Abstract
Subjects exposed to organic solvents frequently complain of respiratory symptoms. Epidemiological studies conducted in these exposed subjects with special reference to respiratory effects are very few and that too are on very small number of subjects. This paper critically reviews most of the epidemiological studies in formaldehyde induced respiratory effects and combines them through meta analysis to get global precise estimates of the respiratory risks.
A computerized bibliographic search revealed 16 epidemiological studies out of which 12 studies were considered for meta analysis. The symptoms of upper respiratory tract were more prevalent as the combined odds of exposed was 5.04 compared to controls. The pooled odds ratio for acute lower respiratory symptoms ranged between 1.85 and 2.91. The mean fall of FVC, FEV1 and FEV1/FVC was only 3.4%, 3.6% and 0.6% respectively, which was not statistically or physiologically considered significant.
Keywords: Formaldehyde, meta analysis, respiratory disorders
INTRODUCTION
Occupational exposure to formaldehyde can occur during its production and during its use in the production of end products in the governmental industry, in the building material industry and in laboratories. Several published reports, research papers and industrial experience suggest that exposure to formaldehyde is associated with adverse effects on respiratory health. Recent review of the studies[1–4] have indicated that the respiratory tract especially the upper respiratory tract is a critical target of the toxicity of airborne formaldehyde by the acute controled exposure human studies, by studies of humans exposed actually or repeatedly under occupational or residential conditions and by studies of animals exposed by inhalation for acute, intermediate and chronic durations. Regarding pulmonary function assessment studies in controlled exposure studies[5–7] in formaldehyde exposed workers during workday shift[8–12] and in repeated exposure human studies[13–19] have shown either no effects or only small and subtle effects from formaldehyde however some studies[20–21] showed small insignificant decrease in some of the lung function parameters during the works-shift. The studies considered in formaldehyde exposed subjects with reference to respiratory effects are on very small number of subjects. This paper critically review the occupationally exposed subjects due to formaldehyde and its respiratory effects and combines them quantitatively (meta analysis) to get a global precise estimate of respiratory risks. The main benefit of meta analysis will improve the power of small or inconclusive studies to answer questions and the ability to identify the sources of diversity across various type of studies
Meta analysis
The quantitative synthesis of previous research has become an important part of the scientific methods. This can only be done by statistically combining information from independent studies examining the same question. The term applied to the techniques for the aggregation and synthesis of prior research is known as meta analysis. The goal of the methodology is to bring together results of different studies, re-analyze the disparate results within the context of their common end points, increase in sensitivity of the analysis to detect the presence of exposure effect and provide a quantitative precise estimates based on the combined data. The detailed rationale for meta analysis in medical studies has been set out elsewhere.[22–23]
MATERIALS AND METHODS
Identification and inclusion criteria of different Studies
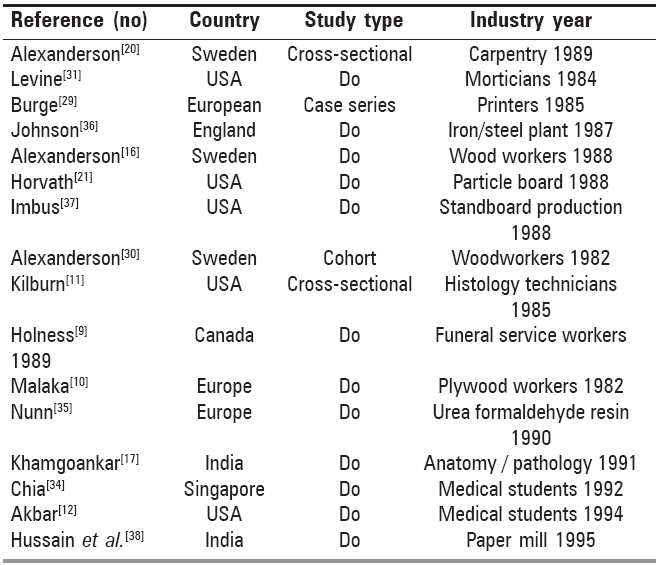
Information on the studies and references by giving key words namely occupational exposure, formaldehyde and pulmonary effects in different search engines were collected. The studies were further screened and only those have been included in meta analysis which have investigated the association between exposure to formaldehyde and respiratory outcomes (lower and upper respiratory symptoms, pulmonary function abnormalities). After thorough screening we located 16 published epidemiological studies for meta analysis. The details of these studies including author, study-type, country and type of industry are provided in Table 1. Mostly all studies were cross-sectional and exposed subjects were industrial workers. Each of the quantitative estimates were scrutinized for problems. Out of the 16 studies, four studies[11,24–26] were further dropped for nonavailability of the quantitative data of either exposed or controls subjects. Only 12 studies were considered for meta analysis. The meta analysis was performed assuming that the effects in the form of odds ratio and lung functions reported in the studies can be seen as a random sample of the effects observed in all possible studies that had met our criteria for selection of studies.
Table 1.
Summary of the epidemiological studies of respiratory diseases due to exposure to formaldehyde
Data analysis
Epi-stat software was used to calculate the individual study odds ratio by making use of the Mental-Haenszel method. Where entries in any of the 2 × 2 table were 0, log odds ratio and weights for that table were not defined, in such cases 1/2 was added to each cell before calculating odds ratio and weights.[27,28] The combined risk ratios and 95% confidence intervals were calculated as per Piegorch et al.[29] after ascertaining the homogeneity of odds ratio between different studies by Chi square statistics.[27,28] To identify potential outlier studies, a graphical display method by Mullen et al[30] was used. For studies with continuous outcome (Lung functions) the effect size was calculated as the difference in mean values between the exposed and control groups divided by standard deviation (SD) for the control group.
Mean exposed - mean control
Effect size = ------------------------------------
SD Control
The mean effect size and 95% confidence were calculated as per Abramson et al., 1995.[31]
RESULTS
Qualitative review for formaldehyde exposed studies.
Several studies have concentrated on inhalation exposure to formaldehyde and its effects on respiratory system.
-
a)
In a cross-sectional study of 186 plywood workers[10] formaldehyde exposure (avg. 1.13 ppm) was associated with increased complaints of cough, phlegm production, asthma, chronic bronchitis and colds. Decrement in FEV1/FVC ratio in exposed subjects compared to controls was significant.
-
b)
A study of carpentry shop workers[24] found an increased prevalence of upper airway irritation compared to controls with typical symptoms including burning sensation in the eyes and throat along with chest tightness. Pulmonary function testing performed on each subject both prior and following work, showed a significant decrease in FEV1 and FEV1/FVC ratio.
-
c)
A study of 47 wood workers[32] exposed to formaldehyde (0.47 mg/m3) showed significantly higher complaints of upper respiratory tract (eyes, nose and throat irritation) along with chest tightness compared to those observed in controls, however acute symptoms of lower respiratory tract and chronic bronchitis did not show any association with exposure. Slight deterioration in lung functions (FEV1) was observed in exposed subjects compared to controls. A significant decrease in FEV1% was also observed in the exposed population over the five-year interval,[20] however, these decrements returned to normal after four weeks of non-exposure showing reversibility of pulmonary function impairment following cessation of exposure. No significant differences in lung functions (FVC, FEV1 and FEV1/FVC) were observed in exposed subjects compared to control group of subjects.
-
d)
In a cross-sectional study symptoms of chronic bronchitis, dyspnea, nose and throat irritation were reported more frequently by 84 funeral service workers compared to a cross-sectional study of 38 nonexposed controls.[9] The mean formaldehyde level measured was 0.36 ppm which ranged between 0.08 and 0.81 ppm. No pulmonary function changes were observed. Similar findings were observed in a cross-sectional study of morticians.[33]
-
e)
A study of spray painters exposed to acid-hardening lacquers[16] containing formaldehyde demonstrated increased symptoms of upper respiratory tract (nose and throat irritation) following a mean exposure level of formaldehyde of 0.48 mg/m3 (range 0.14-2.60 mg/cum). Lung function was decreased by 0.21 L and 0.24 L in the exposed group in FEV1 and FVC respectively compared to nonexposed control group. No change was observed post shift in the exposed workers.
-
f)
A Danish study of respiratory symptoms[25] among cabinet makers and carpenters found an increased prevalence of cough, phlegm and dyspnea among lacquerers compared to nonlacquerers. Potential exposure to other toxins limits the interpretation of association to organic solvents.
-
g)
A study of histology technicians exposed to formaldehyde and xylene observed reduction in pulmonary functions.[34] Vital capacity was significantly reduced among subjects aged 20-60 compared to control population.
-
h)
A cross-sectional study of medical students in Singapore[35] reported increased complaints of mucous membrane irritation after dissection without decrement in FVC and FEV1. The average concentration of formaldehyde was 0.74 ppm, with a peak value of 1.2 ppm.
-
i)
In an another cross-sectional study in India[17] of 148 anatomy and histopathology workers significant pulmonary function decrements, along with increased complaints of productive cough, breathlessness and chest tightness were found. The average concentration of formaldehyde was 1 ppm.
-
j)
In a study of 34 nonsmoking medical students and instructors[12] and 14 participants not exposed to formaldehyde, no significant changes were observed in lung functions (FVC, FEV1, FEV1/FVC) between the two groups, however there was a post shift decline in exposed workers in lung functions. There were also significant rise in complaints of eye, nose and throat irritation in exposed group in comparison to controls. Mean concentration of formaldehyde was 1.24 ppm, which ranged between 0.1 ppm and 2.94 ppm.
Studies on workers exposed to formaldehyde confounded by other toxins
-
a)
A cross-sectional study of 109 particle board workers (exposed) and 254 food processing workers (controls) revealed no change in base line pulmonary functions but statistically significant fall was observed across a work-shift in the exposed workers.[32] Moreover there were increased complaints of cough, phlegm production and burning sensation in the eyes, nose and throat in the exposed subjects. The mean formaldehyde concentration in the particle board facility was 0.62 ppm. The effects were possibly not only due to formaldehyde alone but the presence of respirable particles of wood dust.
-
b)
A six-year follow-up study[26] of 164 workers exposed to formaldehyde failed to establish any association with increased respiratory symptoms and impairment in lung functions. The workers were exposed to a concentration of formaldehyde ranging between 0.1 ppm and 2.00 ppm.
-
c)
In an another study for assessing the effects of formaldehyde on 78 workers from iron and steel foundry[36] were compared with 372 railway yard workers (controls). Complaints of phlegm production, breathlessness and chest tightness were found to be significantly higher in smokers among foundry workers compared to smokers in controls. Mean FEV1 was lower in foundry workers than in controls. Since the foundry workers were exposed to MDI (Methylene Diphenyl Isocyanate), phenol and silica particles along with formaldehyde, it was difficult to attribute the decrease in pulmonary functions due to formaldehyde only.
-
d)
A cross-sectional study of 176 workers in the phenol-formaldehyde-resin coated wood industry[37] found no association of cross-shift pulmonary function and formaldehyde exposure. The exposure of formaldehyde was low (≤0.05 ppm). The selection bias in studied subjects and confounding effects of wood dust exposure limits the interpretation of the data.
-
e)
In a study of workers exposed to formaldehyde in a melamine house in a security paper mill in India along with 27 controls,[38] increased symptoms of cough and dyspnea were observed in the exposed subjects compared to those in controls. Pulmonary function abnormalities were observed in 40% of the exposed subjects compared to 4.5% in controls. Lung functions were significantly lower in exposed subjects compared to unexposed controls.
Meta analysis of respiratory symptoms as outcomes
Data of respiratory symptoms (upper and lower) pertaining to all the studies considered for meta analysis in control and exposed subjects along with odds ratio are presented in Tables 2a and 2b. Lung function data in exposed and control subjects in various studies are presented in Table 3.
Table 2a.
Symptoms pertaining to lower respiratory tract in exposed and control subjects with odds ratio in different studies on exposure to formaldehyde
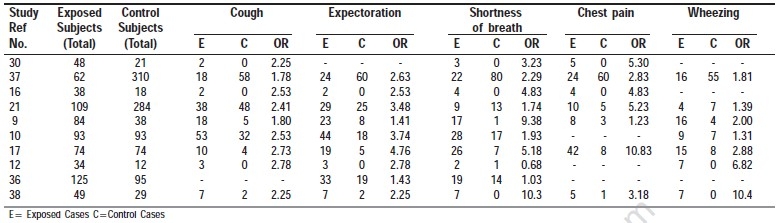
Table 2b.
Symptoms pertaining to upper respiratory tract and chronic bronchitis in exposed and control subjects with odds ratio in different studies on exposure to formaldehyde
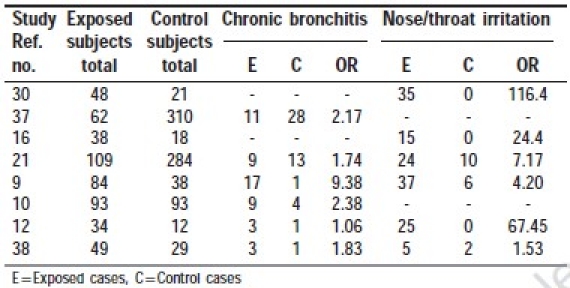
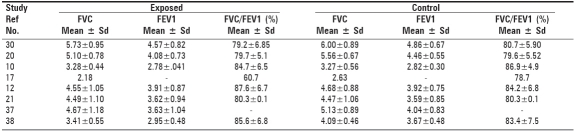
Table 3.
Lung function values reported in different studies on exposure to formaldehyde
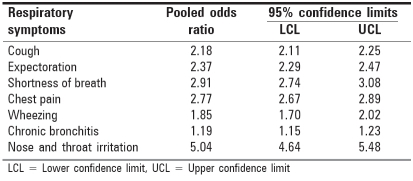
The odds ratio in most of the studies, where the workers were exposed to formaldehyde, for dry cough ranged between 1.8 and 2.8 and for productive cough it ranged between 1.41 and 4.76 [Table 2a]. The combined odds of dry cough and productive cough were 2.18 (95% CL 2.11 to 2.25) and 2.37 (95% CL 2.29 to 2.47) respectively [Table 4]. Odds of dyspnea in most of the studies ranged between 1.74 and 10.30 except in a few studies[12,36] where the odds were low [Table 2a]. Pooled estimate of the odds for shortness of breath was 2.91 with 95 per cent confidence limits from 2.74 to 3.08.
Table 4.
Pooled odds ratio (95% confidence limits) of various symptoms in different studies
For chest pain/tightness/ oppression, the studies showed increased odds ranging between 2.78 and 10.83 where in one study (9) odds was low where in some studies[10,12,36] no symptoms were reported in exposed and control populations. Overall pooled
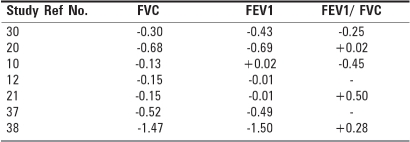
estimate of the odds was 2.77 (95% CL 2.67 to 2.89). Odds of more than two for asthmatic symptoms like wheezing were reported in four studies[9,12,17,39] and no symptom of wheezing was reported in three studies.[16,32,36] The combined odds ratio estimate was 1.85 with 95% confidence range 1.70 to 2.02 [Table 4]. Odds ratio for chronic bronchitis due to exposure to solvents of more than two was reported only in three studies.[9,10,37] In a study done by Johnson[37] the presence of methyl diphenyl- isocyanate, phenol, silica and formaldehyde were responsible for increased prevalence of chronic bronchitis and other respiratory symptoms. However, there were two studies[9,10] which showed definite association of chronic bronchitis with formaldehyde exposure however overall odds for chronic bronchitis was found to be lower (1.19). Symptoms of upper respiratory tract (irritation of eyes, nose and throat) were more prevalent in exposed than in controls almost all the studies reviewed as evidenced in Table 2b and by the pooled odds ratio of 5.04 (95% CL 4.64-5.48) [Table 4]. The effect of organic solvents exposure upon lung functions are summarized in Tables 3 and 5. Most of the studies showed fall in lung functions in exposed group compared to those in control groups but none could attain statistical significance. The mean effect size of fall in FVC was 0.34 (95% CL 0.12 to 0.57), for FEV1.0 it was 0.36 (95% CL 0.11 to 0.61) and for FEV1/FVC ratio fall was 0.06 (95% CL,-0.15-0.27) which corresponds to only 3.4 and 3.6 and 0.6% fall respectively in exposed compared to control which is neither statistically significant nor exceeds the physiologically reproducibility significance.
Table 5.
Effect size of lung functions of studies
DISCUSSION
The increased odds ratio for respiratory symptoms such as dry/productive cough, dyspnea, chest tightness indicate that workers exposed to organic solvents are prone to upper respiratory tract infections (URTI) compared to lower respiratory tract infections (LRTI) associated with insignificant decrease in spirometric variables. Most of the studies have shown no significant relationship between chronic bronchitis and other COPD cases on exposure to organic solvents.
The present study on meta analysis is based on aggregate patient data (APD) and more than 90% studies are on APD compared to individual patient data (IPD) though the later studies are considered better to summarize the results of multiple studies however the resource time and cooperation required for such studies will continue to limit its use. The statistical methods however for estimating summery effect measure are essentially the same for both the approaches. The limitations of meta analysis are thoroughly discussed by Layman et al.[39] So APD analysis continue to be the mainstay of systematic reviews utilized by US preventive service task force and by many professional societies as they are cost-effective, more frequently completed and also considered relevant and valid to editors, reviewers and readers.
The very purpose of lung functions in pulmonary medicine and clinical symptoms pertaining to lower and upper respiratory tract is to assess the level of bronchial obstruction in cases. Hence FVC and FEV1 are periodically and serially used in obstruction changes hence it provides a good diagnostic tool. However there were decrements in lung functions in exposed subjects compared to controls but these were not found to be statistically significant.
The observed FVC and FEV1 in controls [Table 3] from European descent[12,20,21,32,37] were found to higher compared to studies from Asia countries.[17,38] The differences are quite significant which may be because climatic conditions[40] and nutritional and genetic factors[41] contribute to increased lung and chest cage size. Studies[42] show that mechanical properties of the Indians have a lower VC 30 to 35% in males than lungs of a comparable European population. The anthropometric evidence suggests that those of whites of European descent for a given height have a 13.2% larger chest volume at full inspiration than blacks and this may also account for the differences in VC and FEV1 between blacks and whites.
Increased frequency of symptoms of the upper respiratory passages in formaldehyde exposed workers occurs because formaldehyde being water soluble gets dissolved in the mucous of eyes, nose and throat. It is open to discussion whether there exits a reflex mechanism in the small airway that is triggered on direct contact between formaldehyde and mucous membrane of the upper larger airways. It has been demonstrated in guinea pigs that formaldehyde causes such reflex bronchial constriction when it comes in contact with mucous membrane of the nose. It is also possible that formaldehyde may get bound to small particles of wood dust (where workers are engaged in wood industry) and be transported to the lower respiratory tract where it has greater biological effectiveness causing development of respiratory symptoms and disease and impairment in lung functions. In studies where exposure of formaldehyde occurs in the absence of any particles in the air, lung function effects have not been demonstrated. However the chronic effects on pulmonary function following long term, low level exposure to formaldehyde is due to mixed exposure and require further investigation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.American conference of Governmental Industrial Hygienists. Cincinnati, OH: 1992. ACGIH. Threshold limit values for chemical substances and physical agents and biological exposure indices. [Google Scholar]
- 2.Krivanek ND, Imbus HR. Formaldehyde - studies on irritation at low levels. Comments Toxicol. 1992;4:315–30. [Google Scholar]
- 3.Paustenbach D, Alarie Y, Kulle T. A recommended occupational exposure for formaldehyde based on irritation. J Toxicol Environ Health. 1997;50:217–63. [PubMed] [Google Scholar]
- 4.Mathur N, Rastogi SK, Srivastava AK. Occupational epidemiological studies of respiratory disorders due to exposure to organic solvents- Systematic Review with Meta Analysis. Indian J Occup Environ Med. 2001;5:118–26. [Google Scholar]
- 5.Green DJ, Sauder LR, Kulle TJ, Bascom R. Acute response to 3.0 ppm formaldehyde in exercising healthy nonsmokers and asthmatics. Am Rev Respir Dis. 1987;135:1261–6. doi: 10.1164/arrd.1987.135.6.1261. [DOI] [PubMed] [Google Scholar]
- 6.Nordman H, Keskinen H, Tuppuranen M. Formaldehyde asthma--rare or overlooked? J Allergy Clin Immunol. 1985;75:91–9. doi: 10.1016/0091-6749(85)90018-1. [DOI] [PubMed] [Google Scholar]
- 7.Sauder LR, Chatham MD, Green DJ. Acute pulmonary response to formaldehyde exposure in healthy nonsmokers. J Occup Med. 1986;28:420–4. doi: 10.1097/00043764-198606000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Bracken MJ, Leasa DJ, Morgan WK. Exposure to formaldehyde: Relationship to respiratory symptoms and function. Can J Public Health. 1985;76:312–6. [PubMed] [Google Scholar]
- 9.Holness DL, Nethercott JR. Health status of funeral service workers exposed to formaldehyde. Arch Environ Health. 1989;44:222–8. doi: 10.1080/00039896.1989.9935887. [DOI] [PubMed] [Google Scholar]
- 10.Malaka T, Kodama AM. Respiratory health of plywood workers exposed to formaldehyde. Arch Environ Health. 1982;45:288–94. doi: 10.1080/00039896.1990.10118748. [DOI] [PubMed] [Google Scholar]
- 11.Kilburn KH, Wrshaw R, Boylen CT, Johnson SJ, Seidman B, Sinclair R, et al. Pulmonary and neurobehavirol effects of formaldehyde exposure. Arch Environ Health. 1985;40:254–60. doi: 10.1080/00039896.1985.10545928. [DOI] [PubMed] [Google Scholar]
- 12.Akbar KF, Vaquerano MU, Akbar KM, Bisesi MS. Formalehyde exposure, acute pulmonary response and exposure control options in a gross anatomy laboratory. Am J Ind Med. 1994;26:61–75. doi: 10.1002/ajim.4700260106. [DOI] [PubMed] [Google Scholar]
- 13.Boysen M, Zadig E, Digernes V, Abeler V, Reith A. Nasal mucosa in workers exposed to formaldehyde: A pilot study. Br J Ind Med. 1990;47:116–21. doi: 10.1136/oem.47.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edling C, Hellquist H, Odkvist L. Occupational exposure to formaldehyde and histological changes in the nasal mucosa. Br J Ind Med. 1988;45:761–5. doi: 10.1136/oem.45.11.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garry VF, Otman L, Pleus R, Gray D. Formaldehyde in home: Some disease perspectives. Minn Med. 1980;63:107–11. [PubMed] [Google Scholar]
- 16.Alexanderson R, Hendenstierna G, Kolmodin-Hedman B. Respiratory hazards associated with exposure to formaldehyde and solvents in acid-curing paints. Arch Environ Health. 1988;43:222–7. doi: 10.1080/00039896.1988.9934937. [DOI] [PubMed] [Google Scholar]
- 17.Khamgaonkar MB, Fulare MB. Pulmonary effects of formaldehyde exposure. Indian J Chest Dis Allied Sci. 1991;33:9–13. [PubMed] [Google Scholar]
- 18.Kribel D, Sama SR, Cocanour B. Reversible pulmonary response to formaldehyde: A study of clinical anatomy students. Am Rev Respir Dis. 148:1509–15. doi: 10.1164/ajrccm/148.6_Pt_1.1509. [DOI] [PubMed] [Google Scholar]
- 19.Krazyzanowski M, Quackenboss JJ, Lebowitz MD. Chronic respiratory effects of indoor formaldehyde exposure. Environ Res. 1990;52:117–25. doi: 10.1016/s0013-9351(05)80247-6. [DOI] [PubMed] [Google Scholar]
- 20.Alexanderson R, Hendenstierna G. Pulmonary function in wood workers exposed to formaldehyde: A prospective study. Arch Environ Health. 1989;44:5–11. doi: 10.1080/00039896.1989.9935865. [DOI] [PubMed] [Google Scholar]
- 21.Horvath EP, Jr, Anderson H, Jr, Pierce WE, Hanrahan L, Wendlick JD. Effects of formaldehyde on the mucous membrane and lungs. JAMA. 1988;259:701–7. [PubMed] [Google Scholar]
- 22.Taubes G. Epidemiology faces its Limits. Science. 1995;269:164–9. doi: 10.1126/science.7618077. [DOI] [PubMed] [Google Scholar]
- 23.Partnen T. What's with epidemiologic meta-analyses? Scand J Work Environ Health. 1996;22:241–2. doi: 10.5271/sjweh.137. [DOI] [PubMed] [Google Scholar]
- 24.Burge PS, Harries MG, Lam WK, O’Brien IM, Patchett PA. Occupational asthma due to formaldehyde. Thorax. 1985;40:255–60. doi: 10.1136/thx.40.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sabore S, Olsen J. Health complaints and work conditions among lacquerers in the Danish furniture industry. Scan J Soc Med. 1979;7:97–104. doi: 10.1177/140349487900700301. [DOI] [PubMed] [Google Scholar]
- 26.Nunn AJ, Craigen AA, Darbyshire JH, Venables KM, Newman Taylor AJ. Six year follow up of lung function in men occupationally exposed to formaldehyde. Br J Ind Med. 1990;47:747–52. doi: 10.1136/oem.47.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Breslow NE, Day N. The analysis of case control studies 32. Lyon, France: IARC Scientific Publications; 1980. Statistical methods in cancer research.1. [PubMed] [Google Scholar]
- 28.Breslow NE, Day N. The analysis of cohort studies. 82. Lyon, France: IARC Scientific Publications; 1987. Statistical Methods in Cancer Research.1. [PubMed] [Google Scholar]
- 29.Piegorsch WW, Cox LH. Combining environmental information.II: Environmental epidemiology and toxicology. Environmetrics. 1996;7:309–24. [Google Scholar]
- 30.Dolan-Mullen P, Ramirez G, Groff JY. A meta-analysis of randomized trials of prenatal smoking cessation interventions. Am J Obstet Gynecol. 1994;171:1328–34. doi: 10.1016/0002-9378(94)90156-2. [DOI] [PubMed] [Google Scholar]
- 31.Abramson MJ, Puy RM, Weiner JM. Is allergen immunotherapy effective in asthma? A Meta-analysis of randomized controlled trials. Am J Respir Crit Care Med. 1995;151:969–74. doi: 10.1164/ajrccm.151.4.7697274. [DOI] [PubMed] [Google Scholar]
- 32.Alexanderson R, Hendenstierna G, Kolmodin-Hedman B. Exposure to formaldehyde: Effects on pulmonary function. Arch Environ Health. 1982;37:279–84. doi: 10.1080/00039896.1982.10667579. [DOI] [PubMed] [Google Scholar]
- 33.Levine RJ, DalCorso RD, Blunden PB, Battigelli MC. The effects of occupational exposure on the respiratory health of West Virginia morticians. J Occup Med. 1984;26:91–8. [PubMed] [Google Scholar]
- 34.Kilburm KH, Warshaw R, Thornton JC. Pulmonary function and histology technicians compared with women from Michigan: Effects of chronic low dose formaldehyde in a national sample of women. Br J Ind Med. 1989;46:468–72. doi: 10.1136/oem.46.7.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chia SE, Ong CN, Foo S, Lee HP. Medical students exposure to formaldehyde in a gross anatomy dissection laboratory. J Am Coll Health. 1992;41:115–9. doi: 10.1080/07448481.1992.9936310. [DOI] [PubMed] [Google Scholar]
- 36.Johnson AJ, Chan-Yeung M, MacLean L, Atkins E, Dybuncio A, Enarson D. Respiratory abnormalities among workers in an iron steel foundry. Br J Ind Med. 1985;42:94–100. doi: 10.1136/oem.42.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Imbus HR, Tochilin SJ. Acute effect upon pulmonary function of low level exposure to phenol-formaldehyde-resin-coated wood. Am Ind Hyg Assoc J. 1988;49:434–7. doi: 10.1080/15298668891380033. [DOI] [PubMed] [Google Scholar]
- 38.Husain T, Rastogi SK, Mathur N, Gupta BN. Respiratory responses of paper mill workers occupationally exposed to formaldehyde. Ind J Ind Med. 1995;41:2–8. [Google Scholar]
- 39.Lyman GH, Kunderer NM. The strength and limitations of meta analysis. BMC Med Res Methodol. 2005;5:1–7. doi: 10.1186/1471-2288-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Milledge JS. Vital capacity and forced expiratory volume one second in South Indian men. Indian J Chest Dis. 1965;7:95–103. [PubMed] [Google Scholar]
- 41.Cotes JE. 3rd ed. Oxford: Blackwell Scientific Publication; 1975. Lung function assessment and application in medicine. [Google Scholar]
- 42.Kamat SR, Sarma BS, Raju VR, Venkataraman C, Balkrishna M, Bhavsar RC, et al. Indian norms for pulmonary function. J Assoc Physicians India. 1977;25:531–40. [PubMed] [Google Scholar]