Figure 15.
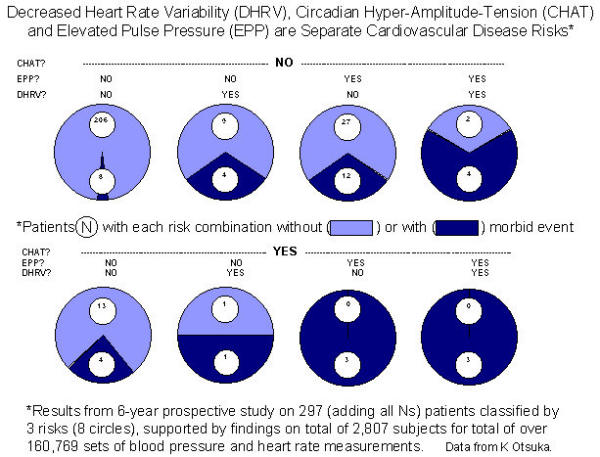
The incidence of morbidity among 121 normotensive and 176 treated hypertensive patients (so diagnosed by their time structure or chronome-adjusted mean, MESOR) with no cardiovascular disease at the outset is compared in a 6-year prospective study among patients presenting without or with 1, 2 or all 3 of 3 risks factors. The risk factors considered are:1. CHAT (brief for circadian hyper-amplitude-tension), a condition characterized by an excessive circadian amplitude of (diastolic) blood pressure (above the upper 95% prediction limit of clinically healthy peers of the same gender and a similar age);2. An elevated pulse pressure (EPP), defined as a difference between the MESORs of systolic and diastolic blood pressure above 60 mmHg; and 3. Decreased heart rate variability (DHRV), defined as a standard deviation of heart rate measurements at 15-min intervals for 48 hours in the lowest 7th percentile of the patient population. Risk was determined at the start of study, based on a 48-hour profile (acceptable for group studies only, one week's monitoring at 30-minute intervals being recommended for individuals) of automatic measurements of blood pressure and heart rate at 15-min intervals with an ambulatory monitor. Morbidity was checked about 6-monthly thereafter. Diagnoses considered were: coronary artery disease, cerebral ischemic events, nephropathy and retinopathy (related to blood pressure disorder). After 6 years, morbidity was diagnosed in 39 of the 297 patients. In the reference population of 214 patients presenting none of the 3 risk factors, morbidity was found in 8 cases (3.7%) (top left). The presence of DRHV or EPP alone raises the incidence of morbidity to 30.8% (top middle). When these two risks are both present, morbidity is doubled (66.7%) (top right). The presence of CHAT (bottom) invariably increases the incidence of morbidity, from 3.7% to 23.5% in the absence of the other two risk factors (bottom left), from 30.8% to 50% or 100% when either DHRV or EPP is also present (bottom middle), or from 66.7% to 100% when all 3 risk factors are present (bottom right). Except for a weak relation between pulse pressure and the standard deviation of heart rate, the 3 risk factors are mostly separate and additive. The results suggest the desirability to routinely assess blood pressure variability in addition to heart rate variability since even in MESOR-normotension, CHAT is associated with a statistically significant increase in cardiovascular disease risk (not shown) [8], and can be successfully treated [80]. Whereas the number of morbid events and the number of patients in this study are small, the results are supported by several other prospective and retrospective chronobiological investigations [8,38,78-82].
