Abstract
Thyroid diseases are common worldwide. In India too, there is a significant burden of thyroid diseases. According to a projection from various studies on thyroid disease, it has been estimated that about 42 million people in India suffer from thyroid diseases. This review will focus on the epidemiology of five common thyroid diseases in India: (1) hypothyroidism, (2) hyperthyroidism, (3) goiter and iodine deficiency disorders, (4) Hashimoto's thyroiditis, and (5) thyroid cancer. This review will also briefly cover the exciting work that is in progress to ascertain the normal reference range of thyroid hormones in India, especially in pregnancy and children.
Keywords: Hypothyroidism, India, thyroid
INTRODUCTION
Thyroid diseases are, arguably, among the commonest endocrine disorders worldwide. India too, is no exception. According to a projection from various studies on thyroid disease, it has been estimated that about 42 million people in India suffer from thyroid diseases.[1] Thyroid diseases are different from other diseases in terms of their ease of diagnosis, accessibility of medical treatment, and the relative visibility that even a small swelling of the thyroid offers to the treating physician. Early diagnosis and treatment remain the cornerstone of management.
This article will focus on five selected thyroid diseases (hypothyroidism, hyperthyroidism, goiter/iodine deficiency disorders, Hashimoto's thyroiditis, and thyroid cancer) and will offer an insight into studies on their prevalence. This review will also briefly cover the exciting work that is in progress to ascertain the normal reference range of thyroid hormones in India, especially in pregnancy and children. Rather than being an exhaustive, in-depth review, this article will discuss selected studies from across the country and the implications and perspectives these studies bring forth, from an Indian context.
HYPOTHYROIDISM
Among the various varieties of hypothyroidism, congenital hypothyroidism is probably the most important, as it is requires an early diagnosis, which is usually followed by appropriate therapy that can prevent the onset of brain damage. Studies from Mumbai have suggested that congenital hypothyroidism is common in India, the disease occurring in 1 out of 2640 neonates, when compared with the worldwide average value of 1 in 3800 subjects.[2] There is often a delay in the diagnosis of congenital hypothyroidism in the country. This delay is attributable to the lack of awareness about the illness, as well as the lack of facilities available or screening program in place to comprehensively screen and test newborns for this illness.
In childhood too, hypothyroidism can occur. In a clinic-based study from Mumbai, out of 800 children with thyroid disease, 79% had hypothyroidism. Common causes of hypothyroidism in these children were thyroid dysgenesis, dyshormonogenesis, and thyroiditis.[2]
Among adult people in India, the prevalence of hypothyroidism has been recently studied. In this population-based study done in Cochin on 971 adult subjects, the prevalence of hypothyroidism was 3.9%.[3] The prevalence of subclinical hypothyroidism was also high in this study, the value being 9.4%. In women, the prevalence was higher, at 11.4%, when compared with men, in whom the prevalence was 6.2%. The prevalence of subclinical hypothyroidism increased with age. About 53% of subjects with subclinical hypothyroidism were positive for anti-TPO antibodies. This was a population-based study, which used cluster sampling strategy.[3] In this study, Urinary Iodine Status was studied in 954 subjects from the same population sampled, and the median value was 211 μg/l; this suggested that this population was iodine sufficient.
HYPERTHYROIDISM
The prevalence of hyperthyroidism has been studied in several studies. In an epidemiological study from Cochin, subclinical and overt hyperthyroidism were present in 1.6% and 1.3% of subjects participating in a community survey.[3] In a hospital-based study of women from Pondicherry, subclinical and overt hyperthyroidism were present in 0.6% and 1.2% of subjects.[4] More than a third of community-detected hyperthyroid cases have positive anti-TPO antibodies, and about 39% of these subjects have a goiter[3] [Figure 1].
Figure 1.
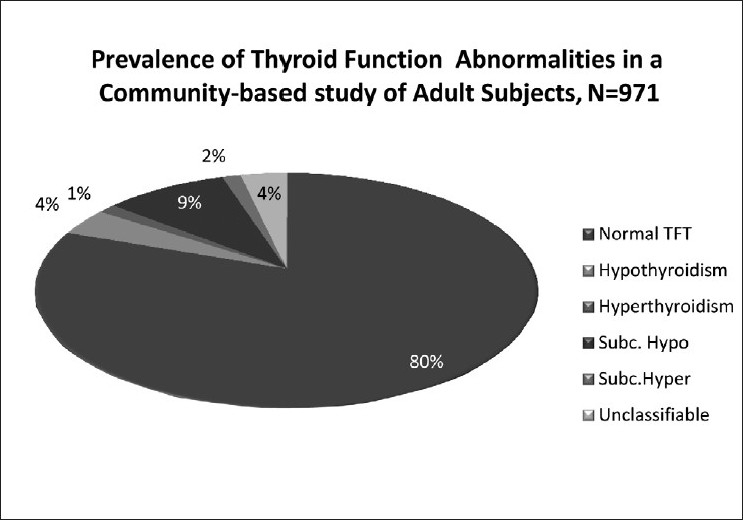
Prevalence of thyroid function abnormalities found in 971 adult subjects form a community study from Kerala, South India.[3]
GOITER AND IODINE DEFICIENCY
Recent population studies have shown that about 12% of adults have a palpable goiter.[3] Autoimmune thyroid disease is probably commoner than iodine deficiency as a cause of goiter in areas that are now iodine sufficient. However, given that iodine deficiency is a problem in India, the importance of iodine deficiency cannot be underestimated in the Indian context.
The link between endemic goiter and iodine deficiency has been researched in India by several eminent researchers, and this has led to the publication of several important reports.[5–7] Critical research has resulted in endemic goiter being reported from all over the country and not just from the Himalayan and Sub-Himalayan regions.[1] Researchers from New Delhi had shown that this was linked to iodine deficiency and that this resulted in decompensated hypothyroidism in many cases.[1] This led to landmark studies which showed that iodine deficiency was associated with hypothyroidism in neonates, setting the scene for the now legendary salt iodization program supported by the Government of India.[1] Subsequent to this program, it was shown that in selected regions of Uttar Pradesh, the prevalence of congenital hypothyroidism had come down from 100/1000 to 18/1000.[1] Several landmark studies have been carried out in the area of iodine deficiency disorders in the country.[5–7]
In the postiodization phase, what happens to the prevalence of goiter? This very important question was answered in an elegantly conducted study.[8] About 14,762 children from all over India were studied for the following characteristics: goiter prevalence, urinary iodine and thiocyanate excretion, functional status of the thyroid, as well as serological and cytopathological markers for thyroid autoimmunity. About 23% of subjects had a goiter. A significantly higher level of median urinary thiocyanate (USCN) excretion was noted in goitrous subjects (0.75 mg/dl) when compared with controls (0.64 mg/dl; P < 0.001). The authors suggested that despite iodization, the prevalence of goiter has not dramatically declined.[8] The researchers noted that thyroid autoimmunity could only partly explain the goiter and concluded that the role of goitrogens is an area that deserves further study.
AUTOIMMUNE THYROIDITIS IN INDIA
Population studies have suggested that about 16.7% of adult subjects have anti-thyroid peroxidase (TPO) antibodies and about 12.1% have anti-thyroglobulin (TG) antibodies. In this same study of 971 subjects, when subjects with abnormal thyroid function were excluded, the prevalence of anti-TPO and anti-TG antibodies was 9.5% and 8.5%.[3]
In a landmark study of Hashimoto's thyroiditis in India, 6283 schoolgirls from all over the country were screened.[9] Among them, 1810 schoolgirls had a goiter. Among them 764 subjects underwent a fine needle aspiration cytology, and of these subjects, 58 (7.5%) had evidence of juvenile autoimmune thyroiditis (the term included both Hashimoto's thyroiditis and focal lymphocytic thyroiditis). Among fine needle aspiration cytology-confirmed cases of juvenile autoimmune thyroiditis, subclinical and overt hypothyroidism were seen in 15% and 6.5%, respectively.[9]
THYROID CANCER AND INDIA
The Indian Council of Medical Research established the National Cancer Registry Program, and the NCRP has collected the data of more than 3,00,000 cancer patients between the periods 1984 and 1993.[10] Among these patients, the NCRP noted 5614 cases of thyroid cancer, and this included 3617 females and 2007 males. The six centers involved in the studies were at Mumbai, Delhi, Thiruvananthapuram, Dibrugarh, Chandigarh, and Chennai. Among them, Thiruvananthapuram had the highest relative frequency of cases of thyroid cancer among all cancer cases enrolled in the hospital registry, 1.99% among males and 5.71% among females. The nationwide relative frequency of thyroid cancer among all the cancer cases was 0.1%–0.2%. The age-adjusted incidence rates of thyroid cancer per 100,000 are about 1 for males and 1.8 for females as per the Mumbai Cancer Registry, which covered a population of 9.81 million subjects. The histological types of thyroid cancer were studied in a Hospital Cancer Registry of 1185 “new cases” of thyroid cancer.[11] The commonest cancer type was papillary, followed by follicular cancer, and the results are summarized in Figure 2.
Figure 2.
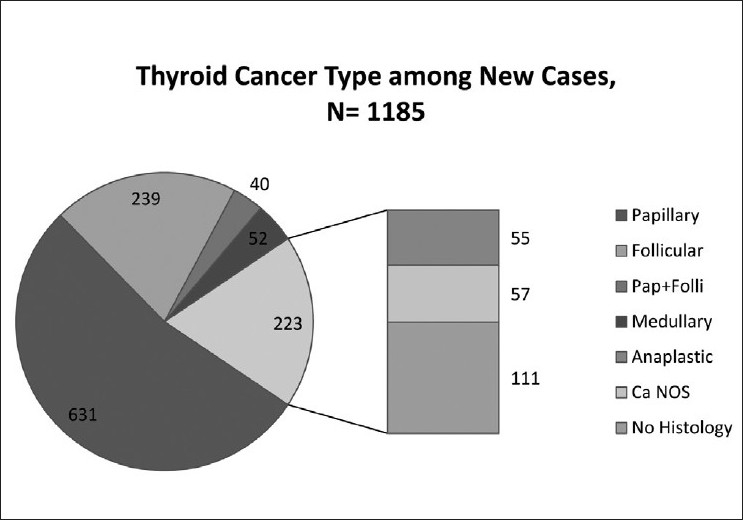
Histological type distribution of 1185 “new cases” of thyroid cancer. Figure based on a table published by Gangadharan et al.[11] Anaplastic, Cancer Not-Otherwise Specified and No histology proof-cases, together, accounted for 223 cases in this survey
REFERENCE RANGES OF THYROID FUNCTION IN PREGNANCY AND CHILDREN
In the past 2 years, exciting work has been carried out to understand the thyroid in pregnancy and childhood in India.[12–14] In the first article, Marwaha et al indicate the normal reference ranges of FT4, FT3, and TSH in pregnant women, and used the 5th and 85th percentile to define the reference ranges in the disease-free subjects. The authors report that the trimester-wise values in the first, second, and third trimesters were FT(3) (1.92–5.86, 3.2–5.73, and 3.3–5.18 pM/l), FT(4) (12–19.45, 9.48–19.58, and 11.32–17.7 pM/l), and TSH (0.6–5.0, 0.44–5.78, and 0.74–5.7 IU/ml), respectively.[12] With regard to iodine deficiency during pregnancy, a hospital-based study from Kolkata has suggested that pregnant women from their center were iodine sufficient.[13]
In a large epidemiological study of 24,685 students from all over India published in 2010, the authors attempted to define normative data on thyroid hormone levels in healthy school children.[14] Among them, the authors calculated the reference ranges from the 5343 subjects. In a separate publication in 2008, the same authors studied normative thyroid hormone ranges in 5122 school children, after excluding children who had a personal or family history of thyroid disease, used thyroid medications, had a goiter, and had hypoechogenicity/nodularity on ultrasound or positivity for serum anti-TPO antibodies.[15] The authors reported that for TSH, the 97th percentile was in the range 6.01–8.4 mIU/l for boys and 5.28–8.04 mIU/l for girls.[15] This, as the authors themselves suggest, offers a compelling argument against lowering the reference range of TSH in this population.
COMMUNITY-BASED ULTRASOUND STUDIES IN INDIA
Interesting work is in progress to ascertain the predictors of thyroid gland size in an Indian population. In a study of 1002 children from Gujarat, the authors note that the prevalence of goiter was very high (80%) when assessed by ultrasound. This was also a population with a high prevalence of malnutrition (82% subjects were underweight). In this population, the authors note that thyroid size was related to several anthropometric parameters. However, it is not clear whether these results are applicable to the general Indian population.[16] In the state of Gujarat, the same group had reported that iodine deficiency continues to be a problem, as more than 20% of the population had a very low median urinary iodine of <50 ΅g/l.[17] In the same population, the prevalence of hypothyroidism has been reported to be about 7%.[17] The use of ultrasound in population studies of thyroid gland size is an exciting new area for research in the field of thyroid epidemiology.[18–20]
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1. [Last accessed on 2011 April 2]. Available from: http://www.ias.ac.in/currsci/oct252000/n%20kochupillai.PDF .
- 2.Desai PM. Disorders of the Thyroid Gland in India. Indian J Pediatr. 1997;64:11–20. doi: 10.1007/BF02795771. [DOI] [PubMed] [Google Scholar]
- 3.Usha Menon V, Sundaram KR, Unnikrishnan AG, Jayakumar RV, Nair V, Kumar H. High prevalence of undetected thyroid disorders in an iodine sufficient adult south Indian population. J Indian Med Assoc. 2009;107:72–7. [PubMed] [Google Scholar]
- 4.Abraham R, Murugan VS, Pukazhvanthen P, Sen SK. Thyroid Disorders In Women of Puducherry. Indian J Clin Biochem. 2009;24:52–9. doi: 10.1007/s12291-009-0009-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karmarkar MG, Deo MG, Kochupillai N, Ramalingaswami V. Pathophysiology of Himalayan endemic goiter. Am J Clin Nutr. 1974;27:96–103. doi: 10.1093/ajcn/27.1.96. [DOI] [PubMed] [Google Scholar]
- 6.Sooch SS, Deo MG, Karmarkar MG, Kochupillai N, Ramachandran K, Ramalingaswami V. Prevention of endemic goitre with iodized salt. 1973. Natl Med J India. 2001;14:185–8. [PubMed] [Google Scholar]
- 7.Pandav CS, Karmarkar MG, Kochupillai N. Recommended levels of salt iodation in India. Indian J Pediatr. 1984;51:53–4. doi: 10.1007/BF02753527. [DOI] [PubMed] [Google Scholar]
- 8.Marwaha RK, Tandon N, Gupta N, Karak AK, Verma K, Kochupillai N. Residual goitre in the postiodization phase: Iodine status, thiocyanate exposure and autoimmunity. Clin Endocrinol (Oxf) 2003;59:672–81. doi: 10.1046/j.1365-2265.2003.01895.x. [DOI] [PubMed] [Google Scholar]
- 9.Marwaha RK, Tandon N, Karak AK, Gupta N, Verma K, Kochupillai N. Hashimoto's thyroiditis: countrywide screening of goitrous healthy young girls in postiodization phase in India. J Clin Endocrinol Metab. 2000;85:3798–802. doi: 10.1210/jcem.85.10.6924. [DOI] [PubMed] [Google Scholar]
- 10.Rao DN. Thyroid Cancer- An Indian Perspective. In: Shah AH, Samuel AM, Rao RS, editors. Thyroid Cancer- An Indian Perspective. Mumbai: Quest Publications; 1999. pp. 3–16. [Google Scholar]
- 11.Gangadharan P, Nair MK, Pradeep VM. Thyroid Cancer in Kerala. In: Shah AH, Samuel AM, Rao RS, editors. Thyroid Cancer- An Indian Perspective. Mumbai: Quest Publications; 1999. pp. 17–32. [Google Scholar]
- 12.Marwaha RK, Chopra S, Gopalakrishnan S, Sharma B, Kanwar RS, Sastry A, Singh S. Establishment of reference range for thyroid hormones in normal pregnant Indian women. BJOG. 2008;115:602–6. doi: 10.1111/j.1471-0528.2008.01673.x. [DOI] [PubMed] [Google Scholar]
- 13.Chakraborty I, Mazumdar P, Chakraborty PS, Chattopadhyay G, Bhowmick K. Iodine deficiency disorder among pregnant women in a tertiary care hospital of Kolkata, India. Southeast Asian J Trop Med Public Health. 2010;41:989–95. [PubMed] [Google Scholar]
- 14.Marwaha RK, Tandon N, Desai AK, Kanwar R, Aggarwal R, Sastry A, et al. Reference range of thyroid hormones in healthy school-age children: Country-wide data from India. Clin Biochem. 2010;43:51–6. doi: 10.1016/j.clinbiochem.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Marwaha RK, Tandon N, Desai A, Kanwar R, Grewal K, Aggarwal R, et al. Reference range of thyroid hormones in normal Indian school-age children. Clin Endocrinol (Oxf) 2008;68:369–74. doi: 10.1111/j.1365-2265.2007.03048.x. [DOI] [PubMed] [Google Scholar]
- 16.Brahmbhatt SR, Brahmbhatt RM, Boyages SC. Impact of protein energy malnutrition on thyroid size in an iodine deficient population of Gujarat (India): Is it an aetiological factor for goiter? Eur J Endocrinol. 2001;145:11–7. doi: 10.1530/eje.0.1450011. [DOI] [PubMed] [Google Scholar]
- 17.Brahmbhatt SR, Fearnley R, Brahmbhatt RM, Eastman CJ, Boyages SC. Study of biochemical prevalence indicators for the assessment of iodine deficiency disorders in adults at field conditions in Gujarat (India) Asia Pac J Clin Nutr. 2001;10:51–7. doi: 10.1046/j.1440-6047.2001.00197.x. [DOI] [PubMed] [Google Scholar]
- 18.Brahmbhatt SR, Brahmbhatt RM, Eastman CJ, Boyages SC. Thyroid ultrasonography consistently identifies goiter in adults over the age of 30 years despite a diminished response with aging of the thyroid gland to the effects of goitrogenesis. Scientific World Journal. 2001;1:243–53. doi: 10.1100/tsw.2001.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marwaha RK, Tandon N, Ashraf GM, Ganguly SK, Batra A, Aggarwal R, et al. Ultrasound evaluation of thyroid size: A large nationwide study of schoolchildren in India. Natl Med J India. 2008;21:69–74. [PubMed] [Google Scholar]
- 20.Marwaha RK, Tandon N, Kanwar R, Ganie MA, Bhattacharya V, Reddy DH, et al. Evaluation of the role of ultrasonography in diagnosis of autoimmune thyroiditis in goitrous children. Indian Pediatr. 2008;45:279–84. [PubMed] [Google Scholar]


