Abstract
Early intervention and prevention in schizophrenia is just over 10 years old. The assumption guiding this field is that intervention is likely to be most effective if it begins before psychosis sets in, ie, during the prodromal phase. Although a substantial number of prodromal treatment programs have been initiated around the world, three early programs have generated most of the intervention findings to date: Personal Assessment and Crisis Evaluation (PACE) in Australia, and the Prevention through Risk Identification, Management, and Education (PRIME) and Recognition and Prevention (RAP) programs in the USA. The data suggest that early intervention leads to a reduction in prodromal symptoms and clinical distress. However, prevention of psychosis remains an unresolved question. Other issues include defining who should be treated, with what, and when. In addition, treatment targets associated with functional disability, such as early prodromal negative symptoms and risk factors, continue to emerge. Newly identified targets, in turn, suggest the need for a variety of novel interventions and treatment strategies.
Keywords: prodrome, treatment, psychosis, prevention, early identification, schizophrenia
Abstract
La intervención precoz y la prevención de la esquizofrenia no tienen más de diez años. El supuesto que guía estas acciones alude a que la intervención resulta probablemente más efectiva si comienza previo a la instalación de la psicosis, es decir, durante la fase prodrómica. Aunque en diversas partes del mundo se han iniciado un número significativo de programas de tratamiento prodrómico, tres de ellos - hasta la fecha - han dado origen a la mayoría de los hallazgos de esta intervención: el Personal Assessment and Crisis Evaluation (PACE) en Australia, y los programas Prevention through Risk Identification, Management and Education (PRIME) y Recognition and Prevention (RAP) en Estados Unidos. Los resultados sugieren que la intervención precoz lleva a una reducción de los síntomas prodrómicos y del distrés clínico. Sin embargo, la prevención de la psicosis persiste como una pregunta sin resolver. Otro aspecto de esta revisión es la definición de quiénes deben ser tratados, con qué y cuándo. Además, continúan apareciendo objetivos terapéuticos que se asocian con incapacidad funcional como son los síntomas negativos prodrómicos precoces y los factores de riesgo. A su vez, síntomas blanco identificados recientemente sugieren la necesidad de una variedad de nuevas intervenciones y estrategias terapéuticas.
Abstract
La notion d'intervention précoce et de prévention dans la schizophrénie vient juste de dépasser 10 ans. L'hypothèse sous-tendant cette réflexion est probablement d'être plus efficace si l'on intervient avant l'installation de la psychose, par exemple, pendant la phase prodomique. Bien que de nombreux programmes de traitements prodromiques aient été débutés dans le monde entier, à ce jour, trois programmes d'intervention précoce sont à l'origine de la plupart des résultats: PACE (Personal Assessment and Crisis Evaluation,) en Australie, PRIME (Prevention through Risk Identification, Management and Education,) et RAP (Recognition and Prevention aux États-Unis. Les données suggèrent qu'une intervention précoce réduit les symptômes prodromiques et la souffrance clinique. Néanmoins, la prévention de la psychose demeure un problème non résolu. D'autres questions restent en suspens comme, qui devrait être traité? avec quoi et quand? De plus, les traitements ciblant l'incapacité fonctionnelle, comme les symptômes négatifs prodromiques précoces et les facteurs de risque, continuent à apparaître. Des cibles nouvellement identifiées font ressentir à leur tour le besoin de diverses nouvelles interventions et stratégies thérapeutiques.
A decade ago, the schizophrenia prevention movement was launched with great expectations. At that time, a handful of treatment studies began, founded more on enthusiasm, Intuition, and Indirect findings than on a solid base of evidence. Today, though still In Its Infancy, the field thrives. Early Intervention programs have dramatically proliferated around the world, and the data, though still sparse, are nonetheless quite encouraging. The target of these studies Is the schizophrenia “prodrome,” which refers to the phase of illness that precedes the onset of psychosis. Treatment, to date, has been largely pharmacological, although at least one major psychotherapy trial has now begun in the United Kingdom.1 In this paper, we will review the treatment findings currently available that address the following basic issues: (i) what should be treated; (ii) when should treatment be initiated; and (iii) how long should treatment last. First, we begin with why: why begin treatment prior to psychosis, the stage of illness that defines schizophrenia?
Why treat the prodromal phase of schizophrenia?
Initially, the prevention movement gained early momentum from the convergence of two, very separate, research traditions. The first of these established the neurodevelopmental view of schizophrenia, now widely accepted throughout the field. This model provides the logic of early intervention. The second tradition is far more empirical, and is based on increasing evidence that early treatment, initiated as close after onset of psychosis as possible, appears to improve outcome. It thus follows from these findings that treatment started before onset might be better still.
The neurodelopmental model
The currently accepted view of schizophrenia holds that it is a gradually unfolding illness, one that has its roots in prenatal development. Though the evidence is indirect, it is believed that a genetic error of some kind (most likely in interaction with other biological and environmental factors) leads to subtle abnormalities in the evolving brain. The resulting pathophysiology is not, in itself, schizophrenia, but rather a susceptibility or vulnerability to the disorder. Subtle vulnerability indicators can be detected throughout late childhood and early adolescence (eg, cognitive impairments, social difficulties), but the underlying disturbance begins to fulminate toward midadolescence, when clinical warning signs (ie, attenuated positive symptoms) become increasingly apparent. A number of models, differing from each other mainly in details, have been derived from this basic set of assumptions.2-10
The neurodevelopmental model is widely supported by both genetic high-risk prospective and birth cohort follow-back studies. In particular, genetic high-risk studies have implicated early cognitive and social skill deficits in young at-risk offsprings of schizophrenic parents who later become ill.11-14 Follow-back studies, such as the British15,16 and Finnish birth cohorts,17 and the large population Swedish conscripts18,19 and Israeli army studies,7 have consistently reported a diversity of cognitive, social, and other developmental precursors to schizophrenia. The application of the neurodevelopmental view to prevention is threefold: first, this model depicts the clinical illness as a long-term, developmental process. As a result, intervention is viewed as being possible well before psychosis sets in, and thus, as having the potential to stop continued progression to illness. Second, the proposed presence of a detectable, biological vulnerability provides the mechanism for early detection. In order to begin preventive treatment prior to illness onset, there must be a way to identify who is in need of intervention. Prodromal vulnerability indicators provide the means to identify those individuals who are at risk for illness. It should be noted that this represents a major advance, since risk has traditionally been a group construct, not definable on an individual level. Third, the course of the prodromal phase of illness and the emergence of deficits point to type of treatment, in indicating the actual targets for treatment (eg, cognition, depression, social anxiety) and when it should begin (early versus late prodrome).
Early treatment findings and the duration of untreated psychosis
Clinical researchers have long noted that many patients with psychosis appear to experience a prodromal phase characterized by alterations in perception and changes in behavior.20-22 As early as 1927, Sullivan observed that ”The great number of our patients have shown for years before the break, clear signs of coming trouble...23 Similarly, Meares22 maintained, “What is needed is not the early diagnosis of schizophrenia, but the diagnosis of prepsychotic schizophrenia.” Despite the widespread clinical recognition of the prodrome, little attention had been directed at this phase of illness until recently, most likely because prevention was not possible. Recent interest has developed and increased with the availability of potential treatment tools: antipsychotic (AP) medication. The importance of early treatment was first suggested by Wyatt et al,24-26 who provided indirect evidence suggesting that the earlier medication was initiated after onset of schizophrenia, the better the outcome, thus suggesting that psychosis itself is toxic to the brain. The association of the duration of untreated psychosis (or DUP) with prognosis has since been supported by a substantial number of studies27,28 (although there are contradictory findings29-31) and has often been cited to suggest that treatment initiated before onset is likely to lead to the best outcome.32,33 The introduction of second-generation APs (SGAPs) with an apparently reduced side-effect profile contributed significantly to the feasibility and ethicality of such early treatment studies. As a result, though less than a decade old, early intervention and prevention studies have now spread throughout the world.34,35
What should be treated?
The issue of what should be treated is highly complex at this stage of research. Since the field is young and continues to evolve, the natural course of the prodrome is not well established and the population continues to be “at risk” rather than to consist of affected patients with a definite syndrome.6,35 As a result, there is some disagreement throughout the field as to what symptoms to treat, and what the short- and long-term treatment goals should be. Rates of conversion to psychosis among prodromal individuals range from 20% to 45%, depending on how the prodrome is defined and measured.36-38 This complicates interpretation of treatment findings and raises the question as to whether emphasis should be directed to prevention (ie, lowering the incidence rates) or reducing functional disability, often present in at-risk individuals regardless of whether psychosis has emerged. Thus far, treatment has primarily targeted attenuated positive symptoms that occur relatively late in the prodrome. Only a minimum of attention has been directed toward treatment of earlier, negative symptoms, identified by previous high-risk and follow-back studies15-19 to be the earliest risk factors of illness. This is an important oversight, since these early deficits appear to be most closely associated with the functional disability (ie, inability to work independently, social isolation) that is thought to restrict prognosis more directly than psychosis, in itself.39,40 Thus, a major research goal, at present not widely recognized, should be to determine whether negative risk factors and deficits can be reduced with early treatment, and, if doing so has in turn the potential to improve functional outcome.
Because of the many unresolved issues characterizing the treatment of the prodromal phase, the questions asked tend to vary widely from site to site. Although the potential for answers is considerable, there are few definitive findings available,41 and the data that do exist are quite variable. Falloon42 conducted the first attempt at prevention using AP medication in a study in rural Britain. In this project, family practitioners were educated to identify prodromal individuals using Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM-III-R) prodromal criteria and to refer these patients to a multidisciplinary early intervention team. Sixteen individuals meeting entry criteria were provided intensive stress management and family psychosocial intervention and were treated with low-dose neuroleptic medication when necessary The results of these efforts suggested that early intervention reduced conversion rates (compared to those previously recorded in the catchment area), although these findings were not considered to be conclusive because the study was conducted under uncontrolled conditions.
Following Falloon, prodromal programs were established in Melbourne, Australia (Personal Assessment and Crisis Evaluation [PACE] clinic),37,43 and in the USA in Connecticut (Prevention through Risk Identification, Management, and Education [PRIME] clinic)44 and New York (Recognition and Prevention [RAP] program),4-6 At present, findings are thus far largely limited to these three original prodromal programs. Although there are some commonalities, each of these programs has adopted different research and treatment strategies. For example, both the McGorry and McGlashan treatment groups (PACE and PRIME clinics) focus on randomized clinic trials. Starting from a very different perspective, Cornblatt et al (RAP program) report findings from a prospective naturalistic study, which is as much concerned with defining risk factors as with treatment. Each of these programs will be described separately
PACE clinic randomized clinical trial
Researchers in the PACE clinic,45,46 which is part of the Early Psychosis Prevention and Intervention Center (EPPIC) program43 in Melbourne, Australia, were the first group to focus on the schizophrenia prodrome in a series of systematic, controlled studies. As a result, this group has conducted much of the groundbreaking conceptual and early research that jump-started the field. Although new trials are underway in the PACE clinic, to date, the major treatment findings have resulted from the original randomized clinical trial (RCT)47 in which a study group receiving low-dose risperidone combined with cognitive behavioral therapy (CBT) was compared with a “needs-based” treatment control group. This was the first randomized, controlled intervention trial conducted in prodromal individuals.
Patients were between 14 and 30 years and met any one or more of three criteria, considered to define “ultra high-risk” (UHR):
Attenuated psychotic symptoms defined as subthreshold attenuated positive symptoms that do not reach psychotic intensity yet represent distinct departures from normal experience.
Brief limited intermittent psychotic symptoms (BLIPS), defined as the presence of infrequent or intermittent psychotic level symptoms of a duration < 1 week, that spontaneously remit.
Trait and state risk factors defined as the presence of psychosis or schizotypal personality disorder in a firstdegree relative or schizotypal personality disorder in the identified patient, and a decrease in functioning that is sustained for 1 month.
Conversion to psychosis, the outcome of interest, is defined as meeting the criteria for a brief limited psychosis for longer than 1 week.
The trial compared a needs-based intervention (NBI, the control condition) with a specific preventive intervention (SPI). The NBI consisted of a focused supportive psychosocial intervention. The SPI combined 1 to 2 mg risperidone with a modified CBT program, in addition to focused supportive intervention. Interventions were provided for 6 months, after which patients in both groups received 6 months of NBI. Treatment was augmented with antidepressants (ADs) and benzodiazepines when necessary in both groups.
Fifty-nine high-risk subjects were randomized and some differences were found between the groups in terms of use of ADs (NBI>SPI) and number of therapy sessions received (SPI>NBI). At 6 months, the rate of conversion to psychotic illness (not necessarily schizophrenia) was significantly higher in the control (NBI) group (36%, 10/28) than the early intervention (SPI) group (10%, 3/31). However, this difference did not hold up at the 1-year mark (36% NBI versus 19% SPI).
If adherence to medication was considered, those who were fully compliant with the intervention procedures in the SPI group were significantly less likely to convert than those in the NBI group at both 6 and 12 months. However, these findings are not conclusive since more than half of the subjects in the SPI group were less than fully compliant with medication. All participants showed symptom improvement across the study including converters (who received treatment immediately, a major advantage of participating in the study) and few adverse effects were reported. However, functional levels remained relatively unchanged, which may indicate that more intensive or longer duration of intervention is needed to elevate global functioning. These findings suggest that short-term treatment can delay psychosis. The authors conclude that the number needed to treat (NNT) of four (ie, four individuals would need to be treated in order to prevent conversion in one) supports continued prodromal trial research. More clarity is expected from a 12-month, randomized, controlled trial initiated in the PACE clinic in 2000, in which risperidone plus CBT will be compared with placebo plus CBT, and with placebo plus befriending.
PRIME clinic randomized double-blind study
McGlashan et al44 at Yale initiated the first double-blind, placebo trial for prodromal patients in 1997. After additional sites were added, 60 subjects were enrolled in the project with 30 randomized to receive olanzapine (5 to 15 mg) and 29 to receive placebo. Medication or placebo was given for 1 year and patients were followed for an additional year. Inclusion criteria were based on the Yung UHR categories, but operationalized by the PRIME prodromal assessment tool, the Scale of Prodromal Symptoms (SOPS).48,49 Conversion to psychosis, defined by this group as any positive symptom at psychotic intensity on SQPS that was of sufficient frequency duration, or was seriously disorganizing or dangerous, warranted removal from the trial and open-label olanzapine was initiated for 6 months. Supportive psychosocial interventions were available for all patients, but effort was made to limit the use of concomitant psychoactive medications. Results analyzed by principal mixed-effects model after 8 weeks of treatment revealed that the olanzapine group showed significant improvement from baseline on SOPS total score, positive symptom scale, negative symptom scale, and disorganized symptom scale. The placebo group did not show any significant change on any scale at any time point. Olanzapine versus placebo group differences were found by week 8 on the SOPS total, negative, and disorganized scales, but not the positive symptom scale. Positive and Negative Symptoms Scale (PANSS) total and positive symptom scores also showed significant differences between the olanzapine and placebo groups. Weight gain was the only side effect reported significantly more often in the olanzapine group, with over 50% of this group gaining more than 7% of their baseline body weight (versus 3% in placebo group).36 Patients receiving olanzapine showed significant within-group improvements on positive symptom scores and a trend toward greater improvement when compared to the placebo group, demonstrating the efficacy of olanzapine over placebo in the treatment of attenuated positive symptoms. Although conversion rates in the placebo group (34%, 10/29) were higher that those in the olanzapine group (16%, 5/31) after 1 year of active treatment, this difference did not reach statistical significance.50 Thus, while results of both the PACE and PRIME studies support the short-term benefits of early treatment, prevention continues to be an open question.41
RAP program naturalistic prospective study
A very different approach has been adopted in the RAP program. Prior to any type of formal treatment trial, the RAP program has been designed to collect data about the longitudinal progression of symptoms and functioning within a naturalistic treatment framework. In this context, psychosocial and pharmacological interventions are provided according to the physician's choice, based on best practice guidelines. This strategy thus provides real world treatment information, which is currently unavailable, especially naturalistic conversion rates. It also provides an initial evidence base to inform the design of treatment trials. Considered as a high-risk study, initial RAP goals are to identify the critical risk factors defining the prodrome; longer-term goals are to evaluate the changes in these deficits associated with treatment.
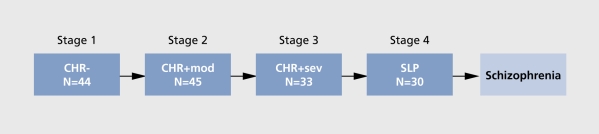
A critical component of the RAP program approach is to cast a wide net to identify patients in various stages of the prodrome. Selection criteria are directly derived from our neurodevelopmental model, which has evolved over several years. The resulting working diagnostic model is presented in (Figure 1).
Figure 1. Expanded four box model. CHR-: clinical high risk-negative; CHR+mod: clinical high risk-positive moderate; CHR+sev: clinical high risk-positive severe; SLP: schizophrenia-like psychosis.
In the diagnostic schema in Figure 1, the term “clinical high risk” (CHR) is substituted for “prodromal”; sample sizes shown in each of the boxes are current as of 1 July 2004. Stage 1 of this diagnostic schema consists primarily of negative-type symptoms (eg, increasing social isolation, school failure, depression) and is referred to as CHR-negative or CHR-. The CHR- stage is followed by the gradual emergence of positive symptoms, which first appear in mild-to-moderate attenuated form (CHR+mod; stage 2), and then increase in severity (CHR+sev; stage 3), although still not of psychotic intensity. In many cases, these positive symptoms evolve into psychosis, though not necessarily meeting criteria for schizophrenia. Presence of only one positive symptom of psychotic intensity is considered stage 4 in the model and is referred to as schizophrenia-like psychosis (or SLP). The sequence is therefore CHR - > CHR+mod - > CHR+sev - > SLP The end point of this process is proposed, in many though not all, cases to be full-blown schizophrenia. This model is designed to focus on the course of development, a process that is not yet well understood.51 Aside from providing a number of entry points into the prodrome, this model also provides a structure for developing and evaluating stage-specific interventions. For example, early treatment data, to be discussed in later sections, suggest that, for the early stages of the prodrome, ADs are associated with a much higher level of adherence in adolescents and appear equally as effective for symptom control as APs. Thus, our focus is on identifying the optimal intervention during each prodromal stage.
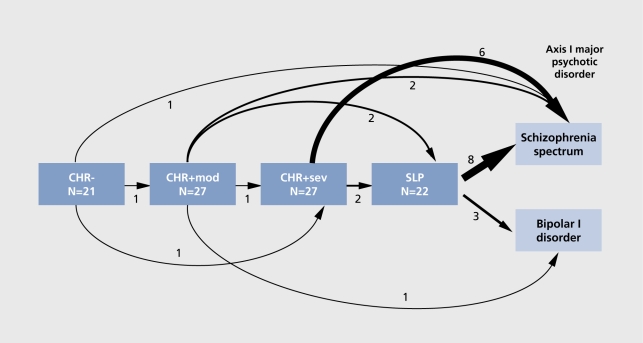
Data from the RAP program concur with the McGorry and McGlashan groups in that our prodromal population is treatment-seeking, highly symptomatic at baseline, and generally benefits from intervention.52 Overall, the conversion rate within the RAP program across subjects with follow-up of at least 6 months is 20%. Consistent with our recruitment strategy and focus on the very early stages of the prodrome, our conversion rate is at the low end of the spectrum. However, when looked at more closely as a function of the RAP theoretical model, the pattern of clinical deterioration for the 97 subjects who, to date, have been followed for at least 1 year (mean follow-up 2.4 years) is highly consistent with our developmentally based expectations. These results are presented in (Figure 2).
Figure 2. Preliminary outcome. Within each box are included those subjects who received that classification at study entry and who also have 1 year of follow-up. Arrows represent outcome as of a 1 June 2004 cutoff date. CHR-: clinical high risk-negative; CHR+mod: clinical high risk-positive moderate; CHR+sev: clinical high risk-positive severe; SLP: schizophrenia-like psychosis.
Within each box are included those subjects who received that classification (ie, CHR-, CHR+mod, etc) at study entry and who also have at least 1 year of followup. Arrows represent outcome as of a 1 June 2004 cutoff date, though only the final outcome is represented (ie, intermediate shifts not shown). This preliminary longitudinal data provide some very early support for our developmental model indicating that rates of conversion will increase as subjects progress across prodromal stages from CHR- to SLR This figure also presents the rates of broadly defined clinical deterioration from any given prodromal stage to a more severe one. As indicated by the figure, frequency of clinical deterioration shows a gradual increase from CHR- (14%) to CHR+mod (22%) to CHR+sev (30%) to SLP (50%).
Naturalistic findings indicate that early treatment may be more complex than typically assumed, in that APs are not necessarily first-line choice in best-standards practice. For those participants in the CHR+ category (which are comparable to the prodromal groups treated by both the McGorry and McGlashan groups), psychiatrists in the RAP program prescribed AD medication as often as AP medication. Furthermore, those on ADs generally did as well as those on APs (all SGAPs),52 This finding has led to initiation of a 16-week, double-blind, double-dummy study of an SGAP (risperidone) versus a typically used AD (sertraline), which is currently underway. Goals of the project are to determine the efficacy of the two classes of medication on symptom reduction and to determine if there is a differential rate of conversion between the groups. Conversion in the study will reflect psychotic symptoms at a high enough frequency and duration to meet Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for a specific psychotic disorder (eg, schizophrenia, schizoaffective, or delusional disorder).
Treating functional disability
Preventing conversion to psychosis is the primary goal of early intervention. However, given the current fluctuation in conversion rates and the small number of subjects who convert in any given study, the collection of conclusive data indicating the success of current interventions using AP medication is a long-term goal and may require several multisite studies.53 Conversion rates can vary dramatically even within a single site. Yung et al,37 for example, reported a conversion rate of 21% (7/33) after an initial 12 months of follow-up, but then, in another sample with refined inclusion criteria, found a 40.8% (20/49) conversion rate at 12 months' follow-up, with 28.5% of the sample converting to schizophrenia or schizoaffective disorder and the balance converting to affective psychoses or brief/unspecified psychosis. Differences in rates are also dependent on how the end point is defined. For example, in the PACE study, outcome is psychosis; in the RAP program, the outcome is schizophrenia, and psychosis is considered to be an intermediate state (represented by the SLP group) with an unclear final outcome. A second, very important direction, however, is the treatment of risk factors and the long-term functional outcome they are associated with; this is a major component of the naturalistic research design of the RAP program. Early risk factors include subtle deficits in cognition, social skills, and school performance, which have been shown both in affected patients and in youngsters at risk to lead to social isolation and poor vocational skills in adulthood. 39,40,52,54,55 According to our theoretical neurodevelopmental model, such core risk factors reflect a vulnerability to later illness and are thought to be early, stable manifestations of underlying brain abnormalities. Early risk factors are of particular interest in an intervention context to the extent that they can be modified by treatment. Our basic hypothesis is that the early treatment of such risk factors will impact the progression of illness and hopefully prevent (or, at least greatly reduce) psychosis and functional disability.
In the RAP program, we have thus far focused on four possible core domains, which appear to be early risk factors: cognitive deficits, affective disturbances, social isolation, and school functioning (referred to in our program as the CASIS cluster). In particular, social deficits and impaired school functioning are the symptoms most commonly reported across patient subgroups, with one or both reported by 94% of all prodromal subjects. In addition, these early childhood/adolescent deficits are thought to be directly related to the social and vocational deficits characteristic of many adults affected with schizophrenia.
Functional outcome domains have not yet received significant attention in the prodromal literature, which has focused almost exclusively on prevention of psychosis and related clinical symptomatology, as discussed above.47,56,57 However, longitudinal studies of affected patients with schizophrenia have repeatedly demonstrated that the long-term course of illness is marked by persistent impairment in community functioning, even when psychotic symptomatology is in remission.58-61 Of further significance, functional impairments, including cognitive, social and occupational/academic deficits are independent of psychotic symptoms. A major goal of the RAP program is to determine the extent to which early intervention will have an impact on these long-standing core deficits, thus improving long-term outcome.
Focus in the RAP program, therefore, has been increasingly directed to areas of functional outcome in addition to conversion to psychosis. Functional disability is both widespread in the prodromal population and very difficult to treat at present. Two areas of outcome are studied in depth: social isolation and deteriorating role functioning, which, in adolescents, refers to school performance. Preliminary outcome data indicate that social functioning is highly stable over time, whereas school performance appears to be more variable. Both of these areas are currently viewed as primary treatment targets in our program.
When to treat and what to treat with
At present, the prodrome is regarded as a unitary clinical entity by most researchers. The assumption that follows is that all patients meeting prodromal criteria should be treated at presentation using the same medication, ie, SGAPs. This choice results from at least two considerations: first, from the assumption that since APs are the best known way of treating affected psychotic patients, they will also be the best way to prevent psychosis from starting in the first place. Second, movement disorders such as tardive dyskinesia no longer appear to be as severe with SGAPs as with the preceding neuroleptics, thus reducing ethical issues involved in treating prepsychotic, at-risk individuals.62 APs are especially appropriate in studies that limit entry criteria to prodromal symptoms conceptually very close to onset of psychosis. As a result, the majority of the individuals in these samples are likely to be in the late prodromal stage and may not be representative of the prodromal period in general.
Early findings emerging from the RAP program have challenged several of the above assumptions to varying extents. First, as indicated by the developmental pattern of clinical deterioration shown above in Figure 2, the prodrome appears to consist of multiple stages, each of which may involve a different type of treatment. The pattern of deterioration shown preliminarily suggests that, rather than later in the prodrome, it might be more effective for intervention to begin in the CHR+mod stage, when symptoms are less severe and possibly more responsive to treatment. In addition, these early clinical findings suggest the importance of initiating some type of treatment at the CHR- stage, although this is likely to be psychosocial rather than pharmacological.
Following this model, the prodromal phase might be more broadly conceptualized as having an early period and a late period, each with different treatment requirements. In the early prodromal phase, affective symptoms and negative attenuated signs are beginning to emerge and to have some impact on age-dependent functioning. For example, in a large-scale retrospective study of prodromal schizophrenia conducted by Hafner and an der Heiden,63 depression and nonspecific symptoms including impairment in social functioning were evident up to 5 years before the onset of positive symptoms. These findings are mirrored in follow-back studies7,64,65 and genetic high-risk studies. 16,54,66 Furthermore, level of social/role functioning attained by onset of psychosis mediated social consequences 5 years later, indicating that successful intervention in the prodromal period could prevent developmental arrest in these areas.67 Medications other than APs may be most useful in treating these early phase deficits and behavioral problems. By contrast, the late prodromal phase is characterized by the development of attenuated positive symptoms that are the harbingers of psychosis. Retrospective reports indicate that although the early prodromal period of largely negative-type symptoms might last from weeks to years,28,68 there is a typically steep decline in the 6-month to 1-year period prior to onset.44 This suggests that APs might best be administered at the point of evident decline, as suggested by McGlashan and colleagues.44,69 Preliminary treatment findings from the RAP program support this developmental treatment perspective. The naturalistic treatment strategy of the RAP clinic, the independent treatment arm of the RAP program, involves the following: (i) treating clinicians are independent of the prodromal study research team; (ii) there are no research guidelines as to treatment; (iii) clinicians are asked to prescribe medication as they would in their private practice, ie, based on best practice guidelines for treatment of symptoms; and (iv) prevention is not taken into consideration. This has generated a rich database of observed treatment data.
The naturalistic treatment data collected over the early years of the RAP program has generated a consistent finding that has been repeated as the prodromal sample has continued to grow. As has been reported several times for patients with attenuated positive symptoms (eg, CHR+)4,5 on small, but increasing samples (with the most recent n=39), the major results are as follows:
Most adolescents with prodromal symptoms are treated with either SGAPs, with ADs (involving a range of selective serotonin reuptake inhibitors [SSRIs]), or with both.
There are no baseline differences in severity of either positive, negative, or depressive symptoms to account for the choice.
Prodromal youngsters treated with ADs do at least as well as those treated with SGAPs over about a 2-year follow-up period.
There is no difference in baseline symptoms, adherence, or outcome between adolescents receiving a combination of SGAP/AD vs SGAPs alone, thus questioning the need for polypharmacy.
Nonadherence to medication appears to be the single most important factor determining conversion to psychosis. Of the 13 prodromal adolescents who converted to psychosis over follow-up, 12 were nonadherent to medication (defined as off medication for 1 month or longer), which, in all cases, was an AP. Nonadherence thus confounds outcome, but suggests that ADs may be an option, since they appear effective clinically and, in comparison with APs, the rate of adherence is very high.
Although in no way conclusive, since naturalistic data are based on nonrandom assignment and are open-label, our initial findings raise several issues. Important among these is the issue of whether APs should be the first-line treatment choice for all prodromal individuals. At present, other possibilities are being explored both in the RAP program and in the other two prodromal programs (ie, PACE and PRIME).
Who long to treat?
There are currently no direct data to support how long treatment will be necessary, either for prevention of psychosis or to reduce functional disability. Previous studies typically lasted from 1 to 2 years. Additional information is also needed to guide researchers in optimal treatment trial duration. To date, treatment trials have been of relatively short duration, generally 6 to 12 months of active treatment with a year or two of followup. How long treatment should be provided is unknown at present. The results of the PRIME trial seem to indicate that symptom improvement is related to being actively medicated and, when medication is withdrawn, symptoms reemerge.70 Perhaps the duration of treatment was not long enough to change the course of the illness. In the RAP program, which, as discussed above, includes early stages of the prodrome, at least 35% of the conversions occurred during years 3 to 4 of the study. Moreover, all but one of the subjects in the RAP program who converted had been off medication for substantial periods of time. Risk for conversion was greatly increased by nonadherence. This suggests that sustained medication may be essential to stave off onset of psychosis. This finding in prodromal youngsters is consistent with the findings reported for first-episode patients, with risk for relapse increased fivefold when nonadherent with medication.31
Future directions
Now a decade into the early intervention work, there has been increased interest in broadening the focus to include interventions that target more than just positive symptoms, and include negative symptoms and functional disability It is clear that more information on the developmental course of the prodrome is needed to identify treatment targets. Several groups have begun to characterize the early versus late prodromal period.52,71 For example, a treatment trial underway in Germany has randomized early-phase prodromal participants to receive a program of CBT or clinical management and randomized late-stage prodromal participants to clinical management alone or in conjunction with AP medication.71 Results from such studies will contribute to our understanding of when treatment should be most profitably initiated, what type of treatment is most appropriate for each prodromal phase, and the criteria most helpful in evaluating short-term treatment effects. This shift in focus may bring about novel interventions such as the use of newly marketed SGAPs, ADs, cognitive enhancers, glycine, /-cycloserine, hormones, and psychosocial interventions that target specific skill deficits (eg, social skills group).
In addition, a collaborative effort under the leadership of Heinssen involving several prodromal research groups in the USA and Canada (Principal Investigators: Addington, Cadenhead, Cannon, Cornblatt, McGlashan, Perkins, Seidman, Tsuang, Walker, and Woods), referred to as the North American Prodromal Longitudinal Study (NAPLS), has been recently formed to provide a common database with a large prodromal sample. This collaboration is expected to increase consistency between studies by developing common methodologies, common measurement instruments, and correspondence between definitions of conversion. Several other networks have been initiated throughout Europe, including the European Prediction of Psychosis Study (EPOS) in Finland, led by Salokangas, and the Swiss Consortium currently headed by Simon. Such collaborations offer the hope that large databases will result, each with far more subjects and statistical power than possible for any study alone. Conclusions have thus far been elusive given the rarity of the prodromal state and the difficulty in ascertaining a substantial prodromal population. Large-scale collaborations offer the promise of generating a solid set of generalizable conclusions about the prodrome, which are reliable, valid, and representative of a broad preschizophrenia population.53
Selected abbreviations and acronyms
- AD
antidepressant
- AP
antipsychotic
- CBT
cognitive behavioral therapy
- CHR
clinical high risk
- NBI
needs-based intervention
- PACE
Personal Assessment and Crisis Evaluation (program)
- PRIME
Prevention through Risk Identification, Management, and Education (program)
- RAP
Recognition and Prevention (program)
- SGAP
second-generation antipsychotic
- SLP
schizophrenia-like psychosis
- SPI
specific preventive intervention
This research was supported in part by National Institute of Mental Health grant MH-61523 to Dr Cornblatt. We would like to thank Ruth Olsen for her help with many of the technical aspects of this manuscript.
Contributor Information
Barbara A. Cornblatt, The Zucker Hillside Hospital, North Shore-Long Island Jewish Health System, Lake Success, NY; Albert Einstein College of Medicine, New York, NY, USA.
Andrea M. Auther, Albert Einstein College of Medicine, New York, NY, USA.
REFERENCES
- 1.Morrison AP., Bentall RP., French P., et al. Randomised controlled trial of early detection and cognitive therapy for preventing transition to psychosis in high-risk individuals. Study design and interim analysis of transition rate and psychological risk factors. Br J Psychiatry. 2002;43(suppI):S78–S84. doi: 10.1192/bjp.181.43.s78. [DOI] [PubMed] [Google Scholar]
- 2.Bassett AS., Chow EW., O'Neill S., Brzustowicz LM. Genetic insights into the neurodevelopmental hypothesis of schizophrenia. Schizophr Bull. 2001;27:417–430. doi: 10.1093/oxfordjournals.schbul.a006884. [DOI] [PubMed] [Google Scholar]
- 3.Cannon TD., van Erp TG., Bearden CE., et al. Early and late neurodevelopmental influences in the prodrome to schizophrenia: contributions of genes, environment, and their interactions. Schizophr Bull. 2003;29:653–669. doi: 10.1093/oxfordjournals.schbul.a007037. [DOI] [PubMed] [Google Scholar]
- 4.Cornblatt BA. The schizophrenia prodrome: promise for prevention. Dialogues Clin Neurosci. 2001;3:93–98. doi: 10.31887/DCNS.2001.3.2/bcornblatt. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornblatt BA., Lencz T., Obuchowski M. The schizophrenia prodrome: treatment and high-risk perspectives. Schizophr Res. 2002;54:177–186. doi: 10.1016/s0920-9964(01)00365-6. [DOI] [PubMed] [Google Scholar]
- 6.Cornblatt BA., Lencz T., Smith CW., Auther A. Treatment of the schizophrenia prodrome. In: Stone WS, Faraone SV, Tsuang MT, eds. Early Clinical intervention and Prevention of Schizophrenia. Totowa, NJ: Humana Press; 2003 [Google Scholar]
- 7.Davidson M., Reichenberg A., Rabinowitz J., Weiser M., Kaplan Z., Mark M. Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. Am J Psychiatry. 1999;156:1328–1335. doi: 10.1176/ajp.156.9.1328. [DOI] [PubMed] [Google Scholar]
- 8.Tsuang MT. Genes, environment, and mental health wellness. Am J Psychiatry. 2000;157:489–491. doi: 10.1176/appi.ajp.157.4.489. [DOI] [PubMed] [Google Scholar]
- 9.Tsuang MT., Stone WS., Faraone SV. Toward reformulating the diagnosis of schizophrenia. Am J Psychiatry. 2000;157:1041–1050. doi: 10.1176/appi.ajp.157.7.1041. [DOI] [PubMed] [Google Scholar]
- 10.Tsuang MT., Stone WS., Faraone SV. Towards the prevention of schizophrenia. Biol Psychiatry. 2000;48:349–356. doi: 10.1016/s0006-3223(00)00934-3. [DOI] [PubMed] [Google Scholar]
- 11.Cornblatt BA. The New York high-risk project to the Hillside Recognition and Prevention (RAP) program. Am J Med Genet. 2002;114:956–966. doi: 10.1002/ajmg.b.10520. [DOI] [PubMed] [Google Scholar]
- 12.Cornblatt BA., Keilp JG. Impaired attention, genetics, and the pathophysiology of schizophrenia. Schizophr Bull. 1994;20:31–46. doi: 10.1093/schbul/20.1.31. [DOI] [PubMed] [Google Scholar]
- 13.Erlenmeyer-Kimling L., Cornblatt B. The New York High-Risk Project: a follow-up report. Schizophr Bull. 1987;13:451–461. doi: 10.1093/schbul/13.3.451. [DOI] [PubMed] [Google Scholar]
- 14.Tsuang MT., Stone WS., Faraone SV. Understanding predisposition to schizophrenia: toward intervention and prevention. Can J Psychiatry. 2002;47:518–526. doi: 10.1177/070674370204700603. [DOI] [PubMed] [Google Scholar]
- 15.Done DJ., Crow TJ., Johnstone EC., Sacker A. Childhood antecedents of schizophrenia and affective illness: social adjustment at ages 7 and 11. BMJ. 1994;309:699–703. doi: 10.1136/bmj.309.6956.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones PB., Done DJ. From birth to onset: a developmental perspective of schizophrenia in two national birth cohorts. In: Keshavan MS, Murray RM, eds. Neurodevelopment and Adult Psychopathology. Cambridge, UK: Cambridge University Press; 1997:119–136. [Google Scholar]
- 17.Cannon M., Jones P., Huttunen MO., Tanskanen A., et al. School performance in Finnish children and later development of schizophrenia: a population-based longitudinal study. Arch Gen Psychiatry. 1999;56:457–463. doi: 10.1001/archpsyc.56.5.457. [DOI] [PubMed] [Google Scholar]
- 18.David AS., Malmberg A., Brandt L., Allebeck P., Lewis G. IQ and risk for schizophrenia: a population-based cohort study. Psychol Med. 1997;27:1311–1323. doi: 10.1017/s0033291797005680. [DOI] [PubMed] [Google Scholar]
- 19.Malmberg A., Lewis G., David A., Allebeck P. Premorbid adjustment and personality in people with schizophrenia. Br J Psychiatry. 1998;172:308–313. doi: 10.1192/bjp.172.4.308. [DOI] [PubMed] [Google Scholar]
- 20.Cameron DE. Early schizophrenia. Am J Psychiatry. 1938;95:567–678. [Google Scholar]
- 21.Kraepelin E. Dementia Praecox and Paraphrenia. Edinburgh, UK: Livingstone; 1919 [Google Scholar]
- 22.Meares A. The diagnosis of prepsychotic schizophrenia. Lancet. 1959;1:55–58. doi: 10.1016/s0140-6736(59)91134-1. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan HS. The onset of schizophrenia. 1927. Am J Psychiatry. 1994;151(suppl):134–139. doi: 10.1176/ajp.151.6.134. [DOI] [PubMed] [Google Scholar]
- 24.Wyatt RJ. Neuroleptics and the natural course of schizophrenia. Schizophr Bull. 1991;17:325–351. doi: 10.1093/schbul/17.2.325. [DOI] [PubMed] [Google Scholar]
- 25.Wyatt RJ., Green MF., Tuma AH. Long-term morbidity associated with delayed treatment of first admission schizophrenic patients: a re-analysis of the Camarillo State Hospital data. Psychol Med. 1997;27:261–268. doi: 10.1017/s0033291796004345. [DOI] [PubMed] [Google Scholar]
- 26.Wyatt RJ., Henter ID. The effects of early and sustained intervention on the long-term morbidity of schizophrenia. J Psychiatr Res. 1998;32:169–177. doi: 10.1016/s0022-3956(97)00014-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haas GL., Garratt LS., Sweeney JA. Delay to first antipsychotic medication in schizophrenia: impact on symptomatology and clinical course of illness. J Psychiatr Res. 1998;32:151–159. doi: 10.1016/s0022-3956(98)00008-9. [DOI] [PubMed] [Google Scholar]
- 28.Loebel AD., Lieberman JA., Alvir JM., Mayerhoff Dl., Geisler SH., Szymanski SR. Duration of psychosis and outcome in first-episode schizophrenia. Am J Psychiatry. 1992;149:1183–1188. doi: 10.1176/ajp.149.9.1183. [DOI] [PubMed] [Google Scholar]
- 29.Craig TJ., Fennig S., Tanenberg-Karant M., Bromet EJ. Rapid versus delayed readmission in first-admission psychosis: quality indicators for managed care. Ann Clin Psychiatry. 2000;12:233–238. doi: 10.1023/a:1009038627449. [DOI] [PubMed] [Google Scholar]
- 30.Ho BC., Andreasen NC., Flaum M., Nopoulos P., Miller D. Untreated initial psychosis: its relation to quality of life and symptom remission in firstepisode schizophrenia. Am J Psychiatry. 2000;157:808–815. doi: 10.1176/appi.ajp.157.5.808. [DOI] [PubMed] [Google Scholar]
- 31.Robinson DG., Woerner MG., Alvir JM., et al. Predictors of treatment response from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 1999;156:544–549. doi: 10.1176/ajp.156.4.544. [DOI] [PubMed] [Google Scholar]
- 32.McGlashan TH. Duration of untreated psychosis in first-episode schizophrenia: marker or determinant of course? Biol Psychiatry. 1999;46:899–907. doi: 10.1016/s0006-3223(99)00084-0. [DOI] [PubMed] [Google Scholar]
- 33.McGorry PD. Evaluating the importance of reducing the duration of untreated psychosis. Aust N Z J Psychiatry. 2000;34(suppl):S145–S149. doi: 10.1080/000486700236. [DOI] [PubMed] [Google Scholar]
- 34.Edwards J., McGorry PD. Implementing Early Intervention in Psychosis: A Guide to Establishing Early Psychosis Services. London, UK: Martin Dunitz; 2002 [Google Scholar]
- 35.Auther AM., Lencz T., Smith CW., Bowie CR., Cornblatt BA. Overview of the first annual workshop on the schizophrenia prodrome. Schizophr Bull. 2003;29:625–631. doi: 10.1093/oxfordjournals.schbul.a007035. [DOI] [PubMed] [Google Scholar]
- 36.Woods SW., Breier A., Zipursky RB., et al. Randomized trial of olanzapine versus placebo in the symptomatic acute treatment of the schizophrenic prodrome. Biol Psychiatry. 2003;54:453–464. doi: 10.1016/s0006-3223(03)00321-4. [DOI] [PubMed] [Google Scholar]
- 37.Yung AR., McGorry PD., McFarlane CA., Jackson HJ., Patton GC., Rakkar A. Monitoring and care of young people at incipient risk of psychosis. Schizophr Bull. 1996;22:283–303. doi: 10.1093/schbul/22.2.283. [DOI] [PubMed] [Google Scholar]
- 38.Yung AR., Phillips LJ., Yuen HP., et al. Psychosis prediction: 12-month follow-up of a high-risk (“prodromal”) group. Schizophr Res. 2003;60:21–32. doi: 10.1016/s0920-9964(02)00167-6. [DOI] [PubMed] [Google Scholar]
- 39.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 40.Green MF., Kern RS., Braff DL., Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 41.Marshall M., Lockwood A. Early intervention for psychosis. Cochrane Database Syst Rev. 2004:CD004718. doi: 10.1002/14651858.CD004718. [DOI] [PubMed] [Google Scholar]
- 42.Falloon IR. Early intervention for first episodes of schizophrenia: a preliminary exploration. Psychiatry. 1992;55:4–15. doi: 10.1080/00332747.1992.11024572. [DOI] [PubMed] [Google Scholar]
- 43.McGorry PD., Edwards J., Mihalopoulos C., Harrigan SM., Jackson HJ. EPPIC: an evolving system of early detection and optimal management. Schizophr Bull. 1996;22:305–326. doi: 10.1093/schbul/22.2.305. [DOI] [PubMed] [Google Scholar]
- 44.McGlashan TH., Zipursky RB., Perkins D., et al. The PRIME North America randomized double-blind clinical trial of olanzapine versus placebo in patients at risk of being prodromally symptomatic for psychosis. I. Study rationale and design. Schizophr Res. 2003;61:7–18. doi: 10.1016/s0920-9964(02)00439-5. [DOI] [PubMed] [Google Scholar]
- 45.Yung AR., McGorry PD. The initial prodrome in psychosis: descriptive and qualitative aspects. Aust N Z J Psychiatry. 1996;30:587–599. doi: 10.3109/00048679609062654. [DOI] [PubMed] [Google Scholar]
- 46.Yung AR., Phillips LJ., McGorry PD., et al. Prediction of psychosis. A step towards indicated prevention of schizophrenia. Br J Psychiatry. 1998;172 (suppl):14–20. [PubMed] [Google Scholar]
- 47.McGorry PD., Yung AR., Phillips LJ., et al. Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Arch Gen Psychiatry. 2002;59:921–928. doi: 10.1001/archpsyc.59.10.921. [DOI] [PubMed] [Google Scholar]
- 48.Miller TJ., McGlashan TH., Woods SW., et al. Symptom assessment in schizophrenic prodromal states. Psychiatr Q. 1999;70:273–287. doi: 10.1023/a:1022034115078. [DOI] [PubMed] [Google Scholar]
- 49.McGlashan TH., Miller TJ., Woods SW., Hoffman RE., Davidson L. Instrument for the assessment of prodromal symptoms and states. In: Miller TJ, Mednick SA, McGlashan TH, eds. Early Intervention in Psychotic Disorders. Amsterdam, Netherlands: Kluwer Academic Publishers; 2001:135–149. [Google Scholar]
- 50.McGlashan, TH, Zipursky, RB, Perkins, DO, et al. Olanzapine versus placebo for the schizophrenic prodrome: 1-year results. Paper presented at: 1 56th Annual Meeting of the American Psychiatric Association; May 17-22, 2003; San Francisco, Calif. [Google Scholar]
- 51.Arnold SE., Rioux L. Challenges, status, and opportunities for studying developmental neuropathology in adult schizophrenia. Schizophr Bull. 2001;27:395–416. doi: 10.1093/oxfordjournals.schbul.a006883. [DOI] [PubMed] [Google Scholar]
- 52.Cornblatt BA., Lencz T., Smith CW., Correll CU., Auther AM., Nakayama E. The schizophrenia prodrome revisited: a neurodevelopmental perspective. Schizophr Bull. 2003;29:633–651. doi: 10.1093/oxfordjournals.schbul.a007036. [DOI] [PubMed] [Google Scholar]
- 53.Heinssen RK., Cuthbert BN., Breiling J., Colpe LJ., Dolan-Sewell R. Overcoming barriers to research in early serious mental illness: issues for future collaboration. Schizophr Bull. 2003;29:737–745. doi: 10.1093/oxfordjournals.schbul.a007043. [DOI] [PubMed] [Google Scholar]
- 54.Dworkin RH., Cornblatt B., Friedmann R., et al. Childhood precursors of affective vs social deficits in adolescents at risk for schizophrenia. Schizophr Bull. 1993;1993:563–577. doi: 10.1093/schbul/19.3.563. [DOI] [PubMed] [Google Scholar]
- 55.Dworkin RH., Lewis JA., Cornblatt BA., Erlenmeyer-Kïmling L. Social competence deficits in adolescents at risk for schizophrenia. J Nerv Ment Dis. 1994;182:103–108. doi: 10.1097/00005053-199402000-00007. [DOI] [PubMed] [Google Scholar]
- 56.Miller TJ., Woods SW., Rosen JL., McGlashan TH. Treatment of psychosis at onset. Am J Psychiatry. 2002;159:153. doi: 10.1176/appi.ajp.159.1.153. [DOI] [PubMed] [Google Scholar]
- 57.Yung AR., Phillips LJ., Yuen HP., McGorry PD. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res. 2004;67:131–142. doi: 10.1016/S0920-9964(03)00192-0. [DOI] [PubMed] [Google Scholar]
- 58.an der Heiden W., Hafner H. The epidemiology of onset and course of schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2000;250:292–303. doi: 10.1007/s004060070004. [DOI] [PubMed] [Google Scholar]
- 59.Harrow M., Sands JR., Silverstein ML. Course and outcome for schizophrenia census other psychotic patients: a longitudinal study. Schizophr Bull. 1997;23:287–303. doi: 10.1093/schbul/23.2.287. [DOI] [PubMed] [Google Scholar]
- 60.Robinson DG., Woerner MG., McMeniman M., Mendelowitz A., Bilder RM. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 2004;161:473–479. doi: 10.1176/appi.ajp.161.3.473. [DOI] [PubMed] [Google Scholar]
- 61.Strauss JS., Carpenter WT., Jr, Bartko JJ. The diagnosis and understanding of schizophrenia. Part III. Speculations on the processes that underlie schizophrenic symptoms and signs. Schizophr Bull. 1974:61–69. doi: 10.1093/schbul/1.11.61. [DOI] [PubMed] [Google Scholar]
- 62.Cornblatt BA., Lencz T., Kane JM. Treatment of the schizophrenia prodrome: is it presently ethical? Schizophr Res. 2001;51:31–38. doi: 10.1016/s0920-9964(01)00236-5. [DOI] [PubMed] [Google Scholar]
- 63.Hafner H., an der Heiden W. The course of schizophrenia in the light of modern follow-up studies: the ABC and WHO studies. Eur Arch Psychiatry Clin Neurosci. 1999;249(suppl)4:14–26. doi: 10.1007/pl00014180. [DOI] [PubMed] [Google Scholar]
- 64.Cannon M., Walsh E., Hollis C., et al. Predictors of later schizophrenia and affective psychosis among attendees at a child psychiatry department. Br J Psychiatry. 2001;178:420–426. doi: 10.1192/bjp.178.5.420. [DOI] [PubMed] [Google Scholar]
- 65.Weiser M., Reichenberg A., Rabinowitz J., et al. Association between nonpsychotic psychiatric diagnoses in adolescent males and subsequent onset of schizophrenia. Arch Gen Psychiatry. 2001;58:959–964. doi: 10.1001/archpsyc.58.10.959. [DOI] [PubMed] [Google Scholar]
- 66.Olin SC., Mednick SA., Cannon T., et al. School teacher ratings predictive of psychiatric outcome 25 years later. Br J Psychiatry. 1998;172(suppl):7–13. [PubMed] [Google Scholar]
- 67.Hafner H., Loffler W., Maurer K., Hambrecht M., an der Heiden W. Depression, negative symptoms, social stagnation and social decline in the early course of schizophrenia. Acta Psychiatr Scand. 1999;100:105–118. doi: 10.1111/j.1600-0447.1999.tb10831.x. [DOI] [PubMed] [Google Scholar]
- 68.Beiser M., Erickson D., Fleming JA., lacono WG. Establishing the onset of psychotic illness. Am J Psychiatry. 1993;150:1349–1354. doi: 10.1176/ajp.150.9.1349. [DOI] [PubMed] [Google Scholar]
- 69.Miller TJ., Zipursky RB., Perkins D., et al. The PRIME North America randomized double-blind clinical trial of olanzapine versus placebo in patients at risk of being prodromally symptomatic for psychosis. II. Baseline characteristics of the “prodromal” sample. Schizophr Res. 2003;61:19–30. doi: 10.1016/s0920-9964(02)00440-1. [DOI] [PubMed] [Google Scholar]
- 70.McGlashan TH., Zipursky RB., Perkins DO., et al. Olanzapine for treatment of the schizophrenia prodrome: 2-year results of a randomized placebocontrolled study. Biol Psychiatry. 2004;55(8S):226S. [Google Scholar]
- 71.Hafner H., Maurer K., Ruhrmann S., et al. Early detection and secondary prevention of psychosis: facts and visions. Eur Arch Psychiatry Clin Neurosci. 2004;254:117–128. doi: 10.1007/s00406-004-0508-z. [DOI] [PubMed] [Google Scholar]