Abstract
Background
To date, multiple myeloma remains an incurable malignancy due to the persistence of minimal residual disease in the bone marrow. In this setting, monoclonal antibodies against myeloma-specific cell surface antigens represent a promising therapeutic approach, which is however hampered by a lack of appropriate target structures expressed across all pathogenic myeloma cell populations. We, therefore, investigated functionally relevant immunoreceptors specifically associated with myeloma cells as well as their clonogenic precursors.
Design and Methods
Potential target proteins were identified using antibody arrays against phosphorylated immunoreceptors with lysates from myeloma cell lines. CD229 expression was confirmed in primary myeloma cells by reverse transcriptase polymerase chain reaction, western blot, fluorescence-activated cell sorting, and immunohistochemistry. Apoptosis, clonogenic growth, and sensitivity to chemotherapy were determined following short-interfering RNA-mediated downregulation of CD229. Antibody-dependent cellular and complement-dependent cytotoxicity were analyzed using a monoclonal antibody against CD229 to demonstrate the antigen’s immunotherapeutic potential.
Results
Our screening assay identified CD229 as the most strongly over-expressed/phosphorylated immunoreceptor in myeloma cell lines. Over-expression was further demonstrated in the CD138-negative population, which has been suggested to represent myeloma precursors, as well as on primary tumor cells from myeloma patients. Accordingly, CD229 staining of patients’ bone marrow samples enabled the identification of myeloma cells by flow cytometry and immunohistochemistry. Down-regulation of CD229 led to a decreased number of viable myeloma cells and clonal myeloma colonies, and enhanced the anti-tumor activity of conventional chemotherapeutics. Targeting CD229 with a monoclonal antibody resulted in complement- and cell-mediated lysis of myeloma cells.
Conclusions
Our results demonstrate that the immunoreceptor CD229 is specifically over-expressed on myeloma cells including their clonogenic precursors and contributes to their malignant phenotype. Monoclonal antibodies against this protein may represent a promising diagnostic and immunotherapeutic instrument in this disease.
Keywords: CD229, SLAM, surface molecules, tumor immunology, multiple myeloma
Introduction
Multiple myeloma (MM) is a clonal plasma cell malignancy with an incidence of approximately 15,000 new cases per year in the USA alone. MM is characterized by an accumulation of mature plasma cells in the bone marrow leading to destruction of bone, symptoms of bone marrow failure, and organ dysfunction. Within the last decade, treatment strategies targeting specific biological mechanisms such as angiogenesis have been developed and seem to improve the outcome of MM patients significantly.1 However, even after application of strategies incorporating new drugs such as bortezomib, thalidomide, and lenalidomide most patients will eventually relapse and succumb to the disease.2,3 One reason for this high rate of relapse even after multimodal and/or high dose chemotherapy plus autologous stem cell transplantation might be the persistence of myeloma stem cells in the bone marrow, since these cells seem to escape standard chemotherapeutic agents.4–6 As a consequence, MM remains essentially incurable by conventional anti-tumor therapy and patients continue to have a median survival of only 5 years.7 New therapeutic targets, expressed by the bulk of end-stage myeloma cells as well as their dormant progenitors, are needed for the development of treatments capable of eradicating minimal residual disease and allowing for increased rate of cures or at least prolonged remissions.
Targeting MM surface molecules by antibodies or immunoconjugates in order to engage the patients’ immune defense mechanisms represents an attractive therapeutic modality for the eradication of MM. Accordingly, therapeutic antibodies against a variety of myeloma antigens, such as CD40,8 CD56,9 CD138,10 and CD20,11 have been developed; however, none of these therapeutics has, so far, proven to be clinically effective and alternative myeloma surface molecules are urgently needed as potential targets.
The family of signaling lymphocytic activation molecules (SLAM) consists of nine leukocyte cell surface molecules [CD229, CD48, CD48-H1, CD84, CD150 (SLAM), CD244, BLAME, CS1, and NTB-A],12 which are members of the immunoglobulin superfamily and are involved in lymphocyte activation.13 In order to identify functionally active surface molecules as potential target antigens we performed an assay screening myeloma cell lines for the presence of phosphorylated immunoreceptors. The SLAM family member CD229, which has been shown to interact with its intracellular adapter protein Grb2 in a phosphorylation-dependent manner,14 showed the strongest over-expression/phosphorylation in all myeloma cell lines. Subsequent analyses confirmed the expression of this surface molecule on primary myeloma cells within patients’ bone marrow while the expression on other human tissues was restricted to certain leukocyte subtypes. CD229, which is identical to molecule Ly-9, was originally defined as a mouse cell surface molecule expressed on thymocytes, and mature B and T lymphocytes. We show here that silencing of CD229 expression contributes to spontaneous as well as chemotherapy-induced apoptosis of myeloma cells and inhibits the growth of clonogenic myeloma precursors. Importantly, targeting CD229 with a monoclonal antibody resulted in specific lysis of myeloma cell lines through antibody-dependent cellular cytotoxicity as well as complement-dependent cytotoxicity. These combined results suggest that CD229 might represent an attractive diagnostic and therapeutic target for MM.
Design and Methods
Cell lines, patients and healthy donors
Myeloma cell lines MOLP-8, RPMI-8226, KMS-12-BM, EJM, IM-9, NCI-H929, OPM-2, and LP-1 were authenticated by and obtained from the German Collection of Microorganisms and Cell Cultures (DSMZ) in 2005 and maintained according to DSMZ protocols. Bone marrow cells and peripheral blood mononuclear cells (PBMC) were obtained from a total of 36 consenting myeloma patients, 7 patients with monoclonal gammopathy of uncertain significance (MGUS), 8 healthy blood donors, and 14 stem cell donors. In addition, routine bone marrow biopsies were obtained from two of the patients and one healthy donor for analysis by immunohistochemistry. All patients were admitted for treatment or diagnostic purposes to the University Medical Center Hamburg-Eppendorf. Myeloma patients and MGUS patients had a median proportion of 33% and 8.9% of bone marrow-infiltrating myeloma cells, respectively, as defined by CD138/CD38 co-expression in flow cytometry. Patients were in disease stages I to III and differed somewhat with regards to treatment status: newly diagnosed (n=27), in untreated relapse after autologous stem cell transplantation (n=2) or allogeneic stem cell transplantation (n=1), treated with thalidomide (n=1), lenalidomide (n=1), bortezomib (n=1), or aurora kinase inhibitor (n=1), and in relapse after allogeneic stem cell transplantation treated with donor lymphocyte infusion (n=1) or bendamustine (n=1). Tonsils were obtained from adult patients undergoing tonsillectomy for chronic tonsillitis. The study protocol had received approval from the local ethics committee (decision number OB-038/06).
Proteome profiler™ assay
The human phospho-immunoreceptor array (R&D Systems, Minneapolis, MN, USA) allows for the simultaneous detection of 59 different phosphorylated immunoreceptors. Briefly, cell lysates from the cell line MOLP-8 were diluted with array buffer, added to a four-well multi-dish and incubated overnight at 2–8°C. After washing, anti-phosphotyrosine antibody conjugated to horse-radish peroxidase was added and chemiluminiscence was quantified after 2 h by scanning the developed X-ray film on a transmission-mode scanner according to the manufacturer’s recommendations.
Qualitative and real-time polymerase chain reaction
Total RNA was extracted using the RNeasy Mini Kit (Qiagen, Hilden, Germany). RNA samples from 20 different non-malignant solid tissues were obtained commercially (Applied Biosystems, Austin, TX, USA). Reverse transcription and conventional and quantitative polymerase chain reaction (PCR) were performed as previously described.14 Primers for the detection of CD229 (NM_001033667; product size 79 bp) were obtained from Qiagen while GAPDH primers were obtained from MWG Biotech, (Ebersberg, Germany).15
Western blot
Whole cell protein extracts were prepared from cell lines and western blotting was performed as previously described.15 We used primary antibodies against CD229 (Clone 249936; R&D Systems), β-actin (ACTB; clone 1; Santa Cruz Biotechnology, Delaware, CA, USA) and a secondary horse-radish peroxidase-labeled anti-mouse monoclonal antibody (R&D Systems). Specific binding was visualized by chemiluminescence (ECL Western Blotting Analysis System, Amersham Biosciences). Appropriate blocking studies were undertaken for all target proteins analyzed, using recombinant proteins in order to confirm the specificity of the staining.
Immunophenotyping
Tonsils, bone marrow and PBMC were stained after density gradient separation with the indicated antibodies and appropriate isotype controls (Online Supplementary Table S1). For routine analysis of primary myeloma samples, fresh bone marrow samples were stained according to the consensus report of the European myeloma network.16 Samples were analyzed using a FC500 cytometer and CXP software (Beckman Coulter) or a FACSCalibur with BD Cell QuestTM Pro (Version 5.2.1) software (Becton Dickinson) or FlowJo Version 7.2.5 (Tree Star Inc., OR, USA).
Immunohistochemistry
Prior to staining with primary murine anti-human CD229 (clone 249936; R&D Systems) and the plasma cell-specific anti-p63 monoclonal antibodies (clone: VS38c, Dako, Denmark), slides were deparaffinized, pretreated in citrate buffer (Zymed, San Francisco, CA, USA) and autoclaved at 121°C for 5 min, or pretreated in Bond epitope retrieval solution (Leica, Germany) for 30 min using a Bond-maX processing module (Menarini, Florence, Italy), respectively. Slides were pretreated with peroxidase block (Dako) followed by blocking with goat serum diluted 1:5 in 50 mmol/L Tris-HCl. Anti-CD229 and anti-p63 antibodies were applied at 1:100 and 1:25 dilutions, respectively. Slides were washed and goat anti-mouse horse-radish peroxidase-conjugated antibody (Dako) was applied for 30 min. After washing, a diaminobenzidine chromogen kit (Dako) was applied according to the manufacturer’s instructions.
Gene silencing by transfection with stealth short-interfering RNA
BLOCK-iT fluorescein-labeled dsDNA, scrambled control short-interfering (si) RNA, and stealth siRNA targeting CD229 were purchased from Invitrogen (Karlsruhe, Germany). The sequences of the gene-specific siRNA were sense GGACCUGA-GAGAAACACAAAGCUUU, antisense AAAGCUUUGUGUU-UCUCUCAGGUCC for siRNA-1: as well as sense CCCAAGU-CACCAUGAAGUCUGUGAA and antisense UUCACAGACU-UCAUGGUGACUUGGG for siRNA-2. Myeloma cell lines were transfected using Lipofectamine 2000 (Invitrogen) according to the manufacturer’s recommendations and transfection efficiency was determined by fluorescence microscopy using fluorescein-labeled double-stranded DNA. Transfection efficiency was 70–80% and cell death was less than 5% at 24 h after transfection.
MTT viability assay
Relative numbers of viable cells were assessed by a 3-(4,5-dimethylthiaxol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay17 72 h after transfection with CD229-specific siRNA or with scrambled control siRNA. Myeloma cells were cultured overnight and subsequently treated with bortezomib or melphalan 12 h before analyses. MTT (ATCC Bioproducts, Wesel, Germany) was added to each well and cells were incubated for 4 h. Absorbance was read at 570 nm using a spectrophotometer (Tecan, Mannedorf, Switzerland).
Measurement of apoptosis
The terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay was performed according to the manufacturer’s recommendations (Millipore, Billerica, MA, USA). Briefly, cells were fixed in 1% paraformaldehyde, and frozen until staining at −20°C using 70% ethanol. Afterwards, cells were incubated sequentially in staining solution for 1 h, and propidium iodide/RNAse A solution for 30 min. For annexin V staining, cells were incubated with annexin V-fluorescein isothiocyanate in Annexin binding buffer (BD Biosciences, San Jose, CA, USA). Analysis by flow cytometry was performed within the subsequent 3 h.
Colony formation assay
MOLP-8 myeloma cells were plated at 1000 cells/mL of methyl-cellulose medium (StemCell Technologies, Cologne, Germany) and 1 mL/well in a six-well culture dish (Nunc, Langensebold, Germany). Plates were incubated at 37°C and colonies consisting of more than 40 cells were counted 10 days after culture initiation.
Antibody-dependent cellular cytotoxicity and complement-dependent cytotoxicity
Cytotoxicity was determined using a lactate dehydrogenase release assay (Promega, Madison, WI, USA). For the analysis of antibody-dependent cellular cytotoxicity, MOLP-8 myeloma cells were transferred to a 96-well, round-bottomed plate at a concentration of 10,000 cells/well. Natural killer cells from healthy donors were separated by negative selection using magnetic beads (Miltenyi Biotech, Bergisch-Gladbach, Germany) and were added to the culture at a concentration of 200,000 cells/well. For the determination of complement-dependent cytotoxicity, 100,000 U-266 myeloma cells were plated into a 96-well, round-bottomed plate and human serum was added at a final concentration of 20%. A monoclonal mouse anti-human IgG1 antibody directed against CD229 (clone HLy 9.1.25, Santa Cruz Biotechnology, Santa Cruz, CA, USA) or an isotype control was added to the wells at different concentrations. Cells were incubated for 4 h and the resulting absorption was analyzed at 490 nm using a spectrophotometer (Tecan). Cytotoxicity was calculated using the following formula:
Statistical analysis
Statistical analyses were performed using SPSS software. The Mann-Whitney U test was used to calculate differences between different experimental conditions. Differences were considered to be statistically significant when the P value was less than 0.05.
Results
Surface molecule CD229 is constitutively expressed on myeloma cell lines including clonogenic myeloma precursors
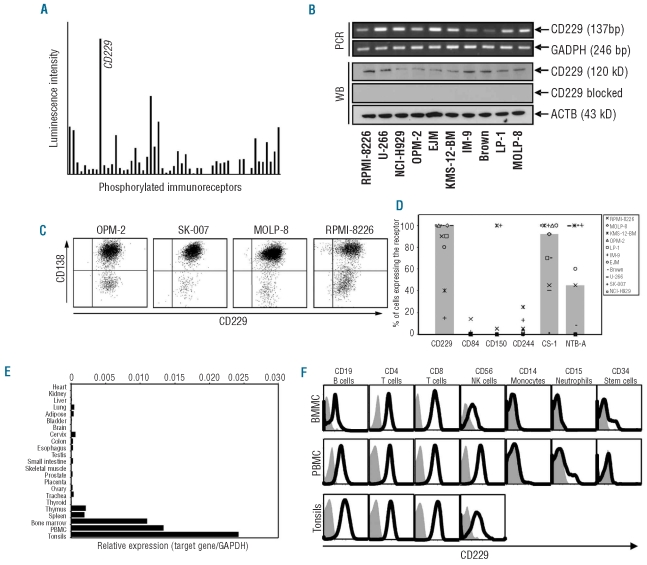
In the search for new diagnostic and therapeutic targets for myeloma we applied an antibody array to lysates of the myeloma cell line MOLP-8. This array enabled us to screen simultaneously for the expression of 59 different phosphorylated immunoreceptors at the protein level. We observed expression of a number of immunoreceptors such as CD28 and CD85 which are commonly known to be expressed on myeloma cells18,19 (Online Supplementary Table S2). However, the SLAM family member CD229 showed by far the strongest level of expression of all the proteins analyzed (Figure 1A).
Figure 1.
CD229 is expressed on myeloma cell lines and primary tumor cells from MM patients. Expression of 59 immune-related surface molecules in lysates of the MM cell line MOLP-8 was analyzed using the human phospho-immunoreceptor array. Bars indicate the mean luminescence intensity of spots representing individual phosphorylated immunoreceptors after subtraction of background levels measured for the internal negative control (A). RNA expression of CD229 was demonstrated by reverse transcriptase-PCR in ten different myeloma cell lines and constant expression of CD229 at the protein level was confirmed using western blot. Housekeeping genes GAPDH and β actin (ACTB) were used as internal controls for PCR and western blot (B). Strong surface expression of CD229 was detected on CD138-positive conventional myeloma cell lines and the CD138-negative subpopulation using flow cytometry (C). Compared to other members of the SLAM family, CD229 showed the strongest and most consistent surface expression on 11 myeloma cell lines as determined by flow cytometry. The percentages of positive cells among a given cell line (symbols) and median expression (gray bars) are shown (D). RNA expression of CD229 was measured in various human tissues using real-time PCR. Highest copy numbers were found in tonsillar tissues (mean expression of 6 patients), PBMC (mean expression of 4 donors) and bone marrow mononuclear cells (mean expression of 10 donors), while thymus and spleen were only marginally positive and no expression was found in any other tissue. Bars indicate expression of CD229 as normalized for copy numbers of the housekeeping gene GAPDH (E). Leukocyte subsets among PBMC, bone marrow mononuclear cells and tonsillar cells were analyzed for CD229 expression by flow cytometry. Results are representative of analyses of four separate donors (F).
As the expression of CD229 on myeloma cells is a hitherto practically unrecognized phenomenon, we next tested ten different myeloma cell lines for its presence. Using conventional reverse transcriptase PCR to differentiate positive from negative cell lines, we found that CD229 RNA was expressed in all ten myeloma cell lines. Additionally, western blot analyses confirmed CD229 protein expression, independently of the phosphorylation status of the receptor, in all myeloma lines (Figure 1B).
Clonogenic precursors are present in the bone marrow of myeloma patients and also among myeloma cell lines. In contrast to the bulk of MM cells these cells have previously been suggested to lack expression of CD138.20 Analyzing four myeloma cell lines by flow cytometry we confirmed surface expression of the CD229 molecule on the bulk of conventional myeloma cells and also on CD138-negative cells from the same cell cultures (Figure 1C).
Finally, as the SLAM family of surface molecules has nine members,12 we performed a comparative analysis of the expression of CD229 and five additional SLAM surface molecules on myeloma cell lines using flow cytometry. We observed that only a minority of cell lines tested expressed CD84, CD150, and CD244. In contrast, SLAM members CS-1 and NTB-A were expressed at significant levels on the majority of myeloma lines. However, the only SLAM molecule that was expressed on all but two myeloma cell lines at high levels was CD229 (Figure 1D).
Among healthy tissues, CD229 expression is restricted to certain lymphocyte subsets within lymphatic organs
Having identified a hitherto unrecognized antigen on myeloma cells which could possibly be used for diagnostic or therapeutic purposes, we next studied CD229 mRNA expression within a wide variety of healthy human tissues (Figure 1E). Using real-time PCR, relatively high levels of CD229 mRNA were found solely in lymphatic tissues such as the thymus, spleen and tonsillar tissue as well as in the bone marrow and within PBMC. No expression or only trace levels of CD229 mRNA were found in any other human tissue tested, which is in agreement with the results of a previous study.21
Further dissecting CD229 expression within human lymphatic organs, flow cytometry was applied to leukocytes derived from human bone marrow, tonsils, and peripheral blood. CD229 surface expression was found on T helper cells (CD3+/CD4+), cytotoxic T cells (CD3+/CD8+), natural killer cells (CD3−/CD56+), and B cells (CD3−/CD19+). In contrast, CD229 was not expressed on monocytes (CD14+) or neutrophils (CD15+). Importantly, CD229 was also absent from CD34+ hematopoietic progenitor cells, which were isolated from donor-derived bone marrow and from the peripheral blood of a stem cell donor after priming with granulocyte colony-stimulating factor (Figure 1F).
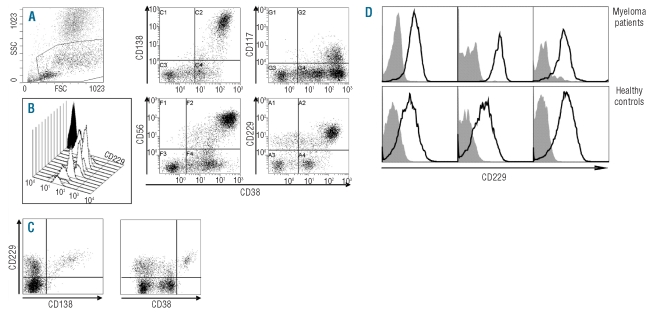
Surface antigen CD229 is expressed on malignant plasma cells from patients with multiple myeloma
Next, we explored CD229 expression on malignant plasma cells within fresh bone marrow samples of myeloma patients at various disease stages. Thirty-six patients with MM who had at least 10% bone marrow infiltration by myeloma cells, as defined by CD138/CD38 co-expression and as confirmed by conventional cytological examination, were included in the analysis. Remarkably, myeloma cells of all 36 patients showed strong expression of CD229 independently of their disease stage or current treatment. Overall, the intensity of CD229 staining was always higher in myeloma cells than in other lymphocyte cell types, such as normal T cells and B cells, found within the bone marrow of the myeloma patients (Figures 2A–B). In five patients, we determined CD229 expression twice during the course of their disease. One had received therapy with bortezomib, one had had a relapse after allogenic stem cell transplantation and the remaining three had untreated stage I or II disease. In addition, we screened seven patients with newly diagnosed MGUS for CD229 expression and could reliably identify bone marrow plasma cells by co-expression of CD138/CD38 and CD229 (Figure 2C).
Figure 2.
CD229 expression on bone marrow-residing primary myeloma cell Bone marrow from patients with MM (N=36) was first screened for CD229 expression by flow cytometry. Viable non-granulocytic cells were gated (A) and myeloma cells were identified by co-expression of CD138+/CD38+, CD117+/CD38+, and CD56+/CD38+. Representative results for CD229 surface expression (open histograms) versus isotype control (black histograms) are shown for nine MM cases (B) and one out of seven MGUS patients included (C). Surface expression of CD229 on bone marrow-residing plasma cells from representative myeloma patients (N=3) and healthy donors (N=3) was analyzed using flow cytometry. Histograms indicate fluorescence of CD138+ plasma cells after staining with anti-CD229 antibody (open histograms) or isotype control (gray area) (D).
Applying immunohistochemistry to bone marrow biopsies from selected patients with MM or MGUS as well as healthy subjects, we confirmed over-expression of CD229 protein on myeloma cells compared to on other bone marrow cells. Expression of CD229 correlated with the presence of plasma cells as indicated by staining with the plasma cell-specific anti-p63 antibody and, accordingly, numbers of bone marrow-residing CD229+ cells increased in the following order: least in healthy subjects, more in MGUS patients, highest values in MM patients (Online Supplementary Figure S1).
Comparing myeloma patients and healthy donors, we found that both groups had significant surface expression of CD229 on CD138+ plasma cells derived from the bone marrow. However, myeloma patients often showed a somewhat higher CD229 expression than the healthy controls (Figure 2D).
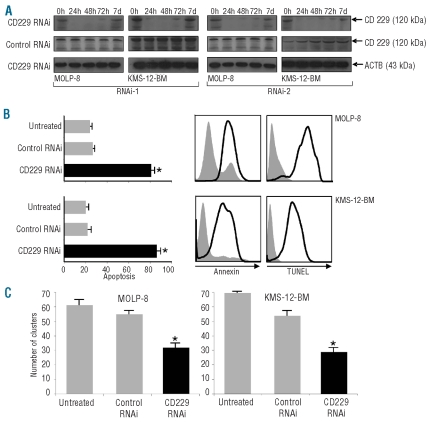
CD229 promotes the survival of myeloma cells in vitro
While CD229 is involved in adhesion between T cells and antigen-presenting cells including B cells,22 nothing is known about its function in myeloma. We, therefore, used RNA interference technology to define the role of this surface molecule in the biology of the malignant plasma cells. We observed a significant down-regulation of CD229 expression starting 24 h after transfection of the myeloma lines MOLP-8 and KMS-12-BM with CD229-specific siRNA (Figure 3A). We usually also detected a second, weaker band below the 120 kDA that is typically assigned to CD229 protein (Figure 3A). This second band most likely represents a 100 kDa splicing variant of CD229 which has previously been described21 and which also disappeared after siRNA transfection. Loss of CD229 protein expression lasted approximately until day 3 after transfection with either one of two different CD229-specific siRNA and was not observed following application of two scrambled control siRNA (Figure 3A). Furthermore, transfection with CD229-specific siRNA did not have an effect on the expression of the housekeeping protein β-actin, further excluding an unspecific off-target effect of transfection with CD229-specific siRNA.
Figure 3.
Silencing of CD229 exerts a pro-apoptotic effect on myeloma cells and decreases the number of clonogenic cells. Myeloma cell lines MOLP-8 and KMS-12-BM were transfected with two different siRNA specific for CD229 or with scrambled control siRNA. Treatment resulted in knockdown of CD229 protein expression in both cell lines starting 24 h after transfection as indicated by immunoblotting. Gene-silencing lasted at least until day 3 after transfection. Housekeeping protein beta actin (ACTB) was used as an internal control (A). Percentages of apoptotic myeloma cells were determined 72 h after transfection with CD229-specific siRNA or with control siRNA and results were compared to those of untreated cells. Bars show mean (+SEM) numbers of apoptotic cells as determined by annexin staining and flow cytometry of three separate experiments and asterisks indicate statistically significant (*P<0.05) differences when compared to untreated cells. Histograms indicate representative results of two different experiments performing transfection with CD229-specific siRNA (open histogram) or control siRNA (gray histogram) followed by flow cytometric analysis of annexin or TUNEL staining (B). In a clonogenic growth assay, clonal MM clusters were counted 7–10 days after culture initiation using the myeloma cell line MOLP-8 (left) or KMS-12-BM (right). Bars indicate mean (+SEM) values derived from three separate experiments. Numbers of colonies produced by myeloma cells transfected with CD229 siRNA or scrambled control siRNA were compared to those of cultures with untreated cells. Asterisks indicate statistically significant differences (*P<0.05) (C).
Based on the observation that, 48h after transfection, cell cultures contained approximately 30% fewer cells following transfection with CD229-specific siRNA than with control constructs, we next determined the number of apoptotic myeloma cells using annexin-staining and a flow-cytometric TUNEL assay (Figure 3B). Flow cytometry revealed increased percentages of apoptotic cells among MOLP-8 and KMS-12-BM myeloma cells after transfection with CD229-specific siRNA but not after transfection with scrambled control siRNA (Figure 3B). This finding strongly suggested an anti-apoptotic effect of CD229 on myeloma cells.
We further tested whether CD229 gene silencing would decrease the number of colonies initiated by myeloma cells. Using a standard colony-forming assay, we detected a significantly reduced number of cell colonies after transfection with CD229-specific siRNA in MOLP-8 and KMS-12-BM cell lines. Again, no significant effect on the formation of colonies was observed after treatment with scrambled control siRNA in the case of either MOLP-8 or KMS-12-BM (Figure 3C).
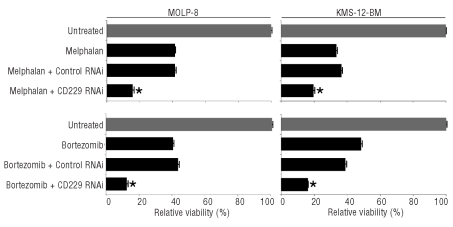
Combination of CD229 short-interfering RNA with chemotherapeutic agents leads to increased myeloma-specific cytotoxicity
As resistance of myeloma cells against traditional and novel therapeutics remains a constant obstacle to effective treatments, we next explored whether CD229 down-regulation would result in an additional cytotoxic effect when combined with chemotherapeutic agents with an established role in myeloma therapy. We, therefore, tested treatment with CD229 siRNA in combination with the traditional anti-myeloma drug melphalan and novel drug bortezomib in an MTT assay with the myeloma lines MOLP-8 and KMS-12-BM. For both cell lines, down-regulation of CD229 increased myeloma-specific cytotoxicity of both chemotherapeutic agents (Figure 4) indicating a potential use for CD229 as an adjunct to conventional therapeutic approaches in MM.
Figure 4.
CD229 silencing potentiates cytotoxic effects of melphalan and bortezomib on myeloma cell lines. Myeloma cell lines MOLP-8 and KMS-12-BM were transfected with CD229 siRNA or with scrambled control siRNA and 72 h after transfection, cells were treated with melphalan (20 μM) or bortezomib (10 nM) for 12 h and then cell viability was assessed via an MTT assay. Results show mean values of three separate experiments and asterisks indicate statistically significant differences (*P<0.05).
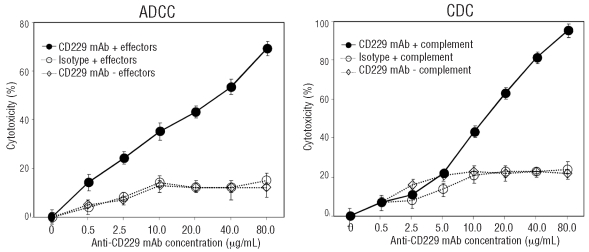
Treatment of myeloma cells with antibodies against CD229 results in specific immune-mediated lysis of tumor cells
A promising strategy for targeting CD229 on myeloma cells would be antibody-based treatment against this surface antigen. We, therefore, explored the ability of a monoclonal anti-CD229 antibody to engage the immune system in a cell- or complement-dependent manner against the myeloma cell lines MOLP-8 and U-266. Application of the CD229-specific antibody led to the induction of strong antibody-dependent cellular cytotoxicity using natural killer cells from healthy donors as effector cells. Importantly, CD229 antibody alone or an isotype control mAb in combination with natural killer cells had no such an effect (Figure 5).
Figure 5.
A monoclonal antibody (mAb) directed against CD229 exerts strong complement-(CDC) and antibody-dependent cytotoxic (ADCC) effects on myeloma cells. When added at different concentrations to cultures of myeloma cell lines MOLP-8 (CDC) or U-266 (ADCC), a monoclonal antibody directed against CD229 exerted significant cell- (left) and complement-dependent (right) cytotoxicity, respectively. Dots indicate mean percentage (±SEM) of maximal cytotoxicity in an lactate dehydrogenase release assay 4 h after addition of CD229 mAb.
Analyzing complement-dependent cytotoxicity exerted by the CD229-specific monoclonal antibody, we found that increasing amounts of antibody in the presence of human serum resulted in dose-dependent lysis of U-266 myeloma cells. CD229 antibody alone or an isotype control monoclonal antibody in combination with complement had no such effect (Figure 5). In summary, these findings suggest that a monoclonal antibody directed against surface molecule CD229 might be developed into a promising instrument for the therapy of MM.
Discussion
CD229 is a receptor belonging to the CD150 family of type I transmembrane glycoproteins. Its has previously been found on naïve and memory B cells and, to a lesser extent, on benign splenic plasma cells.24 Furthermore, CD229 was found to be expressed on cell lines derived from human B-cell malignancies.21 In accordance with these results, we observed expression of CD229 on a variety of myeloma cell lines. Members of the SLAM family of molecules other than CD229 have previously been suggested to be expressed on normal B cells25–31 and SLAM family member CS-1 has also been detected on malignant plasma cells.32 However, our findings indicate that CD229 is the SLAM family member with the highest potential for the development of myeloma-targeting therapies because: (i) CD229 showed the broadest expression of all SLAM members on myeloma cell lines and (ii) CD229 seems to have the most tumor-restricted expression of all SLAM members.21,33 Accordingly, we have shown that CD229 is absent from monocytes and neutrophils. Most importantly CD34-positive cells, which represent the hematopoietic progenitor fraction, were also negative for CD229. This is in agreement with a previous study demonstrating hematopoetic stem cell expression of CD244, CD48 and CD84 while CD229 was the only SLAM member absent from virtually all human stem cell subsets.34
Remarkably, in our study all samples from MGUS or MM patients showed strong expression of CD229 by bone marrow-infiltrating myeloma cells independently of the stage of the disease or treatment. In concert with CD38 and CD138 expression, positivity for CD229 allowed reliable identification of myeloma cells within human bone marrow as the expression of CD229 on myeloma cells was higher than that on any other leukocyte subset. This finding suggests that CD229 might not only represent an attractive therapeutic target but might also be used for diagnostic purposes in MGUS and MM.
Importantly, we show here that CD229 is found on mature CD138-positive myeloma cells as well as on CD138-negative myeloma cells, which have previously been suggested to represent the MM stem cell compartment.4 In our current study, we did not confirm that the CD138-negative fraction of myeloma cells possesses any stem cell characteristics or that the expression of CD229 on CD138-negative myeloma cells is biologically more relevant than its expression on CD138-positive cells. However, an indirect sign of a central functional role of CD229 in myeloma precursors may be the reduced number of colony-initiating cells following specific down-regulation either by increasing apoptosis in this subset or by reducing their colony-forming capacity. While our data do not differentiate between the two possibilities, they do demonstrate a biological imperative for the malignant cells to maintain expression of CD229 consolidating its potential as a reliable clinical parameter. Taken together with data providing indirect evidence for the role of SLAM receptors in the development of memory B cells and plasma cells23 our study points towards a role of CD229 beyond that of an immunomodulatory protein.14,22 We believe that myeloma-related proteins are particularly attractive for targeted (immuno-)therapies if they play central roles in the malignancy’s pathophysiology. Choosing such targets may prevent down-regulation or loss of expression of the respective protein under the therapy-induced selective pressure.
We show here for the first time that the application of a monoclonal CD229-specific antibody results in strong complement-dependent cytotoxicity and antibody-dependent cellular cytotoxicity against myeloma cells. These findings suggest that CD229 might indeed be a myeloma-related protein suitable for the development of a specific and effective antibody-based immunotherapy for MM. It is true that comparably high concentrations of antibody were required in order to achieve substantial complement-dependent cytotoxicity or antibody-dependent cellular cytotoxicity. However, it needs to be stressed that this particular antibody was originally generated in the mouse for purely diagnostic purposes. Humanized antibodies are superior to their mouse counterparts if used in the human system.36 Accordingly, the application of a humanized antibody developed for the clinical setting, preferably of the IgG1 subtype,37 is very likely to result in even stronger myeloma-specific cytotoxicity than the approach presented here.
Taken together, we describe here the expression of CD229 on distinct populations of myeloma cell lines and primary myeloma cells. In healthy individuals CD229 is found on some normal lymphocyte subsets but is absent from myeloid cells as well as from hematopoietic precursors. Ideally, a target antigen would be expressed exclusively on myeloma cells; however, the clinical success of, for example, rituximab, an antibody against CD20, which is expressed on malignant as well as on benign B cells, shows that side effects can be managed if pivotal cells, such as hematopoietic stem cells, are spared by target-oriented therapeutics.38 Demonstrating strong anti-myeloma effects of CD229 targeting alone or in combination with chemotherapy, our results are a first step towards the development of a novel and promising targeted anti-myeloma therapy.
Footnotes
Funding: this work was supported by grants from the Wilhelm Sander-Stiftung (to DA).
The online version of this article has a Supplementary Appendix.
Authorship and Disclosures
The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Palumbo A, Facon T, Sonneveld P, Blade J, Offidani M, Gay F, et al. Thalidomide for treatment of multiple myeloma: 10 years later. Blood. 2008;111(8):3968–77. doi: 10.1182/blood-2007-10-117457. [DOI] [PubMed] [Google Scholar]
- 2.Uy GL, Goyal SD, Fisher NM, Oza AY, Tomasson MH, Stockerl-Goldstein K, et al. Bortezomib administered pre-auto-SCT and as maintenance therapy post transplant for multiple myeloma: a single institution phase II study. Bone Marrow Transplant. 2009;43(10):793–800. doi: 10.1038/bmt.2008.384. [DOI] [PubMed] [Google Scholar]
- 3.Chang JE, Juckett MB, Callander NS, Kahl BS, Gangnon RE, Mitchell TL, et al. Thalidomide maintenance following high-dose melphalan with autologous stem cell support in myeloma. Clin Lymphoma Myeloma. 2008;8(3):153–8. doi: 10.3816/CLM.2008.n.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghosh N, Matsui W. Cancer stem cells in multiple myeloma. Cancer Lett. 2009;277(1):1–7. doi: 10.1016/j.canlet.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loh YS, Mo S, Brown RD, Yamagishi T, Yang S, Joshua DE, et al. Presence of Hoechst low side populations in multiple myeloma. Leuk Lymphoma. 2008;49(9):1813–6. doi: 10.1080/10428190802272676. [DOI] [PubMed] [Google Scholar]
- 6.Huff CA, Matsui W. Multiple myeloma cancer stem cells. J Clin Oncol. 2008;26(17):2895–900. doi: 10.1200/JCO.2007.15.8428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kyle RA, Rajkumar SV. Multiple myeloma. Blood. 2008;111(6):2962–72. doi: 10.1182/blood-2007-10-078022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tai YT, Li X, Tong X, Santos D, Otsuki T, Catley L, et al. Human anti-CD40 antagonist antibody triggers significant antitumor activity against human multiple myeloma. Cancer Res. 2005;65(13):5898–906. doi: 10.1158/0008-5472.CAN-04-4125. [DOI] [PubMed] [Google Scholar]
- 9.Tassone P, Gozzini A, Goldmacher V, Shammas MA, Whiteman KR, Carrasco DR, et al. In vitro and in vivo activity of the maytansinoid immunoconjugate huN901-N2′ - deacetyl - N2′ - (3 - mercapto - 1 -oxopropyl)-maytansine against CD56+ multiple myeloma cells. Cancer Res. 2004;64(13):4629–36. doi: 10.1158/0008-5472.CAN-04-0142. [DOI] [PubMed] [Google Scholar]
- 10.Tassone P, Goldmacher VS, Neri P, Gozzini A, Shammas MA, Whiteman KR, et al. Cytotoxic activity of the maytansinoid immunoconjugate B-B4-DM1 against CD138+ multiple myeloma cells. Blood. 2004;104(12):3688–96. doi: 10.1182/blood-2004-03-0963. [DOI] [PubMed] [Google Scholar]
- 11.Kapoor P, Greipp PT, Morice WG, Rajkumar SV, Witzig TE, Greipp PR. Anti-CD20 monoclonal antibody therapy in multiple myeloma. Br J Haematol. 2008;141(2):135–48. doi: 10.1111/j.1365-2141.2008.07024.x. [DOI] [PubMed] [Google Scholar]
- 12.Sandrin MS, Henning MM, Lo MF, Baker E, Sutherland GR, McKenzie IF. Isolation and characterization of cDNA clones for Humly9: the human homologue of mouse Ly9. Immunogenetics. 1996;43(1–2):13–9. doi: 10.1007/BF00186599. [DOI] [PubMed] [Google Scholar]
- 13.Tangye SG, Phillips JH, Lanier LL. The CD2-subset of the Ig superfamily of cell surface molecules: receptor-ligand pairs expressed by NK cells and other immune cells. Semin Immunol. 2000;12(2):149–57. doi: 10.1006/smim.2000.0217. [DOI] [PubMed] [Google Scholar]
- 14.Martin M, Del Valle JM, Saborit I, Engel P. Identification of Grb2 as a novel binding partner of the signaling lymphocytic activation molecule-associated protein binding receptor CD229. J Immunol. 2005;174(10):5977–86. doi: 10.4049/jimmunol.174.10.5977. [DOI] [PubMed] [Google Scholar]
- 15.Panse J, Friedrichs K, Marx A, Hildebrandt Y, Luetkens T, Bartels K, et al. Chemokine CXCL13 is overexpressed in the tumour tissue and in the peripheral blood of breast cancer patients. Br J Cancer. 2008;99(6):930–8. doi: 10.1038/sj.bjc.6604621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rawstron AC, Orfao A, Beksac M, Bezdickova L, Brooimans RA, Bumbea H, et al. Report of the European Myeloma Network on multiparametric flow cytometry in multiple myeloma and related disorders. Haematologica. 2008;93(3):431–8. doi: 10.3324/haematol.11080. [DOI] [PubMed] [Google Scholar]
- 17.Cory AH, Owen TC, Barltrop JA, Cory JG. Use of an aqueous soluble tetrazolium/formazan assay for cell growth assays in culture. Cancer Commun. 1991;3(7):207–12. doi: 10.3727/095535491820873191. [DOI] [PubMed] [Google Scholar]
- 18.Pellat-Deceunynck C, Bataille R, Robillard N, Harousseau JL, Rapp MJ, Juge-Morineau N, et al. Expression of CD28 and CD40 in human myeloma cells: a comparative study with normal plasma cells. Blood. 1994;84(8):2597–603. [PubMed] [Google Scholar]
- 19.Banham AH, Colonna M, Cella M, Mickelm KJ, Pulford K, Willis AC, et al. Identification of the CD85 antigen as ILT2, an inhibitory MHC class I receptor of the immunoglobulin superfamily. J Leukoc Biol. 1999;65(6):841–5. doi: 10.1002/jlb.65.6.841. [DOI] [PubMed] [Google Scholar]
- 20.Matsui W, Huff CA, Wang Q, Malehorn MT, Barber J, Tanhehco Y, et al. Characterization of clonogenic multiple myeloma cells. Blood. 2004;103(6):2332–6. doi: 10.1182/blood-2003-09-3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de la Fuente MA, Tovar V, Villamor N, Zapater N, Pizcueta P, Campo E, et al. Molecular characterization and expression of a novel human leukocyte cell-surface marker homologous to mouse Ly-9. Blood. 2001;97(11):3513–20. doi: 10.1182/blood.v97.11.3513. [DOI] [PubMed] [Google Scholar]
- 22.Howie D, Sayos J, Terhorst C, Morra M. The gene defective in X-linked lymphoproliferative disease controls T cell dependent immune surveillance against Epstein-Barr virus. Curr Opin Immunol. 2000;12(4):474–8. doi: 10.1016/s0952-7915(00)00123-0. [DOI] [PubMed] [Google Scholar]
- 23.Ma CS, Nichols KE, Tangye SG. Regulation of cellular and humoral immune responses by the SLAM and SAP families of molecules. Annu Rev Immunol. 2007;25:337–79. doi: 10.1146/annurev.immunol.25.022106.141651. [DOI] [PubMed] [Google Scholar]
- 24.Good KL, Avery DT, Tangye SG. Resting human memory B cells are intrinsically programmed for enhanced survival and responsiveness to diverse stimuli compared to naive B cells. J Immunol. 2009;182(2):890–901. doi: 10.4049/jimmunol.182.2.890. [DOI] [PubMed] [Google Scholar]
- 25.Fraser CC, Howie D, Morra M, Qiu Y, Murphy C, Shen Q, et al. Identification and characterization of SF2000 and SF2001, two new members of the immune receptor SLAM/CD2 family. Immunogenetics. 2002;53(10–11):843–50. doi: 10.1007/s00251-001-0415-7. [DOI] [PubMed] [Google Scholar]
- 26.Bottino C, Falco M, Parolini S, Marcenaro E, Augugliaro R, Sivori S, et al. NTB-A [correction of GNTB-A], a novel SH2D1A-associated surface molecule contributing to the inability of natural killer cells to kill Epstein-Barr virus-infected B cells in X-linked lymphoproliferative disease. J Exp Med. 2001;194(3):235–46. doi: 10.1084/jem.194.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Valdez PA, Wang H, Seshasayee D, van Lookeren Campagne M, Gurney A, Lee WP, et al. NTB-A, a new activating receptor in T cells that regulates autoimmune disease. J Biol Chem. 2004;279(18):18662–9. doi: 10.1074/jbc.M312313200. [DOI] [PubMed] [Google Scholar]
- 28.Peck SR, Ruley HE. Ly108: a new member of the mouse CD2 family of cell surface proteins. Immunogenetics. 2000;52(1–2):63–72. doi: 10.1007/s002510000252. [DOI] [PubMed] [Google Scholar]
- 29.Tovar V, del Valle J, Zapater N, Martin M, Romero X, Pizcueta P, et al. Mouse novel Ly9: a new member of the expanding CD150 (SLAM) family of leukocyte cellsurface receptors. Immunogenetics. 2002;54(6):394–402. doi: 10.1007/s00251-002-0483-3. [DOI] [PubMed] [Google Scholar]
- 30.Bouchon A, Cella M, Grierson HL, Cohen JI, Colonna M. Activation of NK cell-mediated cytotoxicity by a SAP-independent receptor of the CD2 family. J Immunol. 2001;167(10):5517–21. doi: 10.4049/jimmunol.167.10.5517. [DOI] [PubMed] [Google Scholar]
- 31.Kumaresan PR, Lai WC, Chuang SS, Bennett M, Mathew PA. CS1, a novel member of the CD2 family, is homophilic and regulates NK cell function. Mol Immunol. 2002;39(1–2):1–8. doi: 10.1016/s0161-5890(02)00094-9. [DOI] [PubMed] [Google Scholar]
- 32.Hsi ED, Steinle R, Balasa B, Szmania S, Draksharapu A, Shum BP, et al. CS1, a potential new therapeutic antibody target for the treatment of multiple myeloma. Clin Cancer Res. 2008;14(9):2775–84. doi: 10.1158/1078-0432.CCR-07-4246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Romero X, Benitez D, March S, Vilella R, Miralpeix M, Engel P. Differential expression of SAP and EAT-2-binding leukocyte cell-surface molecules CD84, CD150 (SLAM), CD229 (Ly9) and CD244 (2B4) Tissue Antigens. 2004;64(2):132–44. doi: 10.1111/j.1399-0039.2004.00247.x. [DOI] [PubMed] [Google Scholar]
- 34.Sintes J, Romero X, Marin P, Terhorst C, Engel P. Differential expression of CD150 (SLAM) family receptors by human hematopoietic stem and progenitor cells. Exp Hematol. 2008;36(9):1199–104. doi: 10.1016/j.exphem.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chatterjee M, Chakraborty T, Tassone P. Multiple myeloma: monoclonal antibodies-based immunotherapeutic strategies and targeted radiotherapy. Eur J Cancer. 2006;42(11):1640–52. doi: 10.1016/j.ejca.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 36.Liu AY, Robinson RR, Hellstrom KE, Murray EDJ, Chang CP, Hellstrom I. Chimeric mouse-human IgG1 antibody that can mediate lysis of cancer cells. Proc Natl Acad Sci USA. 1987;84(10):3439–43. doi: 10.1073/pnas.84.10.3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Natsume A, Niwa R, Satoh M. Improving effector functions of antibodies for cancer treatment: Enhancing ADCC and CDC. Drug Des Devel Ther. 2009;3:7–16. [PMC free article] [PubMed] [Google Scholar]
- 38.Grillo-Lopez AJ. Rituximab: an insider's historical perspective. Semin Oncol. 2000;27(6 Suppl 12):9–16. [PubMed] [Google Scholar]