood Flow Metab. 2005;25:281–290. doi: 10.1038/sj.jcbfm.9600034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cherian L, Goodman JC, Robertson C. Neuroprotection with erythropoietin administration following controlled cortical impact injury in rats. J Pharmacol Exp Ther. 2007;322:789–794. doi: 10.1124/jpet.107.119628. [DOI] [PubMed] [Google Scholar]
- 11.Choi SH, Woodlee MT, Hong JJ, Schallert T. A simple modification of the water maze test to enhance daily detection of spatial memory in rats and mice. J Neurosci Methods. 2006;156:182–193. doi: 10.1016/j.jneumeth.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Chopp M, Zhang ZG, Jiang Q. Neurogenesis, angiogenesis, and MRI indices of functional recovery from stroke. Stroke. 2007;38:827–831. doi: 10.1161/01.STR.0000250235.80253.e9. [DOI] [PubMed] [Google Scholar]
- 13.Cotena S, Piazza O, Tufano R. The use of erythtropoietin in cerebral diseases. Panminerva Med. 2008;50:185–192. [PubMed] [Google Scholar]
- 14.Davis AE. Mechanisms of traumatic brain injury: biomechanical, structural and cellular considerations. Crit Care Nurs Q. 2000;23:1–13. doi: 10.1097/00002727-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Day LB, Weisand M, Sutherland RJ, Schallert T. The hippocampus is not necessary for a place response but may be necessary for pliancy. Behav Neurosci. 1999;113:914–924. doi: 10.1037//0735-7044.113.5.914. [DOI] [PubMed] [Google Scholar]
- 16.Dixon CE, Clifton GL, Lighthall JW, Yaghmai AA, Hayes RL. A controlled cortical impact model of traumatic brain injury in the rat. J Neurosci Methods. 1991;39:253–262. doi: 10.1016/0165-0270(91)90104-8. [DOI] [PubMed] [Google Scholar]
- 17.Ehrenreich H, Hasselblatt M, Dembowski C, Cepek L, Lewczuk P, Stiefel M, et al. Erythropoietin therapy for acute stroke is both safe and beneficial. Mol Med. 2002;8:495–505. [PMC free article] [PubMed] [Google Scholar]
- 18.Ehrenreich H, Weissenborn K, Prange H, Schneider D, Weimar C, Wartenberg K, et al. Recombinant human erythropoietin in the treatment of acute ischemic stroke. Stroke. 2009;40:e647–656. doi: 10.1161/STROKEAHA.109.564872. [DOI] [PubMed] [Google Scholar]
- 19.Goings GE, Sahni V, Szele FG. Migration patterns of subventricular zone cells in adult mice change after cerebral cortex injury. Brain Res. 2004;996:213–226. doi: 10.1016/j.brainres.2003.10.034. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez FF, McQuillen P, Mu D, Chang Y, Wendland M, Vexler Z, et al. Erythropoietin enhances long-term neuroprotection and neurogenesis in neonatal stroke. Dev Neurosci. 2007;29:321–330. doi: 10.1159/000105473. [DOI] [PubMed] [Google Scholar]
- 21.Grasso G, Sfacteria A, Cerami A, Brines M. Erythropoietin as a tissue-protective cytokine in brain injury: what do we know and where do we go? Neuroscientist. 2004;10:93–98. doi: 10.1177/1073858403259187. [DOI] [PubMed] [Google Scholar]
- 22.Grasso G, Sfacteria A, Erbayraktar S, Passalacqua M, Meli F, Gokmen N, et al. Amelioration of spinal cord compressive injury by pharmacological preconditioning with erythropoietin and a nonerythropoietic erythropoietin derivative. J Neurosurg Spine. 2006;4:310–318. doi: 10.3171/spi.2006.4.4.310. [DOI] [PubMed] [Google Scholar]
- 23.Grasso G, Sfacteria A, Meli F, Passalacqua M, Fodale V, Buemi M, et al. The role of erythropoietin in neuroprotection: therapeutic perspectives. Drug News Perspect. 2007;20:315–320. doi: 10.1358/dnp.2007.20.5.1120219. [DOI] [PubMed] [Google Scholar]
- 24.Grasso G, Sfacteria A, Passalacqua M, Morabito A, Buemi M, Macri B, et al. Erythropoietin and erythropoietin receptor expression after experimental spinal cord injury encourages therapy by exogenous erythropoietin. Neurosurgery. 2005;56:821–827. doi: 10.1227/01.neu.0000156493.00904.7e. discussion 821–827. [DOI] [PubMed] [Google Scholar]
- 25.Greenberg DA, Jin K. From angiogenesis to neuropathology. Nature. 2005;438:954–959. doi: 10.1038/nature04481. [DOI] [PubMed] [Google Scholar]
- 26.Guo X, Liu L, Zhang M, Angela B, Zhang J. Correlation of CD34+ cells with Tissue Angiogenesis after Traumatic Brain Injury in a Rat Model. J Neurotrauma. 2009 doi: 10.1089/neu.2008.0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iwai M, Cao G, Yin W, Stetler RA, Liu J, Chen J. Erythropoietin promotes neuronal replacement through revascularization and neurogenesis after neonatal hypoxia/ischemia in rats. Stroke. 2007;38:2795–2803. doi: 10.1161/STROKEAHA.107.483008. [DOI] [PubMed] [Google Scholar]
- 28.Jia L, Chopp M, Zhang L, Lu M, Zhang Z. Erythropoietin in combination of tissue plasminogen activator exacerbates brain hemorrhage when treatment is initiated 6 hours after stroke. Stroke. 2010;41:2071–2076. doi: 10.1161/STROKEAHA.110.586198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee C, Agoston DV. Vascular endothelial growth factor is involved in mediating increased de novo hippocampal neurogenesis in response to traumatic brain injury. J Neurotrauma. 2010;27:541–553. doi: 10.1089/neu.2009.0905. [DOI] [PubMed] [Google Scholar]
- 30.Li Y, Lu Z, Keogh CL, Yu SP, Wei L. Erythropoietin-induced neurovascular protection, angiogenesis, and cerebral blood flow restoration after focal ischemia in mice. J Cereb Blood Flow Metab. 2007;27:1043–1054. doi: 10.1038/sj.jcbfm.9600417. [DOI] [PubMed] [Google Scholar]
- 31.Liao ZB, Zhi XG, Shi QH, He ZH. Recombinant human erythropoietin administration protects cortical neurons from traumatic brain injury in rats. Eur J Neurol. 2008;15:140–149. doi: 10.1111/j.1468-1331.2007.02013.x. [DOI] [PubMed] [Google Scholar]
- 32.Lieutaud T, Andrews PJ, Rhodes JK, Williamson R. Characterization of the pharmacokinetics of human recombinant erythropoietin in blood and brain when administered immediately after lateral fluid percussion brain injury and its pharmacodynamic effects on IL-1beta and MIP-2 in rats. J Neurotrauma. 2008;25:1179–1185. doi: 10.1089/neu.2008.0591. [DOI] [PubMed] [Google Scholar]
- 33.Lu D, Mahmood A, Qu C, Goussev A, Schallert T, Chopp M. Erythropoietin enhances neurogenesis and restores spatial memory in rats after traumatic brain injury. J Neurotrauma. 2005;22:1011–1017. doi: 10.1089/neu.2005.22.1011. [DOI] [PubMed] [Google Scholar]
- 34.Lu D, Mahmood A, Qu C, Hong X, Kaplan D, Chopp M. Collagen scaffolds populated with human marrow stromal cells reduce lesion volume and improve functional outcome after traumatic brain injury. Neurosurgery. 2007;61:596–602. doi: 10.1227/01.NEU.0000290908.38438.B2. discussion 602–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mahmood A, Lu D, Chopp M. Marrow stromal cell transplantation after traumatic brain injury promotes cellular proliferation within the brain. Neurosurgery. 2004;55:1185–1193. doi: 10.1227/01.neu.0000141042.14476.3c. [DOI] [PubMed] [Google Scholar]
- 36.Mahmood A, Lu D, Qu C, Goussev A, Zhang ZG, Lu C, et al. Treatment of traumatic brain injury in rats with erythropoietin and carbamylated erythropoietin. J Neurosurg. 2007;107:392–397. doi: 10.3171/JNS-07/08/0392. [DOI] [PubMed] [Google Scholar]
- 37.Minnerup J, Heidrich J, Rogalewski A, Schabitz WR, Wellmann J. The efficacy of erythropoietin and its analogues in animal stroke models: a meta-analysis. Stroke. 2009;40:3113–3120. doi: 10.1161/STROKEAHA.109.555789. [DOI] [PubMed] [Google Scholar]
- 38.Morris R. Developments of a water-maze procedure for studying spatial learning in the rat. J Neurosci Methods. 1984;11:47–60. doi: 10.1016/0165-0270(84)90007-4. [DOI] [PubMed] [Google Scholar]
- 39.Morris RG, Garrud P, Rawlins JN, O’Keefe J. Place navigation impaired in rats with hippocampal lesions. Nature. 1982;297:681–683. doi: 10.1038/297681a0. [DOI] [PubMed] [Google Scholar]
- 40.Narayan RK, Michel ME, Ansell B, Baethmann A, Biegon A, Bracken MB, et al. Clinical trials in head injury. J Neurotrauma. 2002;19:503–557. doi: 10.1089/089771502753754037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nirula R, Diaz-Arrastia R, Brasel K, Weigelt JA, Waxman K. Safety and efficacy of erythropoietin in traumatic brain injury patients: a pilot randomized trial. Crit Care Res Pract. 2010 doi: 10.1155/2010/209848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Noguchi CT, Wang L, Rogers HM, Teng R, Jia Y. Survival and proliferative roles of erythropoietin beyond the erythroid lineage. Expert Rev Mol Med. 2008;10:e36. doi: 10.1017/S1462399408000860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Popoli P, Pepponi R, Martire A, Armida M, Pezzola A, Galluzzo M, et al. Neuroprotective effects of thymosin beta4 in experimental models of excitotoxicity. Ann N Y Acad Sci. 2007;1112:219–224. doi: 10.1196/annals.1415.033. [DOI] [PubMed] [Google Scholar]
- 44.Royo NC, Schouten JW, Fulp CT, Shimizu S, Marklund N, Graham DI, et al. From cell death to neuronal regeneration: building a new brain after traumatic brain injury. J Neuropathol Exp Neurol. 2003;62:801–811. doi: 10.1093/jnen/62.8.801. [DOI] [PubMed] [Google Scholar]
- 45.Sakanaka M, Wen TC, Matsuda S, Masuda S, Morishita E, Nagao M, et al. In vivo evidence that erythropoietin protects neurons from ischemic damage. Proc Natl Acad Sci U S A. 1998;95:4635–4640. doi: 10.1073/pnas.95.8.4635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schallert T. Behavioral tests for preclinical intervention assessment. NeuroRx. 2006;3:497–504. doi: 10.1016/j.nurx.2006.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Springborg JB, Moller C, Gideon P, Jorgensen OS, Juhler M, Olsen NV. Erythropoietin in patients with aneurysmal subarachnoid haemorrhage: a double blind randomised clinical trial. Acta Neurochir (Wien) 2007;149:1089–1101. doi: 10.1007/s00701-007-1284-z. discussion 1101. [DOI] [PubMed] [Google Scholar]
- 48.Stoica B, Byrnes K, Faden AI. Multifunctional drug treatment in neurotrauma. Neurotherapeutics. 2009;6:14–27. doi: 10.1016/j.nurt.2008.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sun D, McGinn MJ, Zhou Z, Harvey HB, Bullock MR, Colello RJ. Anatomical integration of newly generated dentate granule neurons following traumatic brain injury in adult rats and its association to cognitive recovery. Exp Neurol. 2007;204:264–272. doi: 10.1016/j.expneurol.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 50.Sundholm-Peters NL, Yang HK, Goings GE, Walker AS, Szele FG. Subventricular zone neuroblasts emigrate toward cortical lesions. J Neuropathol Exp Neurol. 2005;64:1089–1100. doi: 10.1097/01.jnen.0000190066.13312.8f. [DOI] [PubMed] [Google Scholar]
- 51.Sutherland RJ, Kolb B, Whishaw IQ. Spatial mapping: definitive disruption by hippocampal or medial frontal cortical damage in the rat. Neurosci Lett. 1982;31:271–276. doi: 10.1016/0304-3940(82)90032-5. [DOI] [PubMed] [Google Scholar]
- 52.Swanson RA, Morton MT, Tsao-Wu G, Savalos RA, Davidson C, Sharp FR. A semiautomated method for measuring brain infarct volume. J Cereb Blood Flow Metab. 1990;10:290–293. doi: 10.1038/jcbfm.1990.47. [DOI] [PubMed] [Google Scholar]
- 53.Thau-Zuchman O, Shohami E, Alexandrovich AG, Leker RR. Vascular endothelial growth factor increases neurogenesis after traumatic brain injury. J Cereb Blood Flow Metab. 2010;30:1008–1016. doi: 10.1038/jcbfm.2009.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tseng MY, Hutchinson PJ, Richards HK, Czosnyka M, Pickard JD, Erber WN, et al. Acute systemic erythropoietin therapy to reduce delayed ischemic deficits following aneurysmal subarachnoid hemorrhage: a Phase II randomized, double-blind, placebo-controlled trial. Clinical article. J Neurosurg. 2009;111:171–180. doi: 10.3171/2009.3.JNS081332. [DOI] [PubMed] [Google Scholar]
- 55.Velly L, Pellegrini L, Guillet B, Bruder N, Pisano P. Erythropoietin 2nd cerebral protection after acute injuries: A double-edged sword? Pharmacol Ther. 2010 doi: 10.1016/j.pharmthera.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 56.Wang L, Chopp M, Gregg SR, Zhang RL, Teng H, Jiang A, et al. Neural progenitor cells treated with EPO induce angiogenesis through the production of VEGF. J Cereb Blood Flow Metab. 2008;28:1361–1368. doi: 10.1038/jcbfm.2008.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang L, Chopp M, Teng H, Bolz M, Francisco MA, Aluigi DM, et al. Tumor necrosis factor alpha primes cerebral endothelial cells for erythropoietin-induced angiogenesis. J Cereb Blood Flow Metab. 2010 doi: 10.1038/jcbfm.2010.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang L, Zhang Z, Wang Y, Zhang R, Chopp M. Treatment of stroke with erythropoietin enhances neurogenesis and angiogenesis and improves neurological function in rats. Stroke. 2004;35:1732–1737. doi: 10.1161/01.STR.0000132196.49028.a4. [DOI] [PubMed] [Google Scholar]
- 59.Wang Y, Zhang ZG, Rhodes K, Renzi M, Zhang RL, Kapke A, et al. Post-ischemic treatment with erythropoietin or carbamylated erythropoietin reduces infarction and improves neurological outcome in a rat model of focal cerebral ischemia. Br J Pharmacol. 2007;151:1377–1384. doi: 10.1038/sj.bjp.0707285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xiong Y, Mahmood A, Chopp M. Angiogenesis, neurogenesis and brain recovery of function following injury. Curr Opin Investig Drugs. 2010;11:298–308. [PMC free article] [PubMed] [Google Scholar]
- 61.Xiong Y, Mahmood A, Lu D, Qu C, Goussev A, Schallert T, et al. Role of gender in outcome after traumatic brain injury and therapeutic effect of erythropoietin in mice. Brain Res. 2007;1185:301–312. doi: 10.1016/j.brainres.2007.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xiong Y, Mahmood A, Lu D, Qu C, Kazmi H, Goussev A, et al. Histological and functional outcomes after traumatic brain injury in mice null for the erythropoietin receptor in the central nervous system. Brain Res. 2008;1230:247–257. doi: 10.1016/j.brainres.2008.06.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xiong Y, Mahmood A, Meng Y, Zhang Y, Qu C, Schallert T, et al. Delayed administration of erythropoietin reducing hippocampal cell loss, enhancing angiogenesis and neurogenesis, and improving functional outcome following traumatic brain injury in rats: comparison of treatment with single and triple dose. J Neurosurg. 2009 doi: 10.3171/2009.9.JNS09844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang R, Wang Y, Zhang L, Zhang Z, Tsang W, Lu M, et al. Sildenafil (Viagra) induces neurogenesis and promotes functional recovery after stroke in rats. Stroke. 2002;33:2675–2680. doi: 10.1161/01.str.0000034399.95249.59. [DOI] [PubMed] [Google Scholar]
- 65.Zhang R, Wang Y, Zhang L, Zhang Z, Tsang W, Lu M, et al. Sildenafil (Viagra) induces neurogenesis and promotes functional recovery after stroke in rats. Stroke. 2002;33:2675–2680. doi: 10.1161/01.str.0000034399.95249.59. [DOI] [PubMed] [Google Scholar]
- 66.Zhang R, Zhang Z, Wang L, Wang Y, Gousev A, Zhang L, et al. Activated neural stem cells contribute to stroke-induced neurogenesis and neuroblast migration toward the infarct boundary in adult rats. J Cereb Blood Flow Metab. 2004;24:441–448. doi: 10.1097/00004647-200404000-00009. [DOI] [PubMed] [Google Scholar]
- 67.Zhang RL, Zhang ZG, Chopp M. Ischemic stroke and neurogenesis in the subventricular zone. Neuropharmacology. 2008;55:345–352. doi: 10.1016/j.neuropharm.2008.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang Y, Xiong Y, Mahmood A, Meng Y, Liu Z, Qu C, et al. Sprouting of corticospinal tract axons from the contralateral hemisphere into the denervated side of the spinal cord is associated with functional recovery in adult rat after traumatic brain injury and erythropoietin treatment. Brain Res. 2010;1353:249–257. doi: 10.1016/j.brainres.2010.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang Y, Xiong Y, Mahmood A, Meng Y, Qu C, Schallert T, et al. Therapeutic effects of erythropoietin on histological and functional outcomes following traumatic brain injury in rats are independent of hematocrit. Brain Res. 2009;1294:153–164. doi: 10.1016/j.brainres.2009.07.077. [DOI] [PMC free article] [PubMed] [Google Scholar]