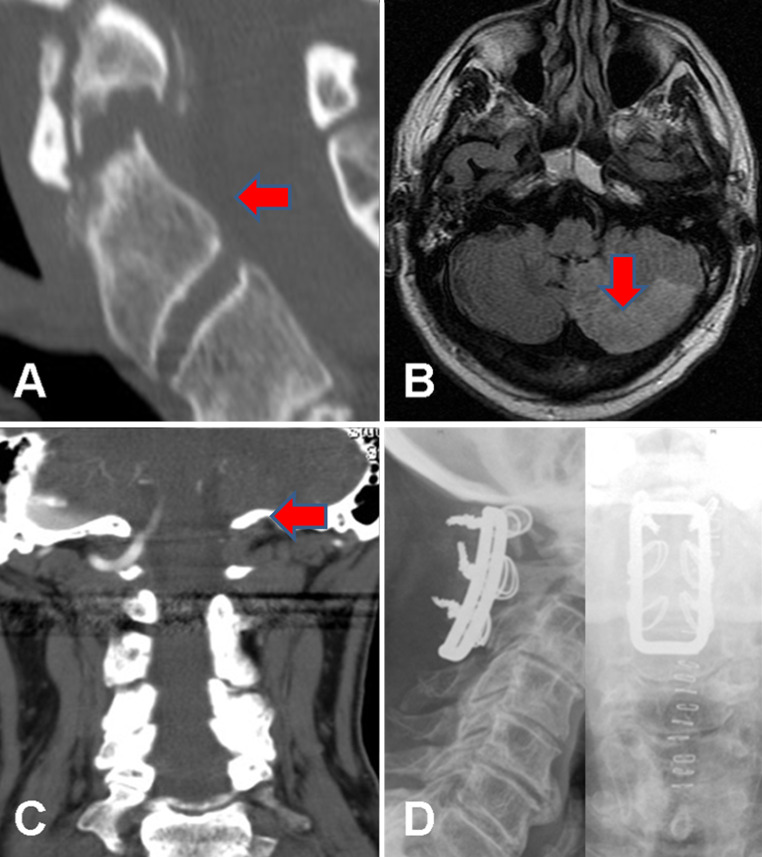
Fig. 2.
Images from a 64-year-old man who presented with acute vertigo and vomiting 2 weeks after a flexion–extension injury of his neck with continued neck pain. At the time of the injury, X-rays and a CT scan (a sagittal reformat) showed an unstable type 2 odontoid fracture, which was managed with a hard collar. An MRI (b axial FLAIR sequence) following admission with clinical features of a cerebellar ischaemic event 2 weeks later showed high signal in the left PICA territory compatible with acute infarction. A CT angiogram (c coronal maximum intensity projection) showed occlusion of the left vertebral artery arising from a dissection at the level of the C1/2 junction. He was managed with immediate anticoagulation using heparin, which was temporarily stopped after 3 days to allow surgery to stabilise the fracture via C1–C3 sublaminar wiring (d AP and lateral post-operative X-rays). He made a good recovery with rehabilitation and his anticoagulation was converted to warfarin, target INR 2–3, and then stopped after 6 months with no further adverse events