Abstract
Advances in genomics and related fields are promising tools for risk assessment, early detection, and targeted therapies across the entire cancer care continuum. In this commentary, we submit that this promise cannot be fulfilled without an enhanced translational genomics research agenda firmly rooted in the population sciences. Population sciences include multiple disciplines that are needed throughout the translational research continuum. For example, epidemiologic studies are needed not only to accelerate genomic discoveries and new biological insights into cancer etiology and pathogenesis, but to characterize and critically evaluate these discoveries in well defined populations for their potential for cancer prediction, prevention and response to treatments. Behavioral, social and communication sciences are needed to explore genomic-modulated responses to old and new behavioral interventions, adherence to therapies, decision-making across the continuum, and effective use in health care. Implementation science, health services, outcomes research, comparative effectiveness research and regulatory science are needed for moving validated genomic applications into practice and for measuring their effectiveness, cost effectiveness and unintended consequences. Knowledge synthesis, evidence reviews and economic modeling of the effects of promising genomic applications will facilitate policy decisions, and evidence-based recommendations. Several independent and multidisciplinary panels have recently made specific recommendations for enhanced research and policy infrastructure to inform clinical and population research for moving genomic innovations into the cancer care continuum. An enhanced translational genomics and population sciences agenda is urgently needed to fulfill the promise of genomics in reducing the burden of cancer.
Keywords: cancer, genetics, genomics, medicine, population sciences, public health, translation
The Widening Gap between Basic Genomic Discoveries and Their Impact on the Population Burden of Cancer
Advances in genomics and other “omics” fields are ushering in a new era of clinical practice in cancer care and prevention including better tumor classification, prognostic markers, predictive indicators of drug response, and the development of new drug therapies, and strategies for monitoring disease (1-4). For decades, many genes have been known to be related to cancer susceptibility, with a strong integration of medical genetics into oncology practice (5). However, the new tools of genomics (including large scale genotyping, sequencing, as well as the study of gene expressions, proteomics, epigenomics) in both germ cell and cancer tissues are paving the way for a more personalized practice of cancer care involving the development of targeted therapies as well as the identification of diagnostic markers for early detection and prognosis (1, 2, 6). Numerous genetic variants have been discovered in relation to cancer etiology using population based genome-wide association studies (GWAS) (7). In addition, many genome-based tests, including personal genome profiles, are already available and some are marketed directly to consumers (8). In an online knowledge base of all new genome-based tests and applications that have either reached the commercial marketplace, or are under development in clinical trials, there are more than 250 new tests in the past year (as of May 1, 2011), most of which are related to cancer (9). Nevertheless, translation of these discoveries into clinical practice and health benefits has been slow (3). In contrast to the implementation of testing for high-penetrance alleles in those with a family history where benefit to individuals and families has been clear, implementation of testing for low-penetrance alleles and other complex biomarkers has unclear benefits and risks. Skepticism still abounds as to the near term value of this emerging technology to reduce the burden of cancer. This can be attributed to a number of factors, including incomplete information on: biological pathways and functions, genotype-outcomes relationships, gene-environment and gene-drug interactions, clinical utility of genomic information in improving health outcomes, as well as behavioral and social factors affecting comprehension, uptake, and impact. There is also a lack of understanding of the validity and utility, effectiveness and cost effectiveness of genomic applications in cancer care and prevention compared with existing standards of care and prevention that do not use genomic approaches (10). Finally, there has been very little information to inform best approaches to implement genomic applications in practice; ensure quality of testing and decision-making processes; educate providers, patients, and the general public; influence public policy; and measure impact on population health outcomes (11-14). In the setting of a US healthcare system that does not provide even basic primary care to a substantial proportion of the population, a strong case needs to be made why, at this point, we should add genomic medicine to the mix. Hence, we see an important emerging role for population sciences not only in facilitating translation of genomic discoveries but also in providing an important scientific perspective for assessing the promise and potential unintended consequences of genomics in cancer control and prevention.
The Emerging Role of Population Sciences in Closing the Genomics Translation Gap
The path from basic science discovery to improved population health outcomes involves several overlapping and nonlinear phases of translational research as described in detail elsewhere (15, 16). Translational research is guided by knowledge synthesis and evidence based recommendations as shown in Figure 1. Traditionally, research investments are heavily concentrated in discovery (T0) and the first phase of translation (T1 or bench to bedside) (16). The outcomes of discovery and early translational research are promising tests, drugs and other interventions (e.g., policy or environmental) that need to be evaluated for their validity and utility in clinical and population settings. To fulfill the promise of these applications to improve health, a robust “post bedside” translational research agenda is needed to evaluate the efficacy of the new applications leading up to evidence based recommendations and policies for their use (T2), to conduct implementation and dissemination science to move discoveries into practice and control programs (T3) and to assess effectiveness, cost effectiveness and outcomes at the population level (T4) (15, 16) (summarized in Figure 1). In order to achieve a post bedside translational research agenda, population sciences are crucial. Population sciences encompass multiple disciplines, including among others, epidemiology (17, 18), behavioral, social and communication sciences (19, 20), implementation and dissemination research (21), health services and comparative effectiveness and outcomes research (22, and regulatory science (23). Population sciences are involved at each step of the translational research continuum and their role predominates in the latter phases of translation (T2 and beyond, 16). Even though population sciences have traditionally made individual contributions to advancing cancer genomics, the influence of these disciplines is best realized when working together with basic and clinical sciences as part of “team” or transdisciplinary science (24). In the rapidly moving field of cancer genomics, randomized clinical trials (RCTs) may not be always feasible or affordable to establish efficacy and effectiveness of new interventions. Although RCTs have been the primary source of information on the predictors of treatment efficacy, adverse outcomes and safety, such studies often are of limited size and duration making it difficult to study rare and long-term events such as cancer and effects of cancer treatment, and they also often under-represent patients with chronic or comorbid health conditions, advanced age, socioeconomic disparities, and diverse ethnicities. In many situations, data (such as on comorbid conditions and lifestyle factors) and specimens may not be available or collected in adequate numbers within existing clinical trials and preclude ancillary studies to answer important clinical questions relevant to cancer genomics. Therefore, well-conducted observational population-based studies, pragmatic and adaptive trials (25-27), carefully monitored natural experiments, simulation modeling (28), and studies based on electronic health records in health care systems (29) will become even more important research tools to complement RCTs in translational genomics in the years to come.
Figure 1. Phases of Translational Research in Cancer Genomics: Beyond Bench to Bedside (adapted from reference 15).
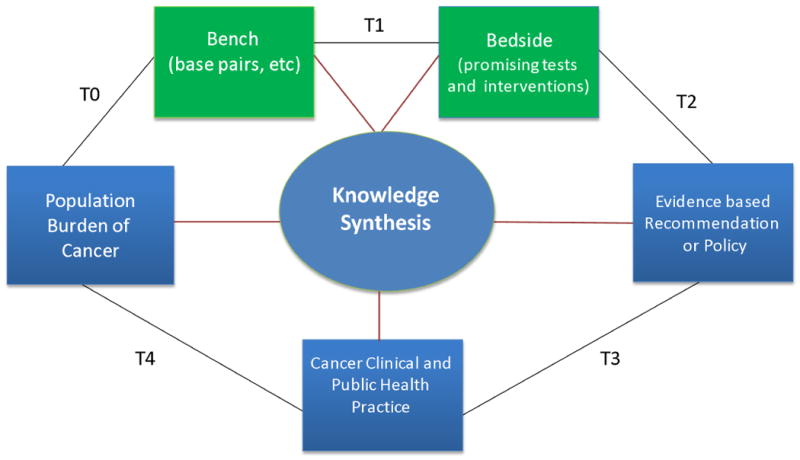
Table 1 illustrates how selected population sciences can address scientific questions that can help close the translation gap of how genomic discoveries contribute to the cancer care continuum, both in healthy and affected persons in community and cancer care settings. In primary care and population settings, knowledge of genes involved in cancer etiology can be used in risk assessment, targeted prevention and early detection as well as reducing the burden of cancer risk factors based on genetic information relevant to behavioral, pharmacologic and environmental interventions. In cancer care settings molecular characterization of tumors, prognostic indicators, pharmacogenomic testing can be used to enhance the safety and effectiveness of cancer therapeutics and improve health outcomes. We then use several examples from population sciences with a specific case approach focus on Lynch syndrome to illustrate the progression along the T1-T4 continuum. For T1 research, through NCI funded epidemiologic consortia, genome-wide association studies (GWAS) have led to the uncovering and risk characterization of numerous low penetrance genes for cancer etiology (30-37). These findings are giving important clues regarding mechanisms of cancer etiology and pathogenesis, with the potential for discovery and development of new intervention targets. For T2 research, a prominent example in cancer is the HER-2/neu oncogene; Slamon et al. show that the amplification of HER-2/neu oncogene correlates with a shorter time to relapse and lower survival rate in women with breast cancer in two independent observational study cohorts (38). These studies led to the development and approval of the target monoclonal antibody Herceptin for the treatment of breast cancer (39). Additional examples of T2 research include recent population-based studies that have evaluated and synthesized information on various prognostic, pharmacogenomic and predictive genomic markers leading to evidence based recommendations for use in practice. Another example is KRAS mutational analysis in the treatment of colorectal cancer. Two observational studies demonstrated that mutations in the KRAS gene were associated with non-response in patients treated for metastatic CRC with Cetuximab. This led to confirmatory studies conducted on specimens collected in completed RCTs (40, 41). In behavioral science, there is an evolving literature at the intersection of behavior, genes and cancer. For example, there have been suggestions that dysregulation in the ras proto-oncogene might play a role in the observed association between depression and later onset of cancer (42). In T3 research, there is a rich literature on the psychosocial factors relevant to counseling for BRCA1 and treatment decisions (e.g. 43-45). The impact of knowledge of low penetrance genes for colorectal cancer on screening behavior and quality of life was recently investigated by Ramsey et al in a population-based study (46). More recently, Bloss et al. investigated the psychobehavioral impact of personal genome profile tests available directly to consumers on health individuals seeking these tests (8). In T4 research, multicenter follow up studies have documented in “real world” settings how implementation of validated genomic applications can reduce the burden of cancer (e.g., showing drastic reduction of mortality with prophylactic surgery among BRCA1 patients in a multicenter observational cohort study, 47).
Table 1. Role of Population Sciences in Translating Genomic Discoveries to Reduce the Burden of Cancer, by context of use of genomic information, and type of population discipline *.
| Scientific Disciplines | General Population/Primary Care | Cancer Care |
|---|---|---|
| I. Epidemiologic and clinical research (T1-T2) | Cohort and case-control population studies can identify and characterize genetic risks, interactions with modifiable risk factors, and evaluate performance and added value of genomics as cancer risk predictors; these studies can also lead to biological insight on causes and pathways in cancer development; as well as inform population surveillance. | Follow up observational studies in cancer care settings assess how tumor and germ line genomic factors can predict treatment response, side effects, prognosis, recurrence mortality and quality of life indicators; evaluate how these factors interact with non-genomic factors in predicting various outcome; these studies can also lead to biological insight into pathways of cancer progression and response to various interventions |
| Examples | Numerous recent findings from GWA studies of various cancers (30-37) | Mutations in the KRAS gene is associated with non-response in patients treated for metastatic CRC with Cetuximab (38, 39) HER2 discovery and correlation with outcomes led to the development of targeted monoclonal antibody, herceptin, which is now part of breast cancer treatment (40, 41) |
| II. Behavioral, social and communication sciences | Studies that assess public & provider understanding of genomic information, evaluate how genomics can improve risk communication, and health behavior change, and use genomics to identify behavioral & environmental intervention targets | Studies that assess patients' understanding & use of genomic information to improve decision making regarding treatment options, assess how behavioral, communication and social factors can modulate impact of targeted genomic based interventions to motivate health behavior and environmental changes |
| Examples | Assessing the psychobehavioral impact of personal genomic profile tests on healthy individuals (8) | Assessing psychological predictors of BRCA counseling and testing decisions among African-American women (44) |
| III. Knowledge synthesis and evidence-based recommendations | Systematic reviews, meta analysis and modeling of basic, clinical and population data to guide evidence recommendations on use of genomic information in reducing cancer occurrence as well as inform additional research and stakeholder decision making | Systematic reviews, meta analysis and modeling of basic, clinical and population data to guide evidence recommendations on use of genomic information in improving cancer care and outcomes, as well as informing additional research and stakeholder decision making |
| Examples | EGAPP knowledge synthesis and recommendation that all new cases of CRC be tested for Lynch syndrome to reduce CRC morbidity and mortality in relatives (52) | EGAPP knowledge synthesis and recommendation that all breast cancer gene expression profiles have insufficient evidence to drive treatment of breast cancer in women-called for RCTs to be done (63) |
| IV. Health services, comparative effectiveness &, outcomes research & implementation science | Studies that assess multilevel determinants of implementation, dissemination and outcomes of genomic information in reducing the population burden of cancer; These include provider and consumer education, policies, coverage, access to services, and cost-effectiveness analyses. Understanding ways to of evidence recommendations (personal, familial, community & health systems) | Studies that assess multilevel factors for implementation and outcomes of using genomic information in cancer care settings. These include patient and provider factors, health care organization factors, policies, coverage and access and cost- effectiveness analyses Understanding ways to increase uptake of evidence recommendations (evidence on rapidly learning healthcare systems) |
| Examples | Cancer prevention and screening practices among women at risk for hereditary breast and ovarian cancer in community settings (43) | Multicenter follow-up study documenting drastic decline in on cancer screening and early mortality in BRCA1 carriers following prophylactic surgery (47) |
A specific aspect of T3 research is assessing how consumers will process and make use of genomic information, particularly given its wide availability. Effective comprehension of this information requires a high level of health literacy and numeracy, yet significant portions of the population do not achieve this high level (48). Moreover, a host of psychological processes can influence responses to the information. For example, some have cautioned that smokers who learn they do not possess the CYP2A6 polymorphism (which has been linked to tobacco dependence) might be less inclined to quit (49), and smokers who believe that lung cancer is genetically predetermined might also be less interested in quitting (50). Genetic risk information could be interpreted differentially depending upon beliefs in fatalism, cultural beliefs, and mental models of disease.
Lynch syndrome illustrates how multiple population sciences have converged to address epidemiological, knowledge synthesis and implementation issues influencing both affected patients and their asymptomatic relatives along the T1-T4 continuum. Lynch syndrome is a relatively common group of autosomal dominant conditions, accounting for approximately 3% of all colorectal cancer (CRC) cases in the United States (51). In 2009, the independent multidisciplinary Evaluation of Genomic Applications in Practice and Prevention (EGAPP) working group recommended screening for Lynch syndrome in all newly diagnosed CRC cases in order to reduce morbidity and mortality in family members (52). This is based on systematic knowledge synthesis of epidemiological information of the prevalence, penetrance, morbidity and mortality in these cases, and findings from intervention studies coupled with early detection in relatives (53, 54). Cost effectiveness analyses have provided additional information on the value of screening for Lynch syndrome in the population (55). There are multiple challenges for exploring how to implement such a recommendation that will require additional data from pilot studies. To that end, the Centers for Disease Control and Prevention (CDC) in collaboration with NCI convened a multidisciplinary working meeting surrounding the issues in implementation of Lynch syndrome screening (Bellcross et al., submitted). Challenges at individual, family, system and policy levels were identified at the meeting leading to clinical and population research strategies. Challenges include lack of provider knowledge of Lynch syndrome and testing issue, ethical issues related to informed consent among probands, use of genetic services, responsibility and psychological impact of cascading from probands to relatives (recently documented by Hadley et al., 56); patient, provider and relatives' compliance, public health and policy infrastructure needs, as well as cost effectiveness for implementation. Thus, population sciences will inform the evolving knowledge for implementation and evaluation of Lynch syndrome cascade screening.
Limited Investment in Translational Genomics and Population Sciences
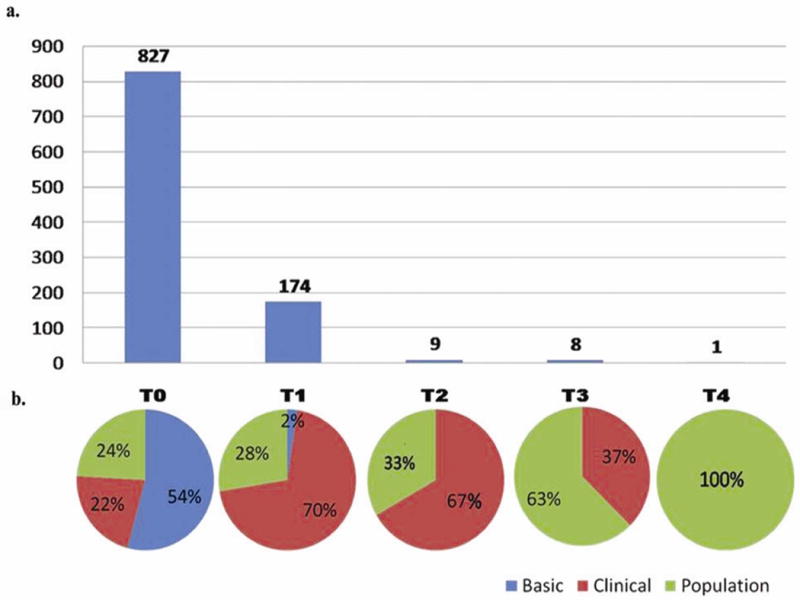
We recently published a portfolio analysis of cancer genomic research funded by the National Cancer Institute showing that less than 2% of funded research is post “bench to bedside” (Figure 2, 16). Moreover, less than 1% of published cancer genomic research is post bedside (16). Although epidemiologic studies are well represented in discovery and early translation through the numerous consortia that NCI has funded, they, along with other population disciplines are severely underrepresented in T2 and beyond. Using funding provided through the American Recovery and Reconstruction Act (ARRA), NCI has tried to fill part of the translation gap through investment in comparative effectiveness research. In 2009, NCI funded a network of 7 research groups to perform knowledge generation and synthesis projects in comparative effectiveness research (CER) in genomic medicine (57). Examples of these projects include: 1) enabling efficient and accurate collection and integration into electronic medical records of personal, family and genomic information for risk assessment and delivery of decision support to providers and patients; 2) conducting CER on the genomics of colorectal cancer (CRC) including evaluating the cost-effectiveness for genetic testing of Lynch Syndrome and KRAS testing in CRC treatment management; 3) developing biospecimen and data registries to support evidence generation and clinical effectiveness research for evaluating pharmacogenomic markers in lung and breast cancer; 4) developing an information infrastructure for CER; 5) CDKN2A/p16 testing and adherence to melanoma prevention behaviors; 6) collaboration with external stakeholders, decision modeling, database linkage, ethics, policy, and clinical trial design to leverage the Southwest Oncology Group clinical trials network; and 7) clinical validity and utility of genomic testing for targeted chemoprevention for prostate cancer. Although the work of this group is still ongoing, it is making substantial contributions to the development of clinical and population study platforms to evaluate genomic applications and the evidentiary approaches to genomic applications in the cancer care continuum (57). Their work also highlights the need for enhanced research infrastructure and platforms in order to conduct translational projects (e.g. access to patient cohorts, biorepositories, electronic health records, and bioinformatics (58).
Figure 2. Numbers and Types of NCI Extramural Funded Cancer Genomics Research in FY2007, By Phase of Translation (from reference 16).
Knowledge Synthesis to Drive Genomics Research, Policy and Practice
Even though many genomic applications are being developed, most currently do not have sufficient evidence to evaluate their clinical validity and utility in practice. The rapid emergence of information on genomic applications requires studies in well defined population groups to evaluate their significance and utility for reducing the burden of cancer as well as advanced methods of systematic reviews using biological, clinical and population data. Additional types of reviews can address concerns of clinicians, health policy makers, health plan administrators, citizen advocates, and other stakeholders, and answer specific questions on what works for what subgroups under what conditions in order to move genomics into large scale applications (59-61).
In order to drive research, policy and practice, CDC, in collaboration with NCI and other partners, sponsors an independent multidisciplinary, nonfederal working group (Evaluation of Genomic Applications in Practice and Prevention, EGAPP) (62) The EGAPP Working Group systematically reviews, synthesizes and updates evidence of validity and utility of genomic applications and makes recommendations for appropriate use. Several recommendations have been issued to date and more are under way (a total of 10, 6 of which are relevant to cancer, including “insufficient evidence” on gene expression profiling in the management of breast cancer [63]). In the process of knowledge synthesis, stakeholder engagement is crucial to understanding various perspectives on how much evidence is needed to cross an evidentiary threshold from research to clinical practice (64). An enhanced collaboration is needed among basic scientists, industry, consumers, clinicians, regulators, payers and policy decision makers using a population perspective (65). This is currently being undertaken by the NCI funded comparative effectiveness research network in cancer genomic medicine (Deverka et al., in preparation).
Recommendations from Recent Multidisciplinary Panels for an Enhanced Population Science Agenda in Translational Genomics
Table 2 summarizes the recommendations for enhancing the population sciences agenda in genomic medicine from several independent panels such as the President's Council of Advisors on Science and Technology (66), the Institute of Medicine (reports on cancer biomarkers (67) and comparative effectiveness research (68), as well as multidisciplinary workshops sponsored and cosponsored by the NCI. The workshops covered a wide variety of topics such as the scientific foundation for the use of genetic risk profiles in risk assessment and disease prevention (69); accelerating discovery and translation of pharmacogenomic applications in the cancer care continuum (70); the role of behavioral, social and communication sciences in fulfilling the potential of genomic applications (71); the use of health services research in implementation and evaluation of genomic applications in cancer (72); and the use of comparative effectiveness research methods in outcome evaluations of genomic applications as well as evidence synthesis and modeling of effects (Goddard in preparation). In addition, issues relevant to implementation in community settings need to be addressed early in the translational research cycle and not delayed until research has been completed to find out major flaws that can interfere with the implementation of genomic applications into practice (73, 74). The emerging picture is that of a rich and nuanced translational genomics research agenda firmly rooted in population sciences. This research agenda can supplement and extend, now and in the future, cancer genomics research in basic sciences and clinical trials.
Table 2. Synopsis of Recommendations from Recent Selected Independent and NIH Sponsored Multidisciplinary Panels and Working Groups for Enhancing the Population Sciences Agenda in Cancer Translational Genomics.
| Workshop/Panel | Goals/description | Recommendations |
|---|---|---|
| President's Council of Advisors on Science and Technology (66) | Identify scientific priorities for personalized medicine | Integrated nationwide network of standardized biospecimen science and repositories; research for validating clinical utility; large US population cohort study investigating genetic and environmental health impacts (selected recommendations) |
| Institute of Medicine report on cancer biomarkers (67) | Review cancer biomarker research, development and implementation | Develop high quality biorepositories in prospectively collected samples; create well defined consensus standards and guidelines for biomarker development validation and use; establish high quality population-based assessments of efficacy and cost-effectiveness of biomarker tests (selected recommendations) |
| Institute of Medicine report on comparative effectiveness research (68) | Establish a definition of comparative effectiveness research and a national top 100 priority list | Compare the effectiveness of adding new biomarkers (including genetic information) with standard care in motivating behavior change and improving clinical outcomes; compare the effectiveness of genetic and biomarker testing and usual care in preventing and treating breast, colorectal, prostate, lung, and ovarian cancer (selected recommendations) |
| NIH- CDC (69) | Enhancing the scientific foundation for using genetic risk profiles in risk assessment and disease prevention | Develop scientific standards for personal genomic tests; enhance multidisciplinary population research; enhance credible knowledge synthesis and dissemination to providers, consumers and policy makers; explore the value of personal utility of genetic information |
| NCI pharmacoepi & Pharmacogenomics working group (70) | Setting a research agenda in pharmacoepidemiology and pharmacogenomics to accelerate translation | Develop and support a knowledge synthesis study group; support observational studies that assess genomic and nongenomic factors affecting treatment response and adverse effects; support research on the utility of promising pharma cogenomic applications in practice; support efforts that integrate basic, clinical and population research |
| NHGRI multidisciplinary panel (71) | Priorities for behavioral, social and communications research | Research to improve the public's genetic literacy to enhance consumer skills; Assess if genomic information improves risk communication and adoption of healthy behaviors more than current approaches; explore if genomics can lead to new behavioral intervention targets; consider multiple levels of influence that contribute to public health problems |
| NCI workshop (72) | Examine the state of health services research in cancer cellular, molecular and genomic technologies; identify priorities for expanding knowledge base | Development of a comprehensive research agenda on health and safety endpoints, utilization patterns, patient and provider preferences, quality of care and access, disparities, economics and quality of life |
| NCI genomics & pesonalized medicine comparative effectiveness research methods working group (Goddard, in prep) | Identify CER approaches that can be employed to answer questions about cancer genomic applications faced by various stakeholders | Several CER approaches can be applied to cancer genomics including, evidence generation and synthesis, stakeholder engagement, in trials and observational studies; decision modeling and economic analyses |
Concluding Remarks
To summarize, there is a large and widening gap between the promise of cancer genomics and the current reality of its impact on cancer care and prevention. We have highlighted the increasing role and need for multiple population sciences to close this translation gap. Population disciplines include, among others, epidemiology, behavioral, social and communication sciences, implementation sciences, health services and comparative effectiveness research. Nevertheless, the current investment in cancer translational genomics research in these disciplines is severely limited. Several recent independent panels and NIH sponsored workshops have recommended increased emphasis and investment in these translational genomics and population sciences. Ideally, such investment should be part of transdisciplinary groups, involving basic, clinical and population sciences. Such an enhanced research agenda in genomics and population sciences is crucial to fulfill the promise of genomics in reducing the global burden of cancer in the 21st century.
Footnotes
The opinions in this article reflect those of the authors and do not necessarily reflect the official position of the CDC or NCI.
In this portfolio analysis, the categories Basic, Clinical and Population were defined as follows
Basic: Laboratory/“bench”-based: characterized by the use and study of human specimens or animal models.
Clinical: Clinic-based application of laboratory techniques and findings to diagnosis, treatment or management of patients.
Population: Characterized by a well-defined community, collaboration-based platforms, large number of human subjects drawn from the general population
References
- 1.McDermott U, Downing JR, Stratton MR. Genomics and the continuum of cancer care. New Engl J Med. 2011;364(4):340–50. doi: 10.1056/NEJMra0907178. [DOI] [PubMed] [Google Scholar]
- 2.Calzone K, Wattendorf D, Dunn BK. The application of genetics and genomics to cancer prevention. Sem Oncol. 2010;37(4):407–18. doi: 10.1053/j.seminoncol.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Varmus H. Ten years on- the human genome and medicine. New Engl J Med. 2010;362(21):2028–9. doi: 10.1056/NEJMe0911933. [DOI] [PubMed] [Google Scholar]
- 4.Lander ES. Initial impact of the sequencing of the human genome. Nature. 2011;470(7333):187–97. doi: 10.1038/nature09792. [DOI] [PubMed] [Google Scholar]
- 5.Plon SE. Unifying cancer genetics. Genet Med. 2011;13(3):203–4. doi: 10.1097/GIM.0b013e31820d5e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ladanyi M, Hogendoom PCW. Cancer biology and genomics: translating discoveries, transforming pathology. J Pathol. 2011;223(2):99–101. doi: 10.1002/path.2812. [DOI] [PubMed] [Google Scholar]
- 7.Stadler ZK, Vijai J, Thom P, et al. Genomewide association studies of cancer predisposition. Hematol Oncol Clin North Am. 2010;24(5):973–996. doi: 10.1016/j.hoc.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Bloss CS, Schork NJ, Topol EJ. Effect of direct-to-consumer genomewide profiling to assess disease risk. New Engl J Med. 2011;364(6):524–34. doi: 10.1056/NEJMoa1011893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gwinn M, Grossnicklaus D, Yu W, et al. Horizon scanning for new genomic tests. Genet Med. 2011;13(2):161–5. doi: 10.1097/GIM.0b013e3182011661. [DOI] [PubMed] [Google Scholar]
- 10.Friends of Cancer Research. Improving medical decisions through comparative effectiveness research: cancer as a case study. [Accessed online April 5, 2011]; at: http://focr.org/files/CER_REPORT_FINAL.pdf.
- 11.Khoury MJ, Berg A, Coates RC, Teutsch SM, Bradley LA. The evidence dilemma in genomic medicine. Health Affairs. 2008;27(6):1600–11. doi: 10.1377/hlthaff.27.6.1600. [DOI] [PubMed] [Google Scholar]
- 12.Taylor BS, Ladanyi M. Clinical cancer genomics: how soon is now. J Pathol. 2011;223(2):318–26. doi: 10.1002/path.2794. [DOI] [PubMed] [Google Scholar]
- 13.Swanton C, Caldas C. From genomic landscapes to personalized cancer management- is there a road map? Ann NY Acad Sci. 2010;1210:34–44. doi: 10.1111/j.1749-6632.2010.05776.x. [DOI] [PubMed] [Google Scholar]
- 14.Phillips KA. Closing the evidence gap in the use of emerging testing technologies in clinical practice. JAMA. 2008;300(21):2542–4. doi: 10.1001/jama.2008.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khoury MJ, Gwinn M, Yoon PW, et al. The continuum of translation research in genomic medicine: how can we accelerate the appropriate integration of human genome discoveries into health care and disease prevention? Genet Med. 2007;9(10):665–674. doi: 10.1097/GIM.0b013e31815699d0. [DOI] [PubMed] [Google Scholar]
- 16.Schully SD, Benedicto CB, Gillanders EM, Wang SS, Khoury MJ. Translational research in cancer genetics: the road less traveled. Publ Health Genomics. 2011;14(1):1–8. doi: 10.1159/000272897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spitz M, Bondy ML. The evolving discipline of molecular epidemiology of cancer. Carcinogenesis. 2010;31(1):127–34. doi: 10.1093/carcin/bgp246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartman M, Loy EY, Ku CS, Chia KS. Molecular epidemiology and its current use in cancer management. Lancet Oncol. 2010;11(4):383–90. doi: 10.1016/S1470-2045(10)70005-X. [DOI] [PubMed] [Google Scholar]
- 19.McBride CM, Koehly LM, Sanderson SC, Kaphingst KA. The behavioral response to personalized genetic information: will genetic risk profiles motivate individuals and families chose more healthful behaviors? Ann Rev Publ Health. 2010;31:89–103. doi: 10.1146/annurev.publhealth.012809.103532. [DOI] [PubMed] [Google Scholar]
- 20.Condit CM. Public understandings of risks from gene-environment interaction in common diseases: implications for public communications. Publ Health Genomics. 2011;14(2):115–124. doi: 10.1159/000314915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rabin BA, Glasgow RA, Kerner JF, Klump MP, Brownson RC. Dissemination and implementation research on community-based cancer prevention: a systematic review. Am J Prev Med. 2010;38(4):443–56. doi: 10.1016/j.amepre.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 22.Khoury MJ, Rich EC, Randhawa G, Teutsch SM, Niederhuber J. Comparative effectiveness research and genomic medicine: an evolving relationship for 21st century medicine. Genet Med. 2009;11(10):707–711. doi: 10.1097/GIM.0b013e3181b99b90. [DOI] [PubMed] [Google Scholar]
- 23.Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. 2010;363(4):301–304. doi: 10.1056/NEJMp1006304. [DOI] [PubMed] [Google Scholar]
- 24.Stokols D, Hall KL, Taylor BK, Moser RP. The science of team science: overview of the field and introduction to the supplement. Am J Prev Med. 2008;35(suppl 2):77–89. doi: 10.1016/j.amepre.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Milstein B, Homer J, Hirsch SM. Analyzing national health reform strategies with a dynamic simulation model. Am J Public Health. 2010;100(5):811–819. doi: 10.2105/AJPH.2009.174490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Avorn J. In defense of pharmacoepidemiology: embracing the yin and the yang of drug research. N Engl J Med. 2007;357(22):2219–21. doi: 10.1056/NEJMp0706892. [DOI] [PubMed] [Google Scholar]
- 27.Atkins D. Creating and synthesizing evidence with decision makers in mind. Integrating evidence from clinical trials and other study designs. Med Care. 2007;45(12 suppl 2):S16–22. doi: 10.1097/MLR.0b013e3180616c3f. [DOI] [PubMed] [Google Scholar]
- 28.Mercer SM, DeVinney BJ, Fine LJ, Green LW. Study designs for effectiveness and translation research: Identifying trade-offs. Am J Prev Med. 2007;33(2):139–154. doi: 10.1016/j.amepre.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 29.Institute of Medicine. The learning healthcare system. Washington D.C.: National Academies Press; 2007. [Google Scholar]
- 30.Hirschhorn JN, Gajdos ZK. Genomewide association studies: results from the first few years and potential implications for clinical medicine. Ann Rev Med. 2011;62:11–24. doi: 10.1146/annurev.med.091708.162036. [DOI] [PubMed] [Google Scholar]
- 31.Thomas G, Jacobs KB, Kraft P, et al. A multistage genome-wide association study in breast cancer identifies two new risk alleles at 1p11.2 and 14q24.1 (RAD51L1) Nat Genet. 2009;41(5):579–84. doi: 10.1038/ng.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Antoniou AC, Wang X, Fredericksen ZS, et al. A locus on 19p13 modifies risk of breast cancer in BRCA1 mutation carriers and is associated with hormone-receptor negative breast cancer in the general population. Nat Genet. 2010;42(10):885–892. doi: 10.1038/ng.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maris JM, Mosse YP, Bradfield JP, et al. Chromosome 6p22 locus associated with clinically aggressive neuroblastoma. New Engl J Med. 2008;358(24):2585–2593. doi: 10.1056/NEJMoa0708698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petersen GM, Amundadottir L, Fuchs CS, et al. A genomewide association study identifies pancreatic cancer susceptibility loci on chromosomes 13q22.1, 1q32.1 and 5p15. 33 Nat Genet. 2010;42(3):224–8. doi: 10.1038/ng.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sun J, Zheng SL, Wiklund F, et al. Sequence variants at 22q13 are associated with prostate cancer risk. Cancer Res. 2009;69(1):10–5. doi: 10.1158/0008-5472.CAN-08-3464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Landi MT, Chatterjee N, Yu K, et al. A genomewide association study of lung cancer identifies a region of chromosome 15p15 associated with risk for adenocarcinoma. Am J Hum Genet. 2009;85(5):679–91. doi: 10.1016/j.ajhg.2009.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tenesa A, Farrington SM, Prendergast JG, et al. Genomewide association scan identifies a colorectal cancer susceptibility locus on 11q23 and replicates risk loci at 8q24 and 18q21. Nat Genet. 2008;40(5):631–40. doi: 10.1038/ng.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Slamon DJ, Clark GM, Wong SG, et al. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235(4785):177–82. doi: 10.1126/science.3798106. [DOI] [PubMed] [Google Scholar]
- 39.Moasser MM. Targeting the function of the HER2 oncogene in human cancer therapeutics. Oncogene. 2007;26(46):6577–92. doi: 10.1038/sj.onc.1210478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang G, Kelley RK. KRAS mutational analysis for colorectal cancer. PLoS Curr. 2010 Sep 2;2 doi: 10.1371/currents.RRN1175. pii: RRN1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dahabreh IJ, Terasawa T, Castaldi PJ, Trikalinos TA. Systematic review: Anti epidermal growth factor receptor treatment effect modification by KRAS mutations in advanced colorectal cancer. Ann Int Med. 2011;154(2):37–49. doi: 10.7326/0003-4819-154-1-201101040-00006. [DOI] [PubMed] [Google Scholar]
- 42.Brewer JK. Behavior genetics of the cancer/depression correlation: a look at the Ras oncogene family and the “cerebral diabetes paradigm”. J Mol Neurosci. 2008;35(3):307–22. doi: 10.1007/s12031-008-9078-2. [DOI] [PubMed] [Google Scholar]
- 43.Morgan D, Sylvester H, Lucas FL, et al. Cancer prevention and screening practices among women at risk for hereditary breast and ovarian cancer after genetic counseling in the community setting. Fam Cancer. 2009;8:277–287. doi: 10.1007/s10689-009-9242-z. [DOI] [PubMed] [Google Scholar]
- 44.Thompson HS, Valdimardottir HB, Duteau-Buck C, et al. Psychosocial predictors of BRCA counseling and testing decision among urban African-American women. Cancer Epi Biom Prev. 2002;11(12):1579–82. [PubMed] [Google Scholar]
- 45.Vos J, Gomez-Garcia E, Oosterwijk JC, et al. Opening the psychological black box in genetic counseling: the psychological impact of DNA testing is predicted by the counselee's perception, the medical impact by the pathogenic or uninformative BRCA1/2 result. Psychooncol. 2010 Nov 11; doi: 10.1002/pon.1864. ahead of print. [DOI] [PubMed] [Google Scholar]
- 46.Ramsey S, Blough D, McDermott C, Clarke L, Bennet R, Burke W, et al. Will knowledge of gene-based colorectal cancer disease risk influence quality of life and screening behavior? Findings from a population-based study. Publ Health Genomics. 2010 Jan 13; doi: 10.1159/000206346. ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Domchek SM, Friebel TM, Singer CF, et al. Association of risk reducing surgery in BRCA1 and BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304(9):967–975. doi: 10.1001/jama.2010.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67(12):2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 49.O'Loughlin J, Paradis G, Kim W, et al. Genetically decreased CYP2D6 and the risk of tobacco dependence: a prospective study of novice smokers. Tob Control. 2004;13(4):422–428. doi: 10.1136/tc.2003.007070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kaphingst KA, LaChance CR, Condit CM. Beliefs about heritability of cancer and health information seeking and preventive behaviors. J Cancer Edu. 2009;24(4):351–356. doi: 10.1080/08858190902876304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Goodenberger M, Lindor NM. Lynch and MYH-associated polyposis: review and testing strategy. J Clin Gastroenterol. 2011 Feb 5; doi: 10.1097/MCG.0b013e318206489c. ahead of print. [DOI] [PubMed] [Google Scholar]
- 52.EGAPP: Recommendation from the EGAPP working group: genetic testing strategies in newly diagnosed individuals with colorectal cancer aimed at reducing morbidity and mortality from Lynch syndrome in relatives. Genet Med. 2009;11(1):35–41. doi: 10.1097/GIM.0b013e31818fa2ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Palomaki GE, McClain MR, Melillo S, Hampel HL, Thibodeau SN. EGAPP supplementary evidence review: DNA testing strategies aimed at reducing morbidity and mortality from Lynch syndrome. Genet Med. 2009;11(1):42–65. doi: 10.1097/GIM.0b013e31818fa2db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Agency for Healthcare Research Quality. Hereditary nonpolyposis colorectal cancer: diagnostic strategies and their implications. [Accessed online March 8, 2011]; at http://www.ahrq.gov/downloads/pub/evidence/pdf/hnpcc/hnpcc.pdf.
- 55.Mvundura M, Grosse SD, et al. Cost effectiveness of genetic testing strategies for Lynch syndrome among newly diagnosed cases of colorectal cancer. Genet Med. 2010;12(2):93–104. doi: 10.1097/GIM.0b013e3181cd666c. [DOI] [PubMed] [Google Scholar]
- 56.Hadley DW, Ashida S, Jenkins JF, Martin JC, Kalzone KA, Kuhn NR, et al. Generation after generation: exploring the psychological impact of providing genetic services through a cascading approach. Genet Med. 2010;12(12):808–15. doi: 10.1097/GIM.0b013e3181f69dbb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.National Cancer Institute, Division of Cancer Control and Population Sciences. comparative effectiveness research in genomics and personalized medicine. [Accessed on March 8, 2011]; at : http://cancercontrol.cancer.gov/od/phg/research.asp?type=CER.
- 58.Kawamoto K, Lobach DF, Willard HF, Ginsburg GS. A national clinical decision support infrastructure to enable the widespread and consistent practice of genomic and personalized medicine. BMC Med Inform Dec Mak. 2009;9:17. doi: 10.1186/1472-6947-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review: A new method of systematic review designed for complex policy interventions. J Health Services Res and Policy. 2005;10(suppl 1):S21–S39. doi: 10.1258/1355819054308530. [DOI] [PubMed] [Google Scholar]
- 60.Glasgow RE. What types of evidence are most needed to advance behavioral medicine? Annals Behav Med. 2008;35(1):19–25. doi: 10.1007/s12160-007-9008-5. [DOI] [PubMed] [Google Scholar]
- 61.Wilfert B, Swen J, Mulder H, et al. From evidence-based medicine to mechanism-based medicine: reviewing the role of pharmacogenetics. Int J Clin Pharmacol. 2011;33(1):3–9. doi: 10.1007/s11096-011-9485-2. [DOI] [PubMed] [Google Scholar]
- 62.EGAPP-Evaluation of Genomic Applications in Practice and Prevention Working Group: Methods of the EGAPP Working Group. [Accessed online March 8, 2001];Genet Med. 2009 11(1):3–14. doi: 10.1097/GIM.0b013e318184137c. at: www.egappreviews.org. [DOI] [PMC free article] [PubMed]
- 63.Evaluation of Genomic Applications in Practice and Prevention Working group. Can tumor gene expression profiling improve outcomes in patients with breast cancer. Genet Med. 2009;11(1):66–73. doi: 10.1097/GIM.0b013e3181928f56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roth JA, Garrison LP, Jr, Burke W, Ramsey SD, Carlsson R, Veenstra DL. Stakeholder perspectives on a risk-benefit framework for genetic testing. Publ Health Genom. 2011;14(2):49–67. doi: 10.1159/000290452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khoury MJ. Dealing with the evidence dilemma in genomics and personalized medicine. Clin Pharmacol Therap. 2010;87(6):636–8. doi: 10.1038/clpt.2010.4. [DOI] [PubMed] [Google Scholar]
- 66.President's Council of Advisors on Science and Technology. Priorities for personalized medicine. [Accessed online March 17, 2011];2008 at: http://www.whitehouse.gov/files/documents/ostp/PCAST/pcast_report_v2.pdf.
- 67.Institute of Medicine. The promises and challenges of improving detection and treatment. National Academies Press; 2007. [Accessed online March 17, 2011]. at: http://www.iom.edu/Reports/2007/Cancer-Biomarkers-The-Promises-and-Challenges-of-Improving-Detection-and-Treatment.aspx. [Google Scholar]
- 68.Sox HC, Greenfield S. Comparative effectiveness research: a report from the Institute of Medicine. Ann Int Med. 2009;151(3):203–5. doi: 10.7326/0003-4819-151-3-200908040-00125. [DOI] [PubMed] [Google Scholar]
- 69.Khoury MJ, McBride CM, Schully SD, et al. The scientific foundation for personal genomics: recommendations from a National Institutes of Health-Centers for Disease Control and Prevention multidisciplinary workshop. Genet Med. 2009;11(8):559–567. doi: 10.1097/GIM.0b013e3181b13a6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Freedman AN, Sansbury LB, et al. Cancer pharmacogenomics and pharmacoepidemiology: setting a research agenda to accelerate translation. JNCI. 2010;102(22):1698–1705. doi: 10.1093/jnci/djq390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.McBride CM, Bowen D, Brody LC, et al. Future health applications for genomics: priorities for communication, behavioral, and social sciences research. Am J Prev Med. 2010;38(5):556–561. doi: 10.1016/j.amepre.2010.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wideroff L, Phillips KA, Randhawa G, et al. A health services research agenda for cellular, molecular and genomic technologies in cancer care. Publ Health Genomics. 2009;12(4):233–244. doi: 10.1159/000203779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Klesges LM, Estabrooks Pa, Glasgow RE, Dzewaltowki D. Beginning with the application in mind: Designing and planning health behavior change interventions to enhance dissemination. Ann Behav Med. 2005;29:66S–75S. doi: 10.1207/s15324796abm2902s_10. [DOI] [PubMed] [Google Scholar]
- 74.National Cancer Institute. [Accessed online April 4, 2011];Designing for Dissemination. www.cancercontrol.cancer.gov/d4d/


