Abstract
Background
Concerns over the rising costs of health care have increased interest in educating residents about the cost impact of medical decisions. While many programs educate residents about the effectiveness of care, little is known about how well residents and faculty know charges of diagnostic tests or both groups' interest in this topic.
Methods
We surveyed internal medicine residents and faculty at an academic tertiary care hospital. Both groups rated their agreement with a series of statements about health care charges on a Likert scale of 1 (strongly disagree) to 9 (strongly agree), and they estimated the charges for 15 commonly ordered diagnostic tests. Estimates within 25% of the true charge were considered correct. The Wilcoxon rank sum test was used to compare responses between residents and faculty.
Results
Seventy of 126 eligible participants (56%) returned surveys. Participants showed poor knowledge of health care charges but expressed a desire to learn more. Physicians also felt that cost-effectiveness should be considered when ordering diagnostic tests, although faculty members felt more strongly about this than did residents. In estimating the charges for diagnostic tests, less than a quarter of all responses were within 25% of the true charge.
Conclusions
Internal medicine physicians poorly estimate the charges for diagnostic tests but have a strong desire to improve their knowledge, suggesting a possible intervention to improve the cost-effectiveness of medical care.
Background
Health care expenditures in the United States exceeded $2.3 trillion in 2008, accounting for 16% of the gross domestic product.1 Per capita, the United States spends more than $7500 a year on health care, a figure 2 to 3 times that of other industrialized countries.2 Despite this monetary investment, the United States lags behind other countries in many key health measures.3 The Congressional Budget Office has estimated that $700 billion (roughly 5% of the nation's gross domestic product) is spent on medical tests and procedures that do not improve health outcomes.4 Concern over this gap between costs and outcomes has resulted in growing interest in improving the cost-effectiveness of care provided by practicing physicians and in teaching medical students and residents about cost-effectiveness and the financial impact of their clinical decisions.5,6 In the 2009 Accreditation Council for Graduate Medical Education (ACGME) Program Requirements for Residency Education in Internal Medicine, training of residents in cost-effective care is required as part of the patient care and systems-based practice competencies.6,7
While judging the effectiveness of medical interventions is a major part of training, doctors are often unaware of the charges for these interventions, which can vary considerably in different health systems.8,9 A number of states have passed legislation attempting to improve the transparency of health care pricing but compliance is often poor.10,11 A systematic review of physician knowledge of diagnostic and nondrug therapeutic costs done in 2008 included 14 studies and found that only one-third of physician estimates were within 20% to 25% of the true costs.12 It is unclear how well these results correlate to the US health care system, since most studies included in the review were done in countries with national health care systems and the only US study included from the last 2 decades looked at a specific diagnostic test.13 To address this gap in the literature, we designed a study to assess how well residents and faculty at an academic institution estimate the charges for a variety of diagnostic tests and to gauge their interest in knowing this information.
Methods
Setting
Oregon Health & Science University (OHSU) is a tertiary care university hospital in Portland, Oregon. An electronic medical records system (Epic Hyperspace, Epic Systems Corporation, Verona, WI) is used in both the inpatient and outpatient settings. All orders, including those for medications and diagnostic tests, are placed through a computerized order entry system. No charge information is provided to the physician at the time of order placement.
Study Subjects
Eligible subjects included all internal medicine faculty members and residents at OHSU. Faculty members (professor, assistant professor, associate professor, or instructor of medicine) work solely at OHSU Hospital and associated clinics. Residents work at both OHSU and the affiliated Portland Veterans Affairs Medical Center, splitting their time roughly equally between the 2 locations. Physicians working solely in subspecialties of internal medicine, subspecialty residents in a preliminary year of internal medicine, physicians with clinical responsibilities solely at other clinics or hospitals, physicians who were involved in pilot-testing the survey, and physicians not practicing clinical medicine at the time of survey distribution were excluded. A total of 126 physicians were eligible to receive the survey.
Survey Design and Distribution
The first section of the survey included 6 statements about health care charges. Respondents were asked to rate their agreement with each statement on a Likert scale ranging from 1 (strongly disagree) to 9 (strongly agree).
In the second section of the survey, subjects were asked to estimate the charges for 15 diagnostic tests. Notably, subjects were asked for the charge (the amount billed to the patient or insurance carrier, before any discounts), as opposed to the cost (the amount that the hospital paid for the test). Laboratory tests were chosen to include those ordered commonly (eg, basic metabolic panel and complete blood count) and more selectively (eg, D-dimer and anti-nuclear antibody) in both inpatient and outpatient practice. Imaging studies were selected to represent a range of modalities and anatomic areas. For imaging studies, participants were asked to estimate the charge for only the imaging test itself (not professional or reading fees).
The final section of the survey collected demographic information. This section also included an open-response area for respondents to note particular charge information they would find helpful. Besides the demographic information, surveys were otherwise anonymous.
The study was considered exempt from review by the university's Institutional Review Board. The survey was pilot-tested by 6 internal medicine physicians and modified to ensure clarity before its distribution at monthly staff meetings and weekly clinic conferences by the principal investigator over a 1-month period. Surveys were mailed to physicians not present at any of the scheduled meetings.
Statistical Analysis
Means and 95% confidence intervals were calculated for the 6 statements assessing physician attitudes, and the Wilcoxon rank sum test was used to compare responses between faculty and residents. The actual charges for laboratory tests were obtained from the Division of Laboratory Medicine Charge Description Master, and charges for imaging tests and electrocardiograms were obtained from the performing departments. Each estimated charge was compared to the actual charge and a percentage error was calculated with the following equation:
To aid the comparison between results from previous studies done in other settings, those estimates within 25% of the actual charge were labeled as “correct.”,12,14,15 Stata, version 10.1 (StataCorp, College Station, TX), was used to perform statistical analyses.
Results
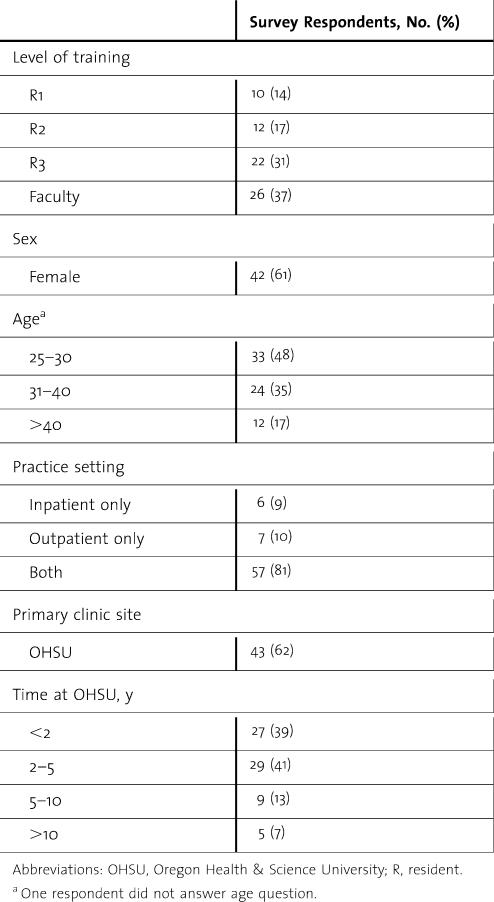
A total of 70 surveys were returned for a response rate of 56%. Of these, 4 had missing data, including 3 surveys missing charge estimations (n = 3 for D-dimer, n = 2 for anti-nuclear antibody, and n = 1 for troponin) and 1 missing demographic information (age and year of graduation from medical school). Respondent demographics are shown in table 1. Respondents were generally similar to nonrespondents with the exception that third-year residents and faculty were more likely than first- and second-year residents to return the survey.
TABLE 1.
Respondent Characteristics
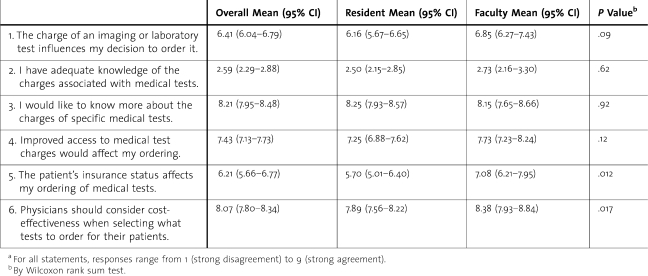
Responses to the attitudinal statements are displayed in table 2. While participants reported having inadequate knowledge of the charges for medical tests, most also reported that the charge of a test affects their decision to order it (statements 1 and 2). Respondents had a significant desire (agreeing more strongly than to any other statement) to know more about the charges of diagnostic tests and felt that improved access to charge information would affect their ordering behavior (statements 3 and 4). There were no statistically significant differences between resident and faculty respondents except for the statements regarding insurance coverage and cost-effectiveness. Faculty physicians were more likely to report that a patient's insurance status affects their ordering behavior (statement 5) and also were more likely to feel that physicians should consider cost-effectiveness when ordering tests (statement 6).
TABLE 2.
Physician Beliefsa
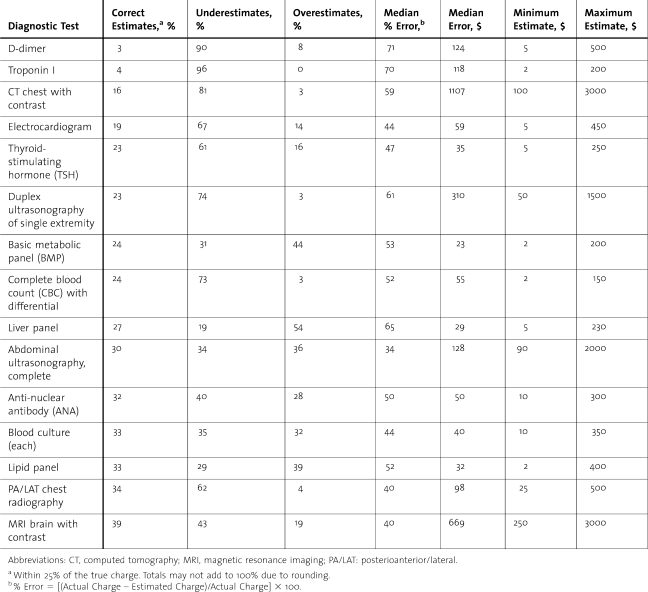
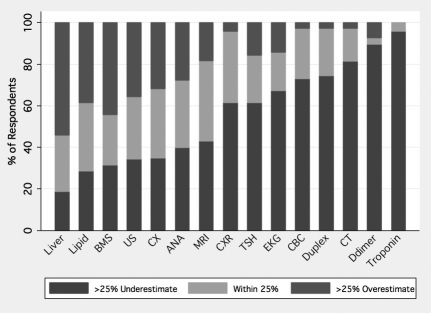
Results of participants' estimations of test charges are shown in table 3 (and supplemental figure). The percentage of correct estimates (defined as those within 25% of the actual charge) ranged from a high of 39% for brain magnetic resonance imaging to a low of 3% for D-dimer test. Overall, less than a quarter (24%) of all estimates were in the correct range. For most tests, the plurality of responses were underestimates; only the basic metabolic set, liver panel, lipid panel, and abdominal ultrasonography had a higher percentage of overestimates than underestimates (no test had a plurality of correct estimates). The tendency for respondents to underestimate test charges was particularly pronounced for higher-charge laboratory tests. The most expensive laboratory tests in our survey (troponin I and D-dimer) were by far the most commonly underestimated and the most commonly incorrect overall.
TABLE 3.
Charge Estimations by Test
FIGURE.
Physician Charge Estimates by Test
Percentage of respondents who underestimated, correctly estimated (within 25%), or overestimated the charge for each diagnostic test.
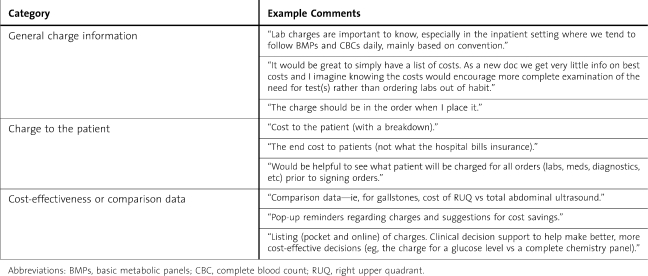
In the last part of the survey, faculty and residents were asked to note any charge information that they would find particularly useful. Responses generally fit in 1 of 3 categories, as shown in table 4.
TABLE 4.
Charge Information Requested by Respondents
Discussion
The results from our survey of internal medicine physicians at 1 academic institution in the United States suggest that physicians have very poor knowledge of the charges for diagnostic tests, as less than a quarter of total charge estimations were within 25% of the true charge. Of the 15 diagnostic tests included in our survey, only 4 (blood culture, lipid panel, chest radiography, and brain magnetic resonance imaging) had correct response rates of greater than 33%. Our results are similar to those from a prior systematic review, which included mostly studies done in countries with national health care systems, in which only a third of diagnostic cost estimates were between 20% and 25% of the true cost.12
These results highlight the need for better education of both resident and faculty physicians on the charges of diagnostic tests. It is notable that faculty felt as uncomfortable as residents at charge estimation, suggesting that little has been done to train physicians in this area to date. A recent study showed low levels of feedback to residents on their resource utilization,16 which may in part be due to the uncertainty faculty members feel regarding their knowledge on this topic. Therefore, it would seem that any intervention would need to target both trainees and their supervising physicians. Our results suggest that both groups are quite open to educational interventions that target this area of need.
Our respondents also felt that improving knowledge of charges would affect their ordering behavior. Given the societal interest in controlling health care costs, it would seem that a fairly straightforward intervention would be to simply improve the transparency of charges. Would such an intervention really change ordering behavior? Several studies, involving both written scenarios,17,18 and real-world settings,19–24 have shown a decrease in test ordering after physicians were provided charge information. In those studies done in real-world settings, providing physicians the charges for select diagnostic tests at the time of ordering (either on an order sheet or in a computer order entry system) produced a 10% to 30% decrease in test ordering and total charges without any significant increase in adverse events. Use of additional educational methods (such as didactic sessions on health care economics or computerized feedback on utilization of services) would most likely provide additional benefit. A recent review on cost-effectiveness and cost-containment curricula in graduate medical education found that interventions that used multiple simultaneous educational strategies were most successful in achieving positive outcomes.25
Our study does have several limitations. As it was performed at a single academic institution and included a specific group of physicians, generalizability is limited. Research in a variety of settings, ranging from community family medicine physicians and residents in British Columbia, Canada, to anesthesiologists at university-affiliated hospitals in Denmark, has found similar results.15,26–28 Performing a similar study in the United States involving multiple institutions would be useful but difficult owing to the significant variation in charges across health care systems. Another limitation of our study is that a relatively high percentage of physicians did not return their surveys, leading to possible response bias. While it seems unlikely that these physicians had significantly different knowledge of charges, it is possible that their beliefs regarding charges might have been different (eg, not completing the survey might be indicative of having less interest in knowing the charges for diagnostic tests). There is also the question of how best to determine the range for “correct” estimations. We chose to use a percentage range, rather than an absolute dollar figure or other measurement, which is in line with the methods used in prior studies.13 This means, of course, that the correct range of estimations for expensive tests is larger than that for inexpensive tests. This did not seem to have that significant of an impact, however, as the more expensive laboratory tests actually had more incorrect responses than the less expensive ones.
Conclusion
Our results are consistent with the need to better educate internal medicine physicians on the charges associated with diagnostic testing. Both faculty and resident physicians have a strong interest in improving their knowledge and it seems likely that better knowledge of charges will lead to more appropriate ordering of diagnostic tests. Further research should focus on identifying the optimal methods to disseminate charge information and improve knowledge of cost-effective care.
Footnotes
Raj T. Sehgal, MD, is a Clinical Assistant Professor of Medicine at the Division of Hospital Medicine, Department of Medicine, University of Texas Health Science Center at San Antonio and South Texas Veterans' Health Care System; and Paul Gorman, MD, is an Associate Professor of Medicine at the Department of Medical Informatics and Clinical Epidemiology, Oregon Health & Science University.
Prior presentations: An abstract of this study was presented at the Society of General Internal Medicine National Meeting on April 30, 2010, in Minneapolis, Minnesota.
Acknowledgements: The primary author received training from the Oregon Health & Science University Human Investigations Program, part of the Oregon Clinical and Translational Research Institute (OCTRI), grant number UL1 RR024140 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The primary author also received a Humanitarian Award from the Oregon Health & Science University Office of Graduate Medical Education that provided partial funding for the study. The funding bodies had no role in study design, data collection/analysis/interpretation, manuscript writing, or manuscript submission.
Funding: The authors report no external funding source.
References
- 1.Centers for Medicare & Medicaid Services. National health expenditure data. Available at: http://www.cms.hhs.gov/NationalHealthExpendData/downloads/highlights.pdf. Accessed March 23, 2010. [Google Scholar]
- 2.Davis K. Slowing the growth of health care costs—learning from international experience. N Engl J Med. 2008;359(17):1751–1755. doi: 10.1056/NEJMp0805261. [DOI] [PubMed] [Google Scholar]
- 3.Nolte E, McKee CM. Measuring the health of nations: updating an earlier analysis. Health Aff (Millwood) 2008;27(1):58–71. doi: 10.1377/hlthaff.27.1.58. [DOI] [PubMed] [Google Scholar]
- 4.Bentley TG, Effros RM, Palar K, Keeler EB. Waste in the U.S. health care system: a conceptual framework. Milbank Q. 2008;86(4):629–659. doi: 10.1111/j.1468-0009.2008.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American College of Physicians. Controlling Health Care Costs While Promoting the Best Possible Health Outcomes [policy monograph] Philadelphia, PA: American College of Physicians; 2009. [Google Scholar]
- 6.Cooke M. Cost consciousness in patient care—what is medical education's responsibility. N Engl J Med. 2010;362(14):1253–1255. doi: 10.1056/NEJMp0911502. [DOI] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in internal medicine. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/140_internal_medicine_07012009.pdf. Accessed April 8, 2010. [Google Scholar]
- 8.Reinhardt UE. The pricing of U.S. hospital services: chaos behind a veil of secrecy. Health Aff (Millwood) 2006;25(1):57–69. doi: 10.1377/hlthaff.25.1.57. [DOI] [PubMed] [Google Scholar]
- 9.Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4(9):e283. doi: 10.1371/journal.pmed.0040283. doi:10.1371/journal.pmed.0040283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farrell KS, Finocchio LJ, Trivedi AN, Mehrotra A. Does price transparency legislation allow the uninsured to shop for care. J Gen Intern Med. 2010;25(2):110–114. doi: 10.1007/s11606-009-1176-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Conference of State Legislatures. State legislation relating to disclosure of health and hospital charges. Available at: http://www.ncsl.org/programs/health/Transparency.htm. Accessed March 23, 2010. [Google Scholar]
- 12.Allan GM, Lexchin J. Physician awareness of diagnostic and nondrug therapeutic costs: a systematic review. Int J Technol Assess Health Care. 2008;24(2):158–165. doi: 10.1017/S0266462308080227. [DOI] [PubMed] [Google Scholar]
- 13.Saunders AF, Divine GW, Weinberger M. Physicians' awareness of mammography charges. Am J Prev Med. 1994;10(6):357–360. [PubMed] [Google Scholar]
- 14.Innes G, Grafstein E, McGrogan J. Do emergency physicians know the cost of medical care. CJEM. 2000 Apr;2(2):95–102. doi: 10.1017/s148180350000467x. [DOI] [PubMed] [Google Scholar]
- 15.Allan GM, Innes GD. Do family physicians know the costs of medical care. Can Fam Physician. 2004 Feb;50:263–270. [PMC free article] [PubMed] [Google Scholar]
- 16.Dine CJ, Miller J, Fuld A, Bellini LM, Iwashyna TJ. Educating physicians-in-training about resource utilization and their own outcomes of care in the inpatient setting. J Grad Med Educ. 2010;2(2):175–180. doi: 10.4300/JGME-D-10-00021.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cummings KM, Frisof KB, Long MJ, Hrynkiewich G. The effects of price information on physicians' test-ordering behavior: ordering of diagnostic tests. Med Care. 1982;20(3):293–301. doi: 10.1097/00005650-198203000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Long MJ, Cummings KM, Frisof KB. The role of perceived price in physicians' demand for diagnostic tests. Med Care. 1983;21(2):243–250. doi: 10.1097/00005650-198302000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Cohen DI, Jones P, Littenberg B, Neuhauser D. Does cost information availability reduce physician test usage. Med Care. 1982;20(3):286–292. doi: 10.1097/00005650-198203000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Seguin P, Bleichner JP, Grolier J, Guillou YM, Malledant Y. Effects of price information on test ordering in an intensive care unit. Intensive Care Med. 2002;28(3):332–335. doi: 10.1007/s00134-002-1213-x. [DOI] [PubMed] [Google Scholar]
- 21.Hampers LC, Cha S, Gutglass DJ, Krug SE, Binns HJ. The effect of price information on test-ordering behavior and patient outcomes in a pediatric emergency department. Pediatrics. 1999;103(4, pt 2):877–882. [PubMed] [Google Scholar]
- 22.Bates DW, Kuperman GJ, Jha A, Rittenberg E, Ma′Luf N, Tanasijevic M, et al. Does the computerized display of charges affect inpatient ancillary test utilization. Arch Intern Med. 1997;157(21):2501–2508. [PubMed] [Google Scholar]
- 23.Pugh JA, Frazier LM, DeLong E, Wallace AG, Ellenbogen P, Linfors E. Effect of daily charge feedback on inpatient charges and physician knowledge and behavior. Arch Intern Med. 1989;149(2):426–429. [PubMed] [Google Scholar]
- 24.Sachdeva RC, Jefferson LS, Coss-Bu J, Done G, Campbell D, Nelson SI, et al. Effects of availability of patient-related charges on practice patterns and cost containment in the pediatric intensive care unit. Ped Crit Care. 1996;24(3):501–506. doi: 10.1097/00003246-199603000-00022. [DOI] [PubMed] [Google Scholar]
- 25.Varkey P, Murad MH, Braun C, Grall KJ. H, Saoji V. A review of cost-effectiveness, cost-containment and economics curricula in graduate medical education. J Eval Clin Pract. 2010;16(6):1055–1062. doi: 10.1111/j.1365-2753.2009.01249.x. [DOI] [PubMed] [Google Scholar]
- 26.Schlunzen L, Simonsen MS, Spangsberg NL, Carlsson P. Cost consciousness among anaesthetic staff. Acta Anaesthesiol Scan. 1999;43(2):202–205. doi: 10.1034/j.1399-6576.1999.430214.x. [DOI] [PubMed] [Google Scholar]
- 27.Allan GM, Innes G. Family practice residents' awareness of medical care costs in British Columbia. Fam Med. 2002;34(2):104–109. [PubMed] [Google Scholar]
- 28.Graham JD, Potyk D, Raimi E. Hospitalists' awareness of patient charges associated with inpatient care. J Hosp Med. 2010;5(5):295–297. doi: 10.1002/jhm.655. [DOI] [PubMed] [Google Scholar]