Abstract
58-year-old woman with a history of breast carcinoma presented with a bilateral ovarian tumor. On fine needle aspiration cytology, diagnosis of metastatic adenocarcinoma was made. At subsequent hysterectomy and bilateral salpingo-oophrectomy, specimen showed extensive metastatic carcinoma involving both ovaries.
Keywords: Breast, metastatic carcinoma, ovary
Introduction
The ovary is a common site of involvement for metastasis. Ovarian involvement is seen at autopsy in about 10% of cases of breast cancer. The metastasis are bilateral in approximately 80% of the cases and in approximately two-thirds of all cases, autopsy and surgical combined.[1]
The median interval between the diagnosis of breast cancer and the ovarian metastasis is 11.5 months and is related to the stage of the breast cancer. The median survival after the diagnosis of ovarian metastasis is 16 months. Lobular carcinomas, including those of signet-ring cell type, spread to the ovary more frequently than those of ductal type.[2] We report ovarian metastasis diagnosed by cytology six years after the case had been operated for infiltrating duct carcinoma.
Case Report
A 58-year-old postmenopausal woman who was operated for breast carcinoma six years back presented with bilateral ovarian mass. The histological type of breast carcinoma was infiltrating ductal cell carcinoma. On fine needle aspiration cytology (FNAC), cells were arranged in cell clusters having high nuclear-cytoplasmic ratio, moderate amount of cytoplasm, vesicular nucleus, with conspicuous nucleoli. On the basis of cytological features, it could not be categorized under any of the primary tumors of the ovary. Keeping in view the past history of breast cancer and bilaterality of the tumor, diagnosis of metastatic adenocarcinoma was given.
Hysterectomy with bilateral salpingo-oophrectomy was performed.
Gross
Endometrium, myometrium and cervix were grossly normal. The right ovary measured 4.5 × 2 × 1 cm and the left was 4.5 × 3 × 2 cm.
Outer surface of both ovaries revealed multiple nodules varying in diameter from 0.5 cm to 1 cm. Cut section of ovary showed multiple well-circumscribed white to yellow nodules of various sizes. Microscopic examination of FNAC of ovarian mass showed malignant cells in overlapping cell clusters with high nuclear cytoplasmic ratio, vesicular chromatin, and prominent nucleoli [Figure1]. Histopathology of ovary showed small cords and clusters of cells in the ovarian cortex. In some foci, a pattern of tubular glands and nests, similar to that of ductal carcinoma of breast was present and other areas showed cells in a diffuse pattern.
Figure 1.
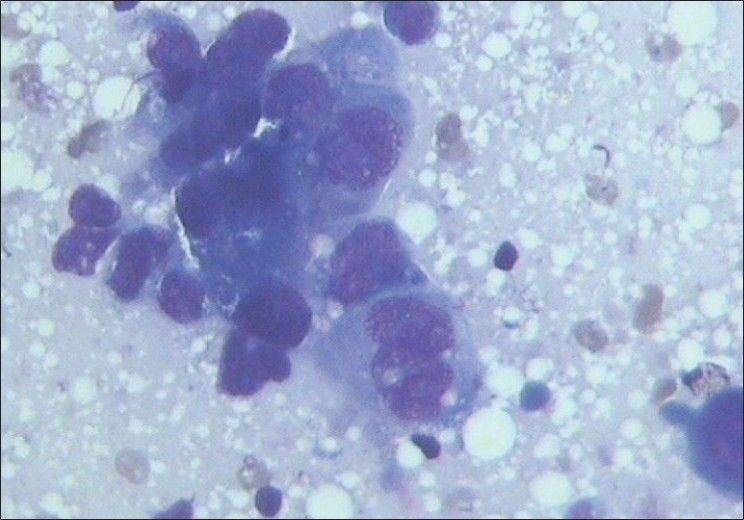
Photomicrograph of FNAC of ovarian mass showing malignant cells arranged in cluster (Giemsa, ×400)
Discussion
Metastatic neoplasms involving ovaries constitute an important group of neoplasms because the therapy for primary ovarian neoplasm is different from that used for metastatic tumors derived from other organs.[3]
The likelihood that an ovarian neoplasm on exploration of a pelvic or abdominal mass is metastatic is 6-7%. The most common site of origin includes the gastrointestinal tract (GIT) (stomach, colon, pancreas, and appendix), breast and hematopoietic system. Several gross and microscopic features suggest the metastatic nature of on ovarian neoplasm. These include bilaterality, presence of multiple nodules of the tumor, involvement of the surface and superficial cortex of the ovary, smaller tumor size, and histological features that are incompatible with a primary ovarian tumor.[4]
It is well recognized that carcinoma of breast can metastasize to any organ although distant metastases are unusual at the time of diagnosis. Metastatic disease frequently arises two to five years following diagnosis. Its likelihood is influenced by factors such as regional nodal status at presentation and histological grade. The pathological tumor type is thought to have a bearing on the sites of spread with lobular carcinoma as opposed to invasive ductal carcinoma being more commonly associated with unusual sites including the GIT and genitourinary tract.[5]
Immunohistochemical staining of ovaries showed specimen negative for ovarian tumor marker (CA-125).
Metastases in the ovary and uterus are present in up to 21% of patients according to autopsy studies. The ovaries are the most common pelvic organ to be affected although the cervix and vagina are also recognized sites of disease spread.[6]
In conclusion, when evaluating a patient with an ovarian tumor, a history of previous malignancy strongly suggests a metastatic nature. Various features supportive of metastatic tumors in the ovary are size less than 9 cm, solid structure, no omental deposits, absence of transition from benign appearing to malignant epithelium and bilateral ovarian tumor.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kiyokawa T, Young RH, Scully RE. Krukenberg tumors of the ovary: A clinicopathologic analysis of 120 cases with emphasis on their variable pathologic manifestations. Am J Surg Pathol. 2006;30:277–99. doi: 10.1097/01.pas.0000190787.85024.cb. [DOI] [PubMed] [Google Scholar]
- 2.Harris M, Howell A, Chrissohou M, Sellwood A comparison of the metastatic pattern of infiltrating lobular carcinoma and infiltrating duct carcinoma of the breast. Br J Cancer. 1984;50:23–30. doi: 10.1038/bjc.1984.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daya D, Nazerali L, Frank GL. Metastatic ovarian carcinoma of large intestinal origin simulating primary ovarian carcinoma: A clinopatholigic study of 25 cases. Am J Clin Pathol. 1992;97:751–8. doi: 10.1093/ajcp/97.6.751. [DOI] [PubMed] [Google Scholar]
- 4.Antila R, Jakanen J, Heikinheimo O. Comparison of secondary and primary ovarian malignancies reveals differences in their pre and perioperative characteristics. Gynecol Oncol. 2006;101:97–101. doi: 10.1016/j.ygyno.2005.09.046. [DOI] [PubMed] [Google Scholar]
- 5.Young RH. From Krukenberg to today: The ever present problems posed by metastatic tumors in the ovary: Part II Adv. Anat Pathol. 2007;14:149–77. doi: 10.1097/PAP.0b013e3180504abf. [DOI] [PubMed] [Google Scholar]
- 6.Tserkezoqlou A, Kontou S, Hadjieleftheriou G, Apostolikas N, Vassilomanolakis M, Sikiotis K, et al. Primary and metastatic ovarian cancer in patient with prior breast carcinoma: Pre-operative markers and treatment results. Anticancer Res. 2006;26:2339–44. [PubMed] [Google Scholar]


