Abstract
Background
Preserving the C7 spinous process during cervical laminoplasty has been reported to prevent axial symptom. Some patients underwent laminectomy and fixation developed the symptom. The objective of this article was to investigate whether axial symptom can be reduced by preserving the C7 spinous process during cervical laminectomy and fixation with lateral mass screw.
Methods
Between 2005 and 2008, data of 53 patients who underwent laminectomy and lateral mass-screw fixation for multilevel cervical myelopathy were reviewed. Analysis consisted of the incidence of axial symptom, Japan Orthopaedic Association (JOA) scores, recovery rate, cervical lordotic angle, and atrophy rate of cervical posterior muscle. Axial symptom severity was quantified by a visual analog scale (VAS). Twenty-five patients were decompressed from C3 to C7 (group A) and 28 from C3 to C6 with dome-shape removal of the C7 superior lamina (group B) .
Results
Analysis of final follow-up data showed improvement in clinical outcome for both groups. No difference in recovery rate, cervical lordotic angle and atrophy rate was observed between groups. Postoperative axial-neck pain was significantly rarer in group B than in group A. Axial symptom severity was correlated with cervical posterior muscle atrophy rate; correlation coefficient was 0.665.
Conclusion
The C7 spinous process might play an important role in preventing axial symptom, but there is a need for randomized, control studies with long-term follow-up to clarify the results.
Introduction
Multilevel cervical myelopathy is usually treated by posterior approaches. Laminectomy permits adequate decompression of the cervical spinal cord and is safely and easily performed but is associated with progressive spinal instability and kyphosis [1, 2]. In recent years, laminoplasty has been widely performed with favorable outcomes [3–6]. However, some disadvantages have also been observed, of which axial symptom is an intractable form of pain around the neck and shoulders and often remains a major concern for several years postoperatively, even in patients with excellent neurologic recovery [7, 8]. Laminectomy with fixation could eliminate the complication by laminectomy alone. Nevertheless, being a posterior procedure, the posterior structure of the cervical spine, which is reported to be the related factor of axial symptom [9, 10], may inevitably be damaged. The incidence of axial symptom after laminectomy with fixation has not yet been elucidated, and it is still unknown whether preserving C7 spinous process, as performed in laminoplasty, would prevent axial symptom [8, 11–13]. Accordingly, the purpose of this retrospective study was to evaluate the effect of preserving the C7 spinous process in relation to axial symptom incidence when laminectomy with instrumentation was performed for multilevel cervical myelopathy.
Materials and methods
Patient population
Between 2005 and 2008, data of 53 patients who underwent laminectomy and lateral mass-screw fixation were retrospectively reviewed. There were 34 men and 19 women (mean age 61.5, range 52–73 years). The average follow-up was 1.8 (range 1–4) years. Inclusion criteria were multilevel cervical myelopathy due to cervical spondylosis (74%) and ossification of the posterior longitudinal ligament (OPLL, 26%) of the cervical spine. Exclusion criteria were radiculopathy, trauma, tumor, and rheumatoid arthritis. Twenty-five patients were decompressed and fixed with lateral mass screws from C3 to C7 (group A) and 28 from C3 to C6 (group B). According to the clinic sequence, each patient was randomly assigned to one of the two groups, but the ultimate choice of procedure was decided upon by the patient before the operation agreement was signed. This study was approved by the Institutional Review Boards, and informed consent was obtained from each patient.
Surgery
After intubation, the patient was placed prone in the head holder. A posterior midline incision was made and the paravertebral muscles were retracted laterally. When the facet joints and lateral masses were identified, screws (Medtronic Sofamor Danek, Memphis, TN, USA) were placed bilaterally with the technique described by Magerl et al. [14]. Rods of appropriate size were selected and bent to match the contour of the lateral masses and secured to the lateral masses by screws. Laminectomy was performed from pedicle to pedicle (C3–C7 in group A; C3–C6 with dome-shape removal of superior lamina of C7 in group B) to ensure adequate spinal canal decompression. The autologous bone obtained from the laminectomy was used for posterolateral fusion (C3–C7 in group A; C3–C6 in group B). The patient used a cervical collar for 2 months after surgery.
Clinical evaluation
Neurological status was assessed according to the Japan Orthopaedic Association (JOA) score before and after surgery; recovery rate was calculated at final follow-up using the following method: (postoperative JOA score − preoperative JOA score)/(17 − preoperative JOA score) × 100%. The incidence of pre- and postoperative axial symptom was investigated in both groups: severity was quantified by a visual analog scale (VAS, 0 mm = no pain, 100 mm = worst pain) at the latest follow-up.
Radiological evaluation
The lordotic angle was measured at the C2 and C7 in neutral-position lateral radiographs using Cobb’s method. Magnetic resonance images (MRI) of the cervical spine were taken before surgery and at the final follow-up. Cross-sectional areas of the cervical posterior muscles, including the trapezius, splenius capitis, semispinalis capitis (SSC), and multifidus muscles, were measured on axial T1-weighted MRI at the levels of C4–C5 and C5–C6. The average of the two levels was used for analysis, and the rate of muscle atrophy was obtained as described by Takeuchi et al. [15]. Data measurements were performed three times by a single observer, and the mean value was used for analysis.
Statistical analysis
A paired t test was used to assess statistical significance of changes between postoperative and preoperative parameters in each group. Statistical comparisons between groups were performed using two-sample t test. Pearson’s correlation coefficient was used to check the correlation between axial pain and several other parameters. The χ 2 test was applied for qualitative data. All statistical analysis was performed using computer statistical software for Windows (version 12.0, SPSS Inc., Chicago, IL, USA). A P value <0.05 was considered to be statistically significant.
Results
JOA score and recovery rate
The JOA score improved from 9.2 ± 1.8 preoperatively to 13.2 ± 2.2 postoperatively (P < 0.001) in group A; it improved from 9.0 ± 2.0 preoperatively to 13.1 ± 1.6 postoperatively (P < 0.001) in group B. The recovery rate was 53.2 ± 22.0, 52.0 ± 17.1%, respectively, for group A and group B. Although the JOA score was significantly improved at final follow-up, there was no statistically significant difference regarding JOA score and recovery rate between groups.
Cervical lordotic angle
The cervical lordotic angle increased from 8.2° ± 3.0° preoperatively to 13.1° ± 2.9°postoperatively (P < 0.001) in group A and from 9.0° ± 5.2° preoperatively to 14.2° ± 3.6° postoperatively (P < 0.001) in group B. The difference between groups was not statistically significant before or after surgery.
Cross-sectional area of the cervical posterior muscles
The cross-sectional area of the cervical posterior muscles decreased from 31.1 ± 3.7 cm2 preoperatively to 30.6 ± 3.9 cm2 postoperatively (P < 0.001) in group A and from 32.5 ± 5.0 cm2 preoperatively to 30.7 ± 4.9 cm2 postoperatively (P < 0.001) in group B. Atrophy rate was 6.4 ± 5.6% and 5.6 ± 3.0%, respectively, for groups A and B. There was no statistically significant difference for either parameter between groups. Clinical and radiologic data of all patients are summarized in Table 1. Bony union was obtained in all patients, and no screw loosening occured at final follow-up.
Table 1.
Perioperative parameters for clinical and radiologic outcomes
| Parameter | Group A (n = 25) | Group B (n = 28) | P value |
|---|---|---|---|
| JOA score | |||
| Preoperative | 9.2 ± 1.8 | 9.0 ± 2.0 | 0.653 |
| Postoperative | 13.2 ± 2.2 | 13.1 ± 1.6 | 0.862 |
| Recovery rate (%) | 53.2 ± 22.0 | 53.2 ± 17.1 | 0.815 |
| Lordotic angle | |||
| Preoperative (°) | 8.2 ± 3.0 | 9.0 ± 5.2 | 0.523 |
| Postoperative (°) | 13.1 ± 2.9 | 14.2 ± 3.6 | 0.228 |
| Cross-sectional area | |||
| Preoperative (cm2) | 31.1 ± 3.7 | 32.5 ± 5.0 | 0.630 |
| Postoperative (cm2) | 30.6 ± 3.9 | 30.7 ± 4.9 | 0.926 |
| Atrophy rate (%) | 6.4 ± 5.6 | 5.6 ± 3.0 | 0.279 |
Both groups demonstrated statistically significant improvement compared with preoperative values
Axial symptom
Axial symptom incidence was 56% (14/25 patients) in group A and 25% (7/28 patients) in group B. The difference was statistically significant between groups (P = 0.021). Axial symptom severity was correlated with atrophy rate of the cervical posterior muscle (correlation coefficient 0.665; P = 0.001; Fig. 1), but not correlated with recovery rate (Fig. 2) or postoperative lordotic angle (Fig. 3).
Fig. 1.
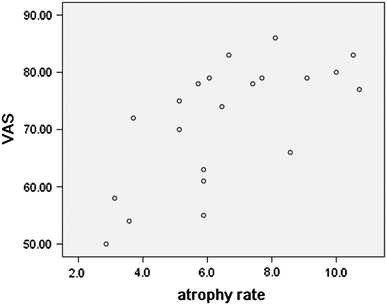
Correlation between severity of axial symptom (visual analog scale) and rate of muscle atrophy
Fig. 2.
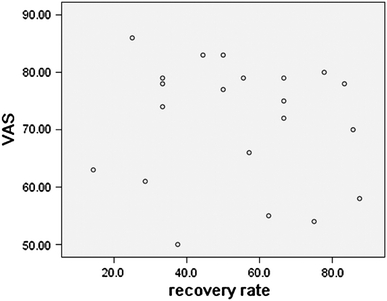
Correlation between severity of axial symptom (visual analog scale) and rate of neurologic functional recovery
Fig. 3.
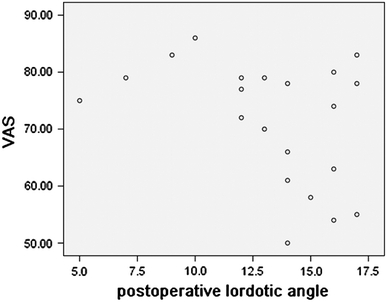
Correlation between severity of axial symptom (visual analog scale) and postoperative cervical lordotic angle
Discussion
Laminectomy is the earliest way to decompress the spinal cord in patients with multilevel cervical compressive myelopathy. However, poor results have been reported, with significant incidences of instability, progressive kyphosis, and neurological deterioration [1–5]. Lateral mass-screw fixation has now become the procedure of choice for stabilizing the cervical spine and preventing kyphosis that can cause progressive neurologic deficits when multilevel decompression is required [16–18]. In our institute, laminectomy combined with lateral mass screw-rod was performed as an alternative to laminectomy alone for multilevel cervical compressive myelopathy. During the follow-up period, we found some patients experienced the so-called axial symptom. To our knowledge, there was no conclusive study of this issue, particularly as to whether preserving C7 spinous process just as performed in laminoplasty would prevent the complication of axial symptom.
At the final follow-up, 40% (21/53) of the entire group showed axial symptom, an incidence similar to that previously reported in postlaminoplasty. The incidence was 56% (14/25) and 25% (7/28) for groups A and B, respectively; the difference was statistically significant. Therefore, much attention should be paid to the complication in laminectomy and fixation.
There is controversy on the source of axial symptom: is it the paravertebral muscle or the C7 spinous process? Kawaguchi et al. [19] pointed out that damage to paraspinal muscles may be a major cause of axial symptom. In the preliminary study of French-door laminoplasty, Yoshida et al. [20] found that reattachment of the spinous process and extensor musculature in patients with cervical myelopathy did not seem to have a significant influence on the development or resolution of axial symptom. However, in the latest prospective study of comparison between open-door and French-door laminoplasty, they reported that axial pain was improved in the latter procedure but became worse in the former [21].
Shiraishi et al. [22] reported a new treatment for cervical spondylotic myelopathy in which a standard laminectomy at appropriate levels is combined with a partial laminectomy of the cephalad half of the laminae at levels where the muscular attachments to the spinous processes are undisturbed. This minimizes damage to the deep extensor muscles. The authors found none of the patients complained of persistent axial symptom, and they believed that preserving the deep extensor muscles was effective in preventing axial symptom. During the following years, similar conclusions have been reached by other surgeons [23–25]. On the other hand, preserving the C7 spinous process was considered to play an important role in decreasing the incidence of postoperative axial symptom. Hosono et al. [8] reported that the incidence of early postoperative axial symptom was 50% in C3–C7 laminoplasty and 16% in C3–C6 laminoplasty; the incidence of late postoperative axial symptom was 29% in C3–C7 laminoplasty, 5.4% in C3–C6 laminoplasty. These differences were statistically significant, which emphasizes the effectiveness of the latter procedure in which the C7 spinous process was preserved [8, 26]. Higashino et al. [11] stated that although the significance of preserving the C7 spinous process in preventing axial symptom was not ascertained in their study, they considered it a means of overcoming this problem.
All the conclusions above were derived from reports on laminectomy or laminoplasty. However, on the basis of cervical anatomy and our results, we hypothesized that there would be a relatively lower incidence of postoperative axial symptom when laminectomy combined fixation was performed while preserving the C7 spinous process. Johnson et al. found that the splenius capitis, trapezius, rhomboideus minor, and serratus posterior superior are densely and closely bound to the C7 spinous process and that the maximum force generated by the trapezius was greater at C7 than at the upper or middle cervical spine [27, 28]. These findings suggest that preserving the C7 spinous process is extremely important. An anatomic study [29] reported that in the C3–C6 procedure, the rhomboideus minor in 35%, the serratus posterior superior in 100%, and the splenius capitis in 67% were partly preserved at the C7 spinous process; the rhomboideus major in 76% and splenius cervicis in 80% were completely preserved without partial dissection of their attachment. Otherwise, in the C3–C7 laminoplasty, the possibility of partial preservation of the rhomboideus minor, serratus posterior superior, and splenius capitis at the C7 spinous process was 0%, 66%, and 29%, respectively; the rhomboideus major in 16% and the splenius cervicis in 56% could be completely preserved. Some surgeons [8, 13] found that axial symptom severity increased in the sitting or upright position and decreased in the supine position because the trapezius and rhomboideus minor attached to the C7 spinous process and scapula are stretched by scapular adduction with downward displacement of the upper extremity. This observation confirmed the significance of preserving the C7 spinous process to prevent axial symptom.
The study reported showed that axial symptom severity was positively correlated with the rate of muscle atrophy, which means the symptom would get worse if the posterior neck muscle were more severely atrophied. Not all patients experienced axial symptom (group A 14/25; group B 7/28). No significant difference in atrophy rate was observed between groups, although the value of atrophy rate in group A was higher than that in group B. Therefore, short-term immobilization and early exercise of the posterior neck muscles are recommended to decrease the rate of muscle atrophy and to eliminate the effect of axial symptom.
Successful treatment of cervical myelopathy requires adequate decompression and prevention of neurological deterioration. However, doubt remains regarding the clinical outcome of C7 spinous process decompression. In laminectomy, the first step is to remove the lamina of the cranial vertebra in standard fashion. Then the ligamentum flavum and the cephalad part of the caudal vertebra lamina are removed. Several authors [22–25] reported that adequate decompression of the spinal cord and satisfactory clinical outcome could be obtained when the inferior lamina of the targeted level was partly preserved.
Spinal cord compression does not commonly occur at the C6–C7 level. Additionally, previous studies reported that the postoperative JOA scores of patients with C3–C6 procedure significantly improved, and there was no significant difference in neurological recovery compared with that in C3–C7 procedure [8, 11, 13, 26]. This might be explained by postoperative MRI in which the diameter of the dural sac at C6–C7 was significantly smaller in the C3–C6 group. There was no difference in the increase in spinal cord diameter between groups [8, 11]. In our study, we observed improved JOA score postoperatively in each group, with no statistically significant difference, although our follow-up was not long.
Conclusion
This study showed that axial symptom was significantly rarer after a C3–C6 procedure than after a C3–C7 procedure. Therefore, the C7 spinous process may play an important role in preventing axial symptom. Axial symptom severity might be affected by musculature atrophy. There are some limitations in our study, and thus randomized, controlled studies with long-term follow-up are needed to confirm the results.
Acknowledgments
No funds were received in support of this work.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg Spine. 2000;93:199–204. doi: 10.3171/spi.2000.93.2.0199. [DOI] [PubMed] [Google Scholar]
- 2.Hansen-Schwartz J, Kruse-Larsen C, Nielsen CJ. Follow-up after cervical laminectomy, with special reference to instability and deformity. Br J Neurosurg. 2003;17:301–305. doi: 10.1080/02688690310001601171. [DOI] [PubMed] [Google Scholar]
- 3.Lee TT, Green BA, Gromelski EB. Safety and stability of open-door cervical expansive laminoplasty. J Spinal Disord Tech. 1998;11:12–15. [PubMed] [Google Scholar]
- 4.Ogawa Y, Toyama Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, Hirabayashi H, Hirabayashi K. Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine. 2004;12:56–58. doi: 10.3171/spi.2004.1.2.0168. [DOI] [PubMed] [Google Scholar]
- 5.Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg Spine. 2002;96:180–189. doi: 10.3171/spi.2002.96.2.0180. [DOI] [PubMed] [Google Scholar]
- 6.Satomi K, Nishu Y, Kohno T, Hirabayashi K. Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine. 1994;19:507–510. doi: 10.1097/00007632-199403000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty: a noticeable complication. Spine. 1996;21:1969–1973. doi: 10.1097/00007632-199609010-00005. [DOI] [PubMed] [Google Scholar]
- 8.Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H. C3–6 laminoplasty takes over C3–7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J. 2006;15:1375–1379. doi: 10.1007/s00586-006-0089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hosono N, Sakaura H, Mukai Y, Ishii T, Yoshikawa H. En bloc laminoplasty without dissection of paraspinal muscles. J Neurosurg Spine. 2005;3:29–33. doi: 10.3171/spi.2005.3.1.0029. [DOI] [PubMed] [Google Scholar]
- 10.Nakama S, Nitanai K, Oohashi Y, Endo T, Hoshino Y. Cervical muscle strength after laminoplasty. J Orthop Sci. 2003;8:36–40. doi: 10.1007/s007760300006. [DOI] [PubMed] [Google Scholar]
- 11.Higashino K, Katoh S, Sairyo K, Sakai T, Kosaka H, Yasui N. Preservation of C7 spinous process does not influence the long-term outcome after laminoplasty for cervical spondylotic myelopathy. Int Orthop. 2006;30:362–365. doi: 10.1007/s00264-005-0062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosono N, Sakaura H, Mukai Y, Yoshikawa H. The source of axial pain after cervical laminoplasty-C7 is more crucial than deep extensor muscles. Spine. 2007;32:2985–2988. doi: 10.1097/BRS.0b013e31815cda83. [DOI] [PubMed] [Google Scholar]
- 13.Kowatari K, Ueyama K, Sannohe A, Yamasaki Y. Preserving the C7 spinous process with its muscles attached: effect on axial symptoms after cervical laminoplasty. J Orthop Sci. 2009;14:279–284. doi: 10.1007/s00776-009-1331-1. [DOI] [PubMed] [Google Scholar]
- 14.Jeanneret B, Magerl F, Ward E, Ward JC. Posterior stabilization of the cervical spine with hook plates. Spine. 1991;16:S56–S63. doi: 10.1097/00007632-199103001-00010. [DOI] [PubMed] [Google Scholar]
- 15.Takeuchi K, Yokoyama T, Aburakawa S, Saito A, Numasawa T, Iwasaki T, Itabashi T, Okada A, Ito J, Ueyama K. Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3–C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis. Spine. 2005;30:2544–2549. doi: 10.1097/01.brs.0000186332.66490.ba. [DOI] [PubMed] [Google Scholar]
- 16.Huang RC, Girardi FP, Poynton AR, Cammisa FP., Jr Treatment of multilevel cervical spondylotic myeloradiculopathy with posterior decompression and fusion with lateral mass plate fixation and local bone graft. J Spinal Disord Tech. 2003;16:123–129. doi: 10.1097/00024720-200304000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Kumar V, Rea G, Mervis L, McGregor J. Cervical spondylotic myelopathy: functional and radiographic long-term outcome after laminectomy and posterior fusion. Neurosurgery. 1999;44(4):771. doi: 10.1097/00006123-199904000-00046. [DOI] [PubMed] [Google Scholar]
- 18.Houten JK, Cooper PR. Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression, and neurological outcome. Neurosurgery. 2003;52:1081–1087. doi: 10.1227/01.NEU.0000057746.74779.55. [DOI] [PubMed] [Google Scholar]
- 19.Kawaguchi Y, Matsui H, Ishihara H, Gejo R, Yoshino O. Axial symptoms after en bloc cervical laminoplasty. J Spinal Disord Tech. 1999;12:392–395. [PubMed] [Google Scholar]
- 20.Yoshida M, Tamaki T, Kawakami M, Nakatani N, Ando M, Yamada H, Hayashi N. Does reconstruction of posterior ligamentous complex with extensor musculature decrease axial symptoms after cervical laminoplasty? Spine. 2002;27:1414–1418. doi: 10.1097/00007632-200207010-00008. [DOI] [PubMed] [Google Scholar]
- 21.Okada M, Minamide A, Endo T, Yoshida M, Kawakami M, Ando M, Hashizume H, Nakagawa Y, Maio K. A prospective randomized study of clinical outcomes in patients with cervical compressive myelopathy treated with open-door or French-door laminoplasty. Spine. 2009;34:1119–1126. doi: 10.1097/BRS.0b013e31819c3b61. [DOI] [PubMed] [Google Scholar]
- 22.Shiraishi T. Skip laminectomy—a new treatment for cervical spondylotic myelopathy, preserving bilateral muscular attachments to the spinous processes: a preliminary report. Spine J. 2002;2:108–115. doi: 10.1016/S1529-9430(01)00118-8. [DOI] [PubMed] [Google Scholar]
- 23.Otani K, Sato K, Yabuki S, Iwabuchi M, Kikuchi S. A segmental partial laminectomy for cervical spondylotic myelopathy: anatomical basis and clinical outcome in comparison with expansive open-door laminoplasty. Spine. 2009;34:268–273. doi: 10.1097/BRS.0b013e318195b27a. [DOI] [PubMed] [Google Scholar]
- 24.Shiraishi T, Fukuda K, Yato Y, Nakamura M, Ikegami T. Results of skip laminectomy-minimum 2-year follow-up study compared with open-door laminoplasty. Spine. 2003;28:2667–2672. doi: 10.1097/01.BRS.0000103340.78418.B2. [DOI] [PubMed] [Google Scholar]
- 25.Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Ito Z, Matsuyama Y. Laminoplasty and skip laminectomy for cervical compressive myelopathy: range of motion, postoperative neck pain, and surgical outcomes in a randomized prospective study. Spine. 2007;32:1980–1985. doi: 10.1097/BRS.0b013e318133fbce. [DOI] [PubMed] [Google Scholar]
- 26.Takeuchi T, Shono Y. Importance of preserving the C7 spinous process and attached nuchal ligament in French-door laminoplasty to reduce postoperative axial symptoms. Eur Spine J. 2007;16:1417–1422. doi: 10.1007/s00586-007-0352-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson GM, Zhang M, Jones DG. The fine connective tissue architecture of the human ligamentum nuchae. Spine. 2000;25:5–9. doi: 10.1097/00007632-200001010-00003. [DOI] [PubMed] [Google Scholar]
- 28.Johnson G, Bogduk N, Nowitzke A, House D. Anatomy and actions of the trapezius muscle. Clin Biomech. 1994;9:44–50. doi: 10.1016/0268-0033(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 29.Ono A, Tonosaki Y, Yokoyama T, Aburakawa S, Takeuchi K, Numasawa T, Wada K, Kachi T, Toh S. Surgical anatomy of the nuchal muscles in the posterior cervicothoracic junction: significance of the preservation of the C7 spinous process in cervical laminoplasty. Spine. 2008;33:E349–E354. doi: 10.1097/BRS.0b013e31817152cc. [DOI] [PubMed] [Google Scholar]


