Abstract
Purpose
To evaluate effectiveness and safety of mycophenolate mofetil (MMF) monotherapy in paediatric autoimmune uveitis.
Methods
We reviewed medical records of patients, 18 years of age or younger, with autoimmune uveitis treated with MMF at our practice from 2005 to 2009. The dose and duration of MMF therapy, inflammation status, visual acuity, previous immunomodulatory therapies, and adverse effects were recorded. In addition, the following subgroups were defined: (1) Durable Disease Control: patients whose uveitis remained quiescent for at least 2 years on MMF monotherapy, with no more than two flare-ups successfully treated with an increase in MMF dosage and/or a short course (<1 month) of corticosteroids; (2) Short-term Inflammation Control: patients whose uveitis remained quiescent for less than 2 years, with no more than one flare-up successfully treated with an increase in MMF dosage and/or a short course of corticosteroids, or who initially achieved inflammation control but discontinued MMF because of significant adverse effects.
Results
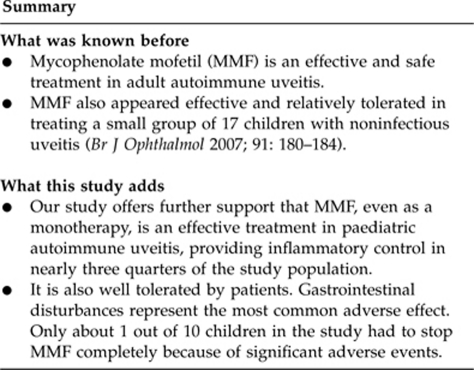
A total of 38 out of 52 patients (73.1%) obtained inflammation control following 2 months of MMF monotherapy, achieving ≤0.5+ grading in anterior chamber cell/flare and vitreous haze. In the cross-sectional analysis, 25 patients (48.1%) met the criteria for Durable Disease Control, and 13 others (25.0%) qualified for Short-term Inflammation Control. Visual acuity remained stable or improved in 94.2% of the study population. Six patients (11.5%) discontinued MMF because of significant adverse effects, the most common of which was gastrointestinal disturbances.
Conclusion
MMF monotherapy appears to be an effective and safe treatment in paediatric autoimmune uveitis.
Keywords: mycophenolate mofetil, cellcept, uveitis, paediatric, immunosuppressive, immunomodulatory
Introduction
Uveitis is a significant cause of visual morbidities in children.1 Similar to the condition found in adults, complications of paediatric uveitis may include band keratopathy, cataract, posterior synechiae, glaucoma, cystoid macular oedema, and a wide spectrum of retinal pathologies.2 Therefore, early diagnosis must be coupled with early and aggressive therapy to control inflammation. However, the necessary medications may be less tolerated and at times require a more prolonged treatment period in children than in adults.3
The gold standard of treatment for patients with autoimmune uveitis has been the use of topical and systemic corticosteroids. Unfortunately, long-term use of these medications is associated with considerable ocular and systemic complications. In addition, these complications are more marked in children.3 Therefore, steroid-sparing immunomodulatory therapies are especially useful in this population. Methotrexate (MTX) is one of the oldest, most studied immunosuppressive agents. Because of its relative ease of use, effectiveness, and safety profile in a variety of ocular and systemic autoimmune diseases, it is frequently used as the first-line steroid-sparing treatment in paediatric uveitis, particularly those associated with juvenile idiopathic arthritis.4,5,6,7,8 Nevertheless, MTX is not tolerated well by all children.9 Therefore, an alternative therapy is called for in these patients.
Mycophenolate mofetil (MMF; CellCept; Roche, Nutley, NJ, USA) is a newer immunosuppressive drug that functions by inhibiting the synthesis of purine and antibody production by B cells.10 Recently, MMF has emerged as an efficacious agent in preventing rejection after kidney transplantation in adults.11,12,13 Over the past decade, several studies have demonstrated a similar clinical effectiveness of MMF in paediatric transplant patients.14,15,16 MMF has also been proven effective in autoimmune diseases in children.17,18,19,20
Here, we report our experience with MMF in paediatric patients with autoimmune uveitis.
Materials and methods
This study was approved by the Institutional Review Board of the Massachusetts Eye and Ear Infirmary. It was compliant with the Health Insurance Portability and Accountability Act and was conducted in accordance with the tenets of the Declaration of Helsinki.
This is a retrospective interventional case series. The study population comprises all the patients with autoimmune uveitis who started MMF therapy at or before the age of 18 years and who were examined at the Massachusetts Eye Research and Surgery Institution, a tertiary uveitis referral centre, between July 2005 and March 2009. We excluded patients who had insufficient follow-up time after MMF therapy was initiated, defined as 6 months or less. We then reviewed every available clinic visit record of each qualified patient, up to his or her most recent visit. The following data were collected from our electronic medical record system (NextGen, Horsham, PA, USA):
General data: These consisted of age, gender, disease laterality, anatomic location(s) of uveitis, and any identifiable underlying systemic diagnosis. The anatomic location(s) of uveitis was recorded according to the guidelines of the Standardization of Uveitis Nomenclature (SUN) Working Group.21
Previous treatment(s) for uveitis: Use of immunomodulatory therapy (IMT) other than corticosteroid immediately before MMF therapy was recorded. This did not include all the medications a patient may have taken in the past.
Inflammation status and visual acuity: Inflammation status was judged by anterior chamber cells/flare and vitreous haze on the basis of the SUN nomenclature mentioned above and the study by Nussenblatt et al.22 Intraocular inflammation was considered active if the anterior chamber cell/flare or vitreous haze was graded >0.5+ at any examination. Conversely, disease was said to be quiescent if these inflammatory parameters were ≤0.5+. Visual acuity was assessed on the Snellen visual acuity chart and recorded specifically from the dates when MMF was initiated and discontinued (where appropriate) and at the last clinic visit.
Treatment parameters: These included duration of MMF treatment, MMF dosages, follow-up time after MMF discontinuation, time taken to reach inflammation control, number of relapses while on MMF, actions taken for relapses, adverse effects, and time taken to develop those adverse effects.
The primary outcome measures of this study were control of inflammation and adverse effects associated with MMF. Control of inflammation was defined as ≤0.5+ anterior chamber cell/flare and vitreal haze in accordance with the SUN nomenclature and the study by Nussenblatt et al.21,22 Adverse effects were assessed through patient history and laboratory evaluation. Visual acuity was a secondary outcome measure; a change of ≥2 lines on the Snellen visual acuity chart was considered clinically significant. The data were then organised in Microsoft Excel spreadsheets (Microsoft Corporation, Redmond, WA, USA) and statistical analysis was performed using Minitab 15 (Minitab Inc., State College, PA, USA).
Furthermore, we defined a subgroup of patients as Durable Disease Control and another as Short-term Inflammation Control:
Durable Disease Control: patients whose uveitis remained quiescent for at least 2 years on MMF monotherapy, with no more than two flare-ups successfully treated with an increase in MMF dosage and/or a short course (<1 month) of corticosteroids.
Short-term Inflammation Control: patients whose uveitis remained quiescent for less than 2 years, with no more than one flare-up successfully treated with an increase in MMF dosage and/or a short course of corticosteroids. In addition, this subgroup also includes patients who initially achieved inflammation control but discontinued MMF subsequently because of significant adverse effects.
Results
Patient characteristics
From July 2005 to March 2009, 58 patients started MMF treatment for their autoimmune uveitis at or before the age of 18 years. Six patients were excluded because of insufficient follow-up time (<6 months). Of the 52 qualifying patients, 24 were male and 28 were female, and the median age at MMF start was 13 years (range: 3–18). The median disease duration before MMF start was 15.5 months (range: 2–132). The diagnoses included juvenile idiopathic arthritis anterior uveitis (25 patients), idiopathic anterior uveitis (8 patients), sarcoidosis anterior uveitis (1 patient), tubulointerstitial nephritis and uveitis syndrome (TINU) anterior uveitis (1 patient), idiopathic intermediate uveitis (9 patients), idiopathic panuveitis (5 patients), sympathetic ophthalmia panuveitis (1 patient), and idiopathic posterior uveitis (2 patients). Overall, 12 patients had unilateral disease and 40 patients had bilateral disease. MMF was the first-line IMT in four patients. The remaining patients had all tried MTX in the past. Among these 48 patients, some had also been on other IMTs, including cyclosporine (four patients), adalimumab (two patients), infliximab (two patients), and etanercept (one patient). The above data are summarised in Table 1.
Table 1. Patient characteristics.
| Number of patients | 52 |
| Gender (n (% of study population)) | |
| Male | 24 (46.2%) |
| Female | 28 (53.8%) |
| Median age at MMF start (years) | 13 (range: 3–18) |
| Median disease duration prior to MMF therapy (months) | 15.5 (range: 2–132) |
| Median duration of MMF therapy (months) | 27 (range: 0.5–50) |
| Median follow-up time after MMF start (months) | 33 (range: 6–53) |
| Diagnosis (n (% of study population)) | |
| JIA anterior uveitis | 25 (48.1%) |
| Idiopathic intermediate uveitis | 9 (17.3%) |
| Idiopathic anterior uveitis | 8 (15.4%) |
| Idiopathic panuveitis | 5 (9.6%) |
| Idiopathic posterior uveitis | 2 (3.8%) |
| Sarcoidosis anterior uveitis | 1 (1.9%) |
| TINU anterior uveitis | 1 (1.9%) |
| Sympathetic ophthalmia panuveitis | 1 (1.9%) |
| Disease laterality (n (% of study population)) | |
| Unilateral | 12 (23.1%) |
| Bilateral | 40 (76.9%) |
| Previous steroid-sparing IMTs (n (% of study population)) | |
| None | 4 (7.7%) |
| Methotrexate | 48 (92.3%) |
| Cyclosporine | 4 (7.7%) |
| Adalimumab | 2 (3.8%) |
| Infliximab | 2 (3.8%) |
| Etanercept | 1 (1.9%) |
Abbreviations: IMT, immunomodulatory therapy; JIA, juvenile idiopathic arthritis; MMF, mycophenolate mofetil; TINU, tubulointerstitial nephritis and uveitis syndrome.
Treatment outcomes
The median duration of the MMF therapy was 27 months (range: 0.5–50), and the median follow-up time after therapy initiation was 33 months (range: 6–53). The median maximal dosage of MMF was 2000 mg daily (range: 600–3000).
A total of 38 out of the 52 study patients (73.1%) achieved inflammation control on MMF monotherapy, achieving ≤0.5+ grading in anterior chamber cell/flare and vitreous haze. It took a median of 2 months (range: 1–6) to establish clear inflammation control in these patients. In our cross-sectional analysis, these 38 patients were further divided into the following subgroups:
Durable Disease Control: 25 patients (48.1% of the study population) fit into this subgroup. Out of them, 16 stayed on MMF monotherapy for a median of 28.5 months (range: 24–36), discontinued MMF because it was deemed that their immune system had been ‘retrained,' and were then followed up for a median of 15 months (range: 5–27) without any disease relapse off any immunosuppressive medication, topical or systemic. The other nine patients were still on MMF at the last follow-up (median treatment duration of 27 months, range: 24–34), but they had begun the tapering process. In addition, over a median follow-up of 38 months (range: 30–51), 13 patients experienced no relapse; 7 patients had relapses (1 relapse each) treated by increasing the MMF dose; 4 patients had relapses (1 relapse in 3 and 2 relapses in 1 other) treated with 4 weeks of topical corticosteroids only; finally, 1 patient required 4 weeks of topical and systemic corticosteroids for his one relapse. In the Durable Disease Control subgroup, the overall rate of uveitis relapse on MMF was 0.29/person-year. Unfortunately, we were unable to gather information on how many relapses each patient had before being referred to us, and thus a comparison of relapse rates before and after MMF was not possible.
Short-term Inflammation Control: 13 patients (25.0% of the study population) fit into this subgroup. Nine of them achieved inflammation control on MMF without concomitant corticosteroids or other IMTs for a median of 15 months (range: 3–22). During this follow-up period, 8 out of the 9 patients experienced no uveitis relapse; 1 patient experienced one relapse that was treated with 4 weeks of topical corticosteroids. Finally, four patients achieved inflammation control initially for a median of 6 months (range: 2–11) without any relapse but had to discontinue the medication because of significant adverse effects.
The frequencies of Durable Disease Control and Short-term Inflammation Control according to the types of uveitis and previous IMTs are shown in Tables 2 and 3.
Table 2. Frequencies of Short-term Inflammation Control and Durable Disease Control in paediatric uveitis patients treated with mycophenolate mofetil monotherapy, according to types of uveitis.
| Types of uveitis | Durable Disease Control (n/N (%))a | Short-term inflammation Control (n/N (%))b | Sum of two groups (n/N (%)) |
|---|---|---|---|
| JIA anterior uveitis | 15/25 (60.0%) | 6/25 (24.0%) | 21/25 (84%) |
| Idiopathic intermediate uveitis | 4/9 (44.4%) | 2/9 (22.3%) | 6/9 (66.7%) |
| Idiopathic anterior uveitis | 4/8 (50.0%) | 2/8 (25.0%) | 6/8 (75%) |
| Idiopathic panuveitis | 1/5 (20.0%) | 2/5 (40.0%) | 3/5 (60.0%) |
| Idiopathic posterior uveitis | 0/2 (0.0%) | 1/2 (50.0%) | 1/2 (50.0%) |
| Sarcoid anterior uveitis | 0/1 (0.0%) | 0/1 (0.0%) | 0/1 (0.0%) |
| TINU anterior uveitis | 1/1 (100.0%) | 0/1 (0.0%) | 1/1 (100.0%) |
| Sympathetic ophthalmia panuveitis | 0/1 (0.0%) | 0/1 (0.0%) | 0/1 (0.0%) |
Abbreviations: JIA, juvenile idiopathic arthritis; TINU, tubulointerstitial nephritis and uveitis syndrome.
Defined as patients whose uveitis remained quiescent for at least 2 years on MMF monotherapy with no more than 2 flare-ups successfully treated with either an increase of the MMF dosage or a short duration (<1 month) of corticosteroids.
Defined as patients whose uveitis remained quiescent for less than 2 years with no more than 1 flare-up successfully treated with either an increase of the MMF dosage or a short duration (<1 month) of corticosteroids, or those who initially achieved inflammation control but had to discontinue MMF because of significant adverse effects.
n/N, no. of patients who met the criteria/no. patients with the type of uveitis.
Table 3. Frequencies of Short-term Inflammation Control and Durable Disease Control in paediatric uveitis patients treated with mycophenolate mofetil monotherapy, according to previous immunomodulatory therapy received.
| Previous IMTs | Durable Disease Control (n/N (%))a | Short-term Inflammation Control (n/N (%))b | Sum of two groups (n/N (%)) |
|---|---|---|---|
| None | 1/4 (25.0%) | 2/4 (50.0%) | 3/4 (75.0%) |
| Methotrexate | 24/48 (50.0%) | 11/48 (22.9%) | 35/48 (72.9%) |
| Cyclosporine | 1/4 (25.0%) | 1/4 (25.0%) | 2/4 (50.0%) |
| Adalimumab | 1/2 (50.0%) | 0/2 (0.0%) | 1/2 (50.0%) |
| Infliximab | 0/2 (0.0%) | 1/2 (50.0%) | 1/2 (50.0%) |
| Etanercept | 0/1 (0.0%) | 0/1 (0.0%) | 0/1 (0.0%) |
Abbreviation: IMT, immunomodulatory therapy.
Defined as patients whose uveitis remained quiescent for at least 2 years on MMF monotherapy with no more than 2 flare-ups successfully treated with either an increase of the MMF dosage or a short duration (<1 month) of corticosteroids.
Defined as patients whose uveitis remained quiescent for less than 2 years with no more than 1 flare-up successfully treated with either an increase of the MMF dosage or a short duration (<1 month) of corticosteroids, or those who initially achieved inflammation control but had to discontinue MMF because of significant adverse effects.
n/N, no. of patients who met the criteria/no. of patients who earlier had been on IMT.
In the remaining 14 patients (26.9% of the study population), MMF was either ineffective as a monotherapy or was poorly tolerated shortly after it was commenced. Three patients required chronic topical corticosteroids (regimen ranged from b.i.d. to q.i.d.) and one patient required both topical and oral corticosteroids (t.i.d. and 5 mg/day, respectively) in addition to MMF to keep her uveitis in quiescence. In six patients, MMF had some degree of disease control but was deemed insufficient, and thus either concomitant IMTs were not discontinued subsequently or additional IMTs were added (two cyclosporine, one infliximab, one cyclosporine plus infliximab, one adalimumab, one daclizumab). In the four remaining patients, MMF was altogether replaced by another IMT (one MTX, one infliximab, two chlorambucil).
Visual outcomes
While being treated with MMF, only three patients (one with unilateral disease and two with bilateral disease) experienced significant vision loss (defined as a drop of 2 or more Snellen chart lines) in one eye each. The reasons for the decreased vision were cataract in one of the patients and macular oedema in the other two. The visual acuity either remained stable or improved in the remaining 49 patients (94.2%).
Adverse effects
In total, 23 patients (44.2%) reported a total of 29 adverse effects from MMF, which are shown in Table 4. Gastrointestinal (GI) disturbance was the most common, with a rate of 0.12/person-year. The median time taken to develop the adverse effects was 5 months (range: 0.5–24) after MMF was initiated. A total of 10 patients (19.2%) reported adverse effects from MMF that were significant enough to impair daily functioning. The complaints resolved following MMF dosage decrease in four patients, without accompanying uveitis relapse. In the other six patients (11.5%), the adverse effects persisted despite dosage decrease and thus MMF was discontinued.
Table 4. Adverse effects of mycophenolate mofetil monotherapy.
| Adverse effects | No. affected (% of study population) | Ratea | 95% CI |
|---|---|---|---|
| Any complication | 29 (55.8) | 0.32 | 0.22–0.46 |
| GI disturbance | 11 (21.2) | 0.12 | 0.06–0.22 |
| Fatigue | 6 (11.5) | 0.07 | 0.02–0.14 |
| Leukopeniab | 5 (9.6) | 0.06 | 0.02–0.13 |
| Pneumonia | 2 (3.8) | 0.02 | 0.003–0.08 |
| Musculoskeletal pain | 2 (3.8) | 0.02 | 0.003–0.08 |
| Headache | 1 (1.9) | 0.01 | 0.0003–0.06 |
| Oral ulcer | 1 (1.9) | 0.01 | 0.0003–0.06 |
| Mood swing | 1 (1.9) | 0.01 | 0.0003–0.06 |
| Significant adverse effects reversed upon dosage decrease | 4 (7.7) | 0.04 | 0.01–0.11 |
| Therapy discontinued because of significant reactions | 6 (11.5) | 0.07 | 0.02–0.14 |
Abbreviations: CI, confidence interval; GI, gastrointestinal.
Defined as number of events per person-year at risk.
Defined as WBC <3500/mm3.
Discussion
To date, several studies have included children in their study population while investigating the use of MMF in ocular inflammatory diseases.23,24,25,26,27,28 The results of these studies, however, do not specifically address the effectiveness and safety of MMF in children. Before the present report, the effectiveness of MMF exclusively in treatment of paediatric uveitis had only been demonstrated in the case series study of 17 children conducted by Doycheva et al.29
In support of that previous work, our data suggest that MMF monotherapy is an effective steroid-sparing treatment in paediatric autoimmune uveitis. Approximately half of our patients (25/52, or 48.1%) met our definition of Durable Disease Control; another nine patients had gained excellent inflammation control at the last follow-up, although they had yet to meet the 2-year mark; finally, four patients were able to achieve inflammation control on MMF monotherapy, although they had to discontinue the medication subsequently because of significant adverse effects. These 13 patients thus fell under the subgroup of Short-term Inflammation Control. Combining the two subgroups, approximately three-quarters of the study population (38/52, or 73.1%) were able to achieve uveitis control for some period of time on MMF monotherapy. Of note, the need for any dosage of concurrent corticosteroids and/or other immunomodulatory agents would disqualify a patient from either subgroup. Overall, it took 2 months for MMF to control inflammation in these patients.
Visual acuity was not used as a primary outcome measure in this study. Nevertheless, during the follow-up period, only three patients (5.8%) in our study experienced significant vision loss (defined as a drop of ≥2 Snellen chart lines) in one eye each. The visual acuity either remained stable or improved in the remaining 49 patients (94.2%). These data suggest that if inflammation is controlled with MMF, the majority of patients will have stable or improved vision.
Our observation that GI disturbances and leukopaenia were common adverse effects of MMF is comparable to previous reports.23,24,25,26,27,28,29,30 In the present study, it took about 5 months to develop these adverse effects while on MMF therapy. In about one-fifth of the study population, the adverse effects were significant, but a decrease in MMF dosage was able to bring the effects under control in approximately half of these patients. More importantly, in each of these patients, dosage decrease did not lead to uveitis relapse. Only about 12% of the study population had to stop MMF completely because of intolerable adverse effects.
This retrospective study is limited by its lack of a control group, small study population, and variable follow-up time. The ascertainment of time to inflammation control and adverse effects was undoubtedly influenced by the study's retrospective nature. However, the patients in this study were evaluated both ophthalmically and hematologically every 6 weeks; hence, it is likely that the timing was accurate to within that time frame. In addition, in our assessment of MMF monotherapy in uveitis control, we attempted to circumvent the problem of variable follow-ups by defining the two subgroups of Durable Disease Control and Short-term Inflammation Control, thereby demonstrating the therapy's effectiveness in patients with both shorter and longer follow-ups alike. This was by no means perfect in dealing with the variable follow-ups, as some patients in Short-term Inflammation Control would have likely been categorised under Durable Disease Control if the follow-up were longer. Nevertheless, this cross-sectional analysis offers a glimpse at what MMF monotherapy was able to accomplish in our study population. Moreover, variable follow-ups especially affect one's ability to evaluate a medication's safety profile, and we compensated for this by presenting the frequencies as well as the rates (in terms of person-year) of adverse effects in our study population. In addition, our centre is a tertiary uveitis referral centre, and thus there is a potential bias towards those patients with more stubborn diseases. Despite these limitations, we have chosen to present these data because the results are very impressive in that MMF without any concurrent corticosteroids and/or immunomodulatory agents was able to induce inflammation control in many of the study patients. We believe that experts who deal with paediatric uveitis regularly may benefit from using MMF as part of the therapeutic repertoire.
In summary, our results suggest that MMF monotherapy is an effective steroid-sparing strategy in paediatric autoimmune uveitis. It was able to induce control of uveitis in nearly three-quarters of the study population, without the need for any concurrent corticosteroid and/or other immunomodulatory agents. It also appeared to be tolerated well in this population. We believe that MMF represents a good alternative in children who have failed MTX as the first-line IMT or are not suitable candidates for MTX. MMF may also be effective in those with diseases unresponsive to calcineurin inhibitors and biological response modifiers, although more data are needed to assess this.
The authors declare no conflict of interest.
Footnotes
This study was presented as a poster at the Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting in May 2009.
References
- Boer J, Wulffraat N, Rothova A. Visual loss in uveitis of childhood. Br J Ophthalmol. 2003;87:879–884. doi: 10.1136/bjo.87.7.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg KD, Feuer WJ, Davis JL. Ocular complications of paediatric uveitis. Ophthalmology. 2004;111:2299–2306. doi: 10.1016/j.ophtha.2004.06.014. [DOI] [PubMed] [Google Scholar]
- Holland GN, Stiehm ER. Special considerations in the evaluation and management of uveitis in children. Am J Ophthalmol. 2003;135:867–878. doi: 10.1016/s0002-9394(03)00314-3. [DOI] [PubMed] [Google Scholar]
- Holz FG, Krastel H, Breitbart A, Schwarz-Eywill M, Pezzutto A, Völcker HE. Low-dose methotrexate treatment in noninfectious uveitis resistant to corticosteroids. Ger J Ophthalmol. 1992;1:142–144. [PubMed] [Google Scholar]
- Dev S, McCallum RM, Jaffe GJ. Methotrexate treatment for sarcoid-associated panuveitis. Ophthalmology. 1999;106:111–118. doi: 10.1016/S0161-6420(99)90011-8. [DOI] [PubMed] [Google Scholar]
- Kremer JM. Methotrexate and emerging therapies. Clin Exp Rheumatol. 1999;17 (6 Suppl 18:S43–S46. [PubMed] [Google Scholar]
- Wallace CA. The use of methotrexate in childhood rheumatic diseases. Arthritis Rheum. 1998;41:381–391. doi: 10.1002/1529-0131(199803)41:3<381::AID-ART2>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- Foeldvari I, Wierk A. Methotrexate is an effective treatment for chronic uveitis associated with juvenile idiopathic arthritis. J Rheumatol. 2005;32:362–365. [PubMed] [Google Scholar]
- Heiligenhaus A, Mingels A, Heinz C, Ganser G. Methotrexate for uveitis associated with juvenile idiopathic arthritis: value and requirement for additional anti-inflammatory medication. Eur J Ophthalmol. 2007;17:743–748. doi: 10.1177/112067210701700509. [DOI] [PubMed] [Google Scholar]
- Kingdon EJ, McLean AG, Psimenou E, Davenport A, Powis SH, Sweny P, et al. The safety and efficacy of MMF in lupus nephritis: a pilot study. Lupus. 2001;10:606–611. doi: 10.1191/096120301682430186. [DOI] [PubMed] [Google Scholar]
- Sollinger HW, US Renal Transplant Mycophenolate Mofetil Study Group Mycophenolate mofetil for the prevention of acute rejection in primary cadaveric renal allograft recipients. Transplantation. 1995;60:225–232. doi: 10.1097/00007890-199508000-00003. [DOI] [PubMed] [Google Scholar]
- European Mycophenolate Mofetil Cooperative Study Group Placebo-controlled study of mycophenolate mofetil combined with cyclosporin and corticosteroids for prevention of acute rejection. Lancet. 1995;345:1321–1325. [PubMed] [Google Scholar]
- Tricontinental Mycophenolate Mofetil Renal Transplantation Study Group A blinded, randomized clinical trial of mycophenolate mofetil for the prevention of acute rejection in cadaveric renal transplantation. Transplantation. 1996;61:1029–1037. [PubMed] [Google Scholar]
- Smith JM, Nemeth TL, McDonald RA. Current immunosuppressive agents in paediatric renal transplantation: efficacy, side-effects and utilization. Pediatr Transplant. 2004;8:445–453. doi: 10.1111/j.1399-3046.2004.00209.x. [DOI] [PubMed] [Google Scholar]
- Dipchand AI, Benson L, McCrindle BW, Coles J, West L. Mycophenolate mofetil in paediatric heart transplant recipients: a single-center experience. Pediatr Transplant. 2001;5:112–118. doi: 10.1034/j.1399-3046.2001.005002112.x. [DOI] [PubMed] [Google Scholar]
- Van Mourik ID, Kelly DA. Immunosuppressive drugs in paediatric liver transplantation. Paediatr Drugs. 2001;3:43–60. doi: 10.2165/00128072-200103010-00004. [DOI] [PubMed] [Google Scholar]
- Filler G, Hansen M, LeBlanc C, Lepage N, Franke D, Mai I, et al. Pharmacokinetics of mycophenolate mofetil for autoimmune disease in children. Pediatr Nephrol. 2003;18:445–449. doi: 10.1007/s00467-003-1133-1. [DOI] [PubMed] [Google Scholar]
- Rao VK, Dugan F, Dale JK, Davis J, Tretler J, Hurley JK, et al. Use of mycophenolate mofetil for chronic refractory immune cytopenias in children with autoimmune lymphoproliferative syndrome. Br J Haematol. 2005;129:534–538. doi: 10.1111/j.1365-2141.2005.05496.x. [DOI] [PubMed] [Google Scholar]
- Moudgil A, Bagga A, Jordan SC. Mycophenolate mofetil therapy in frequently relapsing steroid-dependent and steroid-resistant nephrotic syndrome of childhood: current status and future directions. Pediatr Nephrol. 2005;20:1376–1381. doi: 10.1007/s00467-005-1964-z. [DOI] [PubMed] [Google Scholar]
- Novak I, Frank R, Vento S, Vergara M, Gauthier B, Trachtman H. Efficacy of mycophenolate mofetil in paediatric patients with steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2005;20:1265–1268. doi: 10.1007/s00467-005-1957-y. [DOI] [PubMed] [Google Scholar]
- Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature (SUN) Working Group Standardization of uveitis nomenclature for reporting clinical data: results of the First International Workshop. Am J Ophthalmol. 2005;140:509–516. doi: 10.1016/j.ajo.2005.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussenblatt RB, Palestine AG, Chan CC, Roberge F. Standardization of vitreal inflammatory activity in intermediate and posterior uveitis. Ophthalmology. 1985;92:467–471. doi: 10.1016/s0161-6420(85)34001-0. [DOI] [PubMed] [Google Scholar]
- Thorne JE, Jabs DA, Qazi FA, Nguyen OD, Kempen JH, Dunn JP. Mycophenolate mofetil therapy for inflammatory eye disease. Ophthalmology. 2005;112:1472–1477. doi: 10.1016/j.ophtha.2005.02.020. [DOI] [PubMed] [Google Scholar]
- Siepmann K, Huber M, Stübiger N, Deuter C, Zierhut M. Mycophenolate mofetil is a highly effective and safe immunosuppressive agent for the treatment of uveitis: a retrospective analysis of 106 patients. Graefes Arch Clin Exp Ophthalmol. 2006;244:788–794. doi: 10.1007/s00417-005-0066-8. [DOI] [PubMed] [Google Scholar]
- Sobrin L, Christen W, Foster CS. Mycophenolate mofetil after methotrexate failure or intolerance in the treatment of scleritis and uveitis. Ophthalmology. 2008;115:1416–1421. doi: 10.1016/j.ophtha.2007.12.011. [DOI] [PubMed] [Google Scholar]
- Baltatzis S, Tufail F, Yu EN, Vredeveld CM, Foster CS. Mycophenolate mofetil as an immunomodulatory agent in the treatment of chronic ocular inflammatory disorders. Ophthalmology. 2003;110:1061–1065. doi: 10.1016/S0161-6420(03)00092-7. [DOI] [PubMed] [Google Scholar]
- Teoh SC, Hogan AC, Dick AD, Lee RW. Mycophenolate mofetil for the treatment of uveitis. Am J Ophthalmol. 2008;146:752–760. doi: 10.1016/j.ajo.2008.03.004. [DOI] [PubMed] [Google Scholar]
- Daniel E, Thorne JE, Newcomb CW, Pujari SS, Kaçmaz RO, Levy-Clarke GA, et al. Mycophenolate mofetil for ocular inflammation. Am J Ophthalmol. 2010;149:423–432.e1-2. doi: 10.1016/j.ajo.2009.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doycheva D, Deuter C, Stuebiger N, Biester S, Zierhut M. Mycophenolate mofetil in the treatment of uveitis in children. Br J Ophthalmol. 2007;91:180–184. doi: 10.1136/bjo.2006.094698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okada AA. Immunomodulatory therapy for ocular inflammatory disease: a basic manual and review of the literature. Ocul Immunol Inflamm. 2005;13:335–351. doi: 10.1080/09273940590951034. [DOI] [PubMed] [Google Scholar]


