Abstract
The diagnostic value of the head-up tilt test (HUTT) in discovering vasovagal syndrome depends on the pre-test probability. An accurate anamnesis and clinical examination screens the patients indicated for the HUTT. In patients with unexplained syncope, the R-test is an alternative procedure to discover its cause. In our study, we evaluated the diagnostic significance of the HUTT in a group of 211 patients and of the R-test in a subgroup of 45 patients with negative HUTT results and with negative traditional Holter ECG monitoring (24 hr).
KEY WORDS: R-test, Head-up tilt test, Syncope
INTRODUCTION
Syncope is a very common symptom and it represents an important public health problem because it leads to traumatic lesions, worsens quality of life; it is one of the most common causes of inability and it is associated with elevated health care costs (1, 17). Syncope is defined as a sudden and transitory loss of consciousness and orthostatic position associated with a fast, spontaneous and complete regain of consciousness. The loss of consciousness derives from the reduction in cerebral blood flow.
Lypotimia is defined as a sudden weakness, incapacity to maintain the orthostatic position, visus block out and near loss of consciousness. It can precede the syncopal episode or not (2).
Vasovagal syncope is the most common cause of syncope and it represents about 10–40% of all the causes (19). Vasovagal syncope physiopathology: when we step over from the clinostatic to orthostatic position about 800 ml of blood goes into the subdiaphragmatic part of the body with a reduction in preload into the right ventricle. In patients with vasovagal syncope the mechanoceptors located in the heart and in the carotid bulb send an exaggerated signal to the cerebral trunk with an alterated sympathovagal response and vasodepression (3).
The head-up tilt test (HUTT) is the most efficacious test in studying the vasovagal reaction. In addition, ECG monitoring is very important in discovering the cause of syncope both with traditional ECG 24-hr and the R-test, and with ECG monitoring over a period of 7 days.
The aim of our study was to verify the diagnostic value of the HUTT in patients suspected of vasovagal syndrome and of the R-test in patients with unexplained syncope.
Subjects and methods
In our syncope unit, from 2002–2005, there were 211 patients symptomatic for syncope and/or lypotimia suspicious for vasovagal syndrome. Mean age was 41.5 yrs (range 18–65 yrs); 88 patients were male and 123 were female. Fifty-eight patients had one or more lypotimic episodes in anamnesis and 153 patients had one or more syncopal episodes. Some patients had already undergone other diagnostic tests for syncope such as Holter ECG monitoring, echocardiogram, electrophysiological study, electroencephalogram, encephalic CT, and upper aortic trunk Doppler. All patients candidates for HUTT underwent carotid sinus massage with negative responses. After a detailed description of the test modality, the patients had to give their informed consent. Some general measures were respected when tilt testing was performed. The room where the test is performed should be quiet and with dim lighting. Patients should fast for at least 2 hr before the test.
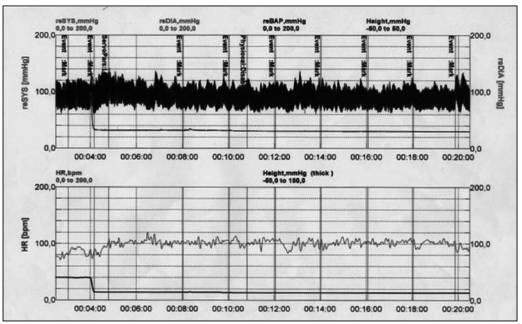
In order to monitor arterial blood pressure (BP), we adopted the F500 system, a versatile non-invasive beat-to-beat monitoring system. It captures the continuous BP waveform, and automatically computes up to 15 important beat-to-beat hemodynamic parameters including cardiac output (CO), stroke volume (SV), total peripheral resistance (TPR), pulse rate variability (PRV) and baroreflex sensitivity (BRS). ECG monitoring at 25 mm/sec in 12 derivations is obtained in the basal position after the supine position phase, every 3 min and every time it was necessary. We used a tilt table with a foot board support to achieve the upright position smoothly and rapidly, and to reset the supine position quickly (<10 sec) when the test is completed to avoid the consequences of a prolonged loss of consciousness. One physician was present throughout the tilt test procedure. We followed the “Italian Protocol”.
This protocol provides a supine pre-tilt phase of at least 5 min when no venous cannulation is performed and at least 20 min when cannulation is undertaken; tilt angle is 60–70°. Passive phase is a minimum of 20 min and a maximum of 45 min. If the passive phase has been negative 400 µg of nitroglicerin spray is used sublingually; the drug challenge phase is about 15–20 min. The end-point of the test is defined as the induction of syncope or a progressive and symptomatic fall in BP for at least 3 min or until a value of 60 mmHg in systolic BP is achieved or the completion of the planned duration of tilt including drug stimulation (15, 16, 18).
Hemodynamic results of HUTT
Type 1 mixed response: heart rate falls at the time of syncope but the ventricular rate does not fall to <40 beats/min or falls to <40 beats/min for <10 sec with or without asystole of <3 sec. BP falls before the heart rate falls.
Type 2A cardio inhibition without a systole: heart rate falls to a ventricular rate <40 beats/min for >10 sec, but asystole of >3 sec does not occur. BP falls before the heart rate falls.
Type 2B cardio inhibition with a systole: a systole occurs for >3 sec. BP fall coincides with or occurs before the fall in heart rate.
Type 3 vasodepressor: heart rate does not fall >10% from its peak at the time of syncope.
Forty-five patients with syncope and a negative response to HUTT, after a negative 24-hr Holter ECG, underwent an ECG ambulatory registration with the R-test that registers ECG over a period of 7 days, and to give an analysis with dedicated software for specific event monitoring.
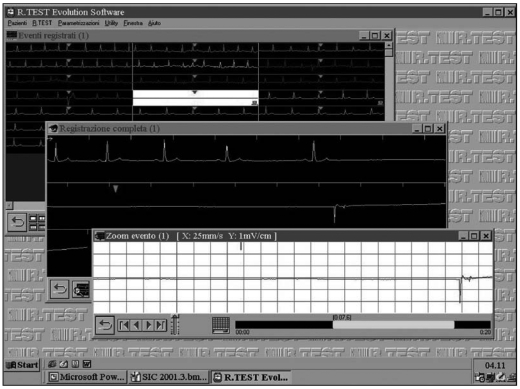
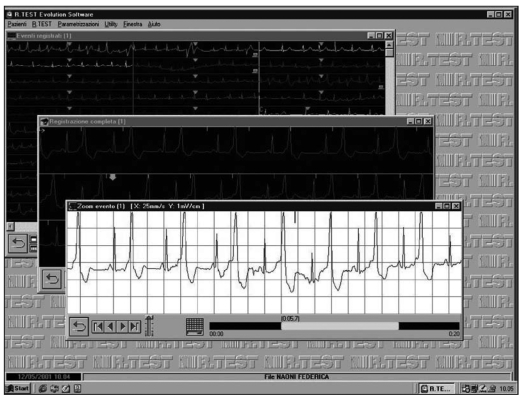
The R-test (Evolution Novacor-Cardioline) is a compact and lightweight ergonomic recorder (45 g batteries included, 60 × 48 × 28 mm) suspended around the neck like a medallion; it is maintained by an auto-adjustable cable, a particularly ergonomic configuration which drastically limits movement artefacts; its advanced miniaturized electronics are capable of real time QRS acquisition and processing.
It stores only significant events; therefore, avoiding the generation of huge data files usually associated with long-term ECG monitoring. The number and type of events recorded, as well as the pre- and post-event time are entirely programmable, allowing either specific screening for the confirmation of a suspected pathology or a wider search field in the absence of strong clinical evidence. Voluntary registration is possible during the specific symptom; in addition, this recorder includes a pre- and a post-registration of specific events.
The R-test evolution is equipped with a new acquisition system favoring the CM5 lead, for excellent results in arrhythmia detection and ST shift measurement in case… The user interface on PCs (RTSoft) is a model of user friendliness. Patient id is directly sent to and stored in the recorder before it starts, for enhanced data treatment safety. Transfer of the recorded data, display of all the events as well as the heart rate curve and event histograms are immediate, allowing a global overview. Each strip can also be zoomed in on separately for a detailed analysis.
RESULTS
Among the patients, 113 were positive to the HUTT and 98 were negative. In the positive group, 87 were females and 26 were males (median age 32 ± 10 yrs), while in the negative group 36 were female and 62 were male (median age 61 ± 10 yrs).
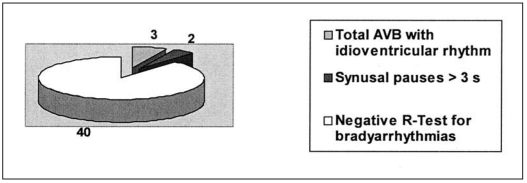
Of the 45 patients who underwent the R-test, five patients were symptomatic for syncope: in three cases there was a registration of complete atrial ventricular block with idio-ventricular rhythm and in two cases there was evidence of major pauses >3 sec (Fig. 1). All these patients needed pacemaker implantation.
Fig. 1.
R-test: results for hypokinetic arrhythmias.
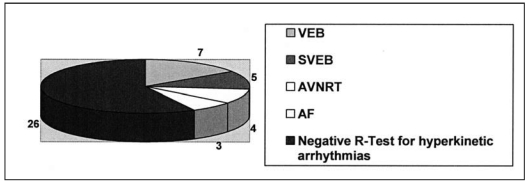
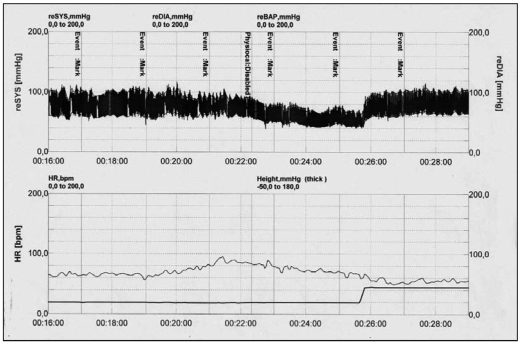
Among the patients submitted to the R-test, 19 patients presented with hyper kinetic arrhythmias (seven patients with ventricular ectopic beats (Fig. 2), five patients with supra-ventricular ectopic beats, four patients with short traits of parossistic supra-ventricular tachycardia and three patients with short traits of atrial fibrillation) (Figs. 3–7).
Fig. 2.
R-test: results for hyperkinetic arrhythmias.
Fig. 3.
Sinusal pauses (5.7 sec) with syncope.
Fig. 7.
Normal result.
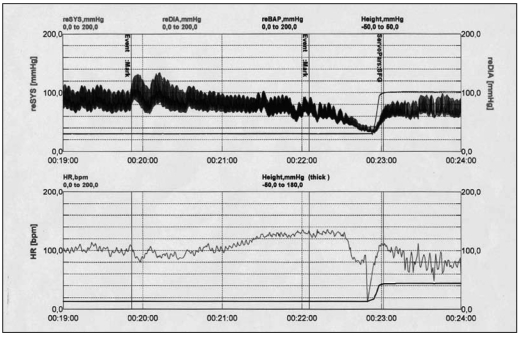
Fig. 4.
Ventricular ectopic beat (bygeminism).
Fig. 5.
A pure vasogenic result.
Fig. 6.
A cardioinhibitory result
DISCUSSION
Syncope is a syndrome consisting of a relatively short period of temporary and self-limited loss of consciousness caused by a transient reduction in blood flow to the brain (most often the result of systemic hypotension). Syncope comprises part of a subset of clinical conditions in which loss of consciousness is transient; other conditions in this group, which are not syncope and should be clearly distinguished from syncope, include, for example, seizure disorders, post-traumatic loss of consciousness and cataplexy (4).
Syncope accounts for up to 3% of emergency room visits and 6% of hospital admissions. The Framingham Study reported that approximately 3% of individuals have a syncopal episode during their lives, although lifetime incidence in the elderly can be as high as 23%. Mortality is generally low, but can be up to 33% at 1 yr in patients with a cardiac aetiology (5). The differential diagnosis is wide. Diagnosis can be made difficult by the intermittent nature of the symptoms, the large number of potential aetiologies, and the lack of a gold standard for clinical investigation. The cost of the investigation of recurrent unexplained syncope can be high, particularly if a relatively benign cause of syncope is overlooked in the process of excluding life-threatening disorders. Recurrences are common after the index event, occurring in up to one-third of patients. The search for an underlying cause in patients with syncope often poses a clinical dilemma and even after extensive evaluation, the specific cause can remain unknown in up to 50% of patients. In selected patients, the diagnostic yield can be improved with the use of specialized studies such as head-up tilt testing. Head-up tilt testing is a widely accepted tool in the investigation of syncope, particularly where there is no evidence of structural heart disease (6).
Initial evaluation with anamnesis, clinical examination, ECG and BP in clinostatic and orthostatic positions screens the patients suspected of vasovagal syncope and cardiogenic syncope. With an initial evaluation a neurogenic reflex can be suspected with indicative data and when other syncope causes have been excluded, independent from tilt-table test results. Patients with positive tilt-table test results and those with a negative response (indefinite syncope) have similar characteristics and prognosis, so it seems they belong in the same population. The key remains in selecting the appropriate patients for each investigation, such as by the presence of a prodrome of autonomic symptoms in those with suspected vasovagal syncope (7).
The absence of a gold standard diagnostic test for vasovagal syncope makes the calculation of the exact specificity and sensitivity of the tilt test difficult, particularly in view of the variable methodology used in the different groups reporting results. The ability of the test to differentiate patients from healthy controls is nonetheless established with specificity generally up to 90% and sensitivity ranging between 32% and 85% with the median closer to the upper number (8).
The diagnostic value of the HUTT in our group of patients is lower than that in the literature data, possibly due to the low pre-test probability. More rigorous application of the guidelines is necessary to optimize the usefulness of the HUTT. Recent studies have seen how a correct and specific anamnesis is able to discover with a high diagnostic value patients affected by vasovagal syndrome (11, 13). However, the tilt test has a higher sensibility in young female patients (10).
Sheldon et al (11) tested the sensitivity and specificity of a preliminary questionnaire about the characteristics of the syncopal episodes and every question was assigned a positive or negative score. The final score was indicative for vasovagal syncope or not. The point score correctly classified 90% of patients, diagnosing vasovagal syncope with 89% sensitivity and 91% specificity; so it is true that a targeted anamnesis could make a diagnosis without the tilt test (14).
The availability of implantable cardiac loop recorders is a significant advance in helping to clarify the situation in patients with unexplained syncope (9). Not unsurprisingly, many patients have been found to have a diagnosis different from that presumed from their history and other investigations as evidenced in the ISSUE-2 study. The ISSUE-2 study with the early application of a loop recorder in patients with unexplained syncope demonstrated that in a minority of patients during syncope recurrences there are tachy or bradyarrhythmias, supraventricular or ventricular that are responsible for syncopal episodes.
In our study, the R-test was able to detect an arrhythmic cause of syncope in some patients with negative HUTT and negative traditional Holter ECG monitoring. In our opinion, R-test ECG monitoring for a period of 7 days, with the possibility of repeating the test, could be a preliminary test to determine the use of the implantable loop recorder in patients with unexplained syncope. It is a very simple method that also reduces the management costs of the unexplained syncope population (12).
REFERENCES
- 1.Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med. 2002;347:878–85. doi: 10.1056/NEJMoa012407. [DOI] [PubMed] [Google Scholar]
- 2.Brignole M, Albon P, Benditt D, et al. Task force on syncope, European society of cardiology - guidelines on management (diagnosis and treatment) of syncope. Eur Heart J. 2001;22:1256–306. doi: 10.1053/euhj.2001.2739. [DOI] [PubMed] [Google Scholar]
- 3.Bartoletti A, Alboni P, Ammirati F, et al. The tilt test enhanced with oral nitroglycerin in patients with unexplained syncope: the Italian Protocol. The Working Group on Syncope of the Associazione Italiana di Aritmologia e Cardiostimolazione - the Arrhythmia Area of the Associazione Nazionale Medici Cardiologi Ospedalieri. Ital Heart J Suppl. 2000;1:226–31. [PubMed] [Google Scholar]
- 4.Benditt DG, Gert Van Dijk J, Sutton R, et al. Syncope. Curr Opin Cardiol. 2004;29:152–229. doi: 10.1016/j.cpcardiol.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Brignole M, Alboni P, Benditt D, et al. Guidelines on management (diagnosis and treatment) of sincope - update 2004 - executive summary and recommendation. Eur Heart J. 2004;25:2054–72. doi: 10.1016/j.ehj.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Sheldon R, Rose S, Koshman M. Comparison of patients with syncope of unknown cause having negative or positive tilt-table tests. Am J Cardiol. 1997;80:581–5. doi: 10.1016/s0002-9149(97)00425-6. [DOI] [PubMed] [Google Scholar]
- 7.Grimm W, Degenhardt M, Hoffman J, Menz V, Wirths A, Maisch B. Syncope recurrence can better be predicted by history than by head-up tilt testing in untreated patients with suspected neurally mediated syncope. Eur Heart J. 1997;18:1465–9. doi: 10.1093/oxfordjournals.eurheartj.a015473. [DOI] [PubMed] [Google Scholar]
- 8.Oribe E, Caro S, Perera R, et al. Syncope: the diagnostic value of head-up tilt testing. Pacing Clin Electrophysiol. 1997;20:874–9. doi: 10.1111/j.1540-8159.1997.tb05489.x. [DOI] [PubMed] [Google Scholar]
- 9.Farwell D, Freemantle N, Sulke N. Use of implantable loop recorders in the diagnosis and management of syncope. Eur Heart J. 2004;25:1257–63. doi: 10.1016/j.ehj.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 10.Del Rosso A, Alboni P, Brignole M, et al. Relation of clinical presentation of syncope to the age of patients. Am J Cardiol. 2005;96:1431–5. doi: 10.1016/j.amjcard.2005.07.047. [DOI] [PubMed] [Google Scholar]
- 11.Sheldon R, Rose S, Connoly S, Ritchie D, Koshman M, Frenneaux M. Diagnostic criteria for vasovagal syncope based on a quantitative history. Eur Heart J. 2006;27:344–50. doi: 10.1093/eurheartj/ehi584. [DOI] [PubMed] [Google Scholar]
- 12.Sutton R, Peterson M. The economics of treating vasovagal syncope. Pacing Clin Electrophysiol. 1997;20:849–50. doi: 10.1111/j.1540-8159.1997.tb03920.x. [DOI] [PubMed] [Google Scholar]
- 13.Alboni P, Brignole M, Menozzi C, et al. Diagnostic value of history in patients with syncope with or without heart disease. J Am Coll Cardiol. 2001;37:1921–8. doi: 10.1016/s0735-1097(01)01241-4. [DOI] [PubMed] [Google Scholar]
- 14.Grimm W, Degenhardt M, Hoffman J, Menz V, Wirths A, Maish B. Syncope recurrence can better be predicted by history than by head-up tilt testing in untreated patients with suspected neurally mediated syncope. Eur Heart J. 1997;9:1465–9. doi: 10.1093/oxfordjournals.eurheartj.a015473. [DOI] [PubMed] [Google Scholar]
- 15.Sutton R, Petersen M, Brignole M, Raviere A, Menozzi C, Giani P. Proposed classification for tilt induced vasovagal syncope. Eur J Cardiac Pacing Electrophysiol. 1992;3:180–8. [Google Scholar]
- 16.Brignole M, Menozzi C, Del Rosso A, et al. New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification. Analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. Europace. 2000;2:66–76. doi: 10.1053/eupc.1999.0064. [DOI] [PubMed] [Google Scholar]
- 17.Mascioli G, Anzola GP, Morandini A, Raddino R, Turelli A, Curnis A, Cicogna R. Diagnosis and follow-up of 330 patients admitted for syncope in the department of cardiology and neurology. How important is an interdisciplinary study? Cardiologia. 1996;41:455–63. [PubMed] [Google Scholar]
- 18.Cicogna R, Bonomi FG, Mascioli G, et al. Hemodynamic and neuroendocrine profile of 2 different cardiovascular responses in vasodepressor syncope induced by the head-up tilt test. G Ital Cardiol. 1992;22:1367–79. [PubMed] [Google Scholar]
- 19.Cicogna R, Bonomi FG, Curnis A, et al. Parapharyngeal space lesions syncope-syndrome A newly proposed reflexogenic cardiovascular syndrome. Eur Heart J. 1993;14:1476–83. doi: 10.1093/eurheartj/14.11.1476. [DOI] [PubMed] [Google Scholar]