Abstract
Context:
Supraglottic airway devices have been used as an alternative to tracheal intubation during laparoscopic surgery.
Aims:
The study was designed to compare the efficacy of Streamlined Liner of the Pharynx Airway (SLIPA) for positive pressure ventilation and postoperative complications with the Laryngeal Mask Airway ProSeal (PLMA) for patients undergoing lower abdominal laparoscopies under general anesthesia with controlled ventilation.
Settings and Design:
Prospective, crossover randomized controlled trial performed on patients undergoing lower abdominal laparoscopic surgeries.
Methods:
A total of 120 patients undergoing lower abdominal laparoscopic surgeries were randomly allocated into two equal groups; PLMA and SLIPA groups. Number of intubation attempts, insertion time, ease of insertion, and fiberoptic bronchoscopic view were recorded. Lung mechanics data were collected 5 minutes after securing the airway, then after abdominal insufflation. Blood traces and regurgitation were checked for; postoperative sore throat and other complications were recorded.
Statistical Analysis:
Arithmetic mean and standard deviation values were calculated and statistical analyses were performed for each group. Independent sample t-test was used to compare continuous variables exhibiting normal distribution, and Chi-squared test for noncontinuous variables. P value <0.05 was considered significant.
Results:
Insertion time, first insertion success rate, and ease of insertion were comparable in both groups. Fiberoptic bronchoscopic view was significantly better and epiglottic downfolding was significantly lower in SLIPA group. Sealing pressure and lung mechanics were similar. Gastric distension was not observed in both groups. Postoperative sore throat was significantly higher in PACU in PLMA group. Blood traces on the device were significantly more in SLIPA group.
Conclusions:
SLIPA can be used as a useful alternative to PLMA in patients undergoing lower abdominal laparoscopic surgery with muscle relaxant and controlled ventilation.
Keywords: Laparoscopic surgery, proseal lma, streamlined liner of the pharynx airway, supraglottic airway devices
INTRODUCTION
Supraglottic airway devices (SGA) have been widely used as an alternative to tracheal intubation during general anesthesia.[1] They are better tolerated, with less coughing, permitting removal when patients are awake and cooperative.[2] One of the most commonly used SGAs is the laryngeal mask airway-ProSeal™ (PLMA, Laryngeal Mask Company, UK), a modified version of the classic laryngeal mask airway (LMA) with an additional channel for gastric tube placement to prevent pulmonary aspiration and a superior cuff that can provide airway sealing pressures higher than those of the classic LMA making it more suitable for surgical procedures in which the employment of classic LMA would not have been considered safe, e.g., laparoscopic surgeries, however; it is not a single-use device.[3,4]
The streamlined liner of the pharynx airway (SLIPA™; SLIPA med SA Pty Ltd Cape Town, South Africa) is a non-cuffed single-use, latex-free SGA, fabricated from soft plastic (ethylene vinyl-acetate copolymer) with an anatomically performed shape which sticks to the pharynx and palate. The body of SLIPA is shaped like a hollow boot with “toe,” “bridge,” and “heel” prominences, which is engaged in the patient's pharynx, allowing it to seal without the use of an inflatable cuff. It therefore does not require cuff inflation and extra straps to maintain a secure airway during positive pressure ventilation. Furthermore, a 50-ml empty internal space allows the removal of pharyngeal secretions, thus reducing the risk of pulmonary aspiration.[5]
Although PLMA had been compared with other airway devices[4,6] during laparoscopic surgery, there are only one comparative research[7] on SLIPA and PLMA during anesthesia for laparoscopic surgery.
The aim of this study was to compare the efficacy of a single-use SGA with noninflatable cuff (SLIPA) for efficacy of positive pressure ventilation and postoperative complications when compared with the standard reusable PLMA for patient undergoing lower abdominal laparoscopies under general anesthesia with controlled ventilation.
METHODS
The study was approved by the institutional human ethics committee (Menoufiya university hospital, Menoufiya city, Egypt), and written informed consent was obtained from all patients. Over nine months, 120 patients (American Society of Anesthesiologists Physical status I, II) scheduled for lower abdominal laparoscopic surgeries were enrolled in this study. Exclusion criteria were patients at risk for aspiration, current sore throat, known lung diseases, morbid obesity, pregnancy, and a suspected difficult airway. The physician inserting the device (one of the authors) had a minimum of 3 years experience in anesthesia and airway management with PLMAs and had used the SLIPA for more than 100 times before study. Patients were randomized into one of 2 equal groups, PLMA group and SLIPA group, with 60 patients in each group.
Modified Mallampati classification was used to evaluate the patients’ airway and the results were recorded at preanesthetic evaluation sheet. In PLMA group, size 3 was used for patients weighing below 50 kg, size 4 for those weighing between 50 and 70 kg, and size 5 for those over 70 kg. After insertion, the cuff was inflated by 20 to 30 ml of air to maintain the cuff pressure at 60 cmH2O with a hand pressure gauge (PORTEX, UK). For male in SLIPA group, size 51 was used for patients less than 165 cm in height, size 53 for those between 165 and 175 cm, and size 55 for those over 175 cm, and for female in SLIPA group, size 47 was used for patients under 155 cm in height, size 49 for those between 155 and 165 cm, and size 51 for those over 165 cm (http://www.SLIPA.com).
In the operating room, the patient was placed supine with the head in sniffing position. After attachment of cardiac monitor and preoxygenation with 100% oxygen for 3 minutes, general anesthesia was induced with midazolam 1 mg i.v. and fentanyl 2 ug.kg-1 i.v. followed within 2 minutes by propofol 2 mg.kg-1 and cisatracurium 0.15 mg.kg-1 to facilitate insertion of SGA. Ventilation was provided through a face mask with 100% oxygen until neuromuscular monitoring revealed full relaxation. The devices were inserted after being lubricated with water-soluble lubricant according to the manufacturer's instruction. Anesthesia was maintained with sevoflurane 1.5 to 2% and 60% N2O in O2 with supplementary fentanyl (50-100 μ) to maintain mean arterial blood pressure and heart rate within 20% of the baseline. Cisatracurium 0.05 mg.kg-1 was administered during surgery as required to maintain a train-of-four ratio of <25%.
Two attempts were allowed for placement of each device, with mask ventilation and oxygen between attempts, and the second attempt was made with a different size. If a secured airway was not achieved, a tracheal tube was used and the patient was excluded from the study.
Effective ventilation was defined as proper chest expansion, a square wave capnograph trace, absence of audible leak, and lack of gastric insufflations. After obtaining an effective airway, the device was connected to a circle breathing system (Primus, Drager, Lubek, Germany) and the lung was initially ventilated with a tidal volume of 8 ml.kg-1, a respiratory rate of 12 breaths per minutes, and I : E ratio of 1 : 2 in volume-controlled mode. Five minutes after securing the airway and then after abdominal insufflation, the lung mechanics were measured using the same anesthesia machine, then the tidal volume and respiratory rate were adjusted to achieve an end tidal carbon dioxide value of 35 to 40 mmHg. Pneumoperitoneum was maintained with carbon dioxide and adjusted to a pressure of 15 mmHg.
After completion of the surgery, the surgeon systematically administered 10 ml ropivacaine 0.75% in the peritoneum through the main umbilical trocar, the anesthetics were discontinued, and the residual neuromuscular block was reversed with neostigmine 0.05 mg.kg-1 and atropine 0.02 mg.kg-1, then the airway device was removed once the patient was awake.
The following data were recorded:
Number of intubation attempts.
Ease of insertion: Insertion was rated as straight forward (insertion succeeded on the first attempt and within 15 seconds), slightly difficult (insertion succeeded on the first attempt, but required more than 15 seconds), obviously difficult (more than one attempt before successful insertion).
Insertion time: The time from jaw opening to successful placement of the airway device, verified by sufficient ventilation and normal capnogram.
Maximal airway sealing pressure; measured by closing the expiratory valve of the breathing circuit and noting the pressure at which leak developed with a fixed gas flow of 3 l/min.[8]
The minimum flow rate required to keep the ascending bellows of the ventilator fully inflated.
Fiberoptic bronchoscopic view: After preoxygenation, the breathing system was disconnected and a 2-mm fiberoptic bronchoscope (Karl Storz GmbH and Co. KG, Tuttlingen, Germany) was inserted through the airway port for evaluating glottic view. The best views from the tip of the orifice of PLMA and SLIPA were graded from 1 to 4 as recommended by Cook and Cranshaw[9] as follows: 1 (only vocal cords seen), 2 (cords and/or arytenoids seen), 3 (only epiglottis seen), 4 (others are seen, e.g., LMA cuff, pharynx). In addition, epiglottic downfolding was also noted.
Gastric air insufflation, monitored by auscultation using a stethoscope positioned over the patient's stomach immediately after insertion of airway, after positioning and at the end of surgery.
Postoperative complications: At the end of surgery, the airway device was removed and evidence of blood stains or regurgitation was checked for. Patients were interviewed 30 minutes after arrival to postanesthetic care unit by anesthetist who was blind to the study, with respect to presence of sore throat (pain independent of phonation or swallowing), dysphonia (pain on phonation/altered voice), and dysphagia (difficulty or pain on swallowing). The questions were “do you have hoarseness of voice or sore throat” and “do you feel any discomfort or pain when you swallow your saliva.” If the answer was yes to any of these questions, the intensity of complaint or pain was assessed using a visual analogue scale rated from 0 to 10 (0 = no discomfort or no pain to 10 = extreme discomfort or maximal imaginable pain). Symptoms’ intensity was also rated in the ward just before leaving the hospital. Similar questions concerning postoperative upper airway discomfort were asked by the surgeons at the day 5 to 7 postoperative visit.
Statistical analysis
Distribution of baseline variables was assessed by the Shapiro-Wilk W tests. To estimate appropriate group size, we referred to SD of leak pressure of PLMA and SLIPA obtained in previous reports and found them to be within 5 cm H2O.[7,10] A sample size of 55 patients would be required to detect such a difference between the groups for a power of 90% at a significance level of 5%; hence, the sample size was increased to 60 patients each, to allow for possible failed insertion. By using SPSS software for Windows, version 11 (SPSS Inc, Chicago, IL, USA), arithmetic mean and standard deviation values for different variables were calculated and statistical analyses were performed for each group. Independent sample t-test was used to compare continuous variables exhibiting normal distribution, and Chi-squared or Fisher exact test (if data is less than 6 in each cell) for noncontinuous variables. P value <0.05 was considered significant.
RESULTS
A total of 120 patients were included in the study, of which 117 patients completed the study. There were no statistically significant differences between both groups regarding patient criteria and anesthetic details [Table 1]. The overall success rate for PLMA and SLIPA were 98% (n = 59) and 96% (n = 58), respectively. In the majority of patients, insertion of SGAD was successful on first attempt. When the first attempts failed, a second one was tried. In three patients, adequate ventilation could not be achieved with the SGADs after two attempts and tracheal tube was used.
Table 1.
Patients’ criteria and anesthetic details
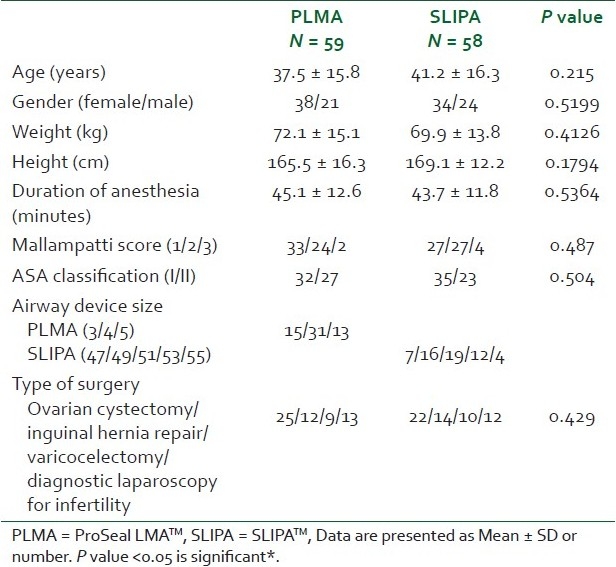
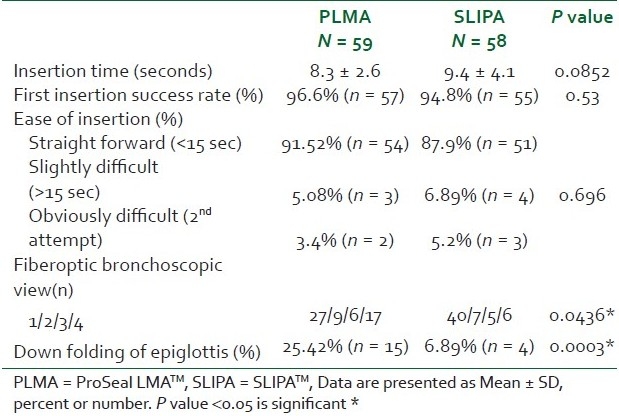
The first attempts for insertion were successful in 96.6% in PLMA group compared with 94.8% in SLIPA group. Regarding ease of insertion, it was straightforward in most of patients in both groups. In the second attempt, the airway was replaced by a smaller size in one patient in PLMA group and one patient in SLIPA group and by a larger size in one patient in PLMA group and two patients in SLIPA group. Insertion time was longer in SLIPA group compared with PLMA group. After insertion, the SLIPA enabled better fiberoptic laryngeal view and showed less epiglottic downfolding [Table 2].
Table 2.
Insertion criteria
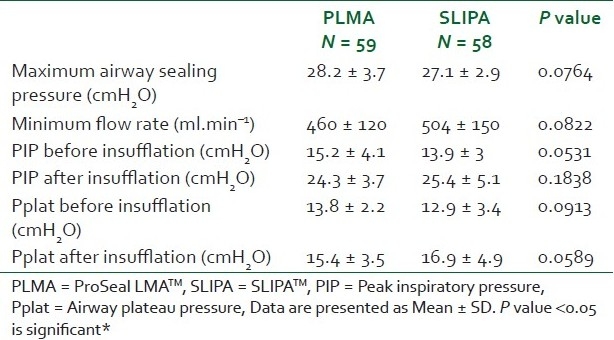
The mean value of maximum airway sealing pressure was 28.2 ± 3.7 mmHg and 27.1 ± 2.9 mmHg in the PLMA and SLIPA groups, respectively. The minimum fresh gas flow rate was below one liter in all patients. Lung mechanics data were similar in the two studied groups [Table 3].
Table 3.
Lung mechanics and airway parameters
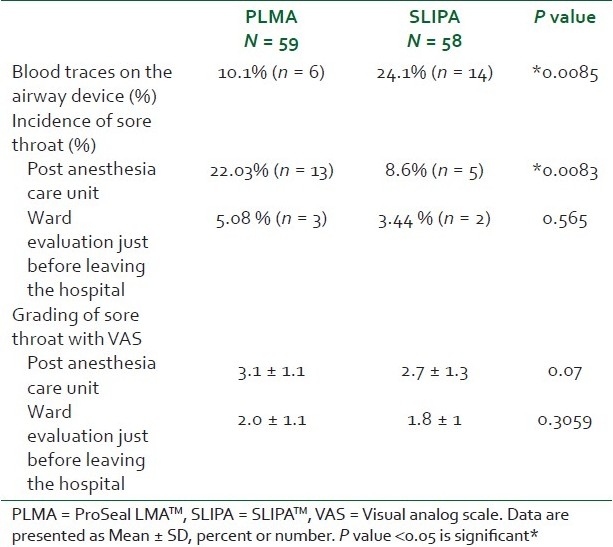
Gastric air insufflation was not observed in either group before or after surgery. Blood traces were noticed on the surface of the device in 24.1% (14 cases) in SLIPA group and in 10.1% (6 cases) of PLMA. Complains of sore throat were noticed at a significantly higher rate in PLMA. The intensity of pain (VAS) was similar in the two groups. The incidence and severity of sore throat decreased significantly before leaving the hospital compared with postanesthesia care unit in both groups. No patient complained of sore throat at the postoperative visit (5-7 days). No patient complained of dysphagia or hoarseness of voice [Table 4].
Table 4.
Complications
DISCUSSION
SGA have been safely used during laparoscopic surgery, despite the expected increased risk of aspiration due to elevated intra-abdominal pressure.[4,11] Brimacombe and Brain[12] initially included a “rule of 15” in guidelines for use of LMA during laparoscopic surgery. These “rules” were Trendelenburg tilt, <15 degree; peritoneal insufflation <15 cm.H2O; and duration of abdominal insufflation <15 minutes. In our study, the head down tilt was ≤15 degree and peritoneal insufflation pressure was preset at 15 mmHg, but the peritoneal insufflation time was not limited to 15 minutes because inadequate ventilation and gastric distension should be evident within 15 minutes of starting insufflation. If it does not occur within 15 minutes, it should not occur later, provided that anesthetic depth and muscular relaxation are adequate and the LMA-C/PLMA is not dislodged. Furthermore, Maltby et al.[13] had previously shown that the LMA-C and ETT with PPV were equally effective during laparoscopic cholecystectomy in nonobese patients, when mean peritoneal insufflation time was 47 minutes.
Successful placement of the device was achieved at the first attempt in 57 patients (96.9%) in PLMA group and in 55 patients (94.8%) in SLIPA group. Miller and Camporota[7] compared SLIPA, PLMA, and standard endotracheal intubation in 150 healthy adult females scheduled to undergo laparoscopic, gynecological procedures under general anesthesia and had a first insertion success rate of 96% and 98% for the PLMA and SLIPA, respectively. Lange et al.[14] compared classic LMA and SLIPA in ophthalmic surgery and had first insertion success rate 100% and 98%, respectively. Another study done by Miller and Light[5] on 120 female undergoing minor gynecological procedures, the first insertion success rate was 95% and 92% for the classic LMA and SLIPA, respectively. Hein et al.[15] conducted study on medical students with no experience on SLIPA or LMA and demonstrated that the first insertion success rate was 83% and 67% with overall success rate 94% and 89% for SLIPA and LMA, respectively. On the other hand, Choi et al.[10] compared SLIPA with PLMA in 60 patient undergoing surgeries under general anesthesia, the first insertion success rates for PLMA and SLIPA were 93.3% and 73.3%, respectively. We assume this variation in results to the relative experience of the anesthesiologist who has inserted the airway and the appropriate selection of the size of SLIPA airway. Correct size selection is important for successful insertion because SLIPA comes in a fixed preformed shape and six adult sizes (47-57). Many previous studies[5,7,15,16] selected SLIPA size by matching the transverse diameter of the device with the patient's thyroid cartilage; however, in our study, we used the size according to the recommendation of the manufacturer, which involved gender and height.
The insertion time was longer than 15 seconds in 12.1% of SLIPA cases and in 8.48% of PLMA cases, with no statistically significant difference. Choi et al.[10] found that the insertion of SLIPA took much longer time and was more difficult with statistically significant difference between both groups. The authors attributed this to the lack of experience and the difficulty of selecting the appropriate size of SLIPA. Miller and Camporota[7] compared SLIPA, PLMA, and standard endotracheal intubation. The insertion time was longer than 15 seconds in10% of SLIPA cases and in 18% of PLMA cases. Our results also come in agreement with Lange et al.,[14] in which the insertion of SLIPA was straightforward in 88%, slightly difficult in 10%, obviously difficult in 0% of cases, and failure in 2% of cases, compared with 90%, 8%, 2%, and 0%, respectively, in LMA group.
Airway sealing pressures and minimum flow rate were comparable in both groups with no statistically significant difference. The minimum fresh gas flow rate in the circle system is another measure of the seal's effectiveness, the seal was sufficient to allow low flow anesthesia (1 l.min-1). Similar findings had been reported in studies comparing sealing qualities of SILPA with PLMA[7,10] or SLIPA with LMA.[5,14] Brimacombe et al.[1] reported that the PLMA had a 10 cmH2O sealing pressure more than the LMA. In our study, the sealing pressure was higher than the PIP in both groups before and after abdominal insufflation. Theoretically, a SGA with a higher sealing pressure should better protect the airway from aspiration.
In our study, the SLIPA enabled better fiberoptic bronchoscopic view (81% compared with 64% in PLMA group). Giatini et al.[17] reported 60% of the LMAs as being in the appropriate location. In another study, when PLMAs and LMAs were compared, 48% of PLMAs and 74% of LMAs were reportedly successful.[18] Choi et al.[10] reported that 60% of PLMAs and 40% of SLIPAs were deemed to be appropriately inserted at fiberoptic assessment and they attributed this value to less experience regarding SLIPA insertion.
Gastric air insufflation did not occur in both groups. Similar findings had been observed in other studies.[5,7,10] Lange et al.[14] observed a higher incidence of gastroesophageal insufflation (19%) in the SLIPA than with the LMA (3%) and this may be related to the choice of the size used and the appropriate position of the device. The SLIPA sizes 47-57 are equivalent to LMA sizes 3-5.5. The authors in their study used LMA 4-6 in comparison.
No regurgitation of gastric contents was observed in both the groups. The ability of SLIPA and PLMA to protect against aspiration has been evident in previous study.[5] Also, the increase in the intra-abdominal pressure has long been known to cause a reflex increase in the tone of the lower esophageal sphincter.[4] The belief that the increase in intra-abdominal pressure during laparoscopic surgery increases the risk of gastroesophageal reflux is erroneous.[11] The reported incidence of clinically significant pulmonary aspiration in healthy patients undergoing elective surgery with classic LMA is 1 in 5 000 to 1 in 12 000.[19] This is a similar order of magnitude to the incidence with ETT or face mask in ASA I or II patients undergoing elective surgery.[4]
In our study, the incidence of sore throat was higher in PLMA (20.3%) group compared with SLIPA (10.3%) group, despite the harder appearance of SLIPA. No patient complaint of dysphonia or dysphagia in both groups. The VAS score for sore throat ranged from 1 to 5. The upper airway symptoms rapidly decreased in incidence and intensity just before leaving the hospital. No one in both groups suffered from persistent upper airway symptoms at the follow-up visit. Our results are against the results of previous studies[5,10] in which SLIPA was associated with a higher incidence of sore throat. The incidences of sore throat according to Miller and Camporota[7] were 57%, 49%, and 30% for endotracheal tubes, SLIPA, and PLMA, respectively. Our results are in accordance with a recent study by Lange et al.[14] in which fewer patients in the SLIPA group compared with those in PLMA group complained of sore throats.
Several reports associate the use of LMA with injuries of the lingual, hypoglossal, and recurrent laryngeal nerves[20,21] and to sore throat.[18,22] When the cuff is used to seal the pharynx, as in the case with PLMA, the initial cuff pressure of 60 cm water gradually increases because of N2O diffusion across the cuff wall. The intracuff pressure significantly increases over 30 minutes.[23] It is thus important to constantly monitor the intracuff pressures.[24] We did not do adjustment of the cuff pressure during surgery, because changing of the cuff pressure may cause slippage of PLMA and gas leakage.
After removal of the airway devices, SLIPAs had significantly higher incidence of blood stains than PLMAs. Reinsertion of SLIPA was associated with blood on the device in all 3 cases, suggesting that the SLIPA has the potential to be more traumatic with the second attempts. The SLIPA is made of stiffer plastic material than the PLMA, which causes more direct trauma to the oral mucosa. Insertion can be helped by an assistant holding up the jaw or by using laryngoscope or gloved left middle or index finger and thumb to create suitable space in the pharynx.[5]
Our study has some limitations. Although the investigators were experienced with both devices, they had more experience with the PLMA than with the SLIPA. The fiberoptic data were collected by the same investigator who inserted the device and was not blinded, and that might have resulted in some bias. The devices were used in nonobese patients with nondifficult airways and no underlying respiratory disorders. The results cannot be extrapolated to other groups of patients.
CONCLUSION
SLIPA effectively conforms to the perilaryngeal anatomy despite the lack of an inflatable cuff, it consistently achieves proper positioning for supraglottic ventilation, so can be used as a useful alternative to PLMA in patients undergoing lower abdominal laparoscopic surgery with muscle relaxant and controlled ventilation. Management of the airway with SLIPA was as simple as using PLMA. Fewer patients in SLIPA group complained of a sore throat, suggesting that SLIPA might increase patient comfort after surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Brimacombe J, Keller C, Boehler M, Puhringer F. Positive pressure ventilation with the ProSeal versus classic laryngeal mask airway: A randomized, crossover study of healthy female patients. Anesth Analg. 2001;93:1351–3. doi: 10.1097/00000539-200111000-00064. [DOI] [PubMed] [Google Scholar]
- 2.Akhtar TM, McMurray P, Kerr WJ, Kenny GN. A comparison of the anesthetic requirement for tolerance of laryngeal mask airway and endotracheal tube. Anaesthesia. 1992;47:668–71. doi: 10.1111/j.1365-2044.1992.tb02387.x. [DOI] [PubMed] [Google Scholar]
- 3.Brain AI, Verghese C, Strube PJ. The LMA ‘ProSeal’-a laryngeal mask with an esophageal vent. Br J Anaesth. 2000;84:650–4. doi: 10.1093/bja/84.5.650. [DOI] [PubMed] [Google Scholar]
- 4.Maltby JR, Beriault MT, Watson NC, Lieper D, Fick GH. The LMA-ProSeal is an effective alternative to tracheal intubation for laparoscopic cholecystectomy. Can J Anesth. 2002;49:857–62. doi: 10.1007/BF03017420. [DOI] [PubMed] [Google Scholar]
- 5.Miller DM, Light D. Laboratory and clinical comparisons of the Streamlined Liner of the Pharynx Airway (SLIPA) with the laryngeal mask airway. Anaesthesia. 2003;58:136–42. doi: 10.1046/j.1365-2044.2003.02962.x. [DOI] [PubMed] [Google Scholar]
- 6.Lu PP, Brimacombe J, Yang C, Shyr M. ProSeal versus the Classic laryngeal mask airway for positive pressure ventilation during laparoscopic cholecystectomy. Br J Anaesth. 2002;88:824–7. doi: 10.1093/bja/88.6.824. [DOI] [PubMed] [Google Scholar]
- 7.Miller DM, Camporota L. Advantage of ProSeal™ and SLIPA™ airways over tracheal tubes for gynecological laparoscopies. Can J Anaesth. 2006;53:188–93. doi: 10.1007/BF03021826. [DOI] [PubMed] [Google Scholar]
- 8.Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth. 1999;82:286–7. doi: 10.1093/bja/82.2.286. [DOI] [PubMed] [Google Scholar]
- 9.Cook TM, Cranshaw J. Randomized crossover comparison of ProSeal Laryngeal Mask Airway with Laryngeal Tube Sonda during anesthesia with controlled ventilation. Br J Anaesth. 2005;95:261–6. doi: 10.1093/bja/aei167. [DOI] [PubMed] [Google Scholar]
- 10.Choi YM, Cha SM, Kang H, Baek CW, Jung YH, Woo YC, et al. The clinical effectiveness of the streamlined liner of pharyngeal airway (SLIPATM) compared with the laryngeal mask airway ProSeal TM during general anesthesia. Korean J Anesthesiol. 2010;58:450–7. doi: 10.4097/kjae.2010.58.5.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones MJ, Mitchell RW, Hindocha N. Effect of increased intra-abdominal pressure during laparoscopy on the lower esophageal sphincter. Anesth Analg. 1989;68:63–5. [PubMed] [Google Scholar]
- 12.Brimacombe JR, Brain AIJ. London: W.B. Saunders Company Ltd; 1996. The laryngeal Mask Airway.A review and Practical Guide; pp. 164–6. [Google Scholar]
- 13.Maltby JR, Beriault MT, Watson NC, Fick GH. Gastric distension and ventilation during laparoscopic cholecystectomy: LMA-Classic vs.tracheal intubation. Can J Anesth. 2000;47:622–6. doi: 10.1007/BF03018993. [DOI] [PubMed] [Google Scholar]
- 14.Lange M, Smul T, Zimmermann P, Kohlenberger R, Roewer N, Kehl F. The effectiveness and patient comfort of the novel streamlined pharynx airway liner (SLIPATM) compared with the conventional laryngeal mask airway in ophthalmic surgery. Anesth Analg. 2007;104:431–4. doi: 10.1213/01.ane.0000252460.94046.7c. [DOI] [PubMed] [Google Scholar]
- 15.Hein C, Owen H, Plummer J. Randomized comparison of the SLIPA (Streamlined Liner of the Pharynx Airway) and SS-LM (Soft Seal Laryngeal Mask) by medical students. Emerg Med Australs. 2006;18:478–83. doi: 10.1111/j.1742-6723.2006.00894.x. [DOI] [PubMed] [Google Scholar]
- 16.Puri GD, Hegde HV, Jayant A. Haemodynamic and Bispectral index response to insertion of the Streamlined Liner of the Pharynx Airway (SLIPA): Comparison with the laryngeal mask airway. Anaesth Intensive Care. 2008;36:404–10. doi: 10.1177/0310057X0803600312. [DOI] [PubMed] [Google Scholar]
- 17.Gaitini L, Yanovski B, Somri M, Vaida S, Riad T, Alfery D. A comparison between the PLA Cobra and the Laryngeal Mask Airway Unique during spontaneous ventilation: A randomized prospective study. Anesth Analg. 2006;102:631–6. doi: 10.1213/01.ane.0000189098.57662.d6. [DOI] [PubMed] [Google Scholar]
- 18.Brimacombe J, Keller C. The ProSeal laryngeal mask airway: A randomized, crossover study with the standard laryngeal mask airway in paralyzed, anesthetized patients. Anesthesiology. 2000;93:104–9. doi: 10.1097/00000542-200007000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Brimacombe JR, Berry A. The incidence of aspiration associated with the laryngeal mask airway: A Meta analysis of published literature. J Clin Anesth. 1995;7:297–305. doi: 10.1016/0952-8180(95)00026-e. [DOI] [PubMed] [Google Scholar]
- 20.Brimacombe J, Clarke G, Keller C. Lingual nerve injury associated with ProSeal laryngeal mask airway: A case report and review of literature. Br J Anaesth. 2005;95:420–3. doi: 10.1093/bja/aei187. [DOI] [PubMed] [Google Scholar]
- 21.Bruce IA, Ellis R, Kay NJ. Nerve injury and laryngeal mask airway. J Laryngol Otol. 2004;118:899–901. doi: 10.1258/0022215042703741. [DOI] [PubMed] [Google Scholar]
- 22.Brimacombe J, Keller C, Fullekrug B, Agro F, Rosenblatt W, Dierdorf SF, et al. A multicenter study comparing the ProSeal and classic laryngeal mask airway in anesthetized, nonparalyzed patients. Anesthesiology. 2002;96:289–95. doi: 10.1097/00000542-200202000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Lmb AB, Wrigley MW. The effect of nitrous oxide on laryngeal mask cuff pressure in vitro and in vivo studies. Anaesthesia. 1992;47:320–3. doi: 10.1111/j.1365-2044.1992.tb02173.x. [DOI] [PubMed] [Google Scholar]
- 24.Lim HK, Lee CS, Song JH. The comparison of laryngeal mask airway and laryngeal tube in spontaneous breathing anesthetized pediatric patients. Korean J Anesthesiol. 2005;49:67–71. [Google Scholar]


