Abstract
Background/Aims
Endoscopic retrograde cholangiopancreatography (ERCP) is the standard approach for the management of biliary complications in liver transplant patients; however, its safety and efficacy have not been established in this setting. This study was performed to evaluate the safety and long-term efficacy of ERCP in transplant patients.
Methods
The case reports of 1,500 liver transplant patients were reviewed. Orthotopic liver transplantation (OLT) patients were matched 1:2 with non-OLT patients and followed-up for long-term outcome (median, 7.4 years).
Results
Of the 1,500 liver transplant patients, 94 (6.3%) underwent 150 ERCPs after OLT. Anastomotic strictures were present in 45 patients, biliary stones in 24, biliary leaks in 7, papillary stenosis in 2, and primary sclerosing cholangitis in 1. An ERCP success rate of 90.7% was achieved; biliary stenting led to resolution of the bile leak in 7/7 (100%) patients, and biliary stones were removed in 21/24 (87.5%) patients. In addition, 34 of 45 patients with anastomotic stricture underwent endoscopic dilation. We obtained complete resolution in 22/34 (64.7%) patients. OLT patients did not show a higher probability of complications (odds ratio [OR], 1.04), of pancreatitis (OR, 0.80) or of bleeding (OR, 1.34).
Conclusions
ERCP is safe and effective for the treatment of post-OLT biliary complications, has a low rate of pancreatitis and results in a durable effect.
Keywords: Biliary complications, Liver transplant, Endoscopic retrograde cholangiopancreatography, Pancreatitis
INTRODUCTION
Biliary complications are a major cause of morbidity and mortality following orthotopic liver transplantation (OLT), occurring in 11% to 38% of OLT recipients.1-3 Most common biliary complications after OLT are biliary leaks and strictures, choledocholithiasis, functional ampullary obstruction.4-6 Usually, during OLT the biliary tract is reconstructed using a duct-to-duct anastomosis, such as choledochocholedochostomy (CCS) or hepaticocholedochostomy, or, less frequently, by Roux-en-Y hepaticojejunostomy. The biliary drainage is the Achilles heel of OLT and biliary strictures occur in 4% to 13% of patients after OLT surgery.1-3 These strictures are categorized as either anastomotic or nonanastomotic. Technical problems are the most frequent cause of anastomotic strictures (size mismatch between the donor and recipient ducts) which represent more than 80% of post-OLT biliary strictures.7-9 Nonanastomotic biliary strictures are mainly caused by ischemia due to hepatic artery thrombosis and prolonged graft cold ischemia time.10 Less frequent causes of nonanastomotic biliary strictures are blood type incompatibility, chronic rejection, recurrent disease and cytomegalovirus infection.11-13
Despite the lack of large, prospective, randomized studies, endoscopic retrograde cholangiopancreatography (ERCP) is the preferred diagnostic and therapeutic procedure of choice in patients with duct-to-duct anastomosis; however, its long-term impact on morbidity and mortality rates has not been fully established due to the relatively short follow-up.
Moreover, low post-ERCP complication rates in OLT patients including pancreatitis, bleeding, stent migration, bile leaks and infection have been reported in prior studies (2% to 6%)14-25 confirming the safety of such endoscopic procedure in this particular subset of patients; however, this conclusion was drawn without adequate control groups. The motivation for the present study also stems from a previous pilot study26 where we found a lower rate of post-ERCP pancreatitis in our OLT recipients compared with the whole cohort of patients that underwent ERCP and a higher bleeding rate. Our study was planned with two main aims. First, to verify whether the discrepancy regarding post-ERCP pancreatitis and bleeding rates was due to different indications and technical execution. To this purpose we compared the OLT population with a non-OLT control group of patients who underwent ERCP in our Institution, well matched for baseline demographic features, indications and technical approach.
Second, to address the issue of the long-term efficacy of ERCP in OLT patients with biliary complications we conducted a prolonged follow-up analysis on all OLT patients at our center with biliary complications who underwent ERCP.
MATERIALS AND METHODS
1. OLT cohort definition
We retrospectively reviewed the medical, transplant clinic, endoscopy and radiology records of all adult recipients of OLT at the Liver Transplant Unit, Molinette Hospital, Torino, Italy, since October 1990 up to December 2007. The number of patients referred for ERCP and indication for the procedure was recorded. The indications for performing an ERCP were based on the history, radiological data, laboratory data, and histologic data showing a cholestatic pattern in the absence of cellular rejection. A liver biopsy was performed in all patients before ERCP. All ERCP procedures were performed by a pool of experienced biliary endoscopists (>2,500 career ERCPs with a work-load of 360 ERCPs annually).
2. Control cohort definition
Control subjects (n=188) were retrospectively identified among non-OLT patients who underwent ERCP, at the same hospital by the same endoscopists, matched 2:1 to OLT patients for age (±5 years), gender, date of ERCP (±12 months), indications, type of therapeutic intervention, and baseline risk factors for post-ERCP pancreatitis. In particular, patients with oncologic indications to ERCP were not considered; we included only patients with biliary stricture caused by surgical procedures (i.e., post-cholecystectomy complications).
3. Complications and efficacy of ERCP
The types of biliary complications diagnosed during ERCP and their managements were systematically retrieved from medical records both for OLT and non-OLT patients using a standardized form. Specific endoscopic therapies, success rate and the biliary outcomes were assessed. Endoscopic success for bile leaks was defined as the resolution of the leak on repeat cholangiography, solely utilizing endoscopic techniques and without the need for subsequent percutaneous or surgical procedures. Endoscopic success for biliary strictures was defined similarly as resolution of the source of obstruction on repeat cholangiography and/or improvement in cholestatic liver tests, solely using endoscopic procedures, and without the need for additional interventional radiology or surgical treatment. Partial resolution was defined by a requirement for only one subsequent therapeutic endoscopic intervention during follow-up.
Procedure-related complications were recorded; regarding post-ERCP pancreatitis, patients were classified as high risk if they had any of the high-risk parameters reported by Freeman and Guda.27 Patients were classified as low risk if the primary indication of ERCP was biliary stone, stricture or bile leak. Patients with these biliary indications who were female, aged <60 years or had pancreatic injection were still retained in the low-risk category; however, we could not assess post-ERCP pancreatitis according to the difficulty of common bile duct cannulation (number of attempts) or the unintentional pancreatic duct cannulation because not described in the endoscopy records. The definition of pancreatitis and grading of its severity were based on consensus criteria.28 Post-ERCP pancreatitis was diagnosed when new-onset or increased abdominal pain caused a prolonged hospital stay of a planned admission of an inpatient and was associated with a serum amylase level increase at least 3-fold above normal at approximately 18 hours after the procedure. The severity was graded as "mild" for those patients with up to 3 additional hospital days, "moderate" for those staying between 4 to 10 days, and "severe" for those who spent more than 10 days or any of the following occurred: hemorrhagic pancreatitis, pancreatic necrosis, pancreatic pseudocyst or the need for percutaneous drainage or surgery.
Bleeding was defined as clinical evidence of hemorrhage with a decrease in haemoglobin greater than 2 g/dL within 10 days from ERCP and the need for endoscopic or other method of obtaining hemostasis.
Cholangitis was diagnosed with the presence of fever, chills, elevated liver enzymes, and/or positive blood culture within 48 hours after the procedure.
4. OLT cohort follow-up
All the patients were followed up with a standardized protocol. After OLT, the patients visited the outpatients clinics at our institutions every 1-6 months and were evaluated with blood examinations and abdominal ultrasonography; other imaging modalities (i.e., computer tomography, magnetic resonance cholangio-pancreatography) or liver histologic assessment were requested if necessary. Follow-up data were obtained from the outpatient medical charts in May 2010.
Given that the control group was formed just to compare the post-ERCP complications rate between two different populations (OLT and non-OLT patients) with similar indications to ERCP, data about the long-term outcome of the non-OLT cohort were not considered.
5. Statistical analysis
To compare the risk of ERCP related complications between OLT and non-OLT cohorts we used a conditional logistic regression model to allow a matched comparison within each strata of patients. In total 94 OLT patients and 188 non-OLT matched controls (1:2 ratio) were analyzed. A ratio higher than 1:2 was considered inefficient, because only little statistical power is gained by further increasing this ratio.
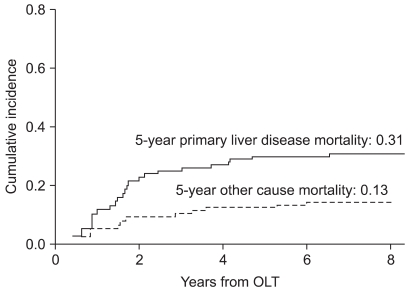
Estimates of the cumulative incidence of cause-specific death (liver disease-related, ERCP-related or other) were calculated for OLT subjects. Since the time of the event was observed incompletely, due to left truncation where early deaths were missed, we applied the cumulative incidence method described by Meister and Schaefer,29 combining corrections for left truncation and competing risks.
RESULTS
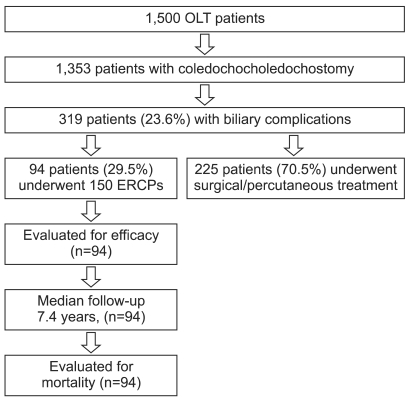
During the period considered, 1,500 patients underwent 1,638 OLTs at our institution with 1,353 (82.6%) undergoing a CCS; all patients who underwent ERCP had CCS. Of 1,353 patients with a CCS, 319 (23.6%) developed biliary complications and 94 (29.5%) underwent ERCP; the remaining 225 patients (70.5%) had a surgical or percutaneous approach, due to surgeon's decision (Fig. 1). Patients' baseline demographic features and indications to ERCP are reported in Table 1.
Fig. 1.
Flow chart of the OLT cohort.
OLT, orthotopic liver transplantation; ERCP, endoscopic retrograde cholangiopancreatography.
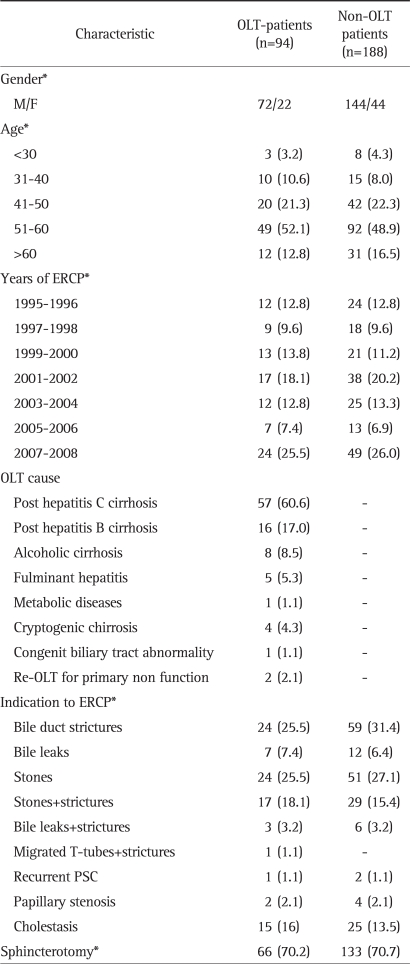
Table 1.
Baseline Demographic Features and ERCP Characteristics of the Patients by Matched Groups
Data are presented as number (%).
ERCP, endoscopic retrograde cholangiopancreatography; OLT, orthotopic liver transplantation.
*Matching variables.
In some cases (39 patients, 41.5%) more than one ERCP session was needed, so the overall number of ERCP sessions was 150. It was not possible to complete the diagnostic or therapeutic session due to technical/anatomic difficulties with inability to obtain a deep biliary cannulation in 14/150 (9.3%) ERCPs.
Out of 94 patients, 15 (15.9%) showed no alteration of the biliary tract; the majority of them (8, 53.3%) were referred to ERCP for cholestasis without radiological abnormalities.
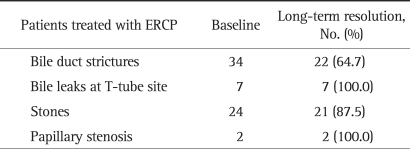
Patients with anastomotic strictures with or without concomitant bile leaks and/or stones (Table 1) were usually treated utilizing 1-5 ERCP procedures over a median of 12 weeks (range, 0 to 18). Stricture was dilated with Boston-Microvasive balloon dilators in a sequential manner followed by stent placement. Every attempt was made to place increasing number of stents (up to a maximum of 3×10 Fr stents). At the beginning of the OLT experience at our institution, the policy was to manage the anastomotic biliary obstructions percutaneously or surgically; for this reason, only 34 of 45 (75%) patients with biliary strictures were treated endoscopically: 5 endoscopic sessions in 3 patients, 4 in 4, 3 in 7, and 2 in 13 until the complete resolution of the stricture was obtained. Seven patients underwent only one endoscopic procedure. In 22 of 34 (64.7%) of these patients the ERCP was curative and no stenotic relapse was observed over the long term; a partial resolution was obtained in 6 patients (17.6%) but all of them needed surgery during the follow-up due to stricture recurrence. In the remaining 6 patients without any endoscopic benefit, all 6 had duct-to-duct mismatches; they underwent radiological (percutaneous biliary dilation) or surgical procedures (hepaticojejunostomy). Technical factors (number of ERCPs performed, number of stents placed, balloon size, number of days stents in place) possibly associated with outcome were evaluated by univariate and multivariate analysis and no significant differences were found. The overall long-term outcome of OLT patients who underwent at least one endoscopic therapeutic session is reported in Table 2.
Table 2.
Long-Term Outcome of Biliary Complications Treated by ERCP in OLT Patients
ERCP, endoscopic retrograde cholangiopancreatography; OLT, orthotopic liver transplantation.
Most biliary leaks occurred at the T-tube site (7/10, 70%) and were treated with sphincterotomy and biliary stent placement. Biliary leak resolution was confirmed a median of 7 weeks (range, 4 to 12) after the initial ERCP during repeat cholangiography: all patients were successfully treated endoscopically and none required percutaneous or surgical interventions; the remaining 3 were peri-anastomotic bile leaks with anastomotic biliary stricture which were treated by surgery as per decision of the surgical team.
Among the patients with biliary stones, 21/24 (87.5%) were managed successfully with biliary sphincterotomy and endoscopic extraction of stones. Similarly, the two patients with papillary stenosis were treated successfully with sphincterotomy.
The only patient with primary sclerosing cholangitis (PSC) recurrence was re-transplanted.
Among non-OLT patients, 25/188 (13.2%) did not show any biliary alteration: all of them were referred to ERCP for unexplained cholestasis; 94/188 (50%) showed post-cholecystectomy biliary strictures with or without stones/bile leaks: ERCP was completely successful in 54 (57.4%) and partially successful in 9 (9.5%). The remaining 29 patients were treated by radiological or surgical procedures. Of 67 patients with biliary stones, post-surgery bile leaks or papillary stenosis, 56 (83.5%) obtained a complete resolution and 11 (16.5%) underwent surgery. Two patients with PSC had no benefit from the endoscopic procedure.
1. Safety
Baseline demographic characteristics of OLT and non-OLT patients are reported in Table 1. OLT patients and non-OLT control patients are similar in matching variables, as expected for successful matching, as shown in Table 1.
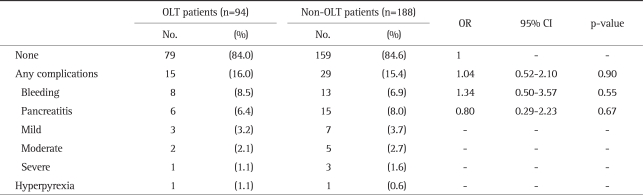
Table 3 reports the distribution of complications by group. The overall complications' incidence is similar across groups (odds ratio [OR], 1.04; 95% confidence interval [CI], 0.52 to 2.10). Neither the hypothesis of an increased overall probability of post-ERCP bleeding (OR, 1.34; 95% CI, 0.50 to 3.57) nor the hypothesis of a decreased probability of post-ERCP pancreatitis (OR, 0.80; 95% CI, 0.29 to 2.23) for OLT vs non-OLT patients seems to be supported by study results.
Table 3.
Comparison of ERCP Complications between OLT and Non-OLT Matched Patients by Conditional Logistic Regression
ERCP, endoscopic retrograde cholangiopancreatography; OLT, orthotopic liver transplantation; OR, odds ratio; CI, confidence interval.
Post-ERCP bleeding was observed in 21 patients (7.4%) and occurred only in those who underwent sphincterotomy (199/282, 70.5%). Fourteen bleeding episodes were seen during the procedure and 7 were delayed (1 to 3 days after); all of them required epinephrine injection and/or haemoclip placement with a successful outcome.
Among OLT patients, none of them showed a cirrhotic relapse at the moment of papillotomy and coagulation parameters (INR and platelets count) were normal in all of them.
2. Follow-up
Of the 94 patients included in this study, none was lost to follow-up; 60 patients (63.8%) were still alive at May 2010 with a median follow-up from OLT of 9.9 years and from first ERCP of 7.4 years. Mortality was due to the recurrence of primary liver disease in 21/34 (61.7%), in 13/34 (38.3%) was due to other causes not related to post-OLT biliary complications: 5 had fatal cardiovascular diseases, 3 bacterial infections with sepsis, 3 multiorgan failure, 2 de novo malignancies (Fig. 2). Interestingly, none of the patients who underwent curative procedures (surgery, PTC, ERCP) for their initial biliary problems showed biliary complications again during the follow-up.
Fig. 2.
Cumulative incidences of primary liver disease-related death (solid line) and other causes of death (dashed line).
OLT, orthotopic liver transplantation.
In particular none of the 22 patients with anastomotic stricture who obtained a complete resolution by therapeutic ERCP showed a recurrence of the stricture over the long term.
DISCUSSION
Despite the lack of large, prospective, randomized studies, ERCP plays a primary role in the management of biliary complications after OLT. The success rates of ERCP reported by several retrospective studies14-23 and two prospective studies24,25 support an endoscopic approach as the first line therapy of post-OLT biliary complications. However, the vast majority of these studies report relatively short (12 to 54 months) follow-up periods; longer follow-up is crucial to ensure that success rates are durable and that successful endoscopic procedures have a long-term impact on morbidity and mortality rates.
Our data show that more than 90% of patients with post-OLT biliary stones or biliary leaks without biliary strictures are successfully treated by ERCP. The endoscopic success rate is lower among patients with post-OLT biliary strictures (64.7%) but is similar to that previously reported by other studies.19,21,30 What is new in this study is the evidence that the endoscopic efficacy is durable over the long-term (median follow up, 7.4 years) with no biliary recurrences throughout the follow-up. This observation is particularly interesting with regard to anastomotic strictures: long-term failure did not occur in any patient. Similar data were obtained and reported by Morelli et al.18 with smaller series (22 patients) and shorter follow-up (54 months); Graziadei et al.25 reported a long-term endoscopic success of 77% in 65 patients with anastomotic strictures followed-up for 39.8 months.
One main objective of our study was the evaluation of safety of ERCP in OLT patients; most of previous studies14-25 reported low rates of ERCP-related complications (2% to 9%) despite the frequent use of potentially harmful interventions (papillotomy, biliary dilation, multiple stent insertion). In particular, the rate of post-ERCP pancreatitis was low with a nearly absent mortality; in a previous report,26 we showed a significant lower percentage of post-ERCP pancreatitis among OLT patients compared with non-OLT patients. Moreover, of the 6 patients with pancreatitis only one had a severe outcome. This observation prompted us to design a careful matched cohort study in order to establish whether this discrepancy was simply due to baseline differences between the two populations or to an unrecognized protective factor in the transplanted group (i.e., immunosuppressive drugs). This hypothesis was not trivial as many anti-rejection drugs may inhibit the release of cytokines which are involved in the early local and late systemic inflammation during the onset of acute pancreatitis.31-34 However, when compared with a well-matched control group, post-ERCP pancreatitis risk among OLT patients was not significantly different both in quantity and in quality suggesting that biliary complications treated by ERCP represent a low risk for acute pancreatitis. Conversely, the apparently higher rate of bleeding episodes found among OLT patients (26) was no longer confirmed when compared with the control group.
Results of the long-term follow-up show that mortality was mainly due to the recurrence of primary liver disease and no one died for causes related to post-OLT biliary complications. Our data are similar to those reported by other Authors.15,18,25 Morelli and co-workers18 reported no ERCP-related mortality, and Rizk et al.15 and Graziadei et al.25 showed that patient and graft survival did not differ significantly in the patients with anastomotic biliary strictures treated by ERCP compared with patients without strictures.
Our study does have a potential methodological weakness: of 45 patients with post-OLT biliary stricture shown by ERCP, only 34 were endoscopically treated because our Liver Transplant Center has not always used therapeutic ERCP in the management of biliary strictures after OLT, particularly in the early nineties. Despite evidence to the contrary,3,35,36 many centers continue to manage the biliary complications percutaneously or surgically. However, age, sex, type of stricture and risk factors did not differ between the endoscopically treated group and the percutaneously/surgically treated group.
In conclusion, therapeutic ERCP leads to long-term efficacy in the majority of OLT patients with biliary complications. Procedure-related adverse events are relatively uncommon and similar to those observed in a comparable group of non-OLT patients.
ACKNOWLEDGEMENTS
The study received a grant of 6,000 Euros by the School of Medicine, University of Turin, Italy.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Lerut J, Gordon RD, Iwatsuki S, et al. Biliary tract complications in human orthotopic liver transplantation. Transplantation. 1987;43:47–51. doi: 10.1097/00007890-198701000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stratta RJ, Wood RP, Langnas AN, et al. Diagnosis and treatment of biliary tract complications after orthotopic liver transplantation. Surgery. 1989;106:675–683. [PubMed] [Google Scholar]
- 3.Rerknimitr R, Sherman S, Fogel EL, et al. Biliary tract complications after orthotopic liver transplantation with choledochocholedochostomy anastomosis: endoscopic findings and results of therapy. Gastrointest Endosc. 2002;55:224–231. doi: 10.1067/mge.2002.120813. [DOI] [PubMed] [Google Scholar]
- 4.Van Thiel DH, Fagiuoli S, Wright HI, Rodriguez-Rilo H, Silverman W. Biliary complications of liver transplantation. Gastrointest Endosc. 1993;39:455–460. doi: 10.1016/s0016-5107(93)70131-5. [DOI] [PubMed] [Google Scholar]
- 5.Langnas AN, Marujo W, Stratta RJ, Wood RP, Shaw BW., Jr Vascular complications after orthotopic liver transplantation. Am J Surg. 1991;161:76–82. doi: 10.1016/0002-9610(91)90364-j. [DOI] [PubMed] [Google Scholar]
- 6.Branch MS, Ciaccia D. Disorders of the biliary tree related to liver transplantation. In: DiMarino A, Benjamin S, editors. Gastrointestinal diseases: an endoscopic approach. Massachusetts: Blackwell Science; 1997. p. 918. [Google Scholar]
- 7.Testa G, Malagò M, Broelseh CE. Complications of biliary tract in liver transplantation. World J Surg. 2001;25:1296–1299. doi: 10.1007/s00268-001-0113-5. [DOI] [PubMed] [Google Scholar]
- 8.Verdonk RC, Buis CI, Porte RJ, et al. Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl. 2006;12:726–735. doi: 10.1002/lt.20714. [DOI] [PubMed] [Google Scholar]
- 9.Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy. 2005;37:857–863. doi: 10.1055/s-2005-870192. [DOI] [PubMed] [Google Scholar]
- 10.Sanchez-Urdazpal L, Gores GJ, Ward EM, et al. Ischemic-type biliary complications after orthotopic liver transplantation. Hepatology. 1992;16:49–53. doi: 10.1002/hep.1840160110. [DOI] [PubMed] [Google Scholar]
- 11.Gugenheim J, Samuel D, Reynes M, Bismuth H. Liver transplantation across ABO blood group barriers. Lancet. 1990;336:519–523. doi: 10.1016/0140-6736(90)92082-s. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig J, Wiesner RH, Batts KP, Perkins JD, Krom RA. The acute vanishing bile duct syndrome (acute irreversible rejection) after orthotopic liver transplantation. Hepatology. 1987;7:476–483. doi: 10.1002/hep.1840070311. [DOI] [PubMed] [Google Scholar]
- 13.Waldman WJ, Knight DA, Adams PW, Orosz CG, Sedmak DD. In vitro induction of endothelial HLA class II antigen expression by cytomegalovirus-activated CD4+ T cells. Transplantation. 1993;56:1504–1512. doi: 10.1097/00007890-199312000-00043. [DOI] [PubMed] [Google Scholar]
- 14.O'Connor HJ, Vickers CR, Buckels JA, et al. Role of endoscopic retrograde cholangiopancreatography after orthotopic liver transplantation. Gut. 1991;32:419–423. doi: 10.1136/gut.32.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rizk RS, McVicar JP, Emond MJ, et al. Endoscopic management of biliary strictures in liver transplant recipients: effect on patient and graft survival. Gastrointest Endosc. 1998;47:128–135. doi: 10.1016/s0016-5107(98)70344-x. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz DA, Petersen BT, Poterucha JJ, Gostout CJ. Endoscopic therapy of anastomotic bile duct strictures occurring after liver transplantation. Gastrointest Endosc. 2000;51:169–174. doi: 10.1016/s0016-5107(00)70413-5. [DOI] [PubMed] [Google Scholar]
- 17.Mosca S, Militerno G, Guardascione MA, Amitrano L, Picciotto FP, Cuomo O. Late biliary tract complications after orthotopic liver transplantation: diagnostic and therapeutic role of endoscopic retrograde cholangiopancreatography. J Gastroenterol Hepatol. 2000;15:654–660. doi: 10.1046/j.1440-1746.2000.02198.x. [DOI] [PubMed] [Google Scholar]
- 18.Morelli J, Mulcahy HE, Willner IR, Cunningham JT, Draganov P. Long-term outcomes for patients with post-liver transplant anastomotic biliary strictures treated by endoscopic stent placement. Gastrointest Endosc. 2003;58:374–379. doi: 10.1067/s0016-5107(03)00011-7. [DOI] [PubMed] [Google Scholar]
- 19.Thuluvath PJ, Atassi T, Lee J. An endoscopic approach to biliary complications following orthotopic liver transplantation. Liver Int. 2003;23:156–162. doi: 10.1034/j.1600-0676.2003.00823.x. [DOI] [PubMed] [Google Scholar]
- 20.Mata A, Bordas JM, Llach J, et al. ERCP in orthotopic liver transplanted patients. Hepatogastroenterology. 2004;51:1801–1804. [PubMed] [Google Scholar]
- 21.Solmi L, Cariani G, Leo P, Miracolo A, Nigro G, Roda E. Results of endoscopic retrograde cholangiopancreatography in the treatment of biliary tract complications after orthotopic liver transplantation: our experience. Hepatogastroenterology. 2007;54:1004–1008. [PubMed] [Google Scholar]
- 22.Shastri YM, Hoepffner NM, Akoglu B, et al. Liver biochemistry profile, significance and endoscopic management of biliary tract complications post orthotopic liver transplantation. World J Gastroenterol. 2007;13:2819–2825. doi: 10.3748/wjg.v13.i20.2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pasha SF, Harrison ME, Das A, et al. Endoscopic treatment of anastomotic biliary strictures after deceased donor liver transplantation: outcomes after maximal stent therapy. Gastrointest Endosc. 2007;66:44–51. doi: 10.1016/j.gie.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 24.Morelli G, Fazel A, Judah J, Pan JJ, Forsmark C, Draganov P. Rapid-sequence endoscopic management of posttransplant anastomotic biliary strictures. Gastrointest Endosc. 2008;67:879–885. doi: 10.1016/j.gie.2007.08.046. [DOI] [PubMed] [Google Scholar]
- 25.Graziadei IW, Schwaighofer H, Koch R, et al. Long-term outcome of endoscopic treatment of biliary strictures after liver transplantation. Liver Transpl. 2006;12:718–725. doi: 10.1002/lt.20644. [DOI] [PubMed] [Google Scholar]
- 26.Sanna C, Saracco GM, Reggio D, et al. Endoscopic retrograde cholangiopancreatography in patients with biliary complications after orthotopic liver transplantation: outcomes and complications. Transplant Proc. 2009;41:1319–1321. doi: 10.1016/j.transproceed.2009.03.086. [DOI] [PubMed] [Google Scholar]
- 27.Freeman ML, Guda NM. Prevention of post-ERCP pancreatitis: a comprehensive review. Gastrointest Endosc. 2004;59:845–864. doi: 10.1016/s0016-5107(04)00353-0. [DOI] [PubMed] [Google Scholar]
- 28.Tarnasky PR, Palesch YY, Cunningham JT, Mauldin PD, Cotton PB, Hawes RH. Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in patients with sphincter of Oddi dysfunction. Gastroenterology. 1998;115:1518–1524. doi: 10.1016/s0016-5085(98)70031-9. [DOI] [PubMed] [Google Scholar]
- 29.Meister R, Schaefer C. Statistical methods for estimating the probability of spontaneous abortion in observational studies--analyzing pregnancies exposed to coumarin derivatives. Reprod Toxicol. 2008;26:31–35. doi: 10.1016/j.reprotox.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Shah JN, Ahmad NA, Shetty K, et al. Endoscopic management of biliary complications after adult living donor liver transplantation. Am J Gastroenterol. 2004;99:1291–1295. doi: 10.1111/j.1572-0241.2004.30775.x. [DOI] [PubMed] [Google Scholar]
- 31.Grewal HP, Kotb M, el Din AM, et al. Induction of tumor necrosis factor in severe acute pancreatitis and its subsequent reduction after hepatic passage. Surgery. 1994;115:213–221. [PubMed] [Google Scholar]
- 32.Hughes CB, Gaber LW, Kotb M, Mohey el-Din AB, Pabst M, Gaber AO. Induction of acute pancreatitis in germ-free rats: evidence of a primary role for tumor necrosis factor-alpha. Surgery. 1995;117:201–205. doi: 10.1016/s0039-6060(05)80086-8. [DOI] [PubMed] [Google Scholar]
- 33.Vaccaro MI, Ropolo A, Grasso D, et al. Pancreatic acinar cells submitted to stress activate TNF-alpha gene expression. Biochem Biophys Res Commun. 2000;268:485–490. doi: 10.1006/bbrc.2000.2151. [DOI] [PubMed] [Google Scholar]
- 34.Norman J, Franz M, Messina J, et al. Interleukin-1 receptor antagonist decreases severity of experimental acute pancreatitis. Surgery. 1995;117:648–655. doi: 10.1016/s0039-6060(95)80008-5. [DOI] [PubMed] [Google Scholar]
- 35.Pfau PR, Kochman ML, Lewis JD, et al. Endoscopic management of postoperative biliary complications in orthotopic liver transplantation. Gastrointest Endosc. 2000;52:55–63. doi: 10.1067/mge.2000.106687. [DOI] [PubMed] [Google Scholar]
- 36.Morelli J, Mulcahy HE, Willner IR, et al. Endoscopic treatment of post-liver transplantation biliary leaks with stent placement across the leak site. Gastrointest Endosc. 2001;54:471–475. doi: 10.1067/mge.2001.117762. [DOI] [PubMed] [Google Scholar]