Abstract
Background
Depression and posttraumatic stress disorder (PTSD) are common in developing and postconflict countries. The purpose of this study is to examine longitudinal changes in PTSD in HIV-infected and uninfected Rwandan women who experienced the 1994 genocide.
Methods
Five hundred thirty-five HIV-positive and 163 HIV-negative Rwandan women in an observational cohort study were followed for 18 months. Data on PTSD symptoms were collected longitudinally by the Harvard Trauma Questionnaire (HTQ) and analyzed in relationship to demographics, HIV status, antiretroviral treatment (ART), and depression. PTSD was defined as a score on the HTQ of ≥2.
Results
There was a continuing reduction in HTQ scores at each follow-up visit. The prevalence of PTSD symptoms changed significantly, with 61% of the cohort having PTSD at baseline vs. 24% after 18 months. Women with higher HTQ score were most likely to have improvement in PTSD symptoms (p<0.0001). Higher rate of baseline depressive symptoms (p<0.0001) was associated with less improvement in PTSD symptoms. HIV infection and ART were not found to be consistently related to PTSD improvement.
Conclusions
HIV care settings can become an important venue for the identification and treatment of psychiatric problems affecting women with HIV in postconflict and developing countries. Providing opportunities for women with PTSD symptoms to share their history of trauma to trained counselors and addressing depression, poverty, and ongoing violence may contribute to reducing symptoms.
Introduction
Although universal global access to antiretroviral therapy (ART) has not yet been achieved, HIV-infected women in low-income and middle-income countries are gaining access to HIV care and ART and, thus, living longer. In sub-Saharan Africa, where >67% of persons with HIV reside, 30% of infected persons needing ART are now estimated to use ART.1 Some countries, such as Botswana and Rwanda, report >60% of HIV-infected persons in need of ART accessing this treatment, with more women than men receiving ART. In these developing and postconflict countries, however, women with HIV often continue to experience psychosocial problems, including poverty, stigma, depression, abuse and violence, and posttraumatic stress disorder (PTSD).2–6 As these women respond to ART and continue accessing HIV care, it is important to understand the impact of these economic and social factors on HIV illness and psychologic distress and the impact of HIV care and medications on these factors.7
Prevalence of depression and PTSD among women with HIV in developing and postconflict countries varies by nation and assessment method. A cross-sectional analysis of HIV-infected patients enrolled in a clinic (74% of whom were women) in South Africa found 14% had depression and 5% had PTSD.8 Another cross-sectional study in South Africa among newly diagnosed HIV-infected persons estimated the prevalence of ever having PTSD as 54% and the incidence of HIV-related PTSD as 40%.9 Most of these studies are cross-sectional and do not reflect interventions or changes in PTSD over time. However, Olley et al.10 found that high rates of depression and PTSD in HIV-infected patients persisted after 6 months of HIV treatment.
Symptoms of grief, depression, and PTSD continue in women in postconflict countries many years after their traumatic experiences. Pham et al.11 surveyed 2074 Rwandans about trauma exposure and prevalence of PTSD symptoms 8 years after the genocide and found that 25% of respondents had PTSD symptoms. Schaal et al.12 studied 194 Rwandan widows for prolonged grief disorder and found that 12 years after the genocide, more than one third reported feelings of longing or yearning and feeling stunned, shocked, or dazed; 28% felt life was unfulfilling, empty, or meaningless. Among women who lived in Rwanda during the 1994 genocide and enrolled in a cohort study of women with HIV, the prevalence of psychologic symptoms was high more than a decade after the genocide: 58% reported symptoms consistent with PTSD, and 81% reported depressive symptoms.13
As more women with HIV in postconflict and developing countries receive HIV care, there will be increasing need and opportunities to address psychologic comorbidities. Providers should understand these patients' experience of violence and subsequent symptoms. This study examines PTSD symptoms in HIV-infected and uninfected Rwandan women, who experienced the 1994 Rwanda genocide, over an 18-month period as ART became available.
Materials and Methods
The Rwanda Women's Interassociation Study and Assessment (RWISA) is an observational cohort study of HIV-infected and uninfected Rwandan women, including survivors of genocidal rape in 1994. The study was initially funded by the National Institute of Allergy and Infectious Diseases and was approved by the Rwandan National Ethics Committee and the Institutional Review Boards of Montefiore Medical Center (Bronx, NY) and Stroger Hospital (Chicago, IL).
From May through November 2005, 936 women (710 HIV-positive and 226 HIV-negative) enrolled in RWISA. Trained Rwandan study staff recruited participants from Rwandan women's associations and HIV clinics in Kigali. Criteria for enrollment included (1) living in Rwanda in 1994 during the genocide, (2) being >15 years of age in 1994, (3) agreeing to be tested and retested for HIV, (4) ability to complete the interview in the Kinyarwanda language, and (5) understanding and giving informed consent. Participants received transportation support, a meal during the study visit, and a modest monetary incentive. Frequency matching during study enrollment found that 50% of both the enrolled HIV-positive and HIV-negative women reported having been raped during the 1994 genocide.
The baseline study visit included an interview, physical and gynecologic examination, and collection of blood, urine, and gynecologic specimens. Rwandan trauma counselors and nurses were trained to conduct the interview and examination in Kinyarwanda. They entered all interview and physical examination data directly into an ACCESS database at the time of the visit. The interview collected demographic, medical, psychosocial, and behavioral information. Blood specimens were taken for CD4 cell count testing.
Three follow-up visits occurred at 6-month intervals and included a brief physical examination, an interview to assess interval historical data, including ART adherence, measurement of depression and PTSD symptoms, incidents of violence, and collection of biologic specimens. Participants who experienced emotional distress because of sensitive questions or recalling of events were counseled onsite and provided with debriefing and referral, if needed, for additional counseling by study trauma counselors at another time. If a participant had an acute medical illness during the study visit, she was referred to a clinical provider in the colocated clinic or to her primary care site.
Measures
Sociodemographic and health factors assessed included age at study visit, marital status, monthly income, employment, educational attainment, reading ability, healthcare use (care settings and treatment by trauma counselors), HIV serostatus, and, for the HIV-positive participants, CD4 cell count and reported use of ART. Participants were also questioned about postgenocidal physical and sexual abuse and threats to their safety.
Harvard Trauma Questionnaire
RWISA trauma counselors were trained by the study psychologist to use the Harvard Trauma Questionnaire (HTQ) to determine events experienced during the 1994 genocide and responses to these events. The HTQ is a cross-culturally validated instrument measuring trauma and torture events and symptoms. In accordance with World Health Organization (WHO) guidelines for cross-cultural translation and adaptation, the HTQ was translated into French, then Kinyarwanda, followed by blind back-translation into French and then English.14 Three focus groups comprising six to eight trauma counselors from different Rwandan women's associations reviewed the questionnaire item-by-item, adapting the HTQ items to the Rwandan experience and the Kinyarwanda linguistic equivalent. The instrument was then piloted to ensure that the words and descriptions of traumatic events and symptoms were relevant to women who had lived in Rwanda during the genocide. The instrument was revised to incorporate this input and then administered by the trained trauma counselors to all RWISA participants.
During the baseline visit, trauma counselors spent 45 minutes administering the HTQ, as well as additional questions about reported rape. Participants were asked specifically about their experiences during the genocide, including trauma experiences, head injury, torture, and rape. Women who reported being raped during the genocide were asked further detailed questions about the method, number of episodes, duration, place, and physical sequelae of the rapes. The trauma counselors and study staff created an environment where women could disclose their traumatic history by answering yes or no to specific questions or by providing a narrative. There was no pressure to disclose more than the participants desired, allowing them to determine how much they wanted to share. The interviewers were trained by a psychologist and responded to emotional distress in culturally sensitive and therapeutic ways. Participants were able to return for up to three debriefing sessions.
The total number of genocidal trauma events was calculated and presented as a number and in relation to the mean number for the cohort. The HTQ also includes a measurement of PTSD, which assessed the three categories of trauma symptoms required for a DSM IV diagnosis: reexperiencing, avoidance, and hyperarousal. Each category had several components, all of which were scored. A final mean score was calculated. Mean HTQ scores >2 meet DSM-IV diagnostic criteria for PTSD, and women with mean HTQ scores >2 were categorized as having PTSD in this study. During the 6-month follow-up study visits, genocidal trauma events were not discussed, but the participants were again asked about trauma symptoms.
Depressive symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D), a widely used validated 20-item scale, measured depressive symptoms, with the standard cutoff of ≥16 indicating clinically significant symptoms of depression and the cutoff of ≥27 indicating major depressive disorder (MDD).15 For each person, the full CES-D score was imputed if 1-3 items were missing, using the person-mean approach, which has been shown to be accurate.16 In this approach, the full CES-D is calculated as:
 |
Statistical analysis
The Cronbach α, a measure of internal consistency reliability, was estimated to be 0.93 for all 40 trauma symptom items of the HTQ and was 0.89 for the CES-D, indicating excellent internal consistency. Differences in reported baseline characteristics, including depressive symptoms and PTSD, between HIV-infected and uninfected women were assessed using chi-square, exact, and t tests as appropriate.
We calculated the change in PTSD from baseline visit to each of the follow-up visits and used linear regression and analysis of variance (ANOVA) models to statistically compare these changes across different characteristics. A multivariate model was then used to examine independent predictors of sustained change from visit 1 to visit 4, including those variables from the univariate model that had the most consistent associations with PTSD change as well as those with theoretical evidence for the association.
Results
Of the 936 participants enrolled in RWISA at baseline, 698 (163 HIV-negative and 535 HIV-positive) subjects completed the baseline HTQ and at least one postbaseline HTQ (visits 2, 3, and 4) and were included in this analysis. The 238 subjects without postbaseline HTQ data were excluded. Participants included in the analysis were similar to those not included in terms of age, marital status, income, education, HIV status, experience of genocidal rape and traumatic events, and baseline HTQ and CES-D scores. However, those included in the analysis reported less depressive symptoms and, for the HIV infected, had higher CD4 cell counts at baseline than did those excluded.
Table 1 shows the demographic and clinical characteristics of the participants by HIV status. The women were mostly poor and had only primary school education; almost half were widowed. Compared to HIV-infected women, uninfected women were significantly older and more likely to be widowed, to have a lower monthly income, and to have attended secondary school. Both HIV-infected and uninfected participants experienced a high number of traumatic events during the genocide, and 60% of the HIV-infected women and 68% of the uninfected women had HTQ scores at baseline consistent with PTSD. Depressive symptoms were significantly more prevalent among the HIV-infected than the HIV-negative participants at baseline and were reported in more than three quarters of the whole study cohort. Women with HIV were significantly more likely to have experienced postgenocidal violence (including sexual or physical abuse or threats) and to have used healthcare and trauma counselor services. At study entry, about one third of the women with HIV had CD4 cell count <200 cells/μL.
Table 1.
Baseline Characteristic of Rwanda Women's Interassociation Study and Assessment Participants with Posttraumatic Stress Disorder Measured for Four Visits
| Parameter | HIV-negative (n=163) | HIV-positive (n=535) | All subjects (n=698) | p value |
|---|---|---|---|---|
| Age, mean (SD)*** | 42.0 (10.2) | 35.0 (6.9) | 36.7 (8.3) | <0.0001 |
| Marital status, n (%)** | 0.015 | |||
| Widowed | 84 (52.5) | 222 (41.5) | 306 (44.1) | |
| Other | 76 (47.5) | 313 (58.5) | 389 (55.9) | |
| Monthly income, n (%)** | 0.0031 | |||
| <10,000 FRW (US$18) | 84 (47.7) | 222 (34.2) | 253 (37.2) | |
| ≥10,000 FRW | 76 (52.3) | 348 (65.8) | 427 (62.8) | |
| Employed, n (%) | 41 (27.1) | 123 (23.6) | 164 (24.4) | 0.39 |
| Schooling, n (%) | 0.07 | |||
| None | 46 (28.8) | 123 (23.1) | 169 (24.4) | |
| Primary school | 92 (57.5) | 357 (67.1) | 449 (64.9) | |
| Secondary school and up | 22 (13.7) | 52 (9.8) | 74 (10.7) | |
| Ability to read most or all, n (%) | 56 (35.0) | 183 (34.4) | 239 (34.5) | 0.92 |
| No. of genocidal trauma events, mean (SD) | 14.4 (6.5) | 13.5 (6.1) | 13.7 (6.2) | 0.091 |
| Nongenocide violence, n (%)** | 44 (27.3) | 192 (36.1) | 236 (34.1) | 0.046 |
| CESD, mean (SD)*** | 20.6 (9.5) | 23.4 (9.0) | 22.8 (9.2) | 0.0006 |
| ≥16, n (%)*** | 104 (63.8) | 436 (81.5) | 540 (77.4) | <0.0001 |
| ≥27, n (%) | 37 (22.7) | 156 (29.2) | 193 (27.7) | 0.11 |
| HTQ, mean (SD) | 2.4 (0.7) | 2.3 (0.7) | 2.4 (0.7) | 0.14 |
| >2, n (%) | 110 (67.5) | 319 (59.6) | 429 (61.5) | 0.081 |
| CD4, mean (SD) (for HIV+ women only) | - | 287 (162) | ||
| CD4 <200, n (%) (HIV+ women) | - | 168 (31.5) | ||
| Saw trauma Counselor past 6 months, n (%)*** | 24 (15.1) | 151 (28.4) | 175 (25.3) | 0.0006 |
p<0.05; **p<0.01; ***p<0.001, between HIV− and HIV+ based on exact tests for categorical variables and t tests for continuous variables.
CES-D, Center for Epidemiologic Studies Depression Scale; FRW, Rwandan francs; HTQ, Harvard Trauma Questionnaire; SD, standard deviation.
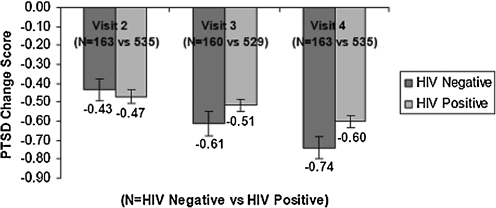
Figure 1 shows the changes in HTQ scores from the baseline visit to visits 2, 3, and 4. There was a continuing reduction in the mean HTQ scores at each follow-up visit, reflecting a sustained reduction in PTSD among both HIV-positive and HIV-negative women. Using the HTQ cutoff of 2.0, the prevalence of PTSD fell from 61% in the entire cohort at baseline to 24% (24.7% HIV-infected and 23.9% uninfected women) at visit 4 (data not shown). Although less striking, participants reported fewer depressive symptoms at visit 4 compared to baseline (77% reported CES-D ≥16 at baseline compared to 57% at visit 4).
FIG. 1.
Change in posttraumatic stress disorder (PTSD), by visit (with standard error).
There was also a reduction in the number of participants who reported seeking care from a trauma counselor over the study period. At the baseline visit, 25% (28.4% of the HIV-infected women and 15.1% of the uninfected women) reported seeing a trauma counselor. This was reduced at each of the next three visits, with only 6.8% (8.2% of HIV-infected women and 1.9% of uninfected women) (p<0.0001) seeking a trauma counselor in the 6 months before visit4 (data not shown).
To better understand which factors were associated with this reduction in PTSD, we analyzed the associations of patient characteristics at baseline with change from the baseline visit to visit 2, 3, and 4 in linear regression models using change as the outcome (Table 2). For example, the variable marital status shows change from study entry to visit 2 of −0.05 for widowed, which means that PTSD declined from baseline to visit 2 by 0.05 units more for those who are widowed than it did for other groups. For the variable of experienced postgenocidal violence, the coefficient of 0.07 from study entry to visit 2 means that for those who experienced genocidal violence, the decline in PTSD from baseline to visit 2 was 0.07 units less than for those who did not.
Table 2.
Univariate Linear Regression of Changes in Harvard Trauma Questionnaire Score from Baseline to Visits 2, 3, and 4 in Rwanda Women's Interassociation Study and Assessment Participants
| |
Change from study entry to visit 2 |
Change from study entry to visit 3 |
Change from study entry to visit 4 |
|||
|---|---|---|---|---|---|---|
| Variable | Estimate | p value | Estimate | p value | Estimate | p value |
| Marital status | ||||||
| Widowed | −0.05 | 0.46 | −0.1 | 0.09 | −0.06 | 0.30 |
| Other | Baseline | Baseline | Baseline | |||
| Age | ||||||
| below median | Baseline | Baseline | Baseline | |||
| Larger than or equal to median age | −0.05 | 0.44 | −0.02 | 0.80 | −0.05 | 0.34 |
| Income (Rwandan francs) | ||||||
| >10,000 (>$18) | Baseline | Baseline | Baseline | |||
| <10,000 (<$18) | 0.08 | 0.22 | 0.05 | 0.43 | 0.01 | 0.92 |
| Education | ||||||
| None | Baseline | Baseline | Baseline | |||
| Primary school | 0.07 | 0.56 | 0.1 | 0.36 | 0.1 | 0.34 |
| Finished secondary school | 0.1 | 0.32 | 0.15 | 0.12 | 0.12 | 0.19 |
| HIV status | ||||||
| HIV− | Baseline | Baseline | Baseline | |||
| HIV+ | −0.04 | 0.63 | 0.1 | 0.16 | 0.14 | 0.037 |
| HIV status and CD4 count | ||||||
| HIV− | Baseline | Baseline | Baseline | |||
| HIV+ CD4 ≥200 cells/μL | −0.06 | 0.46 | 0.11 | 0.14 | 0.14 | 0.040 |
| HIV+ CD4 <200 cells/μL | 0.02 | 0.84 | 0.06 | 0.50 | 0.19 | 0.044 |
| Genocidal rape | ||||||
| Did not experience genocidal rape | Baseline | Baseline | Baseline | |||
| Experienced genocidal rape | 0.01 | 0.82 | −0.13 | 0.030 | −0.16 | 0.0040 |
| Number of genocidal traumatic events (per event) | −0.09 | 0.16 | −0.26 | <0.0001 | −0.24 | <0.0001 |
| Postgenocidal violence | ||||||
| Did not experience postgenocidal violence | Baseline | Baseline | Baseline | |||
| Experienced postgenocidal violence | 0.07 | 0.54 | 0.06 | 0.74 | 0.06 | 0.61 |
| Depression scale | ||||||
| CES-D (per unit) | 0.02 | <0.0001 | 0.03 | <0.0001 | 0.02 | <0.0001 |
| Baseline posttraumatic stress symptoms | ||||||
| Baseline HTQ (per unit) | −0.78 | <0.0001 | −0.9 | <0.0001 | −0.84 | <0.0001 |
| ART use among HIV+ women | ||||||
| Does not report ART use since last visit | Baseline | Baseline | Baseline | |||
| Reports ART use since last visita | 0.11 | 0.11 | 0.02 | 0.73 | −0.01 | 0.84 |
Antiretroviral therapy (ART) use restricted to HIV-positive women.
For reduction in HTQ score between the baseline visit and visit 2 (where the largest reduction between visits was observed), only high baseline PTSD was associated with a significantly reduced HTQ score. This pattern of improvement in PTSD in those participants with the highest baseline HTQ scores continued from baseline to visits 3 and 4. In addition, the likelihood of a reduced HTQ score in visit 3 was significantly increased if the participant reported experiencing more traumatic events. In changes from baseline to visit 4, reporting a higher number of traumatic events and experiencing genocidal rape were significantly associated with reduced HTQ scores. Importantly, those participants with more depressive symptoms (CES-D ≥16) were less likely to show declines in their HTQ scores at each visit. Eighty percent of the cohort had PTSD symptoms decrease from visit 1 to visit 4. In general, the same factors that were associated with linear change in PTSD from visit 1 to visit 4 (Table 2) were also associated with lack of improvement in PTSD from visit 1 to visit 4 (data not shown).
Compared to uninfected women, women with HIV had similar changes in HTQ scores in visits 2 and 3 but a significantly smaller reduction in HTQ scores in visit 4. These changes were not related to their CD4 cell counts. As women with HIV initiated indicated ART, we also investigated the effect of its use on reducing HTQ scores. By the fourth study visit, two thirds of the HIV-infected women reported taking ARTs. As shown in Table 2, however, there was no correlation between antiretroviral medication use and reduced HTQ scores.
We then used a multivariate model to evaluate predictors for the sustained reduction in HTQ scores from the baseline visit to visit 4 (Table 3). We included baseline HTQ score and CES-D ≥16, which had the most consistent associations with PTSD change in the univariate models, along with variables for which there is theoretical evidence for association. We also included HIV status, as we had hypothesized that PTSD could be part of the psychologic response to being infected with HIV. After adjusting for HIV status, CD4 <200 vs. >200 had no association in univariate models and was not included. We used the number of genocidal traumatic events in the model instead of reported experience of genocidal rape, as genocidal traumatic events and genocidal rape were collinear, the number of traumatic events had better associations in univariate models, and genocidal rape is included as a genocidal traumatic event. Previous studies have also found the number of traumatic events to be associated with persistent PTSD. Other variables in Table 2 were not included because of both lack of statistical association in unadjusted models and a priori theoretical evidence for association. In the final model, baseline PTSD continued to be the strongest predictor of improved HTQ score. Reporting depressive symptoms (CES-D ≥16) was again a major factor preventing improved HTQ score.
Table 3.
Final Model for Change in Posttraumatic Stress Disorder from Visit 1 to Visit 4
| Variable | Change from visit 1 to visit 4 (LOCF) Estimate | p value |
|---|---|---|
| Baseline HTQ score (per unit) | −0.92 | <0.0001 |
| Baseline CES-D score (per unit) | 0.04 | <0.0001 |
| HIV status (+vs.−) | 0.03 | 0.38 |
| Number of genocidal traumatic events (per event) | 0.02 | 0.53 |
LOCF, last observation carry forward.
Discussion
RWISA participants demonstrated high levels of PTSD and depressive symptoms at the start of this study more than 10 years after the Rwandan genocide. Encouragingly, the prevalence of PTSD changed significantly over 18 months, with 61% of the cohort having PTSD at baseline and 24% having PTSD at the fourth study visit.
All the participants in RWISA were administered the HTQ. Those reporting more traumatic experiences during the genocide, including rape and higher number of trauma events, were more likely to have reduced levels of PTSD at visit 4. In the final model, we found that those women with the highest HTQ scores, representing clinical PTSD, were most likely to reduce their HTQ scores. These findings point to the greater improved response of those with more severe trauma histories and PTSD symptoms at baseline. Although we cannot exclude regression to the mean (i.e., referral of persons with exacerbation of PTSD symptoms enrolling in the study and then recovering over time) as an explanation for the reductions in HTQ scores in RWISA participants with the most PTSD at baseline, we believe that the experience of sharing their history of trauma and the support of the trained trauma counselors may have contributed to their improvement.
The RWISA participants lived in Rwanda and experienced multiple traumatic events during the 1994 genocide, 11 years before enrollment in RWISA.13 Many women in RWISA reported that responding to the HTQ was their first opportunity to relate their stories in a safe, confidential, and supportive environment. In the introduction to the manual for the HTQ, Mollica et al. write:
… trauma survivors appreciate the opportunity to relate their trauma stories and that in a safe and empathic environment most survivors welcome the opportunity to bear testimony to their own experiences and the suffering of their family and community. For many individuals, it is the first time they have been in a setting in which they feel secure enough to unburden themselves of their memories, a process that can overcome a sense of isolation and foster feelings of relief and comfort.17
The HTQ's use of a checklist, which in our study was adapted to reflect the experiences of survivors in Rwanda, facilitated the sharing of experiences that might not have been easily communicated in an open-ended narrative approach. Additionally, 50% of the participants also answered specific questions about the details of genocidal rape in a therapeutic setting. Finally, women were given the time to share their stories in a nondirected narrative if they chose to do so. Respect, safety, and confidentiality were assured for each participant, in keeping with the administration of the HTQ.
The psychologic burden of trauma and the benefits of some form of narrative intervention are well documented.18,19 RWISA interviewers administered the HTQ and additional detailed questions about rape, which allowed the participants to name the traumas they experienced in a thorough and systematic fashion to trained trauma counselors who were clinically competent, empathic, and nonjudgmental. The participants had access to the trauma counselors after the baseline visit along with follow-up visits, allowing the participants to maintain a connection with the trauma counselor/interviewer. These trauma counselors continued to demonstrate concern by asking follow-up questions about participants' physical and psychologic functioning. It is plausible that this structured experience led to PTSD symptom improvement, particularly for the women who were most symptomatic.20 As PTSD symptoms improved, the women reported less contact with trauma counselors in subsequent follow-up visits, consistent with their general improvement. Although generally used as a diagnostic tool, the HTQ, along with the opportunity to relate a detailed description of the violence they experienced and the support and counseling of RWISA's trained trauma counselor study staff, may have had a significant therapeutic effect in this study.
There was not a consistent relationship of HIV infection to the change in prevalence of PTSD over the 18-month period. In addition, reported ARV use which increased at each subsequent study visit, was not associated with lower HTQ scores. This probably reflects the greater impact of the genocidal trauma on PTSD than HIV infection for both the infected and uninfected women in the cohort.
In the final model in the current study, the number of traumatic events was not associated with change in PTSD, perhaps because more traumatic events were so strongly associated with baseline PTSD, which was included in the multivariate analysis. Other studies have shown that more traumatic events may predict PTSD. In two recent reviews of the literature on trauma in civilian populations, a dose-response relationship between cumulative war trauma and torture and the development and maintenance of PTSD was confirmed.21,22
In one of the few longitudinal studies of psychologic symptoms in persons exposed to severe trauma or societal conflict in Bosnia, Mollica et al.23 found that 23% of those with PTSD at the initial evaluation continued to have symptoms of PTSD after 3 years. Most of those with continued symptoms were found to have comorbid depression. In RWISA, we also found that those with more depressive symptoms (based on the CES-D) were more likely to maintain HTQ scores that met the criteria for PTSD. Improvement in PTSD symptoms is not likely without addressing both depression and the contributing social determinants of health.24 Although comorbidity of PTSD and depression is common in postconflict settings, more severe depressive symptoms may contribute to the maintenance of PTSD.
Limitations
There are some limitations to our study. We cannot definitely determine the impact of the HTQ or the cause of the reduced PTSD prevalence in the follow-up visits, as there was no control group. The RWISA research staff reported that the adapted HTQ and rape questions represented the first time most participants shared their experiences and memories of and feelings about the abuses experienced during the genocide. The trauma counselors were convinced that this communication and the therapeutic relationship allowed many participants to feel unburdened for the first time.
Although the instruments used in this study were adapted, translated, back-translated, and pilot tested among RWISA participants before study initiation and then were found to have reliable internal consistency, they were not formally validated in Rwanda.25 The lack of qualified mental health providers made this validation impossible.
From the data we have collected, we are unable to determine if the diagnosis of HIV influenced PTSD prevalence, as we do not know the date of initial infection or diagnosis of HIV for the participants. However, our data show that the prevalence of PTSD was similar for both the HIV-infected and uninfected groups at baseline.
The impact of Rwandan government judicial policies during the study period was not evaluated. In response to the massive number of criminal cases related to genocide, including rape,26 the Rwandan government adapted a community conflict resolution mechanism, known as Gacaca courts. Based on a traditional community justice system, the Gacaca process enlisted active popular participation in public hearings as a means to facilitate truth telling and accountability and to promote national reconciliation.27 However, the Gacaca court proceedings were public and frequently contributed to the distress level of survivors who had experienced sexual violence by causing feelings of shame, depression, stigmatization, and fear of community or family rejection.28
We also do not know if there were other treatment interventions for PTSD not reported during the study visits in addition to the counseling initially provided by RWISA trauma counselors. This seems unlikely, as there are few mental health providers available in Rwanda and medications for PTSD and depression are not widely available and were not reported as used by the participants. Finally, the Rwandan nongovernmental associations that recruited participants into RWISA may have referred their most distressed members for enrollment in the study, and the levels of PTSD may not be generalizable to other Rwandan women.
Conclusions
As more women in postconflict and developing countries gain access to ART and HIV care, HIV care settings can become an important venue for the identification and treatment of psychiatric problems affecting women with HIV.29 Addressing the multiple burdens of HIV, mental disorders, gender-based violence, and poverty may reduce significant morbidity.30
Acknowledgments
This work was funded by a supplement to the Bronx/Manhattan Consortium of the Women's Interagency HIV Study (WIHS) Study (Principal Investigator Kathryn Anastos, U01-AI-35004). The Bronx WIHS is funded by the National Institute of Allergy and Infectious Diseases, with supplemental funding from the National Cancer Institute, the National Institute on Drug Abuse. M.H.C. is supported in part by a National Institute of Allergy and Infectious Diseases grant U01-A1- 34993. This work was also supported in part by the Center for AIDS Research at the Albert Einstein College of Medicine and Montefiore Medical Center funded by the National Institutes of Health (NIH AI-51519) and by the National Institute of Diabetes and Digestive and Kidney Disease (DK54615).
Part of the data in this article was presented at the International AIDS Meeting in Mexico City, August 7, 2008.
Disclosure Statement
No competing financial interests exist for any of the authors.
References
- 1.UNAIDS. Report on the global HIV/AIDS epidemic 2008: Executive summary. data.unaids.org/pub/GlobalReport/2008/JC1511_GR08_ExecutiveSummary_en.pdf data.unaids.org/pub/GlobalReport/2008/JC1511_GR08_ExecutiveSummary_en.pdf
- 2.Williams DR. Herman A. Stein DJ, et al. Twelve-month mental disorders in South Africa: Prevalence, service use and demographic correlates in the population-based South African Stress and Health Study. Psychol Med. 2008;38:211–220. doi: 10.1017/S0033291707001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whetten K. Whetten RA. Ostermann J, et al. Trauma, anxiety, reported health among HIV-positive persons in Tanzania and the U.S. deep south. AIDS Care. 2008;10:1233–1241. doi: 10.1080/09540120801918636. [DOI] [PubMed] [Google Scholar]
- 4.Olley BO. Abrahams N. Stein DJ. Association between sexual violence and psychiatric morbidity among HIV positive women in South Africa. Afr J Med Med Sci. 2006;35(Suppl):143–147. [PubMed] [Google Scholar]
- 5.Deyessa N. Berhane Y. Alem A, et al. Depression among women in rural Ethiopia as related to socioeconomic factors: A community-based study on women in reproductive age groups. Scand J Public Health. 2008;36:589–597. doi: 10.1177/1403494808086976. [DOI] [PubMed] [Google Scholar]
- 6.Roberts B. Ocaka KF. Browne J, et al. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. 2008;8:38. doi: 10.1186/1471-244X-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murray LK. Semrau K. McCurley E, et al. Barriers to acceptance and adherence of antiretroviral therapy in urban Zambian women: A qualitative study. AIDS Care. 2009;21:78–86. doi: 10.1080/09540120802032643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myer L. Smit J. Roux LL, et al. Common mental disorders among HIV-infected individuals in South Africa: Prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care STDs. 2008;22:147–158. doi: 10.1089/apc.2007.0102. [DOI] [PubMed] [Google Scholar]
- 9.Martin L. Kagee A. Lifetime and HIV-related PTSD among persons recently diagnosed with HIV. AIDS Behav. 2011;15:125–131. doi: 10.1007/s10461-008-9498-6. [DOI] [PubMed] [Google Scholar]
- 10.Olley BO. Seedat S. Stein DJ. Persistence of psychiatric disorders in a cohort of HIV/AIDS patients in South Africa: A 6-month follow-up study. J Psychosom Res. 2006;61:479–484. doi: 10.1016/j.jpsychores.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Pham PN. Weinstein HM. Longman T. Trauma and PTSD symptoms in Rwanda: Implications for attitudes toward justice and reconciliation. JAMA. 2004;292:602–612. doi: 10.1001/jama.292.5.602. [DOI] [PubMed] [Google Scholar]
- 12.Schaal S. Jacob N. Dusingizemungu JP. Elbert T. Rates and risks for prolonged grief disorder in a sample of orphaned and widowed genocide survivors. BMC Psychiatry. 2010;10:55. doi: 10.1186/1471-244X-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen MH. Fabri M. Cai X, et al. Prevalence and predictors of posttraumatic stress disorder and depression in HIV-infected and at-risk Rwandan women. J Womens Health. 2009;18:1783–1791. doi: 10.1089/jwh.2009.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fabri M. Cultural adaptation and translation of assessment instruments: The use of the Harvard Trauma Questionnaire in Rwanda. In: Suzuki L, editor; Ponterotto J, editor. Handbook of multicultural assessment. 3rd. San Francisco, CA: Jossey-Bass; 2008. pp. 195–219. [Google Scholar]
- 15.Cheok F. Schrader G. Banham D, et al. Identification, course, and treatment of depression after admission for a cardiac condition: Rationale and patient characteristics for the Identifying Depression As a Comorbid Condition (IDACC) project. Am Heart J. 2003;146:978–984. doi: 10.1016/S0002-8703(03)00481-2. [DOI] [PubMed] [Google Scholar]
- 16.Bono C. Ried LD. Kimberlin C, et al. Missing data on the Center for Epidemiologic Studies Depression Scale: A comparison of 4 imputation techniques. Res Social Adm Pharm. 2007;3:1–27. doi: 10.1016/j.sapharm.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Mollica RF. McDonald LS. Massagli MP, et al. Measuring trauma, measuring torture. Harvard Program in Refugee Trauma; Cambridge MA: 2004. [Google Scholar]
- 18.Neuner F. Schauer M. Klaschik C, et al. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. J Consult Clin Psychol. 2004;72:579–587. doi: 10.1037/0022-006X.72.4.579. [DOI] [PubMed] [Google Scholar]
- 19.Snider L. Cabrejos C. Marquina EH, et al. Psychosocial assessment for victims of violence in Peru: The importance of local participation. J Biosoc Sci. 2004;36:389–400. doi: 10.1017/s0021932004006601. [DOI] [PubMed] [Google Scholar]
- 20.Kinzie JD. Psychotherapy for massively traumatized refugees: The therapist variable. Am J Psychother. 2001;55:475–490. doi: 10.1176/appi.psychotherapy.2001.55.4.475. [DOI] [PubMed] [Google Scholar]
- 21.Johnson H. Thompson A. The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clin Psychol Rev. 2008;28:36–47. doi: 10.1016/j.cpr.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 22.Steel Z. Chey T. Silove D, et al. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA. 2009;302:537–549. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- 23.Mollica RF. Sarajlic N. Chernoff M, et al. Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among Bosnian refugees. JAMA. 2001;286:546–554. doi: 10.1001/jama.286.5.546. [DOI] [PubMed] [Google Scholar]
- 24.de Jong JT. Komproe IH. Ommeren M. Common mental disorders in postconflict settings. Lancet. 2003;361:2128–2130. doi: 10.1016/S0140-6736(03)13692-6. [DOI] [PubMed] [Google Scholar]
- 25.Bolton P. Betancourt T. Mental health in post-war Afghanistan [Editorial] JAMA. 2004;292:626–628. doi: 10.1001/jama.292.5.626. [DOI] [PubMed] [Google Scholar]
- 26.Organic Law N40/2000 of 26/01/2001 Setting Up “Gacaca Jurisdictions” Organizing Prosecutions for Offences Constituting the Crime of Genocide or Crimes Against Humanity Committed between October 1, 1990, December 31, 1994 [2001 Gacaca Law] Official Gazette of the Republic of Rwanda. Mar 15, 2001. art. 51.
- 27.Penal Reform International, Interim report on research on Gacaca jurisdictions and its preparations. Jul-Dec. 2001. Kigali, 2001:8.
- 28.Human Rights Watch struggling to survive: Barriers to justice for rape victims in Rwanda September 30, 2004, A1610. www.unhcr.org/refworld/docid/42c3bd2b0.html. [Feb 3;2010 ]. www.unhcr.org/refworld/docid/42c3bd2b0.html
- 29.Myer L. Smit J. Roux LL, et al. Common mental disorders among HIV-infected individuals in South Africa: Prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care STDs. 2008;22:147–158. doi: 10.1089/apc.2007.0102. [DOI] [PubMed] [Google Scholar]
- 30.Smit J. Myer L. Middelkoop K, et al. Mental health and sexual risk behaviours in a South African township: A community-based cross-sectional study. Public Health. 2006;120:534–542. doi: 10.1016/j.puhe.2006.01.009. [DOI] [PubMed] [Google Scholar]