Abstract
This article emphasizes on the laboratory investigations that may play a significant role in the prompt management of the patient. Hence, other conditions where laboratory investigations will not play a major role are not included in this article. An attempt has been made to highlight certain issues wherein we can prevent inadvertent ordering of tests to minimize the burden on the overworked emergency laboratory, without compromising patient care. The conditions that will be dealt here include: acute chest pain, acute abdominal pain, road traffic injuries, acute respiratory distress, high grade fever, vomiting, loss of consciousness, poisoning and laboratory accidents, and lastly occupational exposure to potential biological hazards.
Keywords: Laboratory, management, emergencies
INTRODUCTION
The emergency department (ED) of any hospital has a very important role and showcases the managerial and administrative setup of that hospital. The conditions with which a patient will approach the ED vary from rural to urban setup and also depend on the socioeconomic structure of the locality where the hospital is situated. This article gives an overview of common conditions encountered in the ED of most of the hospitals and nursing homes, and how the laboratory medicine can help in better and timely management of the critically ill patients.
ACUTE CHEST PAIN
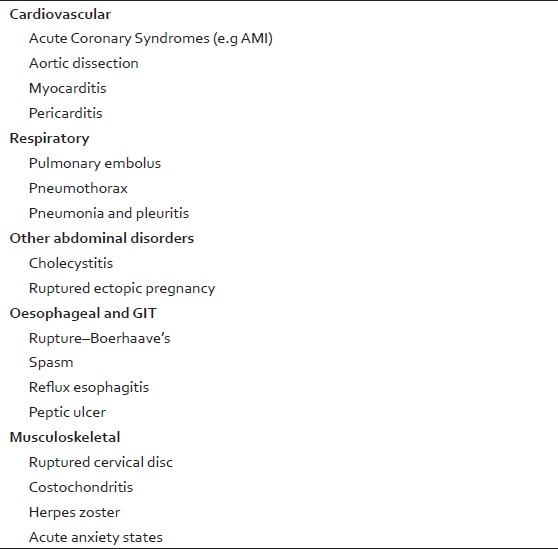
The prompt and accurate diagnosis of acute chest pain is one of the greatest challenges to the emergency physician. Among the various causes of chest pain, the commonest conditions are listed in the Table 1.
Table 1.
Common causes of acute chest pain
However, the most important condition where laboratory medicine can play a significant role is myocardial infarction. Even though other conditions may be life threatening, emergency laboratory investigations may not help much in the immediate management of these conditions and will be only of legal and academic interest. Therefore, the referring physician must use his clinical acumen to reduce the unnecessary burden on the laboratory and financial consequences. At the same time, the emergency laboratory must have the facility for the following investigations with competent person to interpret the results. The diagnosis of acute myocardial infarction (AMI) is of utmost importance to the physician in regards to the high rates of mortality and morbidity related with delay in institution of therapy. The clinical evaluation of acute chest pain is often limited by atypical symptoms and in most patients; the initial electrocardiogram (ECG) is often nondiagnostic. In such circumstances, biochemical indicators would be of choice to diagnose AMI.
TEST PROTOCOL
A strategy[1] when assessing ED patients with chest pain and nondiagnostic ECGs is to order CK-MB and troponin values on presentation in the hope of making an early diagnosis of AMI or unstable coronary syndrome. It is recognized that normal values obtained within 6 h of symptom onset do not exclude an acute coronary syndrome (ACS), and patients at low risk clinically and having normal cardiac markers could be set up for observation. After 6-8 h of symptom duration, the cardiac-specific markers are highly effective in diagnosing AMI, and such values obtained can be used more appropriately to make final decisions. But remember, at no time should results of serum marker tests outweigh ECG findings or clinical assessment of the patient's risk and stability.
Nowadays, bedside tests for cardiac troponins (cTnT and cTnI) are available and these together with myoglobin and CK-MB mass can be used in the diagnosis of patients with chest pain.
JUSTIFICATION
Troponin levels
The American College of Cardiology and the European Society of Cardiology (ACC/ESC) have redefined[2] the diagnostic criteria for myocardial infarction. Under this new definition, the measurement of cardiac troponins is the gold standard diagnostic indicator of myocardial injury in the clinical setting of myocardial ischemia. Furthermore, the ACC/American Heart Association (AHA)[3] guidelines for management of unstable angina recommend monitoring of cardiac troponin in ACS patients for differentiating unstable angina (cardiac troponin within the reference interval) and non-ST-segment-elevation MI (increased cardiac troponin). Both documents define cardiac troponin as an indicator of myocardial necrosis when the maximum concentration of either cardiac troponin T (cTnT) or cardiac troponin I (cTnI) exceeds the decision limit (defined as the 99th percentile of a reference control group) on at least one occasion during the first 24 h after the index clinical event. Furthermore, in the absence of cardiac troponin monitoring, a maximum creatine kinase MB (CKMB) value exceeding the 99th percentile of a reference control group on two successive samples or a maximum value exceeding twice the 99th percentile on one occasion is indicative of myocardial necrosis.
Cardiac troponin levels (troponin-T and troponin-I) have a greater sensitivity and specificity than CK-MB levels in detecting MI. Positive troponin levels are considered virtually diagnostic of MI, as they are without equal in combined specificity and sensitivity in this diagnosis.
They have important diagnostic as well as prognostic roles.
Serum levels increase within 3–12 h from the onset of chest pain, peak at 24–48 h, and return to baseline over 5–14 days.
Note: These markers are time sensitive and, therefore, one has to take into consideration the time of the onset of chest pain and the sample withdrawn and repeat/serial analysis of these enzymes may be required to pin point the diagnosis.
Creatine kinase level
Creatine kinase comprises three isoenzymes, including creatine kinase with muscle subunits (CK-MM), which is found mainly in skeletal muscle; creatine kinase with brain subunits (CK-BB), predominantly found in the brain; and myocardial muscle creatine kinase (CK-MB), which is found mainly in the heart.
Serial measurements[4] of CK-MB isoenzyme levels were previously the standard criterion for diagnosis of AMI. CK-MB levels increase within 3–12 h of onset of chest pain, reach peak values within 24 h, and return to baseline after 48–72 h. Levels peak earlier (wash out) if reperfusion occurs. Sensitivity is approximately 95%, with high specificity.
CK-MB is more concentrated in the myocardium (approximately 15% of the total CK), but it is also present in skeletal muscle. False-positive elevations occur in a number of clinical settings, including trauma, heavy exertion, and myopathies. The relative index calculated by the ratio of [CK-MB (mass)/total CK] μ 100 can differentiate false-positive elevations. A ratio less than three is consistent with a skeletal muscle source. Ratios more than five are cardiac origin. Ratios of three to five represent a gray zone, and often no definite diagnosis can be established.
Myoglobin levels
Urine myoglobin levels rise within 1–4 h from the onset of chest pain.
Myoglobin levels are highly sensitive but not specific, and they may be useful within the context of other studies and in early detection of MI in the ED.
Complete blood cell count
Obtain a complete blood cell count if AMI is suspected, Hb can rule out anemia as a cause of decreased oxygen supply and platelet count is required prior to giving thrombolytics.
Leukocytosis is also common, but not universal, in the setting of AMIsignifying an acute inflammatory state.
A platelet count is necessary if a IIb/IIIa agent is considered.
Chemistry profile
Potassium and magnesium levels need close monitoring in the setting of AMI.
Creatinine level is also needed prior to initiating treatment with an angiotensin-converting enzyme (ACE) inhibitor.
C-reactive protein (CRP) levels: Consider measuring CRP levels and other markers of inflammation upon presentation if an ACS is suspected.
Lipid level profile: This may be helpful if obtained upon presentation because levels can change after 12–24 h of an acute illness.
LIMITATIONS
No currently used cardiac-specific serum marker is both highly sensitive and highly specific for acute infarction within first 6 h following the onset of chest pain.
The total CK level is far too insensitive and a nonspecific test to be used to diagnose AMI. It retains its value, however, as a screening test, and serum of patients with abnormal total CK values should undergo a CK-MB mass assay. This test is highly specific, and an abnormal value (particularly when it exceeds 5% of the total CK value) at any time in a patient with chest pain is highly suggestive of AMI. However, CK-MB levels may be normal in one-fourth to half of the patients at time of presentation. Rapid serial CK-MB assessment greatly increases the diagnostic value of the assay in a timeframe suitable for ED purposes but unfortunately still misses about 10% of patients ultimately diagnosed with AMI.
The cardiac troponins are highly useful as markers of ACSs, rather than specifically of AMI, and abnormal values at any time following chest pain onset are highly predictive of an adverse cardiac event. The ED applicability of the troponins is severely limited, however, because values remain normal in most patients with acute cardiac events up to as long as 6 h following symptom onset.
Myoglobin appeared promising as a marker of early cardiac ischemia but appears to be only marginally more sensitive than CK-MB assays early after symptom onset and less sensitive than CK-MB at 8 h or more after chest pain starts. Rapid serial myoglobin assessment, however, appears highly useful as an early marker of AMI. The marker has a very narrow diagnostic window.
Other conditions in which biochemical markers may not be of much value include:
Renal failure: Cardiac troponin T level (cTnT) is commonly increased in end stage chronic kidney disease (CKD) in the absence of acute myocardial infarction.
NOVEL MARKERS
Several novel markers have been evaluated in clinical studies in recent years.
Heart-type fatty acid-binding protein (H-FABP) is proposed as an early biomarker for AMI. H-FABP[5] is a low-molecular-mass (14–15 kDa) cytoplasmic protein that, along with myoglobin, is among the earliest markers released into circulation after myocardial damage. The H-FABP content of skeletal muscle is only 10–20% of that found in cardiac muscle, whereas the skeletal muscle content of myoglobin is approximately twice that of cardiac muscle. Quantitative measurement of the serum H-FABP concentration has shown[6] to be more sensitive and specific than myoglobin for the early diagnosis of AMI.
B-type natriuretic peptides (BNP), Amino-terminal pro-B-type natriuretic peptides (NT-proBNP), and C-reactive protein (CRP) have also gained great interest and sufficient data has been gathered, justifying clinical application of these novel markers. As a consequence, BNP/NT-proBNP and CRP are mentioned in the current guidelines of the European Society of Cardiology (ESC) as appropriate biomarkers for risk stratification. NT-proBNP is a strong and independent prognostic indicator, representing a particularly strong predictor of heart failure or death. It has been recommended[6] to measure NT-proBNP on (or near) the time of admission and an elevated initial NT-proBNP concentration (value >250 ng/l) should prompt consideration of an early invasive management approach. Consideration should also be given to repeating the NT-proBNP measurement after 24–72 h and again at 3–6 months because these follow-up measurements provide more long-term prognostic information than single measures at presentation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Karras DJ, Kane DL. Serum markers in the emergency department diagnosis of acute myocardial infarction. Emerg Med Clin North Am. 2001;19:321–37. doi: 10.1016/s0733-8627(05)70186-3. [DOI] [PubMed] [Google Scholar]
- 2.JESC/ACC Committee. Myocardial infarction redefined – a consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J. 2000;21:1502–13. doi: 10.1053/euhj.2000.2305. [DOI] [PubMed] [Google Scholar]
- 3.Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee on the management of patients with unstable angina) Circulation. 2000;102:1193–209. doi: 10.1161/01.cir.102.10.1193. [DOI] [PubMed] [Google Scholar]
- 4.Young GP, Gibler WB, Hedges JR, Hoekstra JW, Slovis C, Aghababian R, et al. Serial creatine kinase-MB results are a sensitive indicator of acute myocardial infarction in chest pain patients with nondiagnostic electrocardiograms: the second Emergency Medicine Cardiac Research Group Study. Acad Emerg Med. 1997;4:869–77. doi: 10.1111/j.1553-2712.1997.tb03812.x. [DOI] [PubMed] [Google Scholar]
- 5.Okamoto F, Sohmiya K, Ohkaru Y, Kawamura K, Asayama K, Kimura H, et al. Human heart-type cytoplasmic fatty acid-binding protein (H-FABP) for the diagnosis of acute myocardial infarction. Clinical evaluation of H-FABP in comparison with myoglobin and creatine kinase isoenzyme MB. Clin Chem Lab Med. 2000;38:231–8. doi: 10.1515/CCLM.2000.034. [DOI] [PubMed] [Google Scholar]
- 6.Omland T, de Lemos JA. Amino-Terminal Pro-B-Type Natriuretic Peptides in Stable and Unstable Ischemic Heart Disease. Am J Cardiol. 2008;101:61–6. doi: 10.1016/j.amjcard.2007.11.025. [DOI] [PubMed] [Google Scholar]


